Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Medical Disorders and Orthodontics
Caricato da
Amir MirDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Medical Disorders and Orthodontics
Caricato da
Amir MirCopyright:
Formati disponibili
Journal of Orthodontics, Vol.
36, 2009, 121
Medical disorders and orthodontics
Anjli Patel
Chesterfield Royal Hospital NHS Foundation Trust, Charles Clifford Dental Hospital, Sheffield, UK
Donald J Burden
Orthodontic Division, The Queens University of Belfast, UK
Jonathan Sandler
Chesterfield Royal Hospital NHS Foundation Trust, UK
The orthodontic treatment of patients with medical disorders is becoming an increasing aspect of modern day practice. This article will draw attention to some of the difficulties faced when orthodontic treatment is provided and will make recommendations on how to avoid potential problems. Key words: Medical disorders, orthodontics, guidelines
Introduction
An increasing number of patients with complicated medical conditions and drug regimes are seeking orthodontic treatment. Progress in medicine, higher expectations of quality of life, increased life expectancy have resulted in a greater demand for elective dental and medical treatment.1 Orthodontists need to be aware of the possible clinical implications of many of these diseases. In addition orthodontists see their patients every 6 to 8 weeks and rapidly developing medical problems can manifest themselves at any age. Orthodontists must remain vigilant as they may be the only health care professional seen by otherwise t, young patients on a regular basis. This article examines aspects of some of the conditions that are of relevance to orthodontic practice. A comprehensive medical history should be taken and regularly updated. Case notes should alert the clinician to the patients medical status. All medical conditions should be accurately understood before any treatment is planned and this may involve seeking guidance from the patients physician. Patients should be well informed of all the options and made aware that any orthodontic treatment has been planned with their best interests at heart. It should be highlighted they are not being penalized for their medical condition.2 The importance of excellent oral hygiene should be emphasized to all patients considering a course of orthodontics.
prior to an invasive procedure that could generate a bacteraemia has been a founding principle of dental practice for half a century, although the evidence of benet is limited. Very few cases of IE are now secondary to oral streptococci and Staphylococcus aureus is now the most common pathogen.4 The lack of evidence from human models and changing clinical prole of IE has led several authorities to update their guidelines in recent years (Table 1). Most authorities across Europe and from the United States of America recommend the use of prophylaxis prior to invasive procedures in high-risk patients.58 The National Institute for Health and Clinical Excellence (NICE) issued the most recent guidance for dental practitioners in the United Kingdom in March 2008. NICE has recommended that antibiotic prophylaxis should not be used in patients at risk of infective endocarditis undergoing dental procedures. In addition NICE advises that chlorhexidine mouthwash should not be offered as prophylaxis against IE in at risk patients.9 NICE have based their guidelines on the following facts:
Cardiovascular system
Infective endocarditis (IE)
IE is a rare condition with a high mortality and morbidity.3 The primary prevention of IE is very important. Antibiotic prophylaxis for such patients
N N
The efficacy of antibiotic prophylaxis for IE has never been shown in a randomized trial. A Cochrane review concluded that there was no evidence to support the use of penicillin prophylaxis.10 A direct link between routine orthodontic or dental procedures and IE has never been established conclusively. Although four cases of endocarditis have been reported in patients undergoing orthodontic treatment, no evidence was presented to confirm that orthodontic treatment was a causal factor.1113 General dental and skin hygiene are probably more important for the prevention of IE. The use of antibiotics is by no means risk free. Although prophylactic regimes suggest single dose
Address for correspondence: Jonathan Sandler, Chesterfield Royal Hospital NHS Foundation Trust, Chesterfield Rd, Calow, Chesterfield, S44 5BL, UK. Email: jonsandler@aol.com # 2009 British Orthodontic Society Originally translated into German and published in Information aus Orthodontie und Kieferorthopaedie 2009; 41: 2341. Republished here by permission of Georg Thieme Verlag kG Stuttgart. New York
DOI 10.1179/14653120723346
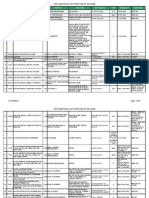
Table 1
Guidelines for the prevention of IE in dentistry National Insitute for Health and Clinical Excellence 2008
2 Patel et al.
European Society of Cardiology 2004 Previous IE. Cardiac valve replacement. Prosthetic systemic or pulmonary shunt or conduit. Previous IE. Cardiac valve replacement. Prosthetic systemic or pulmonary shunt or conduit. Prosthetic valve. Previous IE. Unrepaired or incompletely repaired cyanotic congenital heart disease (CHD). CHD repaired with prosthetic material for 6 months after procedure. Valve disease in cardiac transplant recipients
French Guidelines 2002
British Society for Antimicrobial American Heart Association Chemotherapy 2006 2007
High-risk patients
Prosthetic heart valve, complex congenital cyanotic heart diseases. Previous IE. Prosthetic systemic or pulmonary shunt or conduit. Mitral valve prolapse with valvular regurgitation/severe valve thickening. Non cyanotic congenital heart diseases including bicuspid aortic valves. Hypertrophic cardiomyopathy
Clinical Section
Previous IE. Acquired valvular heart disease with stenosis/regurgitation. Prosthetic valve. Structural CHD including surgically corrected or palliated structural defect excluding isolated atrial septal defect, fully repaired ventricular septal defect or fully repaired patent ductus arteriosus, and closure devices deemed to be endothelialised. Hypertrophic cardiomyopathy
Low-risk patients
Secundum type artial septal defect
Dental procedures requiring prophylaxis in high-risk patients
Dental procedures with risk of gingival/mucosal trauma
Other valve disease mitral valve prolapse with mitral insufficiency, valve thickening. Noncyanotic CHD except Atrial septal defect. Hypertrophic obstructive cardiomyopathy All invasive dental procedures
All invasive dental procedures
JO December 2009
Dental procedures None requiring prophylaxis in moderate- and lowrisk patients
None Optional based on clinical assessment of patient and procedure. Can be given post-op if procedure unduly complex
None Dental procedures involving manipulation of gingival tissue, periapical area of teeth or perforation of oral mucosa. None None
JO December 2009
Clinical Section
Medical disorders and orthodontics
administration, from which non-fatal side effects are usually minor, there is a risk of fatal anaphylaxis, which affects 1225 people per million.14
Orthodontic considerations in patients with cardiovascular disorders
N
Orthodontic considerations in patients with cardiovascular disorders
A risk of bacteraemia induced by traction of unerupted, exposed and bonded teeth has been suggested. Lucas and associates studied the prevalence, intensity and nature of bacteraemia following upper arch debanding in 42 patients and gold chain adjustment in seven patients.18 The authors found no significant difference in the prevalence of bacteraemia between baseline and following debanding or gold chain adjustment. Admittedly the sample size for gold chain adjustment was small
N N
The orthodontist should communicate with the patients physician to confirm the risk of IE. The orthodontist should offer people at risk of IE clear and consistent information about prevention including the following factors: # The risks and benefits of antibiotic prophylaxis and an explanation of why antibiotic prophylaxis is no longer routinely recommended in the United Kingdom. # The importance of maintaining an exemplary standard of oral hygiene and that it is their responsibility to protect themselves. Regular supportive therapy from a hygienist is also advisable. The risk of using electric toothbrushes is poorly defined but a pilot study showed that brushing with a powered toothbrush results in a transient bacteraemia more frequently than brushing with a manual or ultrasonic toothbrush.15 The authors concluded that the resulting bacteraemia might affect patients with congenital heart defects at risk of bacterial endocarditis. However, their results show that vigorous brushing increased bacteraemia from brushing once but do not answer whether bacteraemia incidence would decrease with a program of vigorous daily brushing. # Symptoms that may indicate IE and when to seek specialist advice. The risk of undergoing invasive procedures, including non-medical procedures such as body piercing or tattooing.
Any episode of infection in people at risk of IE should be investigated and treated promptly.
Haematology and patients with bleeding problems
Disorders of the blood, whether acquired or inherited can affect the management of orthodontic patients. Mild bleeding disorders are not problematic to the orthodontist but patients with severe disorders may require more care. A history of a clinically signicant episode is one that
N N N N
continues beyond 12 h requires a patient to call or return to their dental practitioner or seek medical treatment or emergency care results in the development of a haematoma or ecchymosis within the soft tissues requires blood product support.19
The main orthodontic procedure that has been postulated to cause a bacteraemia has been placement of a separator.16 Lucas and co-workers investigated the bacteraemia associated with an upper alginate impression, separator placement, band placement and adjustment of an archwire on a fixed appliance. Blood samples were taken from randomly allocated orthodontic patients immediately before the intervention and then 30 s after the procedure. The mean total number of anaerobic and aerobic bacteria was significantly greater following the placement of a separator, compared with baseline blood cultures. There was no difference noted between baseline and taking an impression or placement of a band. Using similar methodology, Burden and colleagues did not detect a significant difference in the prevalence of pre-debanding (3%) and post-debanding (13%) bacteraemia.17 The authors concluded that this is lower than the prevalence of bacteraemia following toothbrushing and those procedures do not warrant antibiotic prophylaxis.
Inherited coagulopathies deficiencies in clotting factors
Haemophilia is a common example of a clotting factor deciency. Haemophilia A is a sex-linked disorder due to a deciency of Factor VIII. When the Factor VIII level is less than 1% of normal, the condition is classied as severe.20 Other bleeding disorders include Haemophilia B or Christmas disease (factor IX deciency) and von Willebrands disease (defects of von Willebrands factor). As well as problems with bleeding, these patients may be infected with HIV or hepatitis viruses because of the transfusion of infected blood or blood products before 1985. The methods of screening and manufacture have improved, but they do not rule out the risk of virus transmission entirely. The UK Department of Health
The use of orthodontic bands and fixed acrylic appliances should be avoided whenever possible in high-risk patients with poor oral hygiene.
Patel et al.
Clinical Section
JO December 2009
(DoH) carried out a risk assessment concluding that all recipients of UK sourced plasma-derived coagulation factor concentrates used in the period 19802001 should be regarded as being at risk of developing variant Creutzfeldt-Jakob disease (vCJD) for public health purposes.21 Risk assessments have been carried by both the DoH and the World Federation of Haemophilia which could not identify any person with haemophilia who has developed vCJD.22,23 Moreover, they concluded that routine dental treatment including minor oral surgery is unlikely to pose a cross-infection risk.
Orthodontic considerations in patients with bleeding disorders
Orthodontic treatment is not contraindicated in patients with bleeding disorders.24 A thorough history and close liaison with the patients haematologist, oncologist or physician will help reduce the risk of problems occurring.
N N
Patients should be encouraged to maintain excellent, atraumatic oral hygiene.25 If extractions or surgery cannot be avoided, the management of patients with haemophilia relies on careful surgical technique, including an attempt at primary wound closure and the following regimen to: # increase Factor VIII production with 1-desamino-8-Darginine vasopressin (DDAVP) # replace missing Factor VIII with cryoprecipitate, Factor VIII, fresh frozen plasma or purified forms of Factor VIII # antifibrinolytic therapy with transexamic acid or epsilonamino caproic acid (EACA)25
N N N N N
Nerve-block anaesthetic injections are contra-indicated unless there is no better alternative and prophylaxis is provided to prevent the risk of a haematoma forming.26 Chronic irritation from orthodontic appliances should be avoided. Fixed appliances are preferable to removable appliances as the latter can cause gingival irritation.27 Self-ligating brackets are preferable to conventional brackets. If conventional brackets are used, archwires should be secured with elastomeric modules instead of wire ligatures.27 Care is required when placing and removing archwires.1 The duration of orthodontic treatment should be kept to a minimum to reduce the potential for complications.28
their movement through capillaries and hence deprives the tissues of oxygen and in conscious patients causes intense pain. The disease is chronic and life expectancy is shortened to about 45 years.29 Sickle cell trait is the term given to patients who inherit one of the genes of sickle cell disease but without developing the recurrent symptoms. It is not benign and can also have symptoms due to co-morbidity and conditions that can lead to overheating, dehydration and sickling. Sickle cell anaemia is more common in people of African origin where malaria is common but it also occurs in people of Asian and West Indian descent.30 Treatment ranges from NSAIDs for milder vasoocclusive crises to IV opioids.31 Acute chest crises are treated with antibiotics and blood transfusions to reduce the percentage of HbS in the blood. The risks of blood transfusions have been discussed above. Tetracycline may need to be given as an alternative to amoxicillin or ucloxacillin when the child develops multiple drug sensitivity. Chemotherapy32 and bone marrow transplants have also been advocated and these treatments come with their own list of orthodontic considerations. Oral manifestations of sickle cell disease include enamel hypoplasia in the form of white spots on the tooth surface, dentinal hypomineralization, delayed tooth eruption, pale lips and oral mucosa and glossitis. Radiographic signs include osteoporosis and parallel trabeculae amidst teeth but not in edentulous areas.33 Mandibular osteomyelitis in the absence of other problems can occur due to the limited blood supply. Vaso-occlusive crises can predispose the patient to pain and paraesthesia of the inferior alveolar nerve and the lower lip.
Orthodontic considerations in patients with sickle cell anaemia
N N N
Orthodontic treatment is not contra-indicated in sickle cell patients, provided the patient has no or very mild complications and the oral hygiene is excellent. Intervention in these patients favours a multidisciplinary approach involving the patients physician, haematologist, dentist, and family. Emotional stress should be avoided and care should be taken to ensure the surgery is well ventilated and at an ambient temperature.34
Sickle cell anaemia
This is a genetic disorder that is characterized by a haemoglobin gene mutation (HbS as opposed to HbA). Deoxygenation, for example during anaesthesia induces the red cells to deform into a sickle shape. This restricts
A non-extraction approach to treatment is preferred. If extractions are necessary they are best carried out in a hospital environment.34
JO December 2009
Clinical Section
Medical disorders and orthodontics
Orthodontic considerations in patients with sickle cell anaemia
General anaesthetics for elective procedures are contraindicated and hence orthognathic surgery should not be recommended. If a GA in a sickle cell trait patient cannot be avoided careful oxygenation must be ensured. Patients with sickle cell disease itself may require a pre-anaesthetic transfusion so the level of haemoglobin A is at least 50%.35
The orthodontist should be aware of possible pulpal necrosis involving healthy teeth, the changes in bone turnover, mandibular vaso-occlusive crises, and the greater susceptibility to infections.34
It has been recommended that orthodontic forces should be reduced and rest intervals between activations should be increased to restore the regional microcirculation.34
capacity to improve the height velocity.36 Bone density is frequently reduced in long-term survivors of childhood malignancies.37 They also show acute and longterm complications in the oral cavity and in dental and craniofacial development. The most common dental disturbances are arrested root development with Vshaped roots, premature apical closure, microdontia, enamel disturbances and aplasia.38 A common side effect of radiation is salivary dysfunction leading to xerostomia. Craniofacial disturbances were demonstrated by a case controlled study of 17 children treated for ALL with allogeneic BMT and TBI. The ALL group had reduced vertical dimensions of the face, alveolar processes as well as reduced sagittal dimensions of the jaws, characterized by mandibular retrognathism.39
Leukaemia
Leukaemia is divided into acute and chronic forms. Acute lymphoblastic leukaemia (ALL) is the commonest presentation in children accounting for 25% of all childhood tumours. The prognosis in children with ALL is better than that for adults for whom the longterm survival is low. Acute myeloblastic leukaemia (AML) is more common in adults than children and the prognosis is poor. The treatment for acute leukaemia includes chemotherapy or bone marrow transplantation (BMT). Total body irradiation (TBI) and immunosuppression are used to prevent graft-versus-host disease after BMT. Chronic leukaemia involves the proliferation of more mature cells than those found in acute leukaemia. The prognosis is better and adults are more commonly affected than children. Chronic lymphocytic leukaemia (CLL) is more common and patients tend to be asymptomatic. Chronic myeloid leukaemia (CML) affects adults of a younger age group than CLL. The main signs of the chronic leukaemia tend to be splenomegaly and lymph node enlargement. Treatment is with chemotherapy and radiotherapy. The sequelae of treatment may be immediate or may occur several months after treatment. These effects can be caused by the malignancy itself, by the treatment including chemotherapy, radiotherapy and supportive care such as transfusions, antibiotics and immunosuppressive treatment. The degree to which an individual is affected is related to the age at which the disease is diagnosed and treated and the type and intensity of the treatment. The growth rate generally declines in children during treatment for leukaemia. Soon after treatment the normal growth rate is resumed and catch up growth is sometimes seen. Growth hormone therapy has the
Orthodontic considerations in patients with leukaemia Dahlof and Huggare have produced an excellent review on the risk factors to be aware of when planning orthodontic treatment in longterm survivors of childhood malignancy.40 Before diagnosis
Significant orofacial complications of leukaemia in children
include lymphadenopathy, spontaneous gingival bleeding caused by thrombocytopenia (reduction in platelets), labial and lingual ecchymoses and mucosal petechiae, ulceration, gingival swelling, and infections. The orthodontist may be the first to notice signs of the illness.41 Patients presenting with spontaneous bleeding in the presence of good oral hygiene warrant an immediate referral to a physician.2 After diagnosis
Orthodontic treatment should be postponed if the patient
requires chemotherapy as the drugs can exacerbate the thrombocytopenia and agranulocytosis. After treatment
It has been suggested that orthodontic treatment should be postponed until at least 2 years after BMT.2 By then the risk for relapse of the malignancy has diminished and the patient is no longer on immunosuppressive therapy. Additionally, the growth rate and the need for supplemental growth hormone have been assessed.
N N
In view of the fact that TBI can suppress growth, the prognosis for growth modification in skeletal Class II malocclusions is guarded.40 The treatment should be modified to reflect the patients medical condition and planned with the patients best interests in mind. There are no reports about any adverse effects of orthodontic treatment in these patients.42 Treatment mechanics should be aimed at minimising the risk of root resorption, keeping the forces low and accepting a compromised treatment result. There may be merit in treating the upper jaw only to reduce the risk of undesirable events.40
Patel et al.
Clinical Section
JO December 2009
Orthodontic considerations in patients with leukaemia
In patients with short blunt roots, it is wise to monitor the crown to root length after 6 months of fixed appliance treatment. If there is evidence of apical root resorption, treatment should be interrupted for 3 months. The appliance should not be removed but the archwire should be left passive so there can be no active tooth movement.43
asthma.46 This increased prevalence of resorption was conned to mild root blunting and the researchers concluded that longevity or function of posterior teeth would not be adversely affected. Nonetheless patients should be informed of this risk prior to treatment.
Cystic fibrosis
Cystic brosis (CF) is the most common life limiting, childhood-onset, autosomal recessive disorder among people of European heritage. It affects the exocrine glands of the lungs, liver, pancreas and intestines, causing progressive disability due to multisystem failure. The cells are relatively impermeable to chloride ions and thus salt rich secretions are produced. The mucous is viscid and blocks glands of the respiratory and digestive systems. There is a non-productive cough that leads to acute respiratory infection, bronchopneumonia, bronchiectasis, and pancreatic insufciency. Diabetes mellitus may be a complication and patients may have cirrhosis of the liver.47,48 There is no cure for CF. Most individuals with CF die young: many in their 20s and 30s from lung failure; however, with advances in medical treatments, the life expectancy of a person with CF is increasing to ages as high as 40 or 50.49 Heart and lung transplantation are often necessary as CF worsens. Oral effects include hypoplastic enamel and delayed eruption. In the 1970s there were several reports of tetracycline staining of teeth but alternative medications are now used.50 A side effect of antibiotic treatment is the lower prevalence of dental disease.51
Tooth extractions have been implicated in causing osteoradionecrosis (ORN) with a higher incidence in the mandible. There are no reports on the incidence of ORN after tooth extractions in children treated for malignancies. Atraumatic extraction techniques will also reduce the risk of ORN.44
The caries risk may be increased due to salivary dysfunction and as with all patients the oral hygiene should be of a high standard. Topical fluoride application and artificial saliva may be recommended.
A further side effect of anti-cancer treatment is a reduced resistance to infections and atrophy of the oral mucosa. Even minor irritation from orthodontic appliances can lead to severe ulceration. Vacuum formed aligners may be the appliances of choice for selected malocclusions.
If a patient requires additional chemotherapy or radiotherapy, appliances should be removed to reduce the risk for oral complications. Treatment can be recommenced when the patient is in remission with a good prognosis.27 Both the patient and parent should be counselled that this regime is being followed in the best interest of the patient.2
Removable retainers should fit well with little potential to be a source of irritation, ulceration or infection.2
Respiratory system
Respiratory disorders are common and the use of intravenous (IV) sedation and general anaesthesia (GA) for elective procedures may be contraindicated. The unwanted effects of prescribed drugs can also inuence the orthodontic treatment of these patients.
Relevance of drugs in respiratory disorders
The chronic use of corticosteroid inhalers can lead to localized lowered resistance to opportunistic infections. As a result of this oro-pharyngeal candidal infection may occur.52 To avoid this complication, patients should be advised to rinse and gargle with water after the use of their inhaler especially if wearing removable acrylic appliances.53 Candidiasis can be treated with topical antifungal agents such as nyastatin. Additionally the regular use of inhaled corticosteroids can predispose the patient to an adrenal crisis if subjected to stress. The need for steroid cover is discussed in the general section on drugs and orthodontic treatment. Beta-adrenergic agonist bronchodilators such as salbutamol, antimuscarinic bronchodilators, cromoglycates and antihistamines can all produce dry mouth, taste alteration and discolouration of teeth.
Asthma
Approximately 300 million people around the world have asthma, and it has become more common in both children and adults globally in recent years.45 The severity varies from mild to severe. In moderate cases episodes are severe but the patients are symptom free between attacks. In severe asthma the attacks are severe and the child is never asymptomatic and growth and lung function can be affected. There has been a tentative link between orthodontically induced external root resorption and patients with
JO December 2009
Clinical Section
Medical disorders and orthodontics
Orthodontic considerations in patients with respiratory disorders
The patients physician should be contacted before treatment is commenced to evaluate the severity and prognosis of the problem.27 The orthodontist should ensure the patient has their inhaler nearby.1
N N
Patients may not be comfortable in the supine position if they have difficulty breathing.53 The first objective is to prevent acute asthmatic attacks. Treatment can be deferred in patients with poorly controlled asthma and with a history of multiple emergency room visits. It is best to minimize the factors that precipitate attacks in patients at low or moderate risk. Morning appointments when the patient is rested, short waiting and treatment times all help ease stress and anxiety.1
Orthodontic extractions should ideally be carried out under local anaesthesia (LA) with or without relative analgesia (RA) and not GA. If GA is required the patient must be in optimal health with no evidence of a respiratory infection.53 RA with nitrous oxide and oxygen is favoured to intravenous sedation (IV) since the former can be rapidly reversed.53
CF also affects the salivary glands and hence salivary flow can be reduced. These patients, as well as those with drug-induced xerostomia are at a higher risk of decalcification. Aggressive oral hygiene, supplemental topical fluorides, and vigilance for dental disease are necessary to combat these side effects.28
Patients with asthma should be prescribed non-steroidal antiinflammatory drugs (NSAIDs) with caution as many asthmatic patients are allergic to aspirin like compounds. A retrospective, cohort study identified that patients younger than 40 years with a history of multiple respiratory reactions and prior reactions associated with aspirin and NSAIDs were more likely to have a positive oral aspirin challenge.54
The risk of developing epilepsy is 25% over a lifetime. The prevalence of active epilepsy is between 5 and 10 people per 1000 of the population.59 The condition is more common in men and the incidence is high in the rst two decades of life, and then reduces before increasing after the age of 50 years as a result of cerebrovascular disease.56 Hyperventilation, fever, photic stimulation, withdrawal or poor lack of compliance with anticonvulsants, lack of sleep, over-sedation, emotional upset and some medications such as antihistamines can stimulate attacks. Both the condition and the medical management can affect oral health. Phenytoin was once the rst choice in managing epilepsy in younger people but this has fallen out of favour because of its many side effects. These include nausea, mental confusion, acne, hirsutism, hepatitis, erythema multiforme and gingival overgrowth. However, the orthodontist may still encounter patients taking phenytoin. Alternatives such as carbamazepine also have oral side effects including oral ulceration, xerostomia, glossitis and stomatitis.56 Prevention of oral disease and carefully planned dental and orthodontic treatment are essential to the well being of patients with epilepsy. Other forms of treatment for epilepsy such as surgery are unlikely to have implications for orthodontic care.
Orthodontic considerations in patients with epilepsy
Most people who have seizure disorders are able to undergo conventional orthodontic care in the primary care setting. Nonetheless, the orthodontist should ensure the patient has taken their normal anti-epileptic medication, is not too tired and has eaten normally before each appointment.
Neurological disorders
It is important that orthodontists have knowledge of the most common neurological conditions as some problems may manifest initially in the orthodontic chair.55
N N N
The orthodontist should ensure the patient is receiving regular and rigorous preventative dental care to avoid/minimize dental disease. Patients should be aware of and consented for the risk of soft tissue and dental injuries as a result of a seizure.60 Gingival overgrowth associated with phenytoin is the most widely known complication of anti-epileptic medication, with 50% of individuals being affected within 3 months of starting the drug.61 Gingival hyperplasia is greater in those with high plaque scores but there is also a genetic link.62 Gingivectomy is recommended to remove any hyperplastic tissue that interferes with appearance or function. For patients with recurrent hyperplasia, the patients physician should be contacted to discuss alternative medication. Gingival hyperplasia resolves spontaneously within 16 months of phenytoin withdrawal.63
Epilepsy
Epilepsy is a common symptom of an underlying neurological disorder. The seizures can take a variety of forms and epilepsy is considered to be active if a person has had a seizure within the last 2 years or is taking anti-epileptic medication.56 Brain damage due to injury, infection, birth trauma or a cerebrovascular accident accounts for 25% of cases. The other 75% of cases have no identiable cause but there is a familial trend. Epilepsy can develop in some genetic syndromes such as Downs syndrome57 or in Sturge-Weber syndrome.58
Patel et al.
Clinical Section
JO December 2009
Orthodontic considerations in patients with epilepsy
Removable appliances need to be used with caution as they can be dislodged during a seizure. It is not always possible to avoid the use of removable appliances. Wherever possible removable appliances should be designed for maximum retention and made of high impact acrylic.56 Trauma can also result in subluxation of the temporomandibular joints and tooth devitalization, fractures, subluxation or avulsion.
If an individual with a Class II division 1 incisor relationship experiences an aura before a seizure, he or she should carry a soft mouth guard with palatal coverage and extending into the buccal sulci, to use at such times.56
The orthodontic team should be well trained in seizure management. Status epilepticus is a medical emergency and there should be given a benzodiazepine from the emergency drug kit.56
Multiple sclerosis (MS)
MS is a complex neurological condition that occurs as a result of damage to the myelin sheathes within the central nervous system. The damaged areas result in inammation and interference in both sensory and motor nerve transmission. MS is the most common cause of severe disability among young adults in the UK. It has an incidence of 0.1% (1 : 1000) in the general population.64 The diagnosis of MS is usually made between the ages of 20 and 40 years. It is more common in women than men with a ratio of 3 : 2.65 The prognosis depends on the subtype of the disease. The life expectancy of patients is nearly the same as that of the unaffected population, and in some cases a near-normal life is possible.
Subtypes of MS Benign 20% of people with MS. Mild attacks followed by complete recovery and no permanent disability Relapsing/remitting 25% of confirmed cases. Remissions occur spontaneously, relapses unpredictable, some residual damage Secondary progressive 40% of cases. Follows on from relapsing/remitting phase and then remissions cease to occur. Usually 1520 years from onset of symptoms Primary progressive 15%. Symptoms worsen and disability progresses.
have been implicated. It is not an inherited condition but there is a familial link. The main symptoms relevant to oral care include pain and numbness of varying severity in the facial and oral tissues. The arms and hands can also be affected challenging the patients ability to carry out effective oral hygiene. Trigeminal neuralgia is atypical in that patients are younger, the pain may be bilateral and unstimulated. Indeed trigeminal neuralgia in people under 40 can be indicative of MS. Orthodontists should be aware of this and refer affected individuals for a neurological assessment. Transient spasticity occurs when opposing muscles contract or relax at the same time leading to muscle stiffness, lack of coordination, clumsiness, muscle spasm and related pain. This can interfere with the safe delivery of orthodontic treatment and treatment should be delivered until the individual is in remission. Some patients also suffer from a tremor making satisfactory oral hygiene problematic. There is no cure for MS. The focus of treatment is on the prevention of disability and maintenance of quality of life. Drugs, physical treatments and psychological techniques are used. Steroids are often used to help a person over a severe relapse. A plethora of other drugs can be prescribed, several of which can cause dry mouth, ulceration, gingival hyperplasia amongst other symptoms.66
Orthodontic considerations in patients with MS
N N
Treatment should involve a multidisciplinary approach including the patients physician, neurologist, MS specialist nurse and care worker.67 Preventative regimes should be based on the nature of the individuals MS. Custom made toothbrush handles to improve grip and the use of electric toothbrushes to compensate for the loss of manual dexterity and coordination have been recommended.67
It is important to discuss with every patient with MS how he or she prefers to manage his or her symptoms. Appointments should be at their convenience, the environment kept at a comfortable temperature. Patients with spasms should be allowed to get out of the dental chair and move around to relieve them. Individuals with dysphagia should be treated in a semi-reclined position.
Treatment objectives should be tailored to the patients condition. Patients with severe MS may be best treated to a compromised result. Removable appliances may not be tolerated well. In patients with poor coordination the use of intermaxillary traction may be contraindicated.
The aetiology of MS is not understood and various environmental factors such as viruses, climatic factors
JO December 2009
Clinical Section
Medical disorders and orthodontics
Liver disease
Liver disease can result from acute or chronic damage to the liver, usually caused by infection, injury, exposure to drugs or toxic compounds, an autoimmune process, or by a genetic defect. For most childhood liver diseases the cause is unknown. The main effects of liver disease can be categorized into:
Orthodontic considerations in patients with liver disease Hepatitis
All patients should be treated as though they are infected and universal cross-infection control precautions should be taken. Several studies have shown that orthodontists are more complacent than general dental practitioners with regard to cross-infection.70
All members of the team should be immunized against HBV. A booster is required in those with anti-HBs level less than 100.69
N N N N N
coagulation disorders; drug toxicity; disorders of fluid and electrolyte balance; problems with drug therapy; infections.35
Endocrine conditions
Diabetes mellitus (DM)
Infections
Viral hepatitis is undoubtedly of importance to the orthodontist. Hepatitis B (HBV), hepatitis C (HCV) and hepatitis D are blood borne and can be transmitted via contaminated sharps and droplet infection. Aerosols generated by dental hand pieces could infect skin, oral mucous membrane, eyes or respiratory passages of dental personnel and patients. The main orthodontic procedures to result in aerosol generation are removal of enamel during interproximal stripping, removal of residual cement after debonding, and prophylaxis.68 HBV has an incubation period of 6 weeks to 6 months and a small number of infected persons can progress to the carrier state associated with chronic active hepatitis and eventually cirrhosis. Hepatitis B Surface Antigen (HBsAg) is the rst sign of infection. Antibody to HBsAg is associated with protection from infection. Hepatitis B Core Antigen (HBcAg) is detected by the development of an antibody to it. If the person is HBsAg negative but HBcAg positive they are infective. Hepatitis B e Antigen is only found if HBsAg is present and is an indication of infectivity.
Orthodontic considerations in patients with liver disease General liver disease
N N
Care should be taken when prescribing any medication for patients with liver disease. Hepatic impairment can lead to failure of metabolism of some drugs and result in toxicity.69 Patients undergoing liver transplantation will be receiving immunosuppressive drugs that can cause gingival hyperplasia. This effect is discussed in more detail on the section on medication.
Haemostasis will be affected and this should be accounted for when planning treatment.
The term DM is characterized by chronic hyperglycaemia. There are two main categories of DM: Type 1 DM, (insulin dependent, IDDM or juvenileonset diabetes) results from defects in insulin secretion. The onset is usually before adulthood and accounts for approximately 515% of all people with DM. Type 1 DM occurs more frequently in people of European origin than non-European origin. It is life threatening if not treated with exogenous insulin. Type 2 DM (non-insulin dependent NIDDM or mature-onset diabetes) develops as a result of defects in insulin secretion, insulin action or both. There is a link with being overweight. Type 2 DM usually appears in people over the age of 40, although in South Asian and African-Caribbean people often appears after the age of 25.71 However, recently, more children are being diagnosed with the condition, some as young as seven.72 This form of DM is also more prevalent in less afuent populations. It accounts for 8595% of all cases of DM. It is not usually life threatening but chronic complications can affect the quality of life and reduce life expectancy. Gestational diabetes is similar to type 2 DM in that it involves insulin resistance; the hormones of pregnancy can cause insulin resistance in women genetically predisposed to developing this condition. Gestational diabetes typically resolves with delivery of the child, however types 1 and 2 diabetes are chronic conditions. The prevalence of DM is increasing in the UK and worldwide. The World Health Organisation predicts that the global prevalence of type 2 DM will increase from 135 million in 1995 to 300 million in 2025.73 DM is progressive and has potentially harmful consequences for health. Strict blood glucose control, lowering of blood pressure, together with a healthy lifestyle improves well being and protects against long
10
Patel et al.
Clinical Section
JO December 2009
term damage to the eyes, kidneys, nerves, heart and major arteries.74 Oral complications include: xerostomia, burning mouth and/or tongue, candidal infection, altered taste, progressive periodontal disease, dental caries, acetone breath, oral neuropathies, parotid enlargement, sialosis and delayed wound healing. These complications can occur even when the blood glucose is well controlled due to impaired neutrophil function but are all more severe in uncontrolled DM.
Orthodontic considerations in patients with DM
Orthodontic treatment should be avoided in patients with poorly controlled DM as they are more likely to suffer from periodontal breakdown.27 Well-controlled DM is not a contraindication for orthodontic treatment.
N N
Rigorous preventative regimes should be put in place. The patient should be made aware of the consequences of poor oral hygiene and the increased risk of periodontal disease. Early morning appointments are least likely to interfere with the diabetes control regime. Patients should be advised to eat a usual meal and take the medication as usual prior to longer appointments.
Diabetic related microangiopathy can affect the peripheral vascular supply, resulting in unexplained toothache, tenderness to percussion and even loss of vitality.75 It has been suggested that patients with DM should be treatment planned as periodontal patients. Light physiological forces should be used in all patients to avoid overloading the teeth.
in medical care resulting in reduced morbidity and mortality.76 The most common renal condition to present to the orthodontist is chronic renal failure (CRF). CRF occurs after progressive renal damage. The symptoms and signs vary and can affect diverse body systems. Bone disease or renal osteodystrophy is an almost universal feature of CRF. Calcium metabolism is compromised by an elevated parathyroid hormone and by disruption in vitamin D metabolism. This results in secondary hyperparathyroidism. Renal disease also causes anaemia and marrow brosis leads to a reduced platelet count and poor platelet function. Haemostasis is impaired to varying degrees in patients with CRF. Initially treatment is conservative with dietary restriction of sodium, potassium and protein. As the disease progresses dialysis or transplantation are required. Many patients are prescribed steroids to either combat renal disease or to avoid transplant rejection. Immunosuppressant drugs such as cyclosporine and calcium channel antagonists such as nifedipine are also taken to prevent transplant rejection. Immunosuppressants predispose the patients to infections. These drugs can also cause drug induced gingival overgrowth as discussed in the section on drugs and orthodontic treatment. In children CRF leads to decreased growth and sometimes delayed eruption and enamel hypoplasia.
The orthodontic team should be trained to deal with diabetic Orthodontic considerations in patients with renal disorders
emergencies. Hypoglycaemia is characterized by initial signs of tremor, nausea, sweating, anxiety, tachycardia, palpitations, shivering. The patient may complain of visual disturbance and/ or perioral tingling. If these warning signs are not recognized, a second group of neuroglycopenic symptoms occur. These include impaired concentration or confusion, irrational or aggressive behaviour, slurred speech, and drowsiness progressing to coma if untreated. Treatment in the orthodontic surgery75
N N
Orthodontic treatment is not contraindicated in patients if the disease is well controlled. Treatment could be deferred if the renal failure is advanced and dialysis is imminent. If possible treatment could be carried out prior to transplantation to avoid the risks associated with immunosuppressant drugs.
N N N
Conscious 50 g of glucose as a drink, tablet or gel Unconscious 20 ml of 50% Dextrose IV or 1 mg of glucagon should be administered intramuscularly. When the patient is cooperative oral glucose should be given to prevent recurrent hypoglycaemia. If recovery is delayed, the emergency services should be called.
Appointments should be scheduled on non-dialysis days. The day after dialysis is the optimum time for treatment for surgical procedures as platelet function will be optimal and the effect of heparin will have worn off.
Surgical procedures are best carried out under local anaesthetic. The anaemia and the potential electrolyte disturbances that can predispose the patient to cardiac arrhythmias can complicate general anaesthesia.
Renal disorders
Patients with kidney disorders are presenting more frequently in orthodontic practice due to improvements
Haemostasis is impaired as a result of platelet dysfunction
Impaired drug excretion leads to the need for care with drug prescriptions.
JO December 2009
Clinical Section
Medical disorders and orthodontics
11
Orthodontic considerations in patients with renal disorders
The value of prophylactic antibiotics in renal transplant patients on prevention of post-operative complications is questionable or unproven, with the Working Party of the British Society for Antimicrobial Chemotherapy (BSAC) stating that there is no need for antibiotic prophylaxis for dental treatment;77 however the decision to give prophylaxis should be made on an individual basis, in conjunction with the patients renal physician.78
These patients may be taking or have taken steroids but the use of supplemental steroids in dentistry is controversial and is discussed below in the section on drugs and orthodontic treatment.
Animal models have also shown that orthodontic tooth movement is accelerated in rats with renal insufficiency.79 This was attributed to the increase in circulating parathyroid hormone. It has been suggested that orthodontic treatment forces should be reduced and the forces re-adjusted at shorter intervals.79
Musculoskeletal system
Juvenile idiopathic arthritis
resulting in mandibular retrognathism. JIA patients commonly present with skeletal Class II and open bite malocclusions.85 Mandibular asymmetry is seen in cases with unilateral TMJ involvement. Early orthodontic intervention facilitates both the skeletal and the occlusal rehabilitation. The prevalence of dental caries and periodontal disease is higher in adolescents with JIA cases. This has been credited to a combination of factors including difculties in executing good oral hygiene, unfavourable dietary practices and side effects from the long-term administration of medication.86 There are common human leucocyte antigen associations between periodontal disease and JIA which explains their similar inammatory effects. Treatment is aimed at controlling the clinical manifestations by suppressing the articular inammation and pain, preserving joint mobility and preventing deformity. NSAIDs are used in the early stages. More severe cases are prescribed a variety of medicaments such as gold, methotrexate, corticosteroids and antimalarial drugs. These drugs have their own adverse effects which must be reected on during orthodontic treatment planning.
Orthodontic considerations in patients with JIA
Juvenile idiopathic arthritis (JIA) is a severe disease of childhood. It comprises a diverse group of distinct clinical entities of unclear aetiology. JIA is more common in Norway and Australia than in other countries. In Norway, the prevalence is 148.1 cases per 100,000 population and the incidence is 22.6 cases per 100,000 population.80 A cross sectional, community based, point prevalence study reported a prevalence of 4.0 per 1000 in 12-year-old children in urban Australia.81 JIA is classied according to the type of onset of the disease and the number of joints affected during the rst 46 months: pauciarthritis or oligoarthritis denotes four or less joints being involved and polyarthritis when ve or more joints are involved. JIA can be of varying severity with localized and/or systemic complications, including functional impairment of the affected joints. This may result in disturbances in growth and developmental anomalies. There is remission of the disease in adolescence, which happens for 70% of patients.82 The temporomandibular joint (TMJ) is affected in 45% of cases with JIA.83 The diagnosis of TMJ involvement is more difcult than the other joints as the signs and symptoms are missing or weak.84 Hence patients are most often seen when extensive changes have occurred. This can lead to the development of condylar hypoplasia, restricting mandibular growth
The main aim is to allow the child to live as normal life as possible. The functional ability of the TMJ in JIA children should be monitored closely in order to start medical treatment as soon as inflammation begins in the joint. The TMJ in a growing child has immense potential for structural changes and growth can normalize, provided the inflammation is controlled early and mandibular growth is supported.87 There is remission of the disease in adolescence for 70% of patients.88 There are no controlled human studies studying the efficacy of steroid injections on reducing the inflammatory activity in the TMJ; however, a study on rabbits with antigen induced TMJ arthritis did not show any positive long-term benefit of intra-articular steroid injections.89
N N
Oral hygiene aids including modified toothbrush handles and electrical toothbrushes can be recommended to patients with JIA.90 A bite splint can be provided to unload the joint during any acute periods of inflammation. A distracted splint has also been suggested to modify mandibular growth in the same way as conventional functional appliances.87 The use of functional appliances in patients is a controversial area. It has been argued that functional appliances and class II elastics put increased stress on the TMJs and should be avoided;91 however, it has also been suggested that functional appliances protect the joints by relieving the affected TMJ, the aim being to move the mandible into the normal anterior growth rotational pattern thus correcting the skeletal Class II relationship.92
12
Patel et al.
Clinical Section
JO December 2009
Orthodontic considerations in patients with JIA
Surgery can be considered if the problem cannot be treated orthodontically; however, it has been suggested that mandibular surgery should be avoided and instead a patient with severe mandibular deficiency should have maxillary surgery and a genioplasty.28
Osteoporosis
Osteoporosis is a common progressive metabolic bone disease that decreases bone density and deterioration of bone structure. Osteoporosis can develop as a primary disorder or secondarily due to some other factor. It is most common in women after menopause, but may develop in men. Risk factors that cannot be altered include advanced age, being female, oestrogen deciency after menopause,93 and being of European or Asian origin.94 Potentially modiable risk factors include excessive alcohol intake, vitamin D deciency, smoking,95 low body mass index,96 malnutrition, physical inactivity97 Osteoporotic bone loss affects cortical and cancellous (trabecular) bone and animal studies have shown this process can result in decreased oral bone density and alveolar bone loss.98 Both bone resorption and formation are accelerated and excessive bone resorption leads to loss of attachment. This theoretically can affect the rate of tooth movement. Treatment modalities include medication, exercise, a diet sufcient in calcium and vitamin D and lifestyle changes99 In conrmed osteoporosis, bisphoshonate (BP) drugs are the rst-line of treatment in women. Oral BPs are poorly tolerated and are associated with oesophagitis. The chronic nature of osteoporosis necessitates long-term administration of BPs and therefore their safety is clinically important and requires some attention. A recent review of the literature identied 26 cases of osteonecrosis of the jaws (ONJ) in patients on oral BPs for the treatment of osteoarthritis.100 This prevalence is relatively low compared with the 190 million patients with osteoarthritis and osteopenia on oral bisphosphonates.101 The main implications on orthodontic treatment are due to BP use and hence these are discussed in the section below.
pain relievers for a chronic illness. The effects of these medications on tooth movement have been studied. Prostaglandins are important mediators in tooth movement and it has been suggested that the use of over-the-counter NSAIDs can affect the efciency of tooth movement. A study to determine the effect of aspirin, acetaminophen (paracetamol) and ibuprofen on orthodontic tooth movement in rats showed acetaminophen did not affect movement whereas there was a signicant difference between the control group and the aspirin and ibuprofen group. The authors suggest paracetamol may be the analgesic of choice in orthodontic patients.102 Their results suggested that NSAIDs reduce the number of osteoblasts by inhibiting prostaglandin synthesis. This led to the use of cyclooxygenase2 inhibitors (COX-2) drugs, but the effects of these drugs on tooth movement can be very variable. The effects of three different COX-2 inhibitors on tooth movement in Wistar male rats showed that tooth movement was inhibited in rats treated with Rofecoxib. There was, however no signicant difference in tooth movement between the control group (saline) and the other two COX-2 inhibitor groups; Celecoxib and Parecoxib.103 Fortunately rofecoxib is now withdrawn from the market due to its cardiotoxicity. Orthodontists should be aware that products from the same class of drugs may have varying effects on orthodontic tooth movement.
Corticosteroids
These drugs are used for many inammatory and autoimmune diseases. There are two main issues to consider when patients present with a history of corticosteroid use. Firstly, the use of supplemental steroids prior to dental surgery in patients at risk of an adrenal crisis is a contentious issue. The theoretical basis to this practice is that exogenous steroids suppress adrenal function to an extent that insufcient levels of cortisol can be produced in response to stress, posing the risk of acute adrenal crisis with hypotension and collapse. The UK MHRA (Medicines and Healthcare Products Regulatory Agency) and CSM (Committee of Safety of Medicines) together published recommendations in which appear not yet to have been superseded, that include Patients who encounter stresses such as trauma, surgery or infection and who are at risk of adrenal insufciency should receive systemic corticosteroid cover during these periods. This includes patients who have nished a course of systemic corticosteroids of less than 3 weeks duration in the week prior to the stress. Patients on systemic corticosteroid therapy who are at risk of adrenal suppression and are unable to take
Side effects of medication
Non-steroidal anti-inflammatory drugs (NSAIDs)
Pain control during orthodontics is an important aspect of patient compliance. In addition patients may be on
JO December 2009
Clinical Section
Medical disorders and orthodontics
13
tablets by mouth should receive parenteral corticosteroid cover during these periods.104 In contrast various authors have suggested modied guidelines for the management of patients on steroid medications.105 These authors reported on a number of studies conrming the low likelihood of signicant adrenal insufciency even following major surgical procedures. Patients on long-term steroid medication do not require supplementary steroid cover for routine dentistry, including minor surgical procedures, under LA. Instead the blood pressure should be monitored throughout the procedure with IV hydrocortisone available in the event of a crisis.106 Patients undergoing GA for surgical procedures may require supplementary steroids dependent upon the dose of steroid, duration of treatment and severity of the planned surgery.105 The second factor to be aware of is that glucocorticoid therapy is known to affect bone turnover. Kalia and coworkers studied the effect of acute and chronic corticosteroid treatment in rats.107 Their results indicate that bone turnover is reduced in subjects on acute corticosteroid treatment and increased in patients on chronic corticosteroid therapy. The authors postulated that it may be wise to postpone orthodontic treatment on patients on acute doses. They also suggested that orthodontic forces should be reduced and checked more frequently in patients on chronic steroid treatment.
The risk of side effects is greater if the dose is administered intravenously and on a long-term basis.109 Symptoms and signs of ONJ may include pain, swelling, pus formation, paraesthesia, ulceration of soft tissue, intra-oral or extra-oral sinus tracts, loose teeth and exposed bone.110 The pathogenesis of BP associated ONJ is not fully known. One suggestion is that hypodynamic and hypovascular bone is unable to meet an increased demand for repair and remodelling due to physiological stress (mastication), iatrogenic trauma (tooth extraction) or due to odontogenic infection. This can be exacerbated by the following factors:
N N N N N N N N N
corticosteroid treatment; chemotherapy; medical co-morbidities such as diabetes mellitus; the presence of dental disease;111 dental extractions; oral bone surgery; poorly fitted dental appliances; smoking; alcohol abuse.
Radiographic signs include widening of the periodontal ligament space at the molar furcation areas and mottled bone consistent with osteolysis.111
Orthodontic considerations in patients taking BPs
Bisphosphonates (BPs)
These drugs are commonly prescribed to manage osteopenia and osteoporosis or to treat hypercalcaemia caused by bone metastasis in cancer patients (see Table 2). About half of the BP that is resorbed is excreted unchanged by the kidneys; the remainder has a high afnity for bony tissues and a reported half-life of 10 years. BPs inhibit the resorption of trabecular bone by osteoclasts and hence preserve bone density. Although their medical benets have been proven, there are increasing numbers of side effects that can affect orthodontic treatment including delayed tooth eruption, inhibited tooth movement,108 impaired bone healing, and BP-induced osteoradionecrosis (ONJ) of the jaws.
Table 2
N N
Amend the medical history form to identify patients who are taking BPs.112 Orthodontic treatment can only be considered after discussion with the patients physician and other medical specialists they may be under the care of. Ascertain why the patient is on BPs. Assess the risk of osteoradionecrosis via the route of administration, duration of treatment, dose and frequency of use.113
N N
If possible treatment should be carried out prior to BP treatment. In patients at high risk of ONJ, it may be better to accept the malocclusion and consider the benefits of cosmetic dentistry.114
Commonly prescribed bisphosponates, brand names and dosage. Common third generation bisphosphonates Alendronate (Fosamax, Merck) Risedronate (Actonel, Aventis) Ibandronate (Boniva, Roche) Pamidronate (Aredia, Novartis) Zoledronate (Zometa, Novartis) Dosage 70 mg per week 35 mg per week 2.5 mg per day 90 mg per month 4 mg per month
Mode of administration Oral bisphosphonates osteoporosis, Pagets disease, osteogenesis imperfecta IV bisphosphonates cancer
14
Patel et al.
Clinical Section
JO December 2009
Orthodontic considerations in patients taking BPs Discontinuing the drug prior to treatment may not be effective because of its long half life (risedronate, 480 h; alendronate, 10 years z; pamidronate, 300 days; zoledronate, 146 h).115
Orthodontic considerations in patients with DIGO
Patients at risk of DIGO require a team approach with the patient, his or her physician, GDP, periodontist, hygienist and the orthodontist.76 Early liaison with the patients physician is recommended to investigate whether an alternative drug can be prescribed.
Patients on oral BPs are at a lower risk of ONJ or osteoclastic inhibition. Patients should be counselled about inhibited tooth movement, ONJ and impaired bone healing with elective surgery procedures. If orthodontic treatment is indicated, it should be planned to minimize risks including a non-extraction protocol favouring interproximal stripping to limit the treatment time and the degree of tooth movement and so treatment can be discontinued early if needed. Informed consent should outline all the risks associated with orthodontics and BPs.113
Treatment should be aimed at reducing the risk of DIGO occurring or at least preventing the DIGO worsening. The recurring message is to ensure patients have excellent oral hygiene in order to reduce the risk of DIGO.117 A rigorous oral hygiene programme should be instigated from the outset and reinforced during treatment.
A non-extraction approach is preferred in case treatment has to be terminated due to medical problems or exacerbation of the DIGO.76 Additionally, space closing mechanics including nickel titanium closing springs, elastomeric power chain or active ties can impinge on the hyperplastic gingival tissue. Archwire loops could have a similar effect and be displaced buccally, altering the direction of force.76
N N
The clinician should look for signs of ONJ and the patient should be advised to have regular dental check-ups. Some clinicians suggest that one should try to avoid invasive laser therapy or temporary anchorage devices in treatment plans;112 however a recent study of implants placed in 61, female patients taking oral BPs for longer than 3 years, revealed no untoward postoperative sequelae. This suggests that patients who take oral BPs are no more at risk of implant or temporary anchorage device failure than other patients.
Small low profile brackets are recommended and the excess composite around the margins should be removed. Bands should be avoided if possible as they have been associated with significantly more gingival inflammation than bonded molars.119
N
Drug induced gingival overgrowth (DIGO)
DIGO affects a proportion of patients on medication for hypertension, epilepsy and the prevention of organ transplant rejection. The clinical signs can vary in severity from minor overgrowth to complete coverage of standing teeth. These effects are compounded by poor oral hygiene but can occur in the absence of plaque.116 Drifting of teeth can also occur resulting in further aesthetic and functional problems for the patient.78 The main drugs that cause DIGO are phenytoin, cyclosporine and calcium channel blockers including nifedipine, diltiazem, and amlodipine.78 There are a few alternatives for reducing gingival overgrowth.117 One possibility is to have the patient placed on a different drug. There is usually spontaneous regression of the gingival hyperplasia provided the oral hygiene is excellent.118 Non-surgical techniques can limit the occurrence of DIGO, reduce the extent of plaque-induced gingival inammation and reduce the rate of recurrence. In some patients, however the drug is critical to control either their epilepsy, transplant, cardiac condition. In these cases intensive periodontal treatment with excision of the hyperplastic tissue is necessary.
Essix based retainers should be relieved around the gingival margins to maintain alignment. Bonded retainers should be avoided in patients at risk of DIGO.76
Allergies
Two key allergic reactions have been described in the literature. Type I hypersensitivity reactions are an immediate antibody mediated allergic response, occurring within minutes or hours after direct skin or mucosal contact with the allergen.120 This reaction ranges from contact urticaria to full-blown anaphylaxis with respiratory distress and or hypotension. A delayed hypersensitivity reaction (Type IV) usually presents with localized allergic contact dermatitis. It presents with diffuse or patchy eczema on the contact area and may be accompanied initially by itching, redness, and vesicle formation. The reactions are not life threatening but can cause permanent damage if not treated. The face, especially the lips and mouth, is more commonly affected in dental patients who develop a latex allergy. Orthodontic staff should be trained in how to deal with an anaphylactic shock. Figure 1 illustrates the sequence of steps that have been outlined by the Resuscitation Council (UK).121
JO December 2009
Clinical Section
Medical disorders and orthodontics
15
Figure 1 Anaphylaxis treatment algorithm adapted from Resuscitation Council UK guidelines 2008
Nickel
Orthodontists are sometimes required to treat patients with an allergy to nickel and nickel is present in a number of orthodontic materials, notably nickel titanium (NiTi) archwires. The nickel in stainless steel (SS) is thought to be tightly bound to the crystal lattice of the alloy making it difcult for it to leach out. The immune response to nickel is usually a type IV cell mediated delayed hypersensitivity reaction. The rst phase or sensitization to nickel is increasing with the increasing use of jewellery containing the metal. The prevalence of nickel allergy is estimated 11% of all women and 2% of men.122 Re-exposure to nickel can results in contact dermatitis or mucositis and develops over a period of days or rarely up to 3 weeks.123 Fortunately most individuals with nickel allergy do not report reactions to orthodontic appliances containing nickel. A study by Bass and colleagues of 29 subjects (18 female and 11 male) revealed an initial positive skin patch test to nickel sulphate in ve female patients only.124 All 29 patients were followed over their xed appliance treatment. None of the subjects including the positive test patients demonstrated an inammatory reaction or discomfort as a result of orthodontic treatment. It is postulated that a much greater concentration of nickel in the oral mucosa than the skin is necessary to elicit an immune response. Nickel leaching from orthodontic bands, brackets, stainless steel or NiTi archwires has been shown in vitro to occur within the rst week and then decline thereafter.125 Oral
uids, certain foods and uoride media can corrode and accelerate the leaching process.126 Concerns about sensitising orthodontic patients to nickel are not supported by the literature but there are a few case reports of localized allergic responses attributed to nickel containing orthodontic appliances.127,128 Oral clinical signs and symptoms of nickel allergy can include the following: a burning sensation, gingival hyperplasia, angular chelitis, labial desquamation, erythema multiforme, periodontitis, stomatitis with mild to severe erythema, loss of taste or metallic taste, numbness, soreness of the side of the tongue.128
Orthodontic considerations in patients with a nickel allergy
N N N
A dermatologist should confirm a true nickel allergy. Patients with a defined history of atopic dermatitis to nickel containing metals should be treated with caution and closely monitored during orthodontic treatment.129 In patients with diagnosed nickel hypersensitivity and where intra-oral signs and symptoms are present the orthodontist should replace Ni-Ti archwires with one of the following: # stainless steel archwires with a low nickel content; # titanium molybdenum alloy (TMA) which is nickel free; # fibre reinforced composite wires; # pure titanium or gold plated wires.
16
Patel et al.
Clinical Section
JO December 2009
Orthodontic considerations in patients with a nickel allergy
Orthodontic considerations in patients with latex allergy
If the allergic reaction continues, all SS archwires and brackets should be removed. If the allergic reaction is severe the patient should be referred to a physician. Alternative nickel free bracket materials include ceramic, polycarbonate, titanium and gold.129 Fixed appliances may be substituted with plastic aligners in selected cases.
The goal is to significantly reduce exposure to patients routinely. This can be done by cleaning the surgery more frequently with a protein wash, cleaning or changing the air filter more regularly.132
N N
Latex free goods should be stored in a latex-screened area to avoid prior contamination with latex products. Patients with a diagnosed allergy can be offered early morning appointments to reduce the exposure to airborne latex particle.
Latex allergy
The increase in allergic reactions to natural rubber latex over the past two decades has been accredited to the increased use of latex based gloves and universal precautions. Disposable medical gloves, particularly powdered gloves are the main reservoir of latex allergens. Orthodontic elastics used to apply intermaxillary forces are another potential source of the latex protein. Both type I and type IV hypersensitivity reactions can occur. The prevalence of potential type I hypersensitivity to latex is lower than 1% in the general population and between 612% among dental professionals. For the purpose of this review only risks to patients will be discussed. Patients at risk of allergy are those with a history of atopy such as hay fever; asthma; eczema; contact dermatitis and those with spina bida.130 Allergies to certain fruits such as banana, avocado, passion fruit, kiwi and chestnut can also indicate a potential latex allergy. They have proteins that are capable of crossreacting with latex proteins and hence help sensitize the person to latex.131 Clinical tests, of which the skin prick test is considered most accurate, can determine the presence of circulating antibodies to latex. Multiple testing is recommended for increased accuracy of diagnosis. Denitive diagnosis should be based on the medical history, and a positive skin reaction to specic chemicals present in natural rubber latex.
N N
The diagnosed patient should be monitored for signs of adverse reactions. The team should be capable of instigating prompt emergency care. The emergency drugs and resuscitation equipment should be free from latex.133
Latex free orthodontic materials There are a number of latex free alternatives to commonly used orthodontic materials. Natural rubber latex is found in gloves, elastics, separators, elastomeric modules, elastomeric power chain, polishing rubber cups, band removers and masks with latex ties.
Synthetic non-latex gloves made from nitrile, polychloroprene, elastyren and vinyl, are readily available for clinical use. Both latex free and latex gloves have to meet the European standard for single use medical examination gloves.
Russell and coworkers reported that latex free elastics demonstrated greater hysteresis than latex elastics (40% force decay compared with 25% over 24 h).134 The range of forces produced by the non-latex elastics was larger in vitro, but this difference was not deemed to be clinically significant.
N N
Elastomeric separators can be replaced with self-locking separating springs.132 Manufacturers can provide alternatives such as latex free power chain, ligature chain, rotation wedges, headgear components, and masks. It is wise to check with retailers that the product they are marketing is latex free.132
Orthodontic considerations in patients with latex allergy Pre-diagnosis
Eating disorders
The most common eating disorders are anorexia nervosa (AN) and bulimia nervosa (BN). Eating disorders are more common in females and generally have their onset during the teen years but often continue as a chronic illness. AN is an important cause of mortality in adolescent females. Patients with AN have a combination of body image distortion and restricted eating.135 Binge eating and purging are also characteristics of BN.
If a reaction to latex is suspected, patients should be referred to
an allergist, clinical immunologist or dermatologist for testing. Post-diagnosis
The orthodontic team including radiographers should be aware of the implication of treating latex allergy patients.
JO December 2009
Clinical Section
Medical disorders and orthodontics
17
Patients with eating disorders rarely present with problems of compliance. Oral manifestations of eating disorders include dental caries, erosion, dentinal hypersensitivity, salivary gland hypertrophy, raised occlusal restorations and xerostomia.136
Orthodontic considerations in patients with eating disorders
6.
7.
The orthodontist is likely to notice these features and should be suspicious of these illnesses and deal with them sensitively.137 The first referral should be to the patients physician. However, it is important to maintain confidentiality and gain consent.138 Referral to another healthcare professional, such as a physician may be a breach of confidentiality if the patient did not give their consent. These patients are less likely to discuss their illness as they tend to be embarrassed and secretive.
8.
N N
Diet advice is vital as this cohort of patients may drink an excessive quantity of acidic or carbonated drinks to as an alternative to normal food.139 Patients should be counselled not to brush their teeth immediately after vomiting. They should be given advice on how to increase the intra-oral pH by chewing gum, or rinsing the mouth with water or milk.139
9.
Summary
Orthodontic treatment is an elective procedure and clinicians should consider all the treatment options to ensure a satisfactory risk-benet ratio for each and every patient. Comprehensive treatment may not always benet the patient. Treatment should where appropriate be postponed until the medical problem is in remission or the side effects of the drug therapy are minimized. Patients should always be involved in the treatmentplanning phase so that true informed consent can be obtained.
10.
11.
12. 13.
14. 15.
References
1. Sonis ST. Orthodontic management of selected medically compromised patients: cardiac disease, bleeding disorders, and asthma. Semin Orthod 2004; 10: 27780. 2. Sheller B, Williams B. Orthodontic management of patients with hematological malignancies. Am J Orthod Dentofacial Orthop 1996; 109: 57580. 3. Prendergast BD. The changing face of infective endocarditis. Heart 2006; 92: 87985. 4. Moreillon P, Que Y-A. Infective endocarditis. Lancet 2004; 363: 13949. 5. Horstkotte D, Follath F, Gutschik E, et al. Guidelines on prevention, diagnosis and treatment of infective endocarditis executive summary; the task force on infective 16.
17.
18.
19.
endocarditis of the European society of cardiology. Eur Heart J 2004; 25: 26776. Danchin N, Duval X, Leport C. Prophylaxis of infective endocarditis: French recommendations 2002. Heart 2005; 91: 71518. Gould FK, Elliott TS, Foweraker J, et al. Guidelines for the prevention of endocarditis: report of the Working Party of the British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother 2006; 57: 1035 42. Wilson W, Taubert KA, Gewitz M, et al. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. J Am Dent Assoc. 2008; 139(Suppl): 3S24S. NICE Short Clinical Guidelines Technical Team. Prophylaxis Against Infective Endocarditis: Antimicrobial Prophylaxis Against Infective Endocarditis in Adults and Children Undergoing Interventional Procedures. London: National Institute for Health and Clinical Excellence, 2008. Oliver R, Roberts GJ, Hooper L. Penicillins for the prophylaxis in dentistry. Cochrane Database Systematic Reviews 2004; 2: CD003813. Hobson R, Clark JD. Infective Endocarditis associated with orthodontic treatment: a case report. Br J Orthod 1993; 20: 24144. Dajani AS. Bacterial endocarditis after minor orthodontic procedures. J Pediatr 1991; 119: 33940. Biancaiello TM, Romero JR. Bacterial endocarditis after adjustment of orthodontic appliances. J Pediatr 1991; 118: 24849. Ahlstedt S. Penicillin allergy can the incidence be reduced? Allergy 1984; 39: 15164. Misra S, Percival RS, Devine DA, Duggal MS. A pilot study to assess bacteraemia associated with tooth brushing using conventional, electric or ultrasonic toothbrushes. Eur Arch Paediatr Dent 2007; 8: 4245. Lucas VS, Omar J, Vieira A, Roberts GJ. The relationship between odontogenic bacteraemia and orthodontic treatment procedures. Eur J Orthod 2002; 24: 293301. Burden DJ, Coulter WA, Johnston CD, Mullally B, Stevenson M. The prevalence of bacteraemia on removal of fixed orthodontic appliances. Eur J Orthod 2004; 26: 44347. Lucas VS, Kyriazidou, Gelbier, Roberts GJ. Bacteraemia following debanding and gold chain adjustment. Eur J Orthod 2007; 29: 16165. Lockhart PB, Gibson J, Pond SH, Leitch J. Dental management considerations for the patient with an
18
Patel et al.
Clinical Section
JO December 2009
20.
21.
22.
23.
24. 25.
26.
27.
28.
29.
30.
31. 32. 33.
34.
35.
36.
acquired coagulopathy. Part 1: coagulopathies from systemic disease. Br Dent J 2003; 195: 43945. Meechan JG, Greenwood M. General medicine and surgery for dental practitioners Part 9: haematology and patients with bleeding problems. Br Dent J 2003; 195: 305 10. Committee on Dangerous Pathogens (ACDP) and the Spongiform Encephalopathy Advisory Committee (SEAC). Transmissible spongiform encephalopathy agents: safe working and the prevention of infection. Department of Health, UK, June 2003. Economics and operational research division. Risk assessment for vCJD in dentistry. Department of Health, June 2003. Farrugia A. variant Creutzfeldt-Jakob disease and hemophilia further guidance on assessing the risks of plasmaderived products for treating hemophilia. World Federation of Hemophilia task force on Transmissible Spongiform Encephalopathies, 2004. Grossman RC. Orthodontics and dentistry for the hemophilic patient. Am J Orthod 1975; 68: 391403. Gupta A, Epstein JB, Cabay RJ. Bleeding disorders of importance in dental care and related patient management. J Canadian Dent Assoc 2007; 73: 7783. Piot B, Sigaud-Fiks M, Huet P, Fressinaud E, Trossaet M, Mercier J. Management of dental extractions in patients with bleeding disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 93: 24750. Burden D, Mullally B, Sandler J. Orthodontic treatment of patients with medical disorders. Eur J Orthod 2001; 23: 36372. Van Venrooy JR, Proffit WR. Orthodontics care for medically compromised patients: possibilities and limitation. J Am Dent Assoc 1985; 111: 26266. Platt OS, Brambilla DJ, Rosse WF, et al. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med 1994; 331: 102223. Kwiatkowski DP. How malaria has affected the human genome and what human genetics can teach us about malaria. Am J Hum Genet 2005; 77: 17192. Sergeant G, Sergeant B. Painful crises in sickle-cell disease. Lancet 1996; 347: 119091. Platt OS. Hydroxyurea for the treatment of sickle cell anemia. N Engl J Med 2008; 358: 135269. Michaelson J, Bhola M. Oral lesions of sickle cell anemia: case report and review of the literature. J Mich Dent Assoc 2004; 86: 3235. Alves PV, Alves DK, de Souza MM, Torres SR. Orthodontic treatment of patients with sickle-cell anemia. Angle Orthod 2006; 76: 26973. Greenwood M, Meechan JG. General medicine and surgery for dental practitioners. Part 10: The paediatric patient. Br Dent J 2003; 195: 36772. Forsberg CM, Krekmanova L, Dahloff G. The effect of growth hormone therapy on mandibular and cranial base
37.
38.
39.
40.
41. 42.
43.
44.
45. 46.
47.
48. 49. 50.
51.
52.
53.
54.
development in children treated with total body irradiation. Eur J Orthod 2002; 24: 28592. Athanassiadou F, Tragiannidis A, Rousso I, et al. Bone mineral density in survivors of childhood acute lymphoblastic leukemia. Turk J Pediatr 2006; 48: 10104. Nasman M, Forsberg CM, Dahllof G. Disturbances in dental development in long-term survivors after pediatric malignant diseases. Eur J Orthod 1997; 19: 15159. Dahllof G, Forsberg CM, Ringden O, et al. Facial growth and morphology in long-term survivors after bone marrow transplantation. Eur J Orthod 1989; 11: 33240. Dahllof G, Huggare J. Orthodontic considerations in the pediatric cancer patients: a review. Semin Orthod 2004; 10: 26676. Scully C, Cawson RA. Medical Problems in Dentistry, 5th Edn. Edinburgh: Elsevier Churchill Livingstone, 2005. Dahllof G, Jonsson A, Ulmner M, Huggare J. Orthodontic treatment in long-term survivors after pediatric bone marrow transplantation. Am J Orthod Dentofacial Orthop 2001; 120: 45965. Levander E, Malmgren O, Eliasson S. Evaluation of root resorption in relation to two orthodontic treatment regimes. A clinical experimental study. Eur J Orthod 1994; 16: 22328. Sulaiman F, Huryn JM, Zlotolow IM. Dental extractions in the irradiated head and neck patient: a retrospective analysis of Memorial Sloan-Kettering Cancer Center protocols, criteria and end results. J Oral Maxillofac Surg 2003; 61: 112331. http://www.efanet.org/asthma/index.html McNab S, Battistutta D, Tavernea A, Symons AL. External apical root resorption of posterior teeth in asthmatics after orthodontic movement. Am J Orthod Dentofac Orthop 1999; 116: 54561. de Valk HW, van der Graaf EA. Cystic fibrosis-related diabetes in adults: where can we go from here? Rev Diabet Stud 2007; 4: 612. Akata D, Akhan O. Liver manifestations of cystic fibrosis. Eur J Radiol 2007; 61: 1117. Ratjen F. Recent advances in cystic fibrosis. Paediatr Respir Rev 2008; 9: 14448. Primosch RE. Tetracycline discoloration, enamel defects, and dental caries in patients with cystic fibrosis. Oral Surg Oral Med Oral Pathol 1980; 50: 30108. Kinirons MJ. The effect of antibiotic therapy on the oral health of cystic fibrosis children. Int J Paediatr Dent 1992; 2: 13943. Fukushima C, Matsuse H, Saeki S, et al. Salivary IgA and oral Candidiasis in asthmatic patients treated with inhaled corticosteroid. J Asthma 2005; 42: 60104. Greenwood M, Meechan JG. General medicine and surgery for dental practitioners. Part 2: respiratory system. Br Dent J 2003; 194: 59398. Dursun AB, Woessner KA, Simon RA, Karasoy D, Stevenson DD. Predicting outcomes of oral aspirin
JO December 2009
Clinical Section
Medical disorders and orthodontics
19
55.
56. 57. 58.
59. 60. 61.
62.
63.
64. 65. 66.
67. 68.
69.
70.
71. 72.
73.
74.
challenges in patients with asthma, nasal polyps, and chronic sinusitis. Ann Allergy Asthma Immunol 2008; 100: 42025. Hutchinson S, Clark S. Multiple sclerosis presenting to the dental practitioner: a report of two cases. Dent Update 2001; 28: 51617. Fiske J, Boyle C. Epilepsy and oral care. Dent Update 2002; 29: 18087. Fiske J, Shafik HH. Downs syndrome and oral care. Dent Update 2001; 28: 14856. Gorlin RJ, Cohen Jr MM, Hennekam RCM. Syndromes of the Head and Neck, 4th Edn. Oxford: Oxford University Press, 2001. Sander JW. The epidemiology of epilepsy revisited. Curr Opin Neurol 2003; 16: 16570. Sheller B. Orthodontic management of patients with seizure disorders. Semin Orthod 2004; 10: 24751. Seymour RA, Thomason JM, Ellis JS. The pathogenesis of drug-induced gingival overgrowth. J Clin Periodontol 1996; 23: 16575. Hassel TM, Burtner AP, McNeal D, Smith RG. Oral problems and genetic aspects of individuals with epilepsy. Periodontol 2000 1994; 6: 6878. Sanders B, Weddell JA, Dodge NN. Managing patients who have seizure disorders: dental and medical issues. J Am Dent Assoc 1995; 126: 164147. Rosati G. The prevalence of multiple sclerosis in the world: an update. Neurol Sci 2001; 22: 11739. www.mssociety.org.uk Majola MP, McFayden ML, Connolly C, Nair YP, Govender M. Factors influencing phenytoin-induced gingival enlargement. J Clin Periodont 2000; 27: 50612. Fiske J, Griffiths J, Thompson S. Multiple sclerosis and oral care. Dent Update 2002; 29: 27383. Torogulu MS, Bayramoglu O, Yarkin F, Tuli A. Possibility of blood and hepatitis B contamination through aerosols generated during debonding procedures. Angle Orthod 2003; 73: 57178. Greenwood M, Meechan JG. General medicine and surgery for dental practitioners. Part 5: liver disease. Br Dent J 2003; 195: 7173. McCarthy GM, Mamandras AH, MacDonald JK. Infection control in the orthodontic office in Canada. Am J Orthod Dentofacial Orthop 1997; 112: 27581. http://www.diabetes.org.uk/Guide-to-diabetes/ What_is_diabetes/What_is_diabetes/ Pinhas-Hamiel O, Dolan L, Daniels S, Stanford D, Khowry P, Zeilter P. Increased incidence of non-insulin dependent diabetes mellitus amongst adolescents. J Pediatr 1996; 128: 60815. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004; 27: 104753. http://www.diabetes.org.uk/Guide-to-diabetes/Complications/ Long_term_complications/
75. Bensch L, Braem M, van Acker K, Willems G. Orthodontic treatment considerations in patients with diabetes mellitus. Am J Orthod Dentofacial Orthop 2003; 123: 7478. 76. Walker MR, Lovel SF, Melrose CA. Orthodontic treatment of a patient with a renal transplant and drug induced gingival overgrowth: a case report. J Orthod 2007;34:220 228. 77. Dental Practitioners Formulary 19982000, British National Formulary No. 36. London: The Royal Pharmaceutical Society of Great Britain and the British Medical Association, 1998. 78. Butterworth C, Chapple I. Drug-induced gingival overgrowth: a case with auto-correction of incisor drifting. Dent Update 2001; 28: 41116. 79. Shirazi M, Khosrowshahi M, Dehpour AR. The effect of chronic renal insufficiency on orthodontic tooth movement in rats. Angle Orthod 2001; 71: 49498. 80. http://www.emedicine.com/radio/byname/juvenile-rheumatoid-arthritis.htm 81. Manners PJ, Diepeveen DA. Prevalence of chronic arthritis in a population of 12-year-old children in urban Australia. Pediatrics 1996; 98: 8490. 82. Calabro JJ. Juvenile rheumatoid arthritis. Clin Paediatr Med Surg 1988; 5: 5775. 83. Twilt M, Mobers SM, Arends LR, ten Cate R, van Suijlekom-Smit L. Temporomandibular involvement in juvenile idiopathic arthritis. J Rheumatol 2004; 31: 141822. 84. Pederson TK. Clinical aspects of orthodontic treatment for children with juvenile chronic arthritis. Acta Odontol Scand 1998; 56: 36668. 85. Sidiropoulou-Chatzigianni S, Papadopoulos MA, Kolokithas G. Dentoskeletal morphology in children with juvenile idiopathic arthritis compared with healthy children. J Orthod 2001; 28: 5358. 86. Welbury RR, Thomason JM, Fitzgerald JL, Steen IN, Marshall NJ, Foster HE. Increased prevalence of dental caries and poor oral hygiene in juvenile idiopathic arthritis. Rheumatology 2003; 42: 144551. 87. Pederson TK, Grnhj J, Melsen B, Herlin T. Condylar condition and mandibular growth during early functional treatment of children with juvenile chronic arthritis, Eur J Orthod 1996; 17: 38594. 88. Callabro JJ. Juvenile rheumatoid arthritis. Clin Pediatr Med Surg 1988; 5: 5775. 89. Stroustrup P, Kristensen KD, Kuseler A, et al. Reduced mandibular growth in experimental arthritis in the temporomandibular joint treated with intra-articular corticosteroid. Eur J Orthod 2008; 30: 11119. 90. Greenwood M, Meechan JG. General medicine and surgery for dental practitioners. Part 8: Musculoskeletal system. Br Dent J 2003; 195: 24348. 91. Proffit WR. Treatment planning: the search for wisdom. In Proffit WR, White Jr RP (eds.). Surgical Orthodontic Treatment. St Louis: Mosby, 1991, 159.
20
Patel et al.
Clinical Section
JO December 2009
92. Kjellberg H, Kiliardis S, Thilander B. Dentofacial growth in orthodontically treated and untreated children with juvenile chronic arthritis (JCA). A comparison with Angle Class II division 1 subjects. Eur J Orthod 1995; 17: 35773. 93. Prestwood KM, Pilbeam CC, Burleson JA, et al. The short-term effects of conjugated estrogen on bone turnover in older women. J Clin Endocrinol Metab 1994; 79: 36671. 94. Melton LJ. Epidemiology worldwide. Endocrinol Metab Clin North Am 2003; 32: 113. 95. Wong PK, Christie JJ, Wark JD. The effects of smoking on bone health. Clin Sci 2007; 113: 23341. 96. Shapses SA, Riedt CS. Bone, body weight, and weight reduction: what are the concerns? J Nutr 2006; 136: 1453 56. 97. WHO Scientific Group on the Prevention and Management of Osteoporosis (2000 : Geneva, Switzerland). Prevention and management of osteoporosis : report of a WHO scientific group, 2003, available at: http://whqlibdoc. who.int/trs/WHO_TRS_921.pdf. 98. Ashcraft MB, Southard KA, Tolley EA. The effect of corticosteroid-induced osteoporosis on orthodontic tooth movement Am J Orthod Dentofacial Orthop 1992; 102: 31019. 99. Bonaiuti D, Shea B, Iovine R, et al. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev 2002; (3): CD000333. doi:10.1002/14651858.CD000333. PMID 12137611. 100. Pazanias M, Miller P, Blumentals WA, Bernal M, Kothawala P. A review of the literature on osteonecrosis of the jaw in patients with osteoporosis treated with oral bisphosphonates: prevalence, risk factors, and clinical characteristics. Clin Ther 2007; 29: 154858. 101. Advisory task force on Bisphosphonate-related osteonecrosis of the jaws, Americal Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonaterelated osteonecrosis of the jaws. J Oral Maxillofac Surg 2007; 65: 369375. 102. Arias OR, Marquez-Orozco MC. Aspirin, acetaminophen, and ibuprofen: their effects on orthodontic tooth movement. Am J Orthod Dentofacial Orthop 2006; 130: 36470. 103. de Carlos F, Cobo J, Perillan C, et al. Orthodontic tooth movement after different coxib therapies. Eur J Orthod 2007; 29: 59699. 104. http://www.mca.gov.uk/ourwork/monitorsafequalmed/ currentproblems/volume24may.htm. 105. Gibson N, Ferguson JW. Steroid cover for dental patients on long-term steroid medication: proposed clinical guidelines based upon a critical review of the literature. Br Dent J 2004; 197: 68185. 106. Thomason JM, Girdler NM, Kendall-Taylor P, Wastell H, Weddel A, Seymour RA. An investigation into the need for supplementary steroids in organ transplant patients undergoing gingival surgery: a double-blind, split-mouth, cross-over study. J Clin Periodontol 1999; 26: 57782.
107. Kalia S, Melsen B, Verna C. Tissue reaction to orthodontic tooth movement in acute and chronic corticosteroid treatment. Orthod Craniofac Res 2004; 7: 2634. 108. Igarashi K, Mitani H, Adachi H, Shinoda H. Anchorage and retentive effects of a bisphosphonate (AHBuBP) on tooth movement in rats. Am J Orthod Dentofacial Orthop 1994; 106: 27989. 109. Advisory task force on Bisphosphonate-related osteonecrosis of the jaws, Americal Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonaterelated osteonecrosis of the jaws. J Oral Maxillofac Surg 2007; 65: 36975. 110. Marx RE, Sawatari Y, Fortin M, Broumand V. Bisphosphonate-induced exposed bone (osteonecrosis/ osteopetrosis) of the jaws: risk factors, recognition, prevention and treatment. J Oral Maxillofac Surg 2005; 63: 156775. 111. Barker K, Rogers S. Bisphosphonate-associated osteoradionecrosis of the jaws: a guide for the General Dental Practitioner. Dent Update 2006; 33: 27075. 112. Graham JW. Bisphosphonates and orthodontics: clinical implications. J Clin Orthod 2006: 40: 42528. 113. Zahrowski JJ. Bisphosphonate treatment: an orthodontic concern calling for a proactive approach. Am J Orthod Dentofacial Orthop 2007; 131: 31120. 114. Rinchuse DJ, Rinchuse DJ, Sosovicka MF, Robison JM, Pendleton R. Orthodontic treatment of patients using bisphosphonates: a report of 2 cases. Am J Orthod Orthop 2007; 131: 32126. 115. Lin JH. Bisphosphonates: a review of the pharmacokinetic properties. Bone 1996; 18: 7585. 116. Chabria D, Weintraub RG, Kilpatrick NM. Mechanisms and management of gingival overgrowth in paediatric transplant patients: a review. Int J Paediatr Dent 2003; 13: 22029. 117. Marvogiannis M, Ellis JS, Thomason JM, Seymour RA. The management of drug-induced gingival overgrowth. J Clin Periodontol 2006; 33: 43439. 118. James JA, Boomer S, Maxwell AP, et al. Reduction in gingival overgrowth associated with conversion from cyclosporin A to tacrolimus. J Clin Periodontol 2000; 27: 14448. 119. Boyd RL, Baumrind S, Periodontal considerations in the use of bonds or bands on molars in adolescents and adults. Angle Orthod 1992; 62: 11726. 120. Poley GE Jr, Slater JE. Latex allergy. J Allergy Clin Immunol 2000; 105: 105462. 121. Working Party of Resuscitation council (UK). Emergency treatment of anaphylactic reactions. Guidelines for healthcare providers. January 2008; 20, available at: http:// www.resus.org.uk/pages/reaction.pdf 122. Nielson NH, Menne T. Nickel sensitisation and ear piercing in an unselected Danish population. Contact Dermatitis 1993; 29: 1621. 123. Hostynek JJ. Sensitization to nickel: etiology, epidemiology, immune reactions, prevention and therapy. Rev Environ Health 2006; 21: 25380.
JO December 2009
Clinical Section
Medical disorders and orthodontics
21
124. Bass JK, Fine H, Cisneros GJ. Nickel sensitivity in the orthodontic patient. Am J Orthod Dentofac Orthop 1993; 103: 28085. 125. Barrett RD, Bishara SE, Quinn YK. Biodegradation of orthodontic appliances. Part 1: biodegradation of nickel and chromium in vitro. Am J Orthod Dentofac Orthop 1993; 103: 814. 126. Schiff N, Boinet M, Morgan L, et al. Galvanic corrosion between orthodontic wires and brackets in fluoride mouthwashes. Eur J Orthod 2006; 28: 298304. 127. Dunlap CL, Vincent SK, Barker BF. Allergic reaction to orthodontic wire: report of a case. J Am Dent Assoc 1989; 118: 449450. 128. Noble J, Ahing SI, Karaiskos NE, Wiltshire WA. Nickel allergy and orthodontics, a review and report of two cases. Br Dent J 2008; 204: 297300. 129. Leite LP, Bell RA. Adverse hypersensitivity reactions in orthodontics. Semin Orthod 2004; 10: 24043. 130. ADA Council on Scientific Affairs. The dental team and latex hypersensitivity. J Am Dent Assoc 1999; 130: 25764. 131. Isola S, Ricciardi L, Saitta S, et al. Latex allergy and fruit cross-reaction in subjects who are non atopic. Allergy Asthma Proc 2003; 24: 19397. 132. Hain MA, Longman LP, Field E, Harrison J. Natural rubber latex allergy: implications for the orthodontist. J Orthod 2007; 34: 611.
133. Field EA, Longman LP. Guidance for the management of natural rubber latex allergy in dental patients and dental healthworkers. London: Faculty of General Dental Practitioners (UK), The Royal College of Surgeons, 2004. 134. Russell KA, Milne AD, Khanna RA, Lee JM. In vitro assessment of the mechanical properties of latex and non latex orthodontic elastics. Am J Orthod Dentofacial Orthop 2004; 126: 6570. 135. Ashcroft A, Milosevic A. The eating disorders: 1. Current scientific understanding and dental implications. Dent Update 2007; 34: 54454. 136. Neeley WW, Kluemper GT, Hays LR. Psychiatry in orthodontics. Part 1: typical adolescent psychiatric disorders and their relevance to orthodontic practice. Am J Orthod Dentofacial Orthop 2006; 129: 17684. 137. Burke FJT, Bell TJ, Ismail N, Hartley P. Bulimia: implications for the practising dentist. Br Dent J 1996; 180: 42126. 138. Crossley ML, Shearer AC, Mellor AC, Bridgeman AM. Treatment planning for the problem patient: restorative, ethical, legal and psychological perspectives. Dent Update 2001; 28: 24146. 139. Ashcroft A, Milosevic A. The eating disorders: 2. Behavioural and dental management. Dent Update 2007; 34: 61220.
Potrebbero piacerti anche
- Functional ApplianceHGHDFGDocumento40 pagineFunctional ApplianceHGHDFGmustafa_tambawalaNessuna valutazione finora
- V-Bend and Anchorage in Orthodontics: Mehak Arya Iyrmds Dept of OrthodonticsDocumento37 pagineV-Bend and Anchorage in Orthodontics: Mehak Arya Iyrmds Dept of OrthodonticsMehak AryaNessuna valutazione finora
- The MBT Bracket System GuideDocumento11 pagineThe MBT Bracket System GuideNaveenNessuna valutazione finora
- At The Gates of Despair, Beginning of Hope (English Translation) by Florica IchimDocumento72 pagineAt The Gates of Despair, Beginning of Hope (English Translation) by Florica IchimDumitru Ichim100% (1)
- Retention and Relapse in OrthodonticsDocumento46 pagineRetention and Relapse in OrthodonticsFera Sun0% (1)
- Revision Notes Haematology 1 6 PDFDocumento23 pagineRevision Notes Haematology 1 6 PDFCattrainuhNessuna valutazione finora
- Adult Orthodontic TreatmentDocumento16 pagineAdult Orthodontic TreatmentMuhammad AsimNessuna valutazione finora
- Adult Orthodontics SeminarDocumento52 pagineAdult Orthodontics Seminaravanthika krishnaraj100% (2)
- Surgical Procedures in OrthodonticsDocumento36 pagineSurgical Procedures in OrthodonticsAsnovya0% (1)
- Retention and Relapse SeminarDocumento51 pagineRetention and Relapse SeminarShabeel Pn100% (2)
- Roth Vs MBT PDFDocumento8 pagineRoth Vs MBT PDFandiiperezNessuna valutazione finora
- Accelerated OrthodonticsDocumento5 pagineAccelerated OrthodonticsMiguel Soni CasillasNessuna valutazione finora
- Fixed Appliance Design, Function and ConstructionDocumento14 pagineFixed Appliance Design, Function and Constructionsp vumbunu100% (1)
- Self Ligating BracketsDocumento60 pagineSelf Ligating Bracketsbharvi100% (1)
- Loop MechanicsDocumento9 pagineLoop MechanicsMohammed HussainNessuna valutazione finora
- A To Z Orthodontics Vol 9 Preventive and Interceptive OrthodonticsDocumento38 pagineA To Z Orthodontics Vol 9 Preventive and Interceptive OrthodonticsJosue El Pirruris MejiaNessuna valutazione finora
- Basic Cephalometrics: Mark H. Taylor, D.D.S., F.A.C.DDocumento32 pagineBasic Cephalometrics: Mark H. Taylor, D.D.S., F.A.C.DSelimir ProdanovicNessuna valutazione finora
- Non-Extraction Class II TreatmentDocumento27 pagineNon-Extraction Class II TreatmentNeeraj AroraNessuna valutazione finora
- Skeletal Anchorage Systems in Orthodontics Absolute Anchorage Adream or RealityDocumento10 pagineSkeletal Anchorage Systems in Orthodontics Absolute Anchorage Adream or RealitySoe San KyawNessuna valutazione finora
- ONCOLOGY NURSING CARE PLANDocumento19 pagineONCOLOGY NURSING CARE PLANLiezel Cauilan0% (1)
- Tweed - A Philosophy of Orthodontic TreatmentDocumento30 pagineTweed - A Philosophy of Orthodontic TreatmentriofrankfurtNessuna valutazione finora
- AJODO-mechanism-case ReportDocumento10 pagineAJODO-mechanism-case ReportAthira JithendranathNessuna valutazione finora
- Biomechanics and Types of Movement 9b670d85Documento41 pagineBiomechanics and Types of Movement 9b670d85NamBuiNessuna valutazione finora
- MBT Appliance: Mclaughlin Bennett TrevisiDocumento247 pagineMBT Appliance: Mclaughlin Bennett TrevisiJustFine DolittleNessuna valutazione finora
- Malocclusion and TMDDocumento6 pagineMalocclusion and TMDRMTLG2Nessuna valutazione finora
- Nursing Care Plan for Leukemia PatientDocumento2 pagineNursing Care Plan for Leukemia Patientخالد الغامديNessuna valutazione finora
- Fixed AppliancesDocumento60 pagineFixed AppliancesMohsin Habib100% (1)
- MSC Orthodontics - Programme DocumentationDocumento40 pagineMSC Orthodontics - Programme DocumentationRukshad Asif Jaman KhanNessuna valutazione finora
- Fixed Myofunctional ApplianceDocumento32 pagineFixed Myofunctional AppliancePranav Dave100% (1)
- Orthodontic CurriculumDocumento60 pagineOrthodontic CurriculumKiran KumarNessuna valutazione finora
- Schwartz 9th Ed: Chapter Outline: The SpleenDocumento22 pagineSchwartz 9th Ed: Chapter Outline: The SpleenKathryn Reunilla100% (1)
- Various Intrusive ArchsDocumento10 pagineVarious Intrusive ArchsmutansNessuna valutazione finora
- THE ORTHODONTIC ROADMAP: GUIDELINES FOR THE DIAGNOSIS AND TREATMENT OF ORTHODONTIC MALOCCLUSIONSDa EverandTHE ORTHODONTIC ROADMAP: GUIDELINES FOR THE DIAGNOSIS AND TREATMENT OF ORTHODONTIC MALOCCLUSIONSNessuna valutazione finora
- Clear Aligner Therapy - A Case ReportDocumento9 pagineClear Aligner Therapy - A Case ReportDawjeeNessuna valutazione finora
- Cannon BracketsDocumento92 pagineCannon BracketsSzenyes Szabolcs0% (1)
- Anatomy and Physiology Related To Multiple Myelom1Documento15 pagineAnatomy and Physiology Related To Multiple Myelom1Diane Kate Tobias Magno100% (1)
- Extraction Vs Non Extraction Controversy: A Review: January 2018Documento9 pagineExtraction Vs Non Extraction Controversy: A Review: January 2018Jawad TariqNessuna valutazione finora
- Iron-rich foods for sickle cell anemiaDocumento24 pagineIron-rich foods for sickle cell anemiaZyla MalinaoNessuna valutazione finora
- Orthodontics in the Vertical Dimension: A Case-Based ReviewDa EverandOrthodontics in the Vertical Dimension: A Case-Based ReviewNessuna valutazione finora
- Open-Bite Malocclusion: Treatment and StabilityDa EverandOpen-Bite Malocclusion: Treatment and StabilityGuilherme JansonValutazione: 5 su 5 stelle5/5 (1)
- Extractions in Orthodontics: An Update on Indications and PatternsDocumento10 pagineExtractions in Orthodontics: An Update on Indications and Patternsdrzana78100% (1)
- Diagnostic Elements For Tooth Extraction in OrthodonticsDocumento24 pagineDiagnostic Elements For Tooth Extraction in OrthodonticsLanaNessuna valutazione finora
- Few ControversiesDocumento9 pagineFew Controversieshassankhan9849Nessuna valutazione finora
- Open BiteDocumento6 pagineOpen BiteBarot brindaNessuna valutazione finora
- TDocumento2 pagineTNb100% (1)
- Biomechanics of Deep Overbite CorrectionDocumento8 pagineBiomechanics of Deep Overbite CorrectionLuis Paipay SantosNessuna valutazione finora
- Friction in OrthodonticsDocumento9 pagineFriction in Orthodonticsaa bbNessuna valutazione finora
- Biomechanical Implications of Rotation Correction in Orthodontics - Case SeriesDocumento5 pagineBiomechanical Implications of Rotation Correction in Orthodontics - Case SeriescempapiNessuna valutazione finora
- Guide to Timing Orthodontic TreatmentDocumento5 pagineGuide to Timing Orthodontic Treatmentdrzana78Nessuna valutazione finora
- Drugs Commonly Used in Orthodontics and Their EffectsDocumento43 pagineDrugs Commonly Used in Orthodontics and Their EffectsSushma Rayal SANessuna valutazione finora
- KLoop Molar Distalizing AppDocumento7 pagineKLoop Molar Distalizing AppAngie Römer HaroNessuna valutazione finora
- The Midline Diagnosis and Treatment ARTUROCAMACHODocumento10 pagineThe Midline Diagnosis and Treatment ARTUROCAMACHOMiguel AngelNessuna valutazione finora
- Finishing in Lingual OrthodonticsDocumento7 pagineFinishing in Lingual OrthodonticsSreenivasa Krishna ChaitanyaNessuna valutazione finora
- Facial Esthetics in OrthodonticsDocumento9 pagineFacial Esthetics in Orthodonticsroncholo0% (1)
- 66 Allery and OrthodonticDocumento5 pagine66 Allery and OrthodonticShruthi KamarajNessuna valutazione finora
- Paradigm Shift in Orthodontics PDFDocumento28 pagineParadigm Shift in Orthodontics PDFHardiklalakiya0% (1)
- Functional Occlusion in Orthodontics: ClinicalDocumento11 pagineFunctional Occlusion in Orthodontics: ClinicalNaeem MoollaNessuna valutazione finora
- Ortho ScarsDocumento6 pagineOrtho ScarssandeepNessuna valutazione finora
- Orthodontic AssessmentDocumento30 pagineOrthodontic Assessmentmentacity10100% (2)
- Cone Beam Tomography in Orthodontics PDFDocumento8 pagineCone Beam Tomography in Orthodontics PDFdruzair007Nessuna valutazione finora
- A Texbook of Orthodontics PDFDocumento351 pagineA Texbook of Orthodontics PDFBrayzza Lozano AragónNessuna valutazione finora
- Impacted Canine: Presented By: Dr. Ahmed Shihab Supervised By: Dr. SarahDocumento34 pagineImpacted Canine: Presented By: Dr. Ahmed Shihab Supervised By: Dr. SarahAhmed ShihabNessuna valutazione finora
- Aesthetic Brackets GuideDocumento20 pagineAesthetic Brackets GuideNbNessuna valutazione finora
- Scissors Bite-Dragon Helix ApplianceDocumento6 pagineScissors Bite-Dragon Helix ApplianceGaurav PatelNessuna valutazione finora
- Biomechanics of Deep Bite TreatmentDocumento66 pagineBiomechanics of Deep Bite TreatmentMaitreye PriyadarshiniNessuna valutazione finora
- Fixed Orthodontic Appliances: A Practical GuideDa EverandFixed Orthodontic Appliances: A Practical GuideValutazione: 1 su 5 stelle1/5 (1)
- Iub 9999 0Documento13 pagineIub 9999 0Simona VisanNessuna valutazione finora
- Module 13.3 CA in ChildrenDocumento27 pagineModule 13.3 CA in ChildrenkirstenNessuna valutazione finora
- Pielago NCPDocumento2 paginePielago NCPtaehyungieeNessuna valutazione finora
- Dental Considerations in Hematological DisordersDocumento21 pagineDental Considerations in Hematological DisordersMariya FatmaNessuna valutazione finora
- Effect of Point 6 Acupressure On Chemotherapy AssoDocumento9 pagineEffect of Point 6 Acupressure On Chemotherapy AssoUtami DewiNessuna valutazione finora
- Avocados Fight Prostate CancerDocumento2 pagineAvocados Fight Prostate CancerkhnumdumandfullofcumNessuna valutazione finora
- How I Treat Mixed-Phenotype Acute LeukemiaDocumento10 pagineHow I Treat Mixed-Phenotype Acute LeukemiawenyinriantoNessuna valutazione finora
- Data Sheet Daunorubicin Injection: Name of The MedicineDocumento15 pagineData Sheet Daunorubicin Injection: Name of The MedicineAbulHasan Idrus IstarNessuna valutazione finora
- Inhibidor Bomba de Protones e Infecci - NDocumento10 pagineInhibidor Bomba de Protones e Infecci - NSMIBA Medicina100% (1)
- Hypnoparenting Effects Towards Fatigue As An Impact of Chemotherapy Among Pediatric Patients With Acute Lymphoblastic LeukemiaDocumento7 pagineHypnoparenting Effects Towards Fatigue As An Impact of Chemotherapy Among Pediatric Patients With Acute Lymphoblastic LeukemiaMuhammad HaezarNessuna valutazione finora
- Determining The Significance of Persistent LimphocytosisDocumento16 pagineDetermining The Significance of Persistent Limphocytosismatias66Nessuna valutazione finora
- Biochemistry of CancerDocumento20 pagineBiochemistry of CancerJimmy WongNessuna valutazione finora
- Chronic Lymphocytic Leukemia: NCCN Guidelines For PatientsDocumento82 pagineChronic Lymphocytic Leukemia: NCCN Guidelines For PatientsvnNessuna valutazione finora
- Leukemia Literature ReviewDocumento6 pagineLeukemia Literature Reviewafmzmxkayjyoso100% (2)
- About Acute Myeloid Leukemia (AML)Documento9 pagineAbout Acute Myeloid Leukemia (AML)fikriafisNessuna valutazione finora
- Leukemia Case StudyDocumento32 pagineLeukemia Case Studydsaitta108Nessuna valutazione finora
- MCQDocumento17 pagineMCQBethelhem BerhanuNessuna valutazione finora
- Acute Leukemia: Basic PrinciplesDocumento3 pagineAcute Leukemia: Basic PrinciplesPrabhat GuptaNessuna valutazione finora
- All - Relapsed - All-Rez BFM 2002Documento151 pagineAll - Relapsed - All-Rez BFM 2002Gene-v ChongNessuna valutazione finora
- Dresslier Supporting The Leukaemia FoundationDocumento1 paginaDresslier Supporting The Leukaemia FoundationDavroeNessuna valutazione finora
- Hematology Lec MidtermDocumento10 pagineHematology Lec MidtermLoren EscotoNessuna valutazione finora
- Price List Wef 01-Nov2006 NewDocumento107 paginePrice List Wef 01-Nov2006 Newapi-3695832Nessuna valutazione finora
- Acute Leukemia - Multiple Choice Questions - Laboratory HubDocumento14 pagineAcute Leukemia - Multiple Choice Questions - Laboratory HubAssssssNessuna valutazione finora