Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
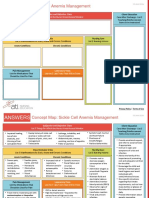
CHF Concept Map
Caricato da
LisaSanders99Descrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
CHF Concept Map
Caricato da
LisaSanders99Copyright:
Formati disponibili
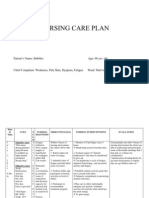
PATIENT INFORMATION Name: Arthur Jackson 73 y. o.
Male Admitting DX: CHF and Uncontrolled A-Fib Medical HX: MI, 4 vessel CABG, Type II DM, HTN, Gout, Hiatal Hernia, A-Fib, Enlarged Prostate Admit Date: 09/09/2011
Diagnostic Test Results: CXR: Reveals moderate pulmonary vascular congestion, cardiomegaly, no signs of atelectasis or infiltrate noted EKG: Atrial Fibrillation ventricular rate 124 no ischemic changes or ectopy noted ECHOCARDIOGRAM: Reveals normal valvular function, irregular heart rhythm, increased volume in L ventricle, Ejection fraction 45%, no clots seen, TEE recommended for further evaluation DUPLEX ULTRASOUND: No Clots noted bilaterally, bilateral popliteal arteries have decreased blood flow
Medications: Lisinopril 5mg PO BID Digoxin 0.125mg PO Daily Coumadin Dosage dependent upon current INR values Lasix 40mg IV BID K-DUR 20 mEq Daily Proscar 5mg daily Glucophage 1000mg PO BID Protonix 40mg IV Daily Coreg 12.5mg BID
Vital Signs BP 188/111 P 122 irregular R 28 labored O2 Sat 92% on RA
T 97.6
Diet: 1800 ADA, Low Sodium 1500ml / 24 hours fluid restriction STRICT I&Os
Abnormal Lab Results: PLT 100,000 (Norm 150,000-450,000) MCH 31.2 (Norm 32-36) BUN 55 (Norm 8-21) Creatinine 1.8 (Norm 0.6-1.2) Digoxin 2.3 (Norm ) PT 17.8 (Norm 11-15 sec X 2-2.5) INR 1.7 (Norm 1 Coumadin 2-3) PTT 38.4 (Norm 60-70 sec) Troponin 0.89 (>0.5 is critical) Myoglobin 23 (Norm 0-2.5) BNP 1385 (Norm <100) UA pending
Patient Goal Get released from the hospital Evaluation Patient was not discharged during shift so the goal has not been reached yet. Continue with current nursing plan.
#1 Decreased Cardiac Output R/T A-Fib AEB irregular heart rate GOAL: The patient will verbalize the S/S of A-Fib and the importance of Digoxin and Coumadin prior to discharge INTERVENTIONS: Assess Blood Pressure and Heart Rate monitor Labs (PT and INR Digoxin) A sudden change in BP can indicated a deterioration in the patients condition; The heart rate is an indication of the cardiac output and the degree to which the body will be oxygenated; Labs will show therapeutic levels of the medications Give Medication: Coumadin, and Digoxin and teach the patient about the importance of taking as its prescribed Coumadin is to help prevent blood clots as a result of A-Fib Digoxin will help improve the cardiac output by increasing the contractility of the heart By teaching the patient each time the medication is administered the importance of the medications are reinforced repeatedly Elevate Legs for 15 minutes every hour This will help with venous return and keep the blood from pooling in the legs EVALUATION: BP decreased slightly 160/90; HR 89; PT and INR are not within therapeutic ranges; Digoxin level is high- doctor was notified and said to continue administering the medication. The patients legs were elevated 15 min Q hour and the patient tolerated it well. ADLs were clustered to decrease the cardiac demand. GOAL EVALUATION: Continue working on this goal until the patient is able to verbalize the importance of taking his medications as prescribed
#2 Excess Fluid Volume R/T Heart failure AEB Weight gain of 27lbs and crackles in the lungs GOAL: Patient will have a total fluid intake of 1500ml/24 and sodium intake of less than 2g INTERVENTIONS: Assess Lung sounds, SaO2, I/Os, and weight A change in lung sounds can indicate either an increase or decrease in fluid volume in a CHF patient; The SaO2 will show the amount of oxygen that is circulating in the blood and the level at which the tissues are receiving O2; a sudden weight gain can indicate fluid retention; CHF patients need to monitor I/Os to ensure there isnt a fluid over load. Give Medication: Lasix and K-DUR; teach the importance of taking Lasix and a potassium supplement when directed Lasix is a diuretic that works at the loop of Henle it is very important to monitor K+ levels and take potassium as needed, because when a patient is also taking Digoxin hypokalemia can lead to dig toxicity Provide low sodium diet along with a daily intake <2g Sodium is directly related to water retention and when a patient is retaining too much fluid it is important to maintain a low sodium diet. EVALUATION: Lung sounds were clearing; SaO2 levels were 98% on RA, and patient had in total intake of 1400ml and a total output of 7300ml, a weight loss of 6kg. Patient tolerated Lasix and K-Dur well, and verbalized the reason he was taking the medications. Patient had a total sodium intake of 1975mg and verbalized the importance of eating fresh fruit and vegetables, and eating less processed foods and demonstrated how to read a food label. GOAL EVALUATION: The goal will be continued. The patient had aintake of <1500ml and a sodium intake of <2000mg the goal was reached but will be continued, patient teaching will also continue till discharge
#3 Activity Intolerance R/T Generalized weakness AEB fatigue, and SOB GOAL: Patient will be demonstrate clustering of activities and be able to perform ADLs throughout shift. INTERVENTIONS: Assess BP, HR and O2 sats, before and after activity Orthostatic hypotension can occur from the medications (vaso dilation and fluid shifts from diuretics) Give medications: Glucophage do maintain a proper glucose level The patient must take his oral diabetic medication to maintain stable glucose levels, during periods of illness the levels may change and must be monitored closely Teach patient how to cluster activities in order to decrease the energy required to perform tasks By clustering the activities the patient will be able to perform his own ADLs and rest in between his periods of exertion. EVALUATION: The patient had no episodes of orthostatic hypotension, patient denied dizziness, and was able to perform ADLs without assistance. Patient maintained O2 sats >97% on RA during activities; Patient took Glucophage and had a blood glucose level of 97, patient verbalized the reason for taking Glucophage this will help keep my sugar levels normal; The patient verbalized and demonstrated how to cluster activities in order to minimize fatigue, patient also asked about an exercise program he could start and was given printed pages explaining how to exercise safely based on CHF GOAL EVALUATION: The goal was met, but the diagnosis needs to be continued through discharge with follow up teaching in home.
#4 Deficient Knowledge R/T Patient not going to doctors appointments AEB: Patients verbalization of not knowing that he had CHF, and asking what that means GOAL: Patient will understand and verbalize causes, treatments, and care related to CHF INTERVENTIONS: Assess knowledge of causes, treatment, and care related to CHF This provides a base for educational planning Educate about normal heart and circulation, CHF disease process, symptoms, dietary modifications, activity guidelines, medications, goals, therapy and community resources This will help to reduce symptoms and readmissions for exacerbation Encourage Questions This will help verify understanding of information EVALUATIONS: The patient said I didnt know I had CHF I thought that I was just gaining weight because I like to eat PT stated that he didnt know that it was that important to go to the doctors because its so expensive and he didnt want to go all the time. The patient was given an information packet that contained community resources for in home services, he was also provided a packet that contained information on CHF and diabetes. The information was read together and then the patient wanted to read through it again and write down questions GOAL EVALUATION: The goal has not been met and needs to be continued beyond discharge, the patient received a referral for home health and a social worker will be in before discharge to set up additional services.
Potrebbero piacerti anche
- Care Plan For CHFDocumento9 pagineCare Plan For CHFJon Djchimz IsidroNessuna valutazione finora
- Concept Map PEDocumento3 pagineConcept Map PERobert MariasiNessuna valutazione finora
- HypokalemiaDocumento3 pagineHypokalemiaSergeiNessuna valutazione finora
- Congestive Heart Failure 1 Concept Map !Documento1 paginaCongestive Heart Failure 1 Concept Map !Franklin A. Salaum IIINessuna valutazione finora
- Nursing Care Plan For Heart Failure ChronicDocumento26 pagineNursing Care Plan For Heart Failure ChronicbrantNessuna valutazione finora
- Nursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Documento9 pagineNursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Gayu Patel0% (1)
- Drug Card SennaDocumento1 paginaDrug Card SennaAdrianne Bazo100% (1)
- Impaired Tissue Integrity - CellulitisDocumento3 pagineImpaired Tissue Integrity - CellulitisKelvin Kurt B. AgwilangNessuna valutazione finora
- Hyperosmolar Hyperglycemic State (HHS)Documento21 pagineHyperosmolar Hyperglycemic State (HHS)Malueth AnguiNessuna valutazione finora
- SBAR Report To Physician About A Critical SitutionDocumento3 pagineSBAR Report To Physician About A Critical SitutionRandolph DjanieNessuna valutazione finora
- Nursing Care Plan Impaired Gas ExchangeDocumento1 paginaNursing Care Plan Impaired Gas ExchangeKarylle PetilNessuna valutazione finora
- PathophysiologyDocumento1 paginaPathophysiologyHazel PalomaresNessuna valutazione finora
- Nursing DiagnosisDocumento7 pagineNursing DiagnosisMariya Mikaela Garcia SoledadNessuna valutazione finora
- Respiratory AcidosisDocumento5 pagineRespiratory Acidosisapi-376421583% (6)
- Concept Map (Aplastic Anemia) b1Documento6 pagineConcept Map (Aplastic Anemia) b1Ran PioloNessuna valutazione finora
- Nursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisDocumento19 pagineNursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisRiza Angela BarazanNessuna valutazione finora
- Concept Map Meningitis TheoryDocumento3 pagineConcept Map Meningitis TheoryMia AuliaNessuna valutazione finora
- NUR129 Endocrine Concept Mapping InstructorDocumento8 pagineNUR129 Endocrine Concept Mapping InstructorAmber EssmanNessuna valutazione finora
- JDM Care PlanDocumento5 pagineJDM Care PlangopscharanNessuna valutazione finora
- Concept Map 360Documento6 pagineConcept Map 360api-273469220Nessuna valutazione finora
- Med-Surg Care PlanDocumento13 pagineMed-Surg Care Planapi-520453750Nessuna valutazione finora
- Concept Map - F and EDocumento1 paginaConcept Map - F and EAbigail LonoganNessuna valutazione finora
- HHNK and DkaDocumento4 pagineHHNK and Dkagoya100% (1)
- Concept Map Due 04Documento9 pagineConcept Map Due 04api-545711468Nessuna valutazione finora
- Rheumatic Joint Disease Study GuideDocumento18 pagineRheumatic Joint Disease Study Guidechalinsammy1Nessuna valutazione finora
- Hypoglycemia: Presented by Farse GhabayenDocumento11 pagineHypoglycemia: Presented by Farse GhabayenFares G. Ghabayen100% (2)
- CarePlan #2Documento3 pagineCarePlan #2Monika StasiakNessuna valutazione finora
- Nursing Care Plan ProjectDocumento12 pagineNursing Care Plan ProjectMj WilliamsNessuna valutazione finora
- Coronary Artery Disease and HypertensionDocumento8 pagineCoronary Artery Disease and HypertensionsnehaNessuna valutazione finora
- Nursing Care PlanDocumento10 pagineNursing Care PlanSittie Rohaina SabanNessuna valutazione finora
- Fluids and Electrolytes ConceptDocumento31 pagineFluids and Electrolytes ConceptDarwin AndalNessuna valutazione finora
- Concept Map SepsisDocumento4 pagineConcept Map SepsisSavanna ChambersNessuna valutazione finora
- Nursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveDocumento2 pagineNursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveFreisanChenMandumotanNessuna valutazione finora
- Potential Complications Signs and SymptomsDocumento2 paginePotential Complications Signs and SymptomsJessica GomezNessuna valutazione finora
- Abdominal TraumaDocumento4 pagineAbdominal TraumaNicoh AvilaNessuna valutazione finora
- Drug Name Mechanism of Action Indication Side Effects Nursing Responsibilities Generic Name: Occasional: DuringDocumento2 pagineDrug Name Mechanism of Action Indication Side Effects Nursing Responsibilities Generic Name: Occasional: Duringhahaha100% (1)
- Chapter041 DIABETESDocumento8 pagineChapter041 DIABETESJelly BeanNessuna valutazione finora
- Nursing Care Plan For HematuriaDocumento2 pagineNursing Care Plan For HematuriaTee Wood63% (8)
- NCP DMDocumento21 pagineNCP DMKate ManalastasNessuna valutazione finora
- LCPDDocumento7 pagineLCPDakoismeNessuna valutazione finora
- Concept MapDocumento5 pagineConcept Mapmild_tea100% (1)
- Nursing Interventions CHFDocumento3 pagineNursing Interventions CHFbanyenye25100% (1)
- Left-Sided Heart FailureDocumento3 pagineLeft-Sided Heart FailureKhalid Mahmud ArifinNessuna valutazione finora
- Chapter 47 Diabetes Mellitus PDFDocumento14 pagineChapter 47 Diabetes Mellitus PDFRLLT100% (1)
- Nursing Care PlanDocumento22 pagineNursing Care PlanjamNessuna valutazione finora
- This Study Resource Was: System DisorderDocumento1 paginaThis Study Resource Was: System DisorderDeo FactuarNessuna valutazione finora
- Welcome To The Case Study Presentation:-: Prostate CancerDocumento22 pagineWelcome To The Case Study Presentation:-: Prostate CancerDengo ChapatieeNessuna valutazione finora
- Management For Acute Lymphocytic LeukemiaDocumento3 pagineManagement For Acute Lymphocytic LeukemiamarivohNessuna valutazione finora
- DiverticulitisDocumento2 pagineDiverticulitisyapyapvinx50% (2)
- Nursing Care PlanDocumento10 pagineNursing Care PlanMalou SanNessuna valutazione finora
- NCP PainDocumento2 pagineNCP PainApril_Ivy_Raga_3835Nessuna valutazione finora
- Morphine (Astramorph)Documento1 paginaMorphine (Astramorph)Adrianne BazoNessuna valutazione finora
- Nursing Diagnosis Impaired Gas ExchangeDocumento7 pagineNursing Diagnosis Impaired Gas ExchangeZycon Rodney Ae'zecquel Gachallan50% (2)
- Peds Concept MapDocumento5 paginePeds Concept Mapapi-496323326Nessuna valutazione finora
- NCC-SickleCellAnemiaManagement ConceptMap InteractivePDFDocumento2 pagineNCC-SickleCellAnemiaManagement ConceptMap InteractivePDFLoggerz Arck100% (1)
- Management of Tuberculosis: A guide for clinicians (eBook edition)Da EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Nessuna valutazione finora
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsDa EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsNessuna valutazione finora
- Mary Cris Canon CHF For or Case Study.Documento12 pagineMary Cris Canon CHF For or Case Study.Mary Cris CanonNessuna valutazione finora
- Hypertensive Cardiovascular DiseaseDocumento16 pagineHypertensive Cardiovascular DiseaseTintin Ponciano100% (1)
- Phonetic Sounds (Vowel Sounds and Consonant Sounds)Documento48 paginePhonetic Sounds (Vowel Sounds and Consonant Sounds)Jayson Donor Zabala100% (1)
- Part 4 Basic ConsolidationDocumento3 paginePart 4 Basic Consolidationtαtmαn dє grєαtNessuna valutazione finora
- Message To St. MatthewDocumento3 pagineMessage To St. MatthewAlvin MotillaNessuna valutazione finora
- DonatelloDocumento12 pagineDonatelloGiorgia Ronfo SP GironeNessuna valutazione finora
- Mark Scheme (Final) January 2020Documento16 pagineMark Scheme (Final) January 2020aqib ameerNessuna valutazione finora
- Basilio, Paul Adrian Ventura R-123 NOVEMBER 23, 2011Documento1 paginaBasilio, Paul Adrian Ventura R-123 NOVEMBER 23, 2011Sealtiel1020Nessuna valutazione finora
- PRS Product DescriptionDocumento42 paginePRS Product DescriptioneliaezekielNessuna valutazione finora
- A Terence McKenna Audio Archive - Part 1Documento203 pagineA Terence McKenna Audio Archive - Part 1BabaYagaNessuna valutazione finora
- Past Simple Present Perfect ExercisesDocumento3 paginePast Simple Present Perfect ExercisesAmanda Trujillo100% (1)
- Chapter 6 Coming of SpainDocumento4 pagineChapter 6 Coming of SpainJayvee MacapagalNessuna valutazione finora
- AUTONICSDocumento344 pagineAUTONICSjunaedi franceNessuna valutazione finora
- Business Intelligence in RetailDocumento21 pagineBusiness Intelligence in RetailGaurav Kumar100% (1)
- Ansys Flu - BatDocumento30 pagineAnsys Flu - BatNikola BoskovicNessuna valutazione finora
- High Court Judgment On Ex Party DecreeDocumento2 pagineHigh Court Judgment On Ex Party Decreeprashant pathakNessuna valutazione finora
- Introducing Identity - SummaryDocumento4 pagineIntroducing Identity - SummarylkuasNessuna valutazione finora
- Corporation Essay ChecklistDocumento5 pagineCorporation Essay ChecklistCamille2221Nessuna valutazione finora
- ABHI Network List As On 30-06-2023Documento3.401 pagineABHI Network List As On 30-06-20233uifbcsktNessuna valutazione finora
- Asterisk 10.0.0 Beta1 SummaryDocumento113 pagineAsterisk 10.0.0 Beta1 SummaryFaynman EinsteinNessuna valutazione finora
- Government of Kerala: Minority CertificateDocumento1 paginaGovernment of Kerala: Minority CertificateBI185824125 Personal AccountingNessuna valutazione finora
- F A T City Workshop NotesDocumento3 pagineF A T City Workshop Notesapi-295119035Nessuna valutazione finora
- The Court of Heaven 1Documento2 pagineThe Court of Heaven 1Rhoda Collins100% (7)
- Mission Veng 29th, 2019Documento4 pagineMission Veng 29th, 2019Lasky ChhakchhuakNessuna valutazione finora
- Equilibrium of Firm Under Perfect Competition: Presented by Piyush Kumar 2010EEE023Documento18 pagineEquilibrium of Firm Under Perfect Competition: Presented by Piyush Kumar 2010EEE023a0mittal7Nessuna valutazione finora
- Types of Sutures and Their IndicationsDocumento6 pagineTypes of Sutures and Their IndicationsAdina BurciuNessuna valutazione finora
- Experiment No 5 ZenerDocumento3 pagineExperiment No 5 ZenerEugene Christina EuniceNessuna valutazione finora
- Ingles Semana 11. P6. 2Q. 4egb. A y BDocumento2 pagineIngles Semana 11. P6. 2Q. 4egb. A y BWendisilla BelenchisNessuna valutazione finora
- Wardancer 4e HomebrewDocumento3 pagineWardancer 4e HomebrewWyjecNessuna valutazione finora
- Hyrons College Philippines Inc. Sto. Niño, Tukuran, Zamboanga Del Sur SEC. No.: CN200931518 Tel. No.: 945 - 0158Documento5 pagineHyrons College Philippines Inc. Sto. Niño, Tukuran, Zamboanga Del Sur SEC. No.: CN200931518 Tel. No.: 945 - 0158Mashelet Villezas ValleNessuna valutazione finora
- Sancticity AllDocumento21 pagineSancticity AllJames DeHart0% (1)
- Gesture and Speech Andre Leroi-GourhanDocumento451 pagineGesture and Speech Andre Leroi-GourhanFerda Nur Demirci100% (2)