Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Queuing Theory Accurately Models The Need For.32
Caricato da
Hannan KüçükDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Queuing Theory Accurately Models The Need For.32
Caricato da
Hannan KüçükCopyright:
Formati disponibili
ECONOMICS
Anesthesiology 2004; 100:1271 6 2004 American Society of Anesthesiologists, Inc. Lippincott Williams & Wilkins, Inc.
Queuing Theory Accurately Models the Need for Critical Care Resources
Michael L. McManus, M.D., M.P.H.,* Michael C. Long, M.D., Abbot Cooper, Eugene Litvak, Ph.D.
Background: Allocation of scarce resources presents an increasing challenge to hospital administrators and health policy makers. Intensive care units can present bottlenecks within busy hospitals, but their expansion is costly and difcult to gauge. Although mathematical tools have been suggested for determining the proper number of intensive care beds necessary to serve a given demand, the performance of such models has not been prospectively evaluated over signicant periods. Methods: The authors prospectively collected 2 years admission, discharge, and turn-away data in a busy, urban intensive care unit. Using queuing theory, they then constructed a mathematical model of patient ow, compared predictions from the model to observed performance of the unit, and explored the sensitivity of the model to changes in unit size. Results: The queuing model proved to be very accurate, with predicted admission turn-away rates correlating highly with those actually observed (correlation coefcient 0.89). The model was useful in predicting both monthly responsiveness to changing demand (mean monthly difference between observed and predicted values, 0.4 2.3%; range, 0 13%) and the overall 2-yr turn-away rate for the unit (21% vs. 22%). Both in practice and in simulation, turn-away rates increased exponentially when utilization exceeded 80 85%. Sensitivity analysis using the model revealed rapid and severe degradation of system performance with even the small changes in bed availability that might result from sudden stafng shortages or admission of patients with very long stays. Conclusions: The stochastic nature of patient ow may falsely lead health planners to underestimate resource needs in busy intensive care units. Although the nature of arrivals for intensive care deserves further study, when demand is random, queuing theory provides an accurate means of determining the appropriate supply of beds.
crowded ICUs is refused,6 there is incomplete understanding of the limits of the downsizing process and no consensus as to the number of ICU beds necessary to serve a given population.7 Nevertheless, ICUs are among the most complex and expensive of all medical resources, and hospital administrators are challenged to meet the demand for intensive care services with an appropriate capacity. Queuing theory is used widely in engineering and industry for analysis and modeling of processes that involve waiting lines.8 In appropriate systems, it enables managers to calculate the optimal supply of xed resources necessary to meet a variable demand. In the past, attempts have been made to apply queuing analysis to a variety of hospital activities, including cardiac care units,9 obstetric services,10 operating rooms,11,12 and emergency departments,13 as a means of directing the allocation of increasingly scarce resources. More recently, health policy investigators have also sought to apply these techniques more widely across entire healthcare systems.14 16 Unfortunately, most proposed queuing models lack real-world validation17 and, perhaps for this reason, have yet to be embraced by physicians and hospital administrators. Therefore, to explore the utility and implications of queuing theory as it relates to the supply and demand for critical care services, we sought to validate a simple queuing model in a busy ICU.
IN the United States, after more than a decade of healthcare restructuring, the number of hospitals continues to decline.1 In some regions of the country, this has produced serious overcrowding, particularly in emergency departments2 4 and intensive care units (ICUs).5 Although there may be growing recognition that mortality is increased among patients to whom admission to
Materials and Methods
We studied all admissions to the medicalsurgical ICU of a large, urban childrens hospital during a 2-yr period. The 18-bed unit provides all manner of noncardiac intensive care services and, in addition to local emergencies, serves a large regional, national, and international referral population. During periods of high demand, external requests for transfer are diverted to other institutions in the region, whereas internal overow is accommodated in off-service care sites, such as the PACU or available beds in a separate, specialized cardiac ICU. Data were collected prospectively as part of the units patient care database and are analyzed here for frequency of admission requests, durations of stay, and crowding. Queuing analysis is dependent on accurate measurement of three variables: arrival rate, service time, and the number of servers in the system. We therefore collected data with special attention to the corresponding hospital
* Department of Anesthesia and the Multidisciplinary Intensive Care Unit, Childrens Hospital Boston, and Associate Professor, Harvard Medical School. Senior Anesthetist, Massachusetts General Hospital, and Adjunct Associate Professor, Boston University School of Management. Senior Analyst, Professor of Operations Management and Director, Boston University Health Policy Institute Program on Variability. Received from the Department of Anesthesia, Pain and Perioperative Medicine, Childrens Hospital, Boston, Massachusetts, and the Health Policy Institute, Boston University, Boston, Massachusetts. Submitted for publication May 28, 2003. Accepted for publication November 15, 2003. Support was provided solely from institutional and/or departmental sources. Address reprint requests to Dr. McManus: Childrens Hospital, 300 Longwood Avenue, Boston, Massachusetts 02115. Address electronic mail to: michael.mcmanus@childrens.harvard.edu. Individual article reprints may be purchased through the Journal Web site, www.anesthesiology.org.
Anesthesiology, V 100, No 5, May 2004
1271
1272
MCMANUS ET AL.
Fig. 1. Distribution of intensive care unit durations of stay over a 2-yr period. Data include all stays of 30 or fewer days and are described by the equation y 227.95e 0.1662 with R2 0.8208.
variables (admission rate, duration of stay, and number of available beds) prospectively. For purposes of modeling, all patients referred for (requesting) admission were considered arrivals. Durations of stay were calculated as (discharge date) (admission date), with all admissions assigned a minimum of 1 day. A computer simulation model of ICU ow was then constructed using spreadsheet software (Excel 2000; Microsoft Corporation, Redmond, WA) and standard queuing formulae.18 The ICU was modeled as a multichannel, single-stage system of identical parallel servers that process randomly patterned arrivals according to exponentially distributed service times. Each ICU bed was treated as one server and a rst come, rst served queuing discipline was assumed. It was further understood that no waiting line was possible for these critically ill patients and, therefore, the probability of waiting equals the probability of rejection. Such a system has been suggested by others as an appropriate construct for evaluating turn-away probabilities and, in the queuing literature, is denoted as M/M/c/c (shorthand notation for systems involving Markovian interarrival times, which are modeled as a Poisson process, Markovian service times, c servers, and c spaces in the system).16 Readers unfamiliar with queuing theory may nd introductions, useful tutorials, and downloadable software suitable for duplicating this work on numerous Internet sites such as those listed in the appendix. With observed monthly admission rates, available beds, and stay durations as inputs, monthly utilizations and rejection probabilities were calculated using queuing theory. Summary calculations over the 2-yr period were also completed. For purposes of monthly analysis, any bed occupied for more than 1 continuous month by the same patient was treated as a bed lost to the system. During the occupied month, therefore, the number of servers in the model was reduced, and the correspondAnesthesiology, V 100, No 5, May 2004
ing admission days were not included in that months duration-of-stay calculations. Associated admission days carrying over into contiguous months were treated as separate admissions when calculating those months average durations of stay. Patients to whom admission was refused and who were transported to another hospital or those diverted to an alternative care site within the hospital (e.g., PACU or specialty ICU) because a bed was unavailable in the primary unit were considered rejected or turn aways. Observed rejection rates were calculated as: (no. of patients refused no. of patients diverted)/total no. of patients requesting admission. During portions of the observation period when the practice was to always maintain one open bed in the primary unit for new in-house emergencies, the total number of available servers in the model was decreased by 1. Very brief ( 1 day) bed closures due to stafng shortfalls were neglected. Statistical Analysis The queuing model selected assumes that daily admission rates (arrivals) follow a Poisson distribution (coefcient of variation 1) and that durations of stay (service times) are either constant or follow an exponential distribution. Others have shown that the arrival rate of patients to ICUs follows a Poisson distribution,7,19 and this behavior was conrmed in data here both by coefcient of variation (1.1) and Kolmogorov-Smirnov test (with t accuracy of 0.0003 and of 0.05, a Poisson distribution is not rejected, P 0.262, using Statt; Geer Mountain Software Corporation, South Kent, CT). As illustrated in gure 1, durations of stay were found to follow an exponential distribution. Validity of the queuing model was assessed using a correlated inspection approach20 with agreement between observed turnaway rates and those predicted by the model assessed
QUEUING THEORY MODELS FOR INTENSIVE CARE
1273
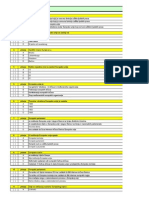
Table 1. Monthly Intensive Care Unit Service Parameters over 2 Years
Month Admissions Beds Available for New Admissions Average Duration of Stay, days Utilization, % Ambulance Diversions Off-service Diversions Total Rejections
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Total
145 155 156 138 139 145 166 144 141 147 170 163 192 166 152 143 145 155 152 160 148 159 142 158 3,680
17 17 17 17 17 18 18 18 18 18 18 18 17 17 15 13 15 16 15 17 17 17 15 16
3.2 3.7 2.8 4.6 3.7 3.5 3.3 3.2 3.5 3.3 3.5 2.5 2.8 3.8 4.4 4.0 4.5 3.3 3.5 3.9 2.4 3.2 3.7 3.6 3.5
78 88 76 89 82 81 83 76 80 78 86 71 84 89 91 90 90 85 86 88 69 82 86 86 83
0 0 0 0 0 0 0 0 0 2 6 2 0 14 14 5 15 12 4 13 3 3 5 8 106
24 35 24 22 12 20 24 4 10 11 28 10 36 34 64 54 45 36 36 31 18 20 35 31 664
24 35 24 22 12 20 24 4 10 13 34 12 36 48 78 59 60 48 40 44 21 23 40 39 770
via linear regression, paired t test, and standard residual analysis (SPSS software; Chicago, IL).
Results
There were 3,786 requests for admission during the period studied. Of these, 3,680 were admitted to the hospital and 106 were diverted to other institutions. Of admissions, 1,374 were patients requiring care for medical illnesses and 2,306 required management of issues related to surgery. Of surgical patients, 2,131 were admitted for care after scheduled procedures whereas 175
were admitted after emergency procedures or unanticipated intraoperative events. Overall service parameters for the study period are presented in table 1. Monthly average admission request rates ranged from 4.6 to 6.2 patients/day. Individual durations of stay ranged from 1 to 190 days. Monthly average durations of stay ranged from 2.4 to 5.5 days. Seventeen patients had durations of stay greater than 45 days, with each occupying a bed for more than 1 calendar month. In addition, during short periods, up to two beds were closed for administrative reasons. In the 18-bed unit, then, the actual number of available beds ranged from 13 to 18 (mean 17).
Fig. 2. Monthly intensive care unit utilization and rejection rates. Diamonds monthly rejection rates predicted by the queuing model; squares percent of total admission requests that could not be accommodated; triangles percent utilization of unit resources during each month.
Anesthesiology, V 100, No 5, May 2004
1274
MCMANUS ET AL.
Fig. 3. Intensive care unit (ICU) rejection rate as a function of utilization. The least squares curve t to the data is described by the equation y 0.0003e7.8221 with r2 0.53.
Observed monthly turn-away rates varied widely, ranging from 3 to 47% (g. 2). Over the observation period, turn-away rates corresponded closely to calculated utilization and were accurately predicted by the queuing model (correlation coefcient 0.897; P 0.001). Overall, the mean difference between observed and predicted values was 0.4% (95% paired t condence interval 2.3%) with a maximum difference of 13% and minimum of 0. Residual and normal probability plots (not shown) contained no signicant outliers or systematic deviations, while the plot of residuals versus predicted values disclosed no nonlinear dependences. For the entire 2-yr period, the observed overall turn-away rate was 21%, and that predicted by the model (using 2-yr average duration of stay and overall average admission rates as inputs) was 22%. In practice, it was observed that when utilization in-
creased above 80 85%, blocking rates (hospital diversions off service transfers) increased abruptly (g. 2). At the highest utilization rate (91%), nearly one half (48%) of all requests for admission could not be accommodated. As illustrated in gure 3, the observed rejection rate was best viewed as an exponential function of utilization. This behavior is consistent with predictions from queuing theory and is widely appreciated as a general property of systems involving waiting lines.21 Sensitivity analysis using the model illustrates the impact of bed closure or patients with very long stay durations on the responsiveness of ICUs running near capacity. Using data from a representative month as inputs, an average admission rate of 5.7 patients/day and a 3.5-day average duration of stay yielded a predicted utilization rate of 86%. The associated predicted rejection rate (21%) agreed well with the observed rejection
Fig. 4. Sensitivity of rejection rate to the number of available intensive care beds. Diamonds utilization; squares rejection rate. As utilization increases above approximately 85%, further increases are accompanied by large increases in rejection rate. At high utilization rates, loss of even a few available beds markedly increases rejections.
Anesthesiology, V 100, No 5, May 2004
QUEUING THEORY MODELS FOR INTENSIVE CARE
1275
rate (19%), and the corresponding monthly utilization was similar to the overall average observed during the 2 yr studied. Given these routine parameters, gure 4 illustrates the tradeoff between utilization and turn-away rate as the number of available beds is varied (whether by stafng changes or the presence of patients with long stays). Because utilization rates approach 100% asymptotically while rejection rates increase exponentially, small gains in utilization are accompanied by rapid degradation of the ability to handle new admissions. This graphically illustrates the dilemma facing many ICUs: Units nancially forced to high utilization must increasingly reject new admissions.
Discussion
This 2-yr experience illustrates that queuing theory may be used to accurately model ICU bed utilization in a large unit operating at or near capacity. Here, the correlation between observed and predicted turn-away rates was extremely high, particularly when noting that dayto-day variations in bed availability (due to patient ow, temporary stafng issues, or the special bed requirements of individual patients) were not considered. To our knowledge, this is the largest experience comparing prospectively acquired data from a functioning ICU with the behavior predicted by a stochastic model. Although the ndings here may be generalized to similar units facing similar demand patterns, they are not necessarily applicable to smaller units, units operating below capacity, or units containing specialized subunits. For example, the results here may signicantly underestimate stresses on smaller units because, for a given utilization rate, rejection rates are higher in smaller than in larger service systems.22 Similarly, the sensitivity analysis provided in gure 3 describes functioning to be expected under arrival rate and service time patterns similar to those observed in our unit. Units with signicantly different patient ow patterns might behave differently. Despite the above limitations, this analysis holds at least four practical implications. First, it clearly demonstrates that the realistic capacity of an ICU is signicantly overestimated by measures that fail to account for the variability of demand. Because patient arrivals are random, occupancy rates are more appropriately discussed in terms of probabilities. As demonstrated here, amid a xed number of available beds, these probabilities are mathematically determined by duration of stay and arrival rate. Common measures of utilization, such as daily census and average occupancy, fail to capture owrelated stresses in the system and mask the reality that patients may frequently be denied access even if the unit seems less than full. A corollary to the above observation is that when utilization is maintained at high levels, there is increasing
Anesthesiology, V 100, No 5, May 2004
probability that patients will be rejected from the system. As the data show, for a typical range of stay durations and arrival rates, lower utilization necessarily produces lower rejection rates, and higher utilization produces higher rejection rates. In the past, conventional wisdom has held that average occupancy targets of 85% may be considered optimal.7 The ndings here are consistent with this because utilization above 85% was associated with rapidly increasing rejection rates. However, averages may be misleading because seemingly acceptable average utilization of 83% may mask prolonged periods of higher utilization wherein rejection rates might be unacceptable. Therefore, for a system to respond adequately to natural peaks in demand, true continuous utilization must be limited, and a predictable number of empty beds must always be maintained in readiness. Although not the subject here, the associated cost of this readiness could be calculated using queuing theory and fairly assigned to beneting stakeholders. Third, the queuing model shows the exquisite sensitivity of bed crises to sudden stafng shortfalls or the presence of patients with extremely long durations of stay. Because both conditions effectively lower the number of available servers, they rapidly degrade the performance of the system. For this reason, analyses that rely on simple duration of stay averages but do not appropriately adjust the number of available servers may tend to overestimate the performance of the system. However, as demonstrated here, if server number is accurately accounted for, queuing theory may be useful in making decisions regarding stafng costs and construction of step-down units. Finally, to the extent that ICU resources are expensive and often saturated, it is important to reconsider the nature of patient arrival patterns. Here, overall arrivals rates were found to be random, and this randomness permitted successful application of a standard stochastic model. However, it is puzzling that this is so when the majority of admissions resulted from scheduled surgical procedures. Although the utilization and rejection relations described above are mathematical consequences of variability within the system, operations management teaches that lower rejection rates should be anticipated if this variability can be reduced. Therefore, more effective management of the elective surgery scheduling process could produce a much smoother demand pattern and, as a result, increase the effective capacity of busy units. Sources of variability may be classied as natural when they result from uncontrollable variations in disease prevalence, severity, or responsiveness and may be classied as articial when they result from controllable variations in the manner by which we choose to deliver care.23 Here, a substantial amount of articial variability can be inferred because the unit modeled precisely as a random process despite the presence of substantial schedulable patient ow. In separate studies, we have
1276
MCMANUS ET AL.
attempted to estimate the impact of uncontrolled patient ow variability on access to intensive care.24 Traditionally, regional requirements for ICU beds have been determined by historical experience and population estimates.25 However, in a market-driven or otherwise nancially austere environment, such determinations are increasingly based on average census gures and occupancy rates. When shortfalls arise or disaster responses are planned, it may be difcult for legislators, health planners, and hospital executives to grasp the true capacity of an intensive care delivery system. Findings here suggest that queuing theory represents a simple and reasonable rst approach to analysis of ICU capacity until more sophisticated and robust models become available.
References
1. American Hospital Association: Hospital Statistics, 2002 edition. Chicago, Health Forum, LLC2002 2. Derlet RW, Richards JR, Kravitz RL: Frequent Overcrowding in U.S. emergency departments. Acad Emerg Med 2001; 8:1515 3. McCabe JB: Emergency department overcrowding: A national crisis. Acad Med 2001; 76:672 4 4. Schull MJ, Szalai J-P, Schwartz B, Redelmeier DA: Emergency department overcrowding following systematic hospital restructuring: Trends at twenty hospitals over ten years. Acad Emerg Med 2001; 8:1037 43 5. Nelson M, Waldrop RD, Jones J, Randall Z: Critical care provided in an urban emergency department. Am J Emerg Med 1998; 16:56 9 6. Metcalfe MA, Sloggett A, McPherson K: Mortality among appropriately referred patients refused admission to intensive-care units. Lancet 1997; 350: 711 7. Green LV: How many hospital beds? Inquiry 2002; 39:400 12 8. Duckworth WE: Operational Research Techniques. London, Methuen & Co., 1962 9. Cooper JK, Corcoran TM: Estimating bed needs by means of queuing theory. N Engl J Med 1974; 291:404 5 10. Milliken RA, Rosenberg L, Milliken GM: A queuing theory model for the prediction of delivery room utilization. Am J Obstet Gynecol 1972; 114:6919 11. Taylor TH, Jennings AM, Nightingale DA, Barber B, Leivers D, Styles M, Magner J: A study of anesthetic emergency work: I. The method of study and introduction to queuing theory. Br J Anaesth 1969; 41:70 5
12. Tucker JB, Barone JE, Cecere J, Blabey RG, Rha CK: Using queueing theory to determine operating room stafng needs. J Trauma 1999; 46:719 13. Scott DW, Factor LE, Gorry GA: Predicting the response time of an urban ambulance system. Health Serv Res 1978; 13:404 17 14. el-Darzi E, Vasilakis C, Chaussalet T, Millard PH: A simulation modeling approach to evaluating length of stay, occupancy, emptiness and bed blocking in a hospital geriatric department. Health Care Manag Sci 1998; 1:1439 15. Bagust A, Place M, Posnett JW: Dynamics of bed use in accommodating emergency admissions: Stochastic simulation model. BMJ 1999; 319:155 8 16. Mulligan JG: The stochastic determinants of hospital-bed supply. J Health Econ 1985; 4:177 85 17. Costa AX, Ridley SA, Shahani AK, Harper PR, De Senna V, Nielsen MS: Mathematical modelling and simulation for planning critical care capacity. Anaesthesia 2003; 58:320 7 18. Gross D, Harris CM: Fundamentals of Queueing Theory, 3rd edition. Indianapolis, Wiley & Sons, 1998 19. Milne E, Whitty P: Calculation of the need for paediatric intensive care beds. Arch Dis Child 1995; 73:5057 20. Law AM, Kelton WD: Simulation Modeling and Analysis, 3rd edition. Boston, McGraw-Hill, 2000 21. Hillier F, Lieberman G: Introduction to Operations Research, 6th edition. Boston, McGraw-Hill, 1995 22. Whitt W: Understanding the efciency of multi-server service systems. Management Sci 1992; 38:708 23 23. Litvak E, Long MC: Cost and quality under managed care: Irreconcilable differences? Am J Manag Care 2000; 6:30512 24. McManus ML, Long MC, Cooper AB, Mandell J, Berwick DM, Pagano M, Litvak E: Variability in surgical caseload and access to intensive care services. ANESTHESIOLOGY 2003; 98:1491 6 25. Schwartz S, Cullen DJ: How many intensive care beds does your hospital need? Crit Care Med 1981; 9:6259
Appendix: Selected Queuing Resources Available on the Internet
1. Ferrier A: An Introduction to Queueing Theory. 1999. Available at: http://www.new-destiny.co.uk/andrew/past_work/queueing_theory/ Andy/. Accessed October 10, 2003 2. Slater T: The Queueing Theory Tutor. 2000. Available at: http:// www.dcs.ed.ac.uk/home/jeh/Simjava/queueing/. Accessed October 10, 2003 3. Ingolfsson A, Gallop F: Queueing ToolPak 3.0. 2002. Available at: http://www.bus.ualberta.ca/aingolfsson/QTP/. Accessed October 10, 2003 4. Kamath M: A Software Package for Rapid Analysis of Queueing Systems [RAQS]. 2001. Available at: http://www.okstate.edu/ cocim/raqs/. Accessed October 10, 2003
Anesthesiology, V 100, No 5, May 2004
Potrebbero piacerti anche
- 21 - ICOnEC - 2015 - Badea IrinaDocumento9 pagine21 - ICOnEC - 2015 - Badea IrinaHannan KüçükNessuna valutazione finora
- BankScopeUG 2014Documento346 pagineBankScopeUG 2014Hannan KüçükNessuna valutazione finora
- Pitanja Za Ispit Općeg ZnanjaDocumento184 paginePitanja Za Ispit Općeg ZnanjaRizlak100% (1)
- FMWWW - Bc.edu Repec Bocode X Xtabond2Documento17 pagineFMWWW - Bc.edu Repec Bocode X Xtabond2Hannan KüçükNessuna valutazione finora
- SP 111014Documento9 pagineSP 111014Hannan KüçükNessuna valutazione finora
- Hadith of The Day - 99 Names of Allah (SWT)Documento18 pagineHadith of The Day - 99 Names of Allah (SWT)Hannan KüçükNessuna valutazione finora
- Basel3 Phase in ArrangementsDocumento1 paginaBasel3 Phase in ArrangementsVytalyNessuna valutazione finora
- Getting Started with Bankscope DatasetDocumento43 pagineGetting Started with Bankscope DatasetAliNessuna valutazione finora
- Arellano BondDocumento22 pagineArellano BondVu Thi Duong BaNessuna valutazione finora
- Bank Capital RequirementDocumento106 pagineBank Capital RequirementMuhammad KhurramNessuna valutazione finora
- Basel 3 Summary TableDocumento1 paginaBasel 3 Summary TableIzian SherwaniNessuna valutazione finora
- Geneve Chapitre2Documento83 pagineGeneve Chapitre2Hannan KüçükNessuna valutazione finora
- Prikaz ProhaskaDocumento6 paginePrikaz ProhaskaHannan KüçükNessuna valutazione finora
- Bank CapitalDocumento37 pagineBank CapitalHannan KüçükNessuna valutazione finora
- Economic Regulatory ActualDocumento30 pagineEconomic Regulatory ActualHannan KüçükNessuna valutazione finora
- 0003520Documento149 pagine0003520Hannan KüçükNessuna valutazione finora
- The Relationship Between Capital Requirements and Bank BehaviorDocumento34 pagineThe Relationship Between Capital Requirements and Bank BehaviorHannan KüçükNessuna valutazione finora
- Article 07 The Relationship Between Capital StructureDocumento10 pagineArticle 07 The Relationship Between Capital StructureHannan KüçükNessuna valutazione finora
- Gupea 2077 19299 1Documento55 pagineGupea 2077 19299 1Hannan KüçükNessuna valutazione finora
- Goodness of Fit FariasDocumento15 pagineGoodness of Fit FariasHannan KüçükNessuna valutazione finora
- Rutgers Lib 34217 PDF 1Documento147 pagineRutgers Lib 34217 PDF 1Hannan KüçükNessuna valutazione finora
- 0003520Documento149 pagine0003520Hannan KüçükNessuna valutazione finora
- 2013-24 - Spring - Study Questions For Final ExamDocumento9 pagine2013-24 - Spring - Study Questions For Final ExamHannan KüçükNessuna valutazione finora
- Measuring Inequality: Using The Lorenz Curve and Gini CoefficientDocumento4 pagineMeasuring Inequality: Using The Lorenz Curve and Gini CoefficientHannan KüçükNessuna valutazione finora
- Https Doc 14 BK Apps Viewer - GoogleusercontentDocumento14 pagineHttps Doc 14 BK Apps Viewer - GoogleusercontentHannan KüçükNessuna valutazione finora
- The International Monetary System, 1870 - 1973: Slides Prepared by Thomas BishopDocumento42 pagineThe International Monetary System, 1870 - 1973: Slides Prepared by Thomas BishopJeyshree GkmNessuna valutazione finora
- The 2012 Overture:: An Overview of Municipal BondsDocumento14 pagineThe 2012 Overture:: An Overview of Municipal BondsHannan KüçükNessuna valutazione finora
- Chap 019Documento11 pagineChap 019Hannan KüçükNessuna valutazione finora
- Banks or Bonds? Building A Municipal Credit Market: George E. Peterson Senior Fellow The Urban Institute Washington, DCDocumento18 pagineBanks or Bonds? Building A Municipal Credit Market: George E. Peterson Senior Fellow The Urban Institute Washington, DCHannan KüçükNessuna valutazione finora
- Assessment of Local Economic Development Capacities According To Business-Friendly Scheme in Case of Tešanj'S MunicipalityDocumento4 pagineAssessment of Local Economic Development Capacities According To Business-Friendly Scheme in Case of Tešanj'S MunicipalityHannan KüçükNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (72)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- A A A A C C C C A A A A D D D D Eeee M M M M IIII C C C C S S S S C C C C IIII Eeee N N N N C C C C Eeee S S S SDocumento3 pagineA A A A C C C C A A A A D D D D Eeee M M M M IIII C C C C S S S S C C C C IIII Eeee N N N N C C C C Eeee S S S SnelisaNessuna valutazione finora
- Military Nurses in VietnamDocumento3 pagineMilitary Nurses in VietnamChildren Of Vietnam Veterans Health Alliance100% (2)
- Essential VDocumento4 pagineEssential Vapi-385640092Nessuna valutazione finora
- Fertility AwarenessDocumento5 pagineFertility AwarenessGabriela GascaNessuna valutazione finora
- Bedside Output: Jehanna Mar E. Abdurahman Adzu Som Level IDocumento6 pagineBedside Output: Jehanna Mar E. Abdurahman Adzu Som Level IJehannaMarEnggingAbdurahmanNessuna valutazione finora
- Eye Exam Guide for Common Structures & Visual TestsDocumento32 pagineEye Exam Guide for Common Structures & Visual TestsArlyn Mendenilla100% (1)
- SALAM Specialist Hospital Floor PlanDocumento1 paginaSALAM Specialist Hospital Floor PlanIT Dept. SALAM SPECIALIST HOSPITAL KUALA TERENGGANUNessuna valutazione finora
- HOSPITAL LISTINGDocumento12 pagineHOSPITAL LISTINGSiddharth KumarNessuna valutazione finora
- Orthotics - ProstheticsDocumento8 pagineOrthotics - Prostheticsalpriani patrasNessuna valutazione finora
- Yellow Fever Vaccination Centre in MalaysiaDocumento9 pagineYellow Fever Vaccination Centre in MalaysiaAngeline LeeNessuna valutazione finora
- Criticare Vitalcare 506N3 - Service Manual PDFDocumento254 pagineCriticare Vitalcare 506N3 - Service Manual PDFLuis Colipí SantanderNessuna valutazione finora
- Project 599204 Epp 1 2018 1 It Eppka1 JMD MobDocumento2 pagineProject 599204 Epp 1 2018 1 It Eppka1 JMD MobHafsal M HNessuna valutazione finora
- Laying Out Arnold Palmer HospitalDocumento2 pagineLaying Out Arnold Palmer HospitalazilaNessuna valutazione finora
- Johan KipsDocumento29 pagineJohan KipsdagensmedicinNessuna valutazione finora
- Dr. Witra Irfan, SP.B (K) V - DVTDocumento29 pagineDr. Witra Irfan, SP.B (K) V - DVTmuhammad azharanNessuna valutazione finora
- (UGM) Pengumuman Abstrak NSCE 2018Documento4 pagine(UGM) Pengumuman Abstrak NSCE 2018ahmadNessuna valutazione finora
- Hypoglycemic Activity of Java Plum (Syzygium Cumini) Fruit Extract in Albino Winster Rat ObjectivesDocumento2 pagineHypoglycemic Activity of Java Plum (Syzygium Cumini) Fruit Extract in Albino Winster Rat ObjectivesAguilan, Alondra JaneNessuna valutazione finora
- DAFTAR HARGA TGL. 04 JANUARI 2022Documento52 pagineDAFTAR HARGA TGL. 04 JANUARI 2022lllaelaNessuna valutazione finora
- Super Mental TrainingDocumento259 pagineSuper Mental TrainingWilliam Dias de Andrade100% (1)
- Local Anesthesia in Pediatric Dentistry Lecture Students 2009 MDocumento88 pagineLocal Anesthesia in Pediatric Dentistry Lecture Students 2009 MIoana DănilăNessuna valutazione finora
- 3) Buku Log Clinical Practice Record PERIOPERATIVE CAREDocumento41 pagine3) Buku Log Clinical Practice Record PERIOPERATIVE CAREAslam AssandakaniNessuna valutazione finora
- YDS Phrasal Verb Soru TipiDocumento7 pagineYDS Phrasal Verb Soru TipiAhmet GürkanNessuna valutazione finora
- CancerDocumento84 pagineCancerKaruna KumariNessuna valutazione finora
- Myasthenia GravisDocumento7 pagineMyasthenia Gravisエド パジャロン100% (1)
- Benefits of Breast FeedingDocumento4 pagineBenefits of Breast FeedingAzAm KiOngNessuna valutazione finora
- Noakes 2000Documento23 pagineNoakes 2000Nicolás Ayelef ParraguezNessuna valutazione finora
- HirsutismDocumento19 pagineHirsutismCita KresnandaNessuna valutazione finora
- Journal ClubDocumento3 pagineJournal ClubNephrology On-DemandNessuna valutazione finora
- Arachnoid Granulations PDFDocumento5 pagineArachnoid Granulations PDFsebacosNessuna valutazione finora
- International Business: Anglo American PLC Case StudyDocumento10 pagineInternational Business: Anglo American PLC Case StudySujeet KumarNessuna valutazione finora