Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Maternal Reviewer
Caricato da
Ivy DGDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Maternal Reviewer
Caricato da
Ivy DGCopyright:
Formati disponibili
1. A postpartum patient was in labor for 30 hours and had ruptured membranes for 24 hours.
For which of the following would the nurse be alert? a. Endometritis b. Endometriosis c. Salpingitis d. Pelvic thrombophlebitis 2. A client at 36 weeks gestation is schedule for a routine ultrasound prior to an amniocentesis. After teaching the client about the purpose for the ultrasound, which of the following client statements would indicate to the nurse in charge that the client needs further instruction? a. The ultrasound will help to locate the placenta b. The ultrasound identifies blood flow through the umbilical cord c. The test will determine where to insert the needle d. The ultrasound locates a pool of amniotic fluid 3. While the postpartum client is receiving herapin for thrombophlebitis, which of the following drugs would the nurse Mica expect to administer if the client develops complications related to heparin therapy? a. Calcium gluconate b. Protamine sulfate c. Methylegonovine (Methergine) d. Nitrofurantoin (macrodantin) 4. When caring for a 3-day-old neonate who is receiving phototherapy to treat jaundice, the nurse in charge would expect to do which of the following? a. Turn the neonate every 6 hours b. Encourage the mother to discontinue breast-feeding c. Notify the physician if the skin becomes bronze in color d. Check the vital signs every 2 to 4 hours 5. A primigravida in active labor is about 9 days post-term. The client desires a bilateral pudendal block anesthesia before delivery. After the nurse explains this type of anesthesia to the client, which of the following locations identified by the client as the area of relief would indicate to the nurse that the teaching was effective? a. Back b. Abdomen c. Fundus d. Perineum 6. The nurse is caring for a primigravida at about 2 months and 1 week gestation. After explaining self-care measures for common discomforts of pregnancy, the nurse determines that the client understands the instructions when she says: a. Nausea and vomiting can be decreased if I eat a few crackers before arising b. If I start to leak colostrum, I should cleanse my nipples with soap and water c. If I have a vaginal discharge, I should wear nylon underwear d. Leg cramps can be alleviated if I put an ice pack on the area
7. Thirty hours after delivery, the nurse in charge plans discharge teaching for the client about infant care. By this time, the nurse expects that the phase of postpartal psychological adaptation that the client would be in would be termed which of the following? a. Taking in b. Letting go c. Taking hold d. Resolution 8. A pregnant client is diagnosed with partial placenta previa. In explaining the diagnosis, the nurse tells the client that the usual treatment for partial placenta previa is which of the following? a. Activity limited to bed rest b. Platelet infusion c. Immediate cesarean delivery d. Labor induction with oxytocin 9. Nurse Julia plans to instruct the postpartum client about methods to prevent breast engorgement. Which of the following measures would the nurse include in the teaching plan? a. Feeding the neonate a maximum of 5 minutes per side on the first day b. Wearing a supportive brassiere with nipple shields c. Breast-feeding the neonate at frequent intervals d. Decreasing fluid intake for the first 24 to 48 hours 10. When the nurse on duty accidentally bumps the bassinet, the neonate throws out its arms, hands opened, and begins to cry. The nurse interprets this reaction as indicative of which of the following reflexes? a. Startle reflex b. Babinski reflex c. Grasping reflex d. Tonic neck reflex 11. A primigravida client at 25 weeks gestation visits the clinic and tells the nurse that her lower back aches when she arrives home from work. The nurse should suggest that the client perform: a. Tailor sitting b. Leg lifting c. Shoulder circling d. Squatting exercises 12. Which of the following would the nurse in charge do first after observing a 2-cm circle of bright red bleeding on the diaper of a neonate who just had a circumcision? a. Notify the neonates pediatrician immediately b. Check the diaper and circumcision again in 30 minutes c. Secure the diaper tightly to apply pressure on the site d. Apply gently pressure to the site with a sterile gauze pad 13. Which of the following would the nurse Sandra most likely expect to find when assessing a pregnant client with abruption placenta? a. Excessive vaginal bleeding
b. Rigid, boardlike abdomen c. Titanic uterine contractions d. Premature rupture of membranes 14. While the client is in active labor with twins and the cervix is 5 cm dilates, the nurse observes contractions occurring at a rate of every 7 to 8 minutes in a 30-minute period. Which of the following would be the nurses most appropriate action? a. Note the fetal heart rate patterns b. Notify the physician immediately c. Administer oxygen at 6 liters by mask d. Have the client pant-blow during the contractions 15. A client tells the nurse, I think my baby likes to hear me talk to him. When discussing neonates and stimulation with sound, which of the following would the nurse include as a means to elicit the best response? a. High-pitched speech with tonal variations b. Low-pitched speech with a sameness of tone c. Cooing sounds rather than words d. Repeated stimulation with loud sounds 16. A 31-year-old multipara is admitted to the birthing room after initial examination reveals her cervix to be at 8 cm, completely effaced (100 %), and at 0 station. What phase of labor is she in? a. Active phase b. Latent phase c. Expulsive phase d. Transitional phase 17. A pregnant patient asks the nurse Kate if she can take castor oil for her constipation. How should the nurse respond? a. Yes, it produces no adverse effect. b. No, it can initiate premature uterine contractions. c. No, it can promote sodium retention. d. No, it can lead to increased absorption of fat-soluble vitamins. 18. A patient in her 14th week of pregnancy has presented with abdominal cramping and vaginal bleeding for the past 8 hours. She has passed several cloth. What is the primary nursing diagnosis for this patient? a. Knowledge deficit b. Fluid volume deficit c. Anticipatory grieving d. Pain 19. Immediately after a delivery, the nurse-midwife assesses the neonates head for signs of molding. Which factors determine the type of molding? a. Fetal body flexion or extension b. Maternal age, body frame, and weight c. Maternal and paternal ethnic backgrounds d. Maternal parity and gravidity
20. For a patient in active labor, the nurse-midwife plans to use an internal electronic fetal monitoring (EFM) device. What must occur before the internal EFM can be applied? a. The membranes must rupture b. The fetus must be at 0 station c. The cervix must be dilated fully d. The patient must receive anesthesia 21. A primigravida patient is admitted to the labor delivery area. Assessment reveals that she is in early part of the first stage of labor. Her pain is likely to be most intense: a. Around the pelvic girdle b. Around the pelvic girdle and in the upper arms c. Around the pelvic girdle and at the perineum d. At the perineum 22. A female adult patient is taking a progestin-only oral contraceptive, or minipill. Progestin use may increase the patients risk for: a. Endometriosis b. Female hypogonadism c. Premenstrual syndrome d. Tubal or ectopic pregnancy 23. A patient with pregnancy-induced hypertension probably exhibits which of the following symptoms? a. Proteinuria, headaches, vaginal bleeding b. Headaches, double vision, vaginal bleeding c. Proteinuria, headaches, double vision d. Proteinuria, double vision, uterine contractions 24. Because cervical effacement and dilation are not progressing in a patient in labor, Dr. Smith orders I.V. administration of oxytocin (Pitocin). Why must the nurse monitor the patients fluid intake and output closely during oxytocin administration? a. Oxytoxin causes water intoxication b. Oxytocin causes excessive thirst c. Oxytoxin is toxic to the kidneys d. Oxytoxin has a diuretic effect 25. Five hours after birth, a neonate is transferred to the nursery, where the nurse intervenes to prevent hypothermia. What is a common source of radiant heat loss? a. Low room humidity b. Cold weight scale c. Cools incubator walls d. Cool room temperature 26. After administering bethanechol to a patient with urine retention, the nurse in charge monitors the patient for adverse effects. Which is most likely to occur? a. Decreased peristalsis b. Increase heart rate c. Dry mucous membranes d. Nausea and Vomiting
27. The nurse in charge is caring for a patient who is in the first stage of labor. What is the shortest but most difficult part of this stage? a. Active phase b. Complete phase c. Latent phase d. Transitional phase 28. After 3 days of breast-feeding, a postpartal patient reports nipple soreness. To relieve her discomfort, the nurse should suggest that she: a. Apply warm compresses to her nipples just before feedings b. Lubricate her nipples with expressed milk before feeding c. Dry her nipples with a soft towel after feedings d. Apply soap directly to her nipples, and then rinse 29. The nurse is developing a teaching plan for a patient who is 8 weeks pregnant. The nurse should tell the patient that she can expect to feel the fetus move at which time? a. Between 10 and 12 weeks gestation b. Between 16 and 20 weeks gestation c. Between 21 and 23 weeks gestation d. Between 24 and 26 weeks gestation 30. Normal lochial findings in the first 24 hours post-delivery include: a. Bright red blood b. Large clots or tissue fragments c. A foul odor d. The complete absence of lochia
1. Answer A. Endometritis is an infection of the uterine lining and can occur after prolonged rupture of membranes. Endometriosis does not occur after a strong labor and prolonged rupture of membranes. Salpingitis is a tubal infection and could occur if endometritis is not treated. Pelvic thrombophlebitis involves a clot formation but it is not a complication of prolonged rupture of membranes. 2. Answer B. Before amniocentesis, a routine ultrasound is valuable in locating the placenta, locating a pool of amniotic fluid, and showing the physician where to insert the needle. Color Doppler imaging ultrasonography identifies blood flow through the umbilical cord. A routine ultrasound does not accomplish this. 3. Answer B. Protamine sulfate is a heparin antagonist given intravenously to counteract bleeding complications cause by heparin overdose. 4. Answer D. While caring for an infant receiving phototherapy for treatment of jaundice, vital signs are checked every 2 to 4 hours because hyperthermia can occur due to the phototherapy lights. 5. Answer D. A bilateral pudental block is used for vaginal deliveries to relieve pain primarily in the perineum and vagina. Pudental block anesthesia is adequate for episiotomy and its repair.
6. Answer A. Eating dry crackers before arising can assist in decreasing the common discomfort of nausea and vomiting. Avoiding strong food odors and eating a high-protein snack before bedtime can also help. 7. Answer C. Beginning after completion of the taking-in phase, the taking-hold phase lasts about 10 days. During this phase, the client is concerned with her need to resume control of all facets of her life in a competent manner. At this time, she is ready to learn self-care and infant care skills. 8. Answer A. Treatment of partial placenta previa includes bed rest, hydration, and careful monitoring of the clients bleeding. 9. Answer C. Prevention of breast engorgement is key. The best technique is to empty the breast regularly with feeding. Engorgement is less likely when the mother and neonate are together, as in single room maternity care continuous rooming in, because nursing can be done conveniently to meet the neonates and mothers needs. 10. Answer A. The Moro, or startle, reflex occurs when the neonate responds to stimuli by extending the arms, hands open, and then moving the arms in an embracing motion. The Moro reflex, present at birth, disappears at about age 3 months. 11. Answer A. Tailor sitting is an excellent exercise that helps to strengthen the clientsback muscles and also prepares the client for the process of labor. The client should be encouraged to rest periodically during the day and avoid standing or sitting in one position for a long time. 12. Answer D. If bleeding occurs after circumcision, the nurse should first apply gently pressure on the area with sterile gauze. Bleeding is not common but requires attention when it occurs. 13. Answer B. The most common assessment finding in a client with abruption placenta is a rigid or boardlike abdomen. Pain, usually reported as a sharp stabbing sensation high in the uterine fundus with the initial separation, also is common. 14. Answer B. The nurse should contact the physician immediately because the client is most likely experiencing hypotonic uterine contractions. These contractions tend to be painful but ineffective. The usual treatment is oxytocin augmentation, unless cephalopelvic disproportion exists. 15. Answer A. Providing stimulation and speaking to neonates is important. Some authorities believe that speech is the most important type of sensory stimulation for a neonate. Neonates respond best to speech with tonal variations and a high-pitched voice. A neonate can hear all sound louder than about 55 decibels. 16. Answer D. The transitional phase of labor extends from 8 to 10 cm; it is the shortest but most difficult and intense for the patient. The latent phase extends from 0 to 3 cm; it is mild in nature. The active phase extends form 4 to 7 cm; it is moderate for the patient. The expulsive phase begins immediately after the birth and ends with separation and expulsion of the placenta. 17. Answer B. Castor oil can initiate premature uterine contractions in pregnant women. It also can produce other adverse effects, but it does not promote sodium retention. Castor oils is not known to increase absorption of fat-soluble vitamins, although laxatives in general may decrease absorption if intestinal motility is increased.
18. Answer B. If bleeding and cloth are excessive, this patient may become hypovolemic. Pad count should be instituted. Although the other diagnoses are applicable to this patient, they are not the primary diagnosis. 19. Answer A. Fetal attitudethe overall degree of body flexion or extensiondetermines the type of molding in the head a neonate. Molding is not influence by maternal age, body frame, weight, parity, or gravidity or by maternal and paternal ethnic backgrounds. 20. Answer A. Internal EFM can be applied only after the patients membranes have ruptures, when the fetus is at least at the -1 station, and when the cervix is dilated at least 2 cm. although the patient may receive anesthesia, it is not required before application of an internal EFM device. 21. Answer A.During most of the first stage of labor, pain centers around the pelvic girdle. During the late part of this stage and the early part of the second stage, pain spreads to the upper legs and perineum. During the late part of the second stage and during childbirth, intense pain occurs at the perineum. Upper arm pain is not common during ant stage of labor. 22. Answer D. Women taking the minipill have a higher incidence of tubal and ectopic pregnancies, possibly because progestin slows ovum transport through the fallopian tubes. Endometriosis, female hypogonadism, and premenstrual syndrome are not associated with progestin-only oral contraceptives. 23. Answer C. A patient with pregnancy-induced hypertension complains of headache, double vision, and sudden weight gain. A urine specimen reveals proteinuria. Vaginal bleeding and uterine contractions are not associated with pregnancy-induces hypertension. 24. Answer A. The nurse should monitor fluid intake and output because prolonged oxytoxin infusion may cause severe water intoxication, leading to seizures, coma, and death. Excessive thirst results form the work of labor and limited oral fluid intakenot oxytoxin. Oxytoxin has no nephrotoxic or diuretic effects. In fact, it produces an antidiuretic effect. 25. Answer C. Common source of radiant heat loss includes cool incubator walls and windows. Low room humidity promotes evaporative heat loss. When the skin directly contacts a cooler object, such as a cold weight scale, conductive heat loss may occur. A cool room temperature may lead to convective heat loss. 26. Answer D. Bethanechol will increase GI motility, which may cause nausea, belching, vomiting, intestinal cramps, and diarrhea. Peristalsis is increased rather than decreased. With high doses of bethanechol, cardiovascular responses may include vasodilation, decreased cardiac rate, and decreased force of cardiac contraction, which may cause hypotension. Salivation or sweating may gently increase. 27. Answer D. The transitional phase, which lasts 1 to 3 hours, is the shortest but most difficult part of the first stage of labor. This phase is characterized by intense uterine contractions that occur every 1 to 2 minutes and last 45 to 90 seconds. The active phase lasts 4 to 6 hours; it is characterized by contractions that starts out moderately intense, grow stronger, and last about 60 seconds. The complete phase occurs during the second, not first, stage of labor. The latent phase lasts 5 to 8 hours and is marked by mild, short, irregular contractions.
28. Answer B. Measures that help relieve nipple soreness in a breast-feeding patient include lubrication the nipples with a few drops of expressed milk before feedings, applying ice compresses just before feeding, letting the nipples air dry after feedings, and avoiding the use of soap on the nipples. 29. Answer B. A pregnant woman usually can detect fetal movement (quickening) between 16 and 20 weeks gestation. Before 16 weeks, the fetus is not developed enough for the woman to detect movement. After 20 weeks, the fetus continues to gain weight steadily, the lungs start to produce surfactant, the brain is grossly formed, and myelination of the spinal cord begins. 30. Answer A. Lochia should never contain large clots, tissue fragments, or membranes. A foul odor may signal infection, as may absence of lochia.
Myrna, whos 4 months pregnant asks the nurse how much and what type of exercise she should get during pregnancy. How should nurse Maricel counsel her? a. b. c. d. 2. a. b. c. d. 3. a. b. c. d. 4. a. b. c. d. 5. Try high-intensity aerobics, but limit sessions to 15 minutes daily. Perform gentle back-lying exercises for 30 minutes daily. Walk briskly for 10 to 15 minutes daily, and gradually increase this time. Exercise to raise the heart rate above 140 beats/minute for 20 minutes daily. Linda, whos 37 weeks pregnant comes to the clinic for a prenatal checkup. To assess the clients Are you planning to have epidural anesthesia? Have you begun prenatal classes? What changes have you made at home to get ready for the baby? Can you tell me about the meals you typically eat each day? Nurse Tanya is aware that the best place to detect fetal heart sounds for a client in the first trimester Above the symphysis pubis Below the symphysis pubis Above the umbilicus At the umbilicus Lovelyn, asks the nurse whether she can take castor oil for her constipation. How should the nurse Yes, it produces no adverse effects. No, it can initiate premature uterine contractions. No, it can promote sodium retention. No, it can lead to increased absorption of fat-soluble vitamins. A client at 35 weeks gestation complains of severe abdominal pain and passing clots. The clients
preparation for parenting, nurse Kim might ask which question?
of pregnancy?
respond?
vital signs are blood pressure 150/100 mm Hg, heart rate 95 beats/minute, respiratory rate 25
breaths/minute, and fetal heart tones 160 beats/minute. Nurse Nikki must determine the cause of the bleeding and respond appropriately to this emergency. Which of the following should the nurse do first? a. b. c. d. 6. Examine the vagina to determine whether her client is in labor Assess the location and consistency of the uterus Perform an ultrasound to determine placental placement Prepare for immediate delivery When assessing a client during her first prenatal visit, nurse Lucy discovers that the client had a
reduction mammoplasty. The mother indicates she wants to breast-feed. What information should the nurse give to this mother regarding breast-feeding success? a. b. c. d. 7. a. b. c. d. 8. Its contraindicated for you to breast-feed following this type of surgery. I support your commitment; however, you may have to supplement each feeding with formula. You should check with your surgeon to determine whether breast-feeding would be possible. You should be able to breast-feed without difficulty. When questioned, Alma admits she sometimes has several glasses of wine with dinner. Her alcohol Alcohol addiction Anencephaly Down syndrome Learning disability Nurse Helen has a client at 30 weeks gestation who has tested positive for the human
consumption puts her fetus at risk for which condition?
immunodeficiency virus (HIV). What should the nurse tell the client when she says that she wants to breast-feed her baby? a. b. c. d. 9. a. b. c. d. 10. a. b. c. d. Encourage breast-feeding so that she can get her rest and get healthier Encourage breast-feeding because its healthier for the baby Encourage breast-feeding to facilitate bonding Discourage breast-feeding because HIV can be transmitted through breast milk During each prenatal checkup, nurse Paul obtains the clients weight and blood pressure and Evaluating the client for edema Measuring the clients hemoglobin (Hb) level Obtaining pelvic measurements Determining the clients Rh factor Which of the following instructions should nurse Dan give to a client whos 26 weeks pregnant and Encourage her to increase her intake of roughage and to drink at least six glasses of water per day. Tell her to ask her caregiver for a mild laxative. Suggest the use of an over-the-counter stool softener. Tell her to go to the evaluation unit because constipation may cause contractions.
measures fundal height. What is another essential part of each prenatal checkup?
complains of constipation?
11. a. b. c. d. 12. a. b. c. d. 13.
During the 6th month of pregnancy, Gail reports intermittent earaches and a constant feeling of A serious neurologic disorder Eustachian tube vascularization Increasing progesterone levels An ear infection Malou, 2 months pregnant, has hyperemesis gravidarum. Which expected outcome is most Client will accept the pregnancy and stop vomiting. Client will gain weight according to the expected pattern for pregnancy. Client will remain hospitalized for the duration of pregnancy to relieve stress. Client will exhibit uterine growth within the expected norms for gestational age. When assessing a pregnant client with diabetes mellitus, nurse Gio stays alert for signs and
fullness in the ears. What is the most likely cause of these symptoms?
appropriate for her?
symptoms of a vaginal or urinary tract infection (UTI). Which condition makes this client more susceptible to such infections? a. b. c. d. 14. Electrolyte imbalances Decreased insulin needs Hypoglycemia Glycosuria Josephine, 11 weeks pregnant, is admitted to the facility with hyperemesis gravidarum. She tells the
nurse she has never known anyone who had such severe morning sickness. The nurse understands that hyperemesis gravidarum results from: a. b. c. d. 15. a. b. c. d. 16. a. b. c. d. a neurologic disorder. inadequate nutrition. an unknown cause. hemolysis of fetal red blood cells (RBCs). A client has come to the clinic for her first prenatal visit. Nurse Alex should include which of the During the first 3 months, avoid all medications except ones prescribed by your caregiver. Medications that are available over the counter are safe for you to use, even early on. All medications are safe after youve reached the 5th month of pregnancy. Consult with your health care provider before taking any medications. A pregnant client asks how she can best prepare her 3-year-old son for the upcoming birth of a Tell your son about the childbirth about 1 month before your due date. Reassure your son that nothing is going to change. Reprimand your son if he displays immature behavior. Involve your son in planning and preparing for a sibling.
following statements about using drugs safely during pregnancy in her teaching?
sibling. Nurse Lou should make which suggestion?
17. a. b. c. d. 18. a. b. c. d. 19. a. b. c. d. 20.
Nurse Cathy is caring for a 16-year-old pregnant client. The client is taking an iron supplement. A glass of milk A cup of hot tea A liquid antacid A glass of orange juice Nurse Rey is using Doppler ultrasound to assess a pregnant woman. When should the nurse expect 7 weeks 11 weeks 17 weeks 21 weeks Nurse Edith is caring for a client whos on ritodrine therapy to halt premature labor. What condition Hypoglycemia Crackles Bradycardia Hyperkalemia Noemi, a newly pregnant woman tells the nurse that she hasnt been taking herprenatal
What should this client drink to increase the absorption of iron?
to hear fetal heart tones?
indicates an adverse reaction to ritodrine therapy?
vitamins because they make her nauseated. In addition to telling the client how important taking the vitamins are, the nurse should advise her to: a. b. c. d. 21. a. b. c. d. 22. a. b. c. d. switch brands. take the vitamin on a full stomach. take the vitamin with orange juice for better absorption. take the vitamin first thing in the morning. A client is scheduled for amniocentesis. When preparing her for the procedure, nurse Vince should Ask her to void. Instruct her to drink 1 L of fluid. Prepare her for I.V. anesthesia. Place her on her left side. After determining that a pregnant client is Rh-negative, Dr. Smith orders an indirect Coombs test. To determine the fetal blood Rh factor To determine the maternal blood Rh factor To detect maternal antibodies against fetal Rh-negative factor To detect maternal antibodies against fetal Rh-positive factor
do which of the following?
What is the purpose of performing this test in a pregnant client?
23. a. b. c. d. 24. a. b. c. d. 25. a. b. c. d.
During a routine prenatal visit, a pregnant client reports heartburn. To minimize her discomfort, Eat small, frequent meals. Limit fluid intake sharply. Drink more citrus juice. Take sodium bicarbonate. A pregnant client asks nurse Mary about the percentage of congenital anomalies caused by drug 1% 10% 20% 60% Sandy, age 39, visits the nurse practitioner for a regular prenatal check-up. Shes 32 weeks pregnancy-induced hypertension (PIH). iron deficiency anemia. cephalopelvic disproportion. sexually transmitted diseases (STDs).
nurse Faith should include which suggestion in the plan of care?
exposure. How should the nurse respond?
pregnant. When assessing her, the nurse should stay especially alert for signs and symptoms of:
Answer C. Taking brisk walks is one of the easiest ways to exercise during pregnancy. The client should begin by walking slowly for 10 to 15 minutes per day and increase gradually to a comfortable speed and a duration of 30 to 45 minutes per day. The pregnant client should avoid high-intensity aerobics because these greatly increase oxygen consumption; pregnancy itself not only increases oxygen consumption but reduces oxygen reserve. Starting from the 4th month of pregnancy, the client should avoid back-lying exercises because in this position the enlarged uterus may reduce blood flow through the vena cava. The client should avoid exercises that raise the heart rate over 140 beats/minute because the cardiovascular system already is stressed by increased blood volume during pregnancy. 2. Answer C. During the third trimester, the pregnant client typically perceives the fetus as a separate being. To verify that this has occurred, the nurse should ask whether she has made appropriate changes at home such as obtaining infant supplies and equipment. The type of anesthesia planned doesnt reflect the clients preparation for parenting. The client should have begun prenatal classes earlier in the pregnancy. The nurse should have obtained dietary information during the first trimester to give the client time to make any necessary changes. 3. Answer A. In the first trimester, fetal heart sounds are loudest in the area of maximum intensity, just above the clients symphysis pubis at the midline. Fetal heart sounds arent heard as well in the other locations. 4. Answer B. Castor oil can initiate premature uterine contractions in pregnant women. It also can produce other adverse effects, but it doesnt promote sodium retention. Castor oil isnt known to increase
absorption of fat-soluble vitamins, although laxatives can decrease absorption if intestinal motility is increased. 5. Answer B. The nurse must determine whether placenta previa or abruptio placentae is the problem. (Fifty percent of all clients with hypertension will develop abruptio placenta.) In this case, the presenting symptoms are highly suggestive of an abruption, so the nurse must determine the level of the uterus and mark that level on the clients abdomen. She must also check the consistency of the uterus; a uterus that is filling with blood because the placenta has detached early is rigid. Bleeding from a placental previa is usually painless. A vaginal examination is contraindicated in the presence of bleeding. Most nurses havent been taught how to perform an ultrasound. If the client has a placental abruption, birth will most likely be by cesarean section. 6. Answer B. Recent breast reduction surgeries are done in a way to protect the milk sacs and ducts, so breast-feeding after surgery is possible. Still, its good to check with the surgeon to determine what breast reduction procedure was done. There is the possibility that reduction surgery may have decreased the mothers ability to meet all of her babys nutritional needs, and some supplemental feeding may be required. Preparing the mother for this possibility is extremely important because the clients psychological adaptation to mothering may be dependent on how successfully she breast-feeds. 7. Answer D. Maternal alcohol use during pregnancy may cause fetal and neonatal central nervous system deficits such as learning disabilities. It also may lead to characteristic physical anomalies and growth retardation. Maternal alcohol use doesnt cause alcohol addiction in the fetus or neonate. Anencephaly occurs when the cranial end of the neural tube fails to fuse before the 26th day of gestation; this condition isnt related to maternal alcohol use. Down syndrome results from a chromosomal disorder. 8. 9. Answer: D. Transmission of HIV can occur through breast milk, so breast-feeding should be Answer A. During each prenatal checkup, the nurse should evaluate the client for edema, a possible discouraged in this case. sign of pregnancy-induced hypertension (PIH). If edema exists, the nurse should assess for high blood pressure and proteinuria other signs of PIH. Hb is measured during the first prenatal visit and again at 24 to 28 weeks gestation and at 36 weeks gestation. The pelvis is measured and the Rh factor determined during the first prenatal visit. 10. Answer A. The best instruction is to encourage the client to increase her intake of high-fiber foods (roughage) and to drink at least six glasses of water per day. Mild laxatives and stool softeners may be needed, but dietary changes should be tried first. Straining during defecation and diarrhea can stimulate uterine contractions, but telling the client to go to the evaluation unit doesnt address her concern. 11. Answer B. During pregnancy, increasing levels of estrogen not progesterone cause vascularization of the eustachian tubes, leading to such problems as earaches, impaired hearing, and a constant feeling of fullness in the ears. Nothing in the question implies that the client has a serious neurologic disorder or an ear infection. 12. Answer D. For a client with hyperemesis gravidarum, the goal of nursing care is to achieve optimal fetal growth, which can be evaluated by monitoring uterine growth through fundal height
assessment. The nurse shouldnt assume that excessive vomiting signifies the client doesnt accept the pregnancy. Clients with hyperemesis gravidarum rarely gain weight according to the expected pattern. They may be hospitalized briefly to regulate fluid and electrolyte status, but they dont require hospitalization for the duration of pregnancy. In fact, hospitalization may add to the stress of pregnancy by causing family separation and financial concerns. 13. Answer D. Glycosuria predisposes the pregnant diabetic client to vaginal infections (especially Candida vaginitis) and UTIs, because the hormonal changes of pregnancy affect vaginal pH and the bladder. Electrolyte imbalances and hypoglycemia arent associated with vaginal infections or UTIs. Insulin requirements may decrease in early pregnancy; however, as the clients food intake improves and maternal and fetal glycogen stores increase, insulin requirements also rise. 14. Answer C. The cause of hyperemesis gravidarum isnt known. However, etiologic theories implicate hormonal alterations and allergic or psychosomatic conditions. No evidence suggests that hyperemesis gravidarum results from a neurologic disorder, inadequate nutrition, or hemolysis of fetal RBCs. 15. Answer D. Because all medications can be potentially harmful to the growing fetus, telling the client to consult with her health care provider before taking any medications is the best teaching. The client needs to understand that any medication taken at any time during pregnancy can be teratogenic. 16. Answer D. Being involved in the pregnancy helps reinforce a childs position in the family and minimizes feelings of neglect and abandonment. Telling the child about the childbirth only 1 month before the due date wouldnt allow enough time to prepare him for the sibling and would prevent him from conceptualizing the passage of time. Reassuring him that nothing will change would be misleading; instead, the parents should discuss which aspects of family life will be changed by the upcoming birth and which will remain the same. Parents should reward mature behavior and ignore immature behavior. 17. 18. 19. Answer D. Increasing vitamin C enhances the absorption of iron supplements. Taking an iron Answer B. Using Doppler ultrasound, fetal heart tones may be heard as early as the 11th week of Answer B. Use of ritodrine can lead to pulmonary edema. Therefore, the nurse should assess for supplement with milk, tea, or an antacid reduces the absorption of iron. pregnancy. Using a stethoscope, fetal heart tones may be heard between 17 and 20 weeks of gestation. crackles and dyspnea. Blood glucose levels may temporarily rise, not fall, with ritodrine. Ritodrine may cause tachycardia, not bradycardia. Ritodrine may also cause hypokalemia, not hyperkalemia. 20. Answer B. Prenatal vitamins commonly cause nausea and taking them on a full stomach may curb this. Switching brands may not be helpful and may be more costly. Orange juice tends to make pregnant women nauseated. The vitamins may be taken at night, rather than in the morning, to reduce nausea. 21. Answer A. To prepare a client for amniocentesis, the nurse should ask her to empty her bladder to reduce the risk of bladder perforation. Before transabdominal ultrasound, the nurse may instruct the client to drink 1 L of fluid to fill the bladder (unless ultrasound is done before amniocentesis to locate the placenta). I.V. anesthesia isnt given for amniocentesis. The client should be supine during the procedure; afterward, she should be placed on her left side to avoid supine hypotension, promote venous return, and ensure adequate cardiac output.
22.
Answer D. The indirect Coombs test measures the number of antibodies against fetal Rh-positive
factor in maternal blood. The maternal blood Rh factor is determined before the indirect Coombs test is done. No maternal antibodies against fetal Rh-negative factor exist. 23. Answer A. To relieve heartburn, the nurse should advise a pregnant client to eat smaller meals at shorter intervals; drink six to eight 8-oz glasses of fluid daily to minimize regurgitation and reflux of stomach contents; and avoid citrus juice, which may act as a gastric irritant and worsen heartburn, and sodium bicarbonate, which may disrupt the bodys sodium-potassium balance. 24. 25. Answer A. Drug exposure causes 1% of congenital anomalies. Answer A. Mature pregnant clients are at increased risk for PIH and are more likely to require
cesarean delivery. Also, their fetuses and neonates have a higher mortality and a higher incidence of trisomies. Iron deficiency anemia, cephalopelvic disproportion, and STDs may occur in any client regardless of age.
Potrebbero piacerti anche
- Practice Exam 2 OB NursingDocumento21 paginePractice Exam 2 OB NursingSpurgis Rickard90% (21)
- Maternity Nursing EXAM REVIEWDocumento8 pagineMaternity Nursing EXAM REVIEWJulienne Sanchez-Salazar100% (2)
- ATI Maternal Newborn Chapter 1-ContraceptionDocumento23 pagineATI Maternal Newborn Chapter 1-ContraceptionVin Lorenzo Campbell100% (4)
- Maternity Nursing ObDocumento11 pagineMaternity Nursing ObMayls Sevilla Calizo74% (19)
- Maternal and Child Health Pracice Test 1-2-3Documento84 pagineMaternal and Child Health Pracice Test 1-2-3chuppepay100% (1)
- Obstetrics Nursing QuestionsDocumento11 pagineObstetrics Nursing Questionsurangel2214Nessuna valutazione finora
- Practice Test Pediatric Nursing 100 ItemsDocumento10 paginePractice Test Pediatric Nursing 100 ItemsannjelynespeletaNessuna valutazione finora
- Nurseslabs Maternity Nursing Q OnlyDocumento6 pagineNurseslabs Maternity Nursing Q OnlyCharles Malcolm Dalugdug100% (1)
- Maternal in ChildDocumento15 pagineMaternal in ChildRenalyn VillasencioNessuna valutazione finora
- OB Exam 1Documento25 pagineOB Exam 1pauchanmnl100% (1)
- Maternal Practice Test 4Documento14 pagineMaternal Practice Test 4Cj AguilarNessuna valutazione finora
- Practice Test IIDocumento18 paginePractice Test IIbeautifulme031690100% (1)
- 1 Maternal & ChildDocumento14 pagine1 Maternal & ChildYa Mei Li100% (1)
- MCN 1Documento5 pagineMCN 1Aijem RyanNessuna valutazione finora
- Comprehensive Exam NCM 350Documento23 pagineComprehensive Exam NCM 350JustJ ThingsNessuna valutazione finora
- Maternal and Child Health Nursing 2 (30 Items)Documento11 pagineMaternal and Child Health Nursing 2 (30 Items)hasan ahmdNessuna valutazione finora
- DrillsDocumento18 pagineDrillsJean CuentaNessuna valutazione finora
- Practice Test IIDocumento18 paginePractice Test IIShella Marie Usquisa100% (3)
- Local Media6484230877636161591Documento22 pagineLocal Media6484230877636161591AZ BaldovidonaNessuna valutazione finora
- Maternal and Child Nursing 3Documento15 pagineMaternal and Child Nursing 3gellie100% (1)
- 4 Ob ExamDocumento9 pagine4 Ob ExamKim Ramos100% (1)
- NCM 101 Obstetrics ExamDocumento14 pagineNCM 101 Obstetrics ExamLouie John Abila100% (1)
- Ob 1Documento13 pagineOb 1iandame100% (1)
- Ob Set A and B QuesDocumento17 pagineOb Set A and B QuesBok Delos SantosNessuna valutazione finora
- Ob ExamDocumento8 pagineOb ExamRamones JokerNessuna valutazione finora
- 100 Item ObstetricsDocumento28 pagine100 Item ObstetricsTon Ton100% (2)
- OB Midwifery Set 1 PDFDocumento9 pagineOB Midwifery Set 1 PDFSquidward Tentacles100% (1)
- Obstetrics Nursing QuestionsDocumento13 pagineObstetrics Nursing Questionsicy43150% (2)
- 100 Items OB Questions byDocumento17 pagine100 Items OB Questions byPetrovich Tamag100% (1)
- Maternal and Child HealthDocumento72 pagineMaternal and Child Healthannamargie07100% (3)
- Sec. 3C - 1 - OB Questions (Answer Key) - BrendaDocumento20 pagineSec. 3C - 1 - OB Questions (Answer Key) - Brendacididok84Nessuna valutazione finora
- MCN Post Test IIDocumento14 pagineMCN Post Test IIquidditch07Nessuna valutazione finora
- Post-Partum Review Questions - Handout 2 With Answers /rationalesDocumento9 paginePost-Partum Review Questions - Handout 2 With Answers /rationalesnkuligowski100% (2)
- MCN - P2 Post Test (Reviewer)Documento3 pagineMCN - P2 Post Test (Reviewer)cianixNessuna valutazione finora
- ObstetricsDocumento19 pagineObstetricsMoon Boo ChanNessuna valutazione finora
- A4.Fundamentals - 25item With RationaleDocumento4 pagineA4.Fundamentals - 25item With RationaleBlardy Falking You Benchod BlardyNessuna valutazione finora
- Ob Post PartumDocumento25 pagineOb Post PartumYa Mei LiNessuna valutazione finora
- Obsterical Nclex QuesDocumento14 pagineObsterical Nclex Quesms_m_r1082Nessuna valutazione finora
- Maternal and ChildDocumento204 pagineMaternal and Childmj CanilangNessuna valutazione finora
- Maternal and Child Health Nursing Exam Drill Aug 2011Documento4 pagineMaternal and Child Health Nursing Exam Drill Aug 2011nikko042790100% (1)
- Gynecology Test QuestionsDocumento6 pagineGynecology Test Questionsdhodejun lizhaldeNessuna valutazione finora
- Maternal and Child Nursing Sample ExamDocumento8 pagineMaternal and Child Nursing Sample Examteabagman0% (1)
- MCN DX Test 2010Documento9 pagineMCN DX Test 2010jjbautista100% (2)
- Abnormal OB, DanielDocumento7 pagineAbnormal OB, DanielBhebz C. GarolNessuna valutazione finora
- OB Exam 11 A AnswerDocumento14 pagineOB Exam 11 A AnswerDianeNessuna valutazione finora
- OBDocumento4 pagineOBCharlie Cotoner FalgueraNessuna valutazione finora
- FHCDocumento8 pagineFHCAmiel Francisco ReyesNessuna valutazione finora
- 100 Items OBDocumento15 pagine100 Items OBKajou MichiyoNessuna valutazione finora
- Nurse QuizDocumento21 pagineNurse QuizOleOhhNessuna valutazione finora
- College of Nursing: Batangas State UniversityDocumento11 pagineCollege of Nursing: Batangas State UniversityArcon AlvarNessuna valutazione finora
- Haad Mle FundaDocumento20 pagineHaad Mle FundaGreggy Francisco LaraNessuna valutazione finora
- OB Answer KeyDocumento23 pagineOB Answer Keyicy431Nessuna valutazione finora
- Maternity NursingDocumento24 pagineMaternity NursingJen Arcillas Tuble - Iledan100% (1)
- Obstetrics OBDocumento65 pagineObstetrics OBVicviclookTheking100% (1)
- ExamDocumento33 pagineExamRhiza Pagdanganan100% (1)
- OB-GYN Conceptual ExamDocumento21 pagineOB-GYN Conceptual Examquidditch07100% (5)
- Maternal and Child PreboardDocumento17 pagineMaternal and Child PreboardMichelle GambolNessuna valutazione finora
- MCNDocumento4 pagineMCNAijem RyanNessuna valutazione finora
- Pathological Obstetrics, Basic Family Planning and Care of InfantsDocumento96 paginePathological Obstetrics, Basic Family Planning and Care of InfantsScarlet AmodiaNessuna valutazione finora
- Hyperemesis Gravidarum AND Wernicke'S Encephalopathy SyndromeDocumento18 pagineHyperemesis Gravidarum AND Wernicke'S Encephalopathy SyndromeRaden Atika PermadiNessuna valutazione finora
- Nausea and Vomiting of PregnancyDocumento8 pagineNausea and Vomiting of PregnancycintacitraNessuna valutazione finora
- Nausea & Vomiting in PregnancyDocumento8 pagineNausea & Vomiting in PregnancyStanNessuna valutazione finora
- Hyperemesis Gravidarum, With Metabolic DerangementDocumento5 pagineHyperemesis Gravidarum, With Metabolic DerangementmethuselahchintalaNessuna valutazione finora
- Maternal Test Questions 3Documento6 pagineMaternal Test Questions 3dhodejun lizhaldeNessuna valutazione finora
- OB Quiz MidtermsDocumento13 pagineOB Quiz MidtermsJhay-r BaldoNessuna valutazione finora
- HT On Hyperemesis GravidumDocumento15 pagineHT On Hyperemesis GravidumPriyaNessuna valutazione finora
- Hyperemesis GravidarumDocumento34 pagineHyperemesis GravidarumSiti Nurhayati100% (1)
- Jurnal Hiperemesis GravidarumDocumento13 pagineJurnal Hiperemesis GravidarumfauziyahabidahNessuna valutazione finora
- Hyperemesis GravidarumDocumento5 pagineHyperemesis GravidarumsalamredNessuna valutazione finora
- Maternal and Child Healthe Nursing MCQ 6Documento18 pagineMaternal and Child Healthe Nursing MCQ 6shanika100% (1)
- Hyperemesis Gravidarum 1Documento26 pagineHyperemesis Gravidarum 1Jas Castro Jovero100% (3)
- 4.hyperemesis & Amniotic Fluid DisorderDocumento53 pagine4.hyperemesis & Amniotic Fluid DisorderjosephNessuna valutazione finora
- Postpartum Clinical QuizDocumento6 paginePostpartum Clinical QuizAmy100% (1)
- Causes of Vomiting and How To Treat in AdultsDocumento8 pagineCauses of Vomiting and How To Treat in Adultsto van quyenNessuna valutazione finora
- HYPEREMESIS GRAVIDARUM GT 69 NotesDocumento6 pagineHYPEREMESIS GRAVIDARUM GT 69 NotesFara WakeshimaNessuna valutazione finora
- mc2 p1 ExamDocumento12 paginemc2 p1 Examjovan teopizNessuna valutazione finora
- DrillsDocumento18 pagineDrillsJean CuentaNessuna valutazione finora
- Hepatic Disease in PregnancyDocumento37 pagineHepatic Disease in PregnancyElisha Joshi100% (1)
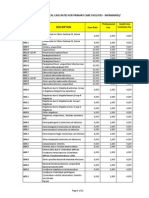
- PhilHealth Circular No. 0035, s.2013 Annex 5 List of Medical Case Rates For Primary Care FacilitiesDocumento22 paginePhilHealth Circular No. 0035, s.2013 Annex 5 List of Medical Case Rates For Primary Care FacilitiesChrysanthus HerreraNessuna valutazione finora
- Cannabinoid Hyperemesis Syndrome CHS 2506 PILDocumento3 pagineCannabinoid Hyperemesis Syndrome CHS 2506 PILH PsychNessuna valutazione finora
- Hyperemesis GravidarumDocumento10 pagineHyperemesis GravidarumFarxan Da Napolian BwoyNessuna valutazione finora
- Algoritma Tatalaksana Hiperemesis Gravidarum, RCOG16Documento2 pagineAlgoritma Tatalaksana Hiperemesis Gravidarum, RCOG16rayyanzubaidi100% (1)
- Abnormal PregnancyDocumento179 pagineAbnormal PregnancyMilkii Du NikusNessuna valutazione finora
- Nausea & VomitingDocumento20 pagineNausea & VomitingBrendel Lyn AcordonNessuna valutazione finora
- Mega Nerv FaDocumento5 pagineMega Nerv FaFloid FernandezNessuna valutazione finora
- Sas 5Documento9 pagineSas 5Leaflor Ann ManghihilotNessuna valutazione finora
- TPN and Pregnancy: Related To Hyperemesis GravidarumDocumento37 pagineTPN and Pregnancy: Related To Hyperemesis Gravidarumapi-319236078Nessuna valutazione finora