Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
List of Drugs Pharmacology 2
Caricato da
Maisarah Ab SamadDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
List of Drugs Pharmacology 2
Caricato da
Maisarah Ab SamadCopyright:
Formati disponibili
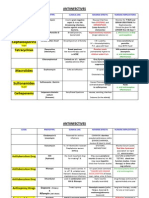
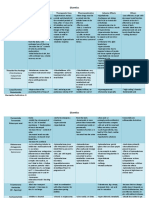
LIST OF DRUGS (PHARMACOLOGY) TYPE NAME M/A @ CHARS Commonly used anti-hypertensive drug Diuretic -Can be used alone
or Combination with Loop (renal ACEI, ARB, b-blockers insufficiency) & CCB Thiazide ( normal renal) -thiazides -amiloride/ hydrochlorothiazide -Indapamine SR -Indapamine -Triamterene/ hydrochlorothiazide Calcium Channel Decreasing of Blockers (CCB) intracellular Nifedipine availability of Ca2+ Verapamil Diltiazem EFFECTS Antihypertensive Lower BP Decrease preload ~ reduce circulating volume BAD EFFECTS High dose~ -Serum cholesterol , glucose, uric acid & Ca levels -Decrease K, Na & Mg levels -Erectile dysfunction CONTRAINDICATION *patient with gout *renal insufficiency
Smooth muscle relaxation Vasodilator action
b- blocker (-lol) ~ propanolol
Inhibit adrenergic (adrenalin=NE/E) response ~means block sympathetic act.
-Decrease heart rate -Reduce rennin release -local anasthetics
ACE inhibitors (pine/verapamil) Amlodipine Diltiazem Felodipine Isradipine Lacidipine Nicardipine Nifedipine verapamil Angiotensin Receptor Blockers (ARBs) (-tan) -losartan -candesartan -irbesartan
Cause arteriolar and venodilation
Lowering BP
-initial tachycardia -hypotension --headache -flushing -ankle oedema -nausea -constipation Bradycardia Heart block Peripheral vascular disease Sick-sinus syndrome Asthma/COPD Enhance coronary artery disease tiredness -cough -angioedema -increase foetal n neonatal mortality
Use of sublingual nifedipine
Patient with Impaired CHO tolerance in prediabetic patients Partial & complete heart block
-renovascular disease - pregnant mother
-Block only Lowering BP thromboxane A2 receptor, -Block action of A-II (vasoconstricyion, central & peripheral sympathetic stimulation, relez of aldosterone, salt n water reabsortion, vasopressin relez) Anti-anginal drug (stable angina/angina pectoris: unstable angina: variant angina) Angina pectoris: coronary blood flow inadequate to meet myocardial oxygen demand Result from: artherosclerosis & spasm of coronary artery Nitrates Venodilator/ Short acting: vasodilator -Nitroglycerine Long acting:
hypotension hypokalemia headache dizziness weakness
pregnancy
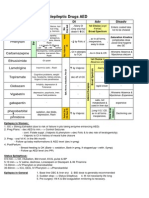
-Isosorbide mononitrate -Isosorbide dinitrate -blockers cardiac Non-selective: contractility -Propanolol Cardioselective blockers (1) -Atenolol -Metoprolol Ca2+ channel blocker Inhibit Ca2+ entrance (CCB) into cardiac & Dihydropyridine: Smooth muscle -Nifedipine -Amlodipine Non-dihydropyridine: -Verapamil -Diltiazem Sedatives & Hypnotics Sedative: reduces anxiety and has calming effect Hypnotic: produce drowsiness, encourage onset and maintenance of sleep Benzodiazepines -bind to BZ receptor -sedative-hypnotic site on GABA -anxiolytic - increase receptor -anticonvulsant affinity for GABA -muscle relaxant -increase the frequency of opening of the chloride channels *GABA is the major inhibitory neurotransmitter in the CNS Barbiturates -promote GABA -cause sedative and (induced increase in promote sleep chloride conductance -anticonvulsant actions at GABA synapse) -anaesthesia -can directly cause in increase chloride conductance at higher doses Action are nonspecific and other excitable tissue are also inhibited at high doses (e.g.cardiovascular) Buspirone -acts on 5 HT 1 -relieves anxiety without receptors(partial marked sedation agonist) -no hypnotic or -suitable for anticonvulsant activity generalized anxiety Other (older) sedative hypnotic drugs -glutethimide -chloral hydrate -Similar action to -paradehyde barbiturate
-dependence -drowsiness and confusion -ataxia -cognitive impairment -tolerance
-drowsiness -CNS depression -paradoxical excitement -can precipitate acute porphyria in susceptible individuals
Acute porphyria in susceptible individuals *affect the nervous system or skin, or both. porphyria is due to the deficiency of heme.
-tachycardia -nervousness -palpitations -GIT distress
Not effective in panic disorder
-meprobamate -similar to barbiturate Anti-Psychotics Psychosis: loss of contact with reality + delusions & hallucinations Positive symptoms (delusion, hallucination) Negative symptoms (social withdrawal, blunted effect) Overactivity of dopamine at D2 receptors (limbic system & 5HT (serotonin) overactivity at 5HT2A
neocortex) Typical Antipsychotics *Phenothiazines (chlorpromazine) *Butyrophenones (haloperidol) *Thioxanthenes (flupentixol) *Other heterocyclics: sulpiride, pimozide
Alleviate +ve symptoms Bind & block D2 receptors Dopamine receptor D2 type (D2,D3,D4) D1 type (D1,D5)
USES: Psychosis Mania Organic brain syndrome Anxiety Antiemetics Mesolimbic-mesocotical: relieve behavioural manifestations of shizo.
Atypical Antipsychotics *Clozapine *Olanzapine *Risperidone
Alleviate +ve & -ve symptoms Block D2 (potency) & 5HT2A (potency)
agitated aggressive Withdrawn patients become more responsive & communicative Hallucination, delusion, disorganized incoherent thinking disappear gradually Less EPS
Basal ganglia (nigrostriatal pw) extrapyramidal effects Acute: parkinsonism Akathisia Dystonia Malignant neuroleptic syndrm Chronic: Tardive dyskinesia P.gland (tuberoinfundibular) Hyperprolactinemia menstrual irregular gynaecomastia galactorrhea Block muscarinic r: dry mouth, urinary retention,memory impairment Block 1-adrenergeic & H1-receptor: reflex tachycardia, hypotension, sedation Cardiovascular: Ventricular arrhythmias (thioridazine) Metabolic: Weight gain (olanzapine,clozapine Diabetes mellitus Cardiovascular: Ventricular arrhythmias
ADVERSE EFFECTS: Cholestatic jaundice Skin eruptions Agranulocytosis (clozapine) Cataract (chlorpromazine) Retinal deposit (thioridazine)
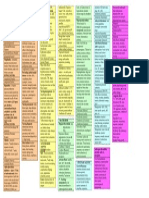
Anti-depressants persistent lowering mood, inability to experience pleasure in usual activities Classification: -reactive depression -endogenous depression * -bipolar effective disorder depression PATHOGENESIS: Monoamine hypothesis Neurotrophic Hypothesis functional amine dependent Loss of neurotrophic support neurotransmission (5HT & NA) (neurogenesis & synaptic connectivity) Selective serotonin reuptake inhibitors (SSRI) -fluoxetine -citalopram -escitalopram -fluvoxamine Inhibit NE and/or 5HT reuptake (acting on transporter) Clinical uses -major depression -severe anxiety disorders -Panic disorder (TCAs) -Phobic disorder (TCAs) -obsessive compulsory disorder (TCA,SSRI)
Neuroendocrine factors Abnormality hypothalamo-pituitaryadrenal axis cortisol , corticotrophine RH
Selective serotonin noradrenaline reuptake inhibitors (SNRI) -venlafaxine -desvenlafaxine -duloxetine -milnacipran Tricyclic antidepressants (TCA) -imipramine -clomipramine -desipramine -amitriptyline
-post-traumatic stress disorder (TCA,SSRI) -enuresis(bedwetting) in children & old pts -attention deficit hyperactivity disorder -psychosomatic disorder -chronic pain states
Low risk of interaction
TCA + *phenytoin,aspirin, phenothiazines TCA protein binding TCA effects *barbiturates TCA metabolism *SSRI (fluoxetine) TCA to toxic
Serotonin antagonist -trazadone -nefazodone Tetracyclic & unicyclic antidepressants -mirtazapine -bupropion -amoxapine -maprotiline Monoamine oxidase inhibitors Irreversible: -phenelzine -isocarboxazid -tranylcypromine Reversible: -Seligiline -Moclobemide
Block postsynaptic specific receptors
Inhibit degradation of monoamine (inhibit MAO) Excess neurotransmitter diffuse into synaptic cleft availability of monoamines binding Transcription of protein & inhibition of others Mood elevation
Drug interaction wif: SSRI & TCA -serotonin syndrome (too much 5HT) *hyperthermia *tremor *convulsions Agents + indirect sympathomimetics, amphetamine *bp Pethidine *severe respiratory *depression Cheese,wine ( tyramine= Sympathomimetic amine displace NA) *hypertensive crisis
Snippets: serotonin regulate mood, appetite, sleep muscle contraction 7 5HT receptors
Anesthesia: blocking sensation of one small part of the body to total unconsciousness General anesthesia: affect brain cells Lose of consciousness (reversible) analgesia muscle relaxation loss of reflexes Pre-anesthetic medication *to reduce anxiety *Benzodiazepines (anxiolysis) *to reduce pain (analgesia) *Morphine & NSAIDs *prevent bronchial *Antihistamines/ secretion anticholinergic drug *reduce gastric secretion *H2 receptor blockers / Proton pump inhibitor *to prevent nausea *Antihistamine (Promethazine) During surgery ST bind with GABA r Anesthesia (induction) Disadvantages: Inducing agent (I.V) Short duration
*Allergic to barbiturate
Sodium thiopental *ultra-short acting barbiturate *rapid & smooth onset * lipophilic Propofol Ketamine, Etomidate Inducing agent (inhale) Nitrous oxide
Open Cl- channel Hyperpolarization depress CNS anesthesia Induction & maintainance cation conductance in ion-channel Block excitatory neurotransmitter in brain X activity neuronal nicotinic AcH receptor Inhibit conduction of AP Neuromuscular blocker ability of Ach to open ligandgated ion channelparalyse Non-irritant Rapid induction of anesthesia Short recovery time Good analgesic effect X depress respiratory center /vasomotor center (VMC) Very potent anesthetic agent Smooth induction Non-irritant Pleasant to inhale
Anti-analgesic respiratory centr ( response to CO2 / hypoxia) BP myocardial actvty
*Acute intermittent porphyria *cardiovascular instability
potent anesthetic Oxidize components of Vit B12 Always used with halothane Combine wif O2 *Slow induction *Slow recovery *Lack analgesic efct *Depress cardio,respiratiory *Cause severe hepatic toxicity
Halothane (liquid)
Muscle relaxants Tubocurarine Gallamine Atracurium Pancuronium After Surgery: neostigmine
Produce muscle relaxation
Recover muscle paralyse Recover from unconscioucness Local Anesthetic numbing small local area, X unconsciousness analgesic Lidocaine Block AP propagation Cocaine in nociceptive neuron Procaine Block Na channels (inactivate) K Regional anethesia channel open K -spinal efflux -epidural repolarization
Toxicity: CVS: cardiac activity Hypotension CNS: Restleness Visual & auditory prob Convulsion Allergy: Insulin shock: Hypoglycaemia - Excess level of insulin - Weak - Drowsy - Confused - Hungry - Dizzy - Coma
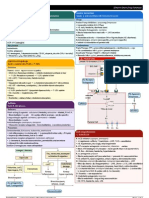
Drugs Diabetes Mellitus Insulin [subcutaneous@IV]
Rapid acting: Humalog - 15 min b4 meal - Onset : < 30 min - Peak: 30 min 1 h - Duration: 2 4 h Short acting: Regular - Onset: 30 min 1 h - Peak: 2 5 h - Duration: 5 10 h Intermediate acting: Lente - Onset: 1 3 h - Peak: 6 14 h - Duration: 18 24
h Long acting: Ultralente - Onset: 4 6 h - Peak: 16 24 h - Duration: 24 28 h Oral Antidiabetic Agent 1. Secretagogues Sulphonylureas Tolbutamide Glipizide Glyburide Glipemiride
Stimulate insulin release from cell Block ATP sensitive channel Depolarization 2+ Ca influx hepatic glucose production peripheral insulin sensitivity Sama ngan sulphonylureas More rapidly absorbed and eliminated
Weight gain Hyperinsulinemia Hypoglycaemia Renal hepatic insufficiency
Renal Insufficiency delayed excretion of drug Accumulation Hypoglycaemia
Meglitinides Repaglinide Nateglinide
Repaglinides: - Hypoglycaemia - Upper respiratory tract infection - Rhinitis - Bronchitis - Headache - Weight gain Nateglinide: - Nausea - Diarrhoea - Dizziness - Light headedness
2. Sensitizers Biguanides Metformin
hepatic glucose production inhibit hepatic gluconeogenesis skeletal muscle glucose uptake & metabolisme free fatty acids # PPAR involved in genes transcription regulating glucose and fat metabolism. Glitazones (bind) Peroxisome Proliferator Activated Receptor y (PPARy)
Nausea Vomiting Diarrhoea Stomach pain
Glitazones Rosiglitazone Pioglitazone
- Water retention - Tissue swelling - Weight gain
PPARs act on Peroxisome Proliferator Responsive Elements (PPRE) Influence insulin sensitive genes Enhance production of mRNAs of insulin dependent enzyme Better use of glucose by the cells
3. -glucosidase Inhibitors Acarbase Miglitol
-glucosidase inhibitors Inhibit enzyme [that breakdown polysaccharide sucrose] Slow down glucose absorption Cortisol binds to - Effect on metabolism (carb, glucocorticoid protein & fat metabolism. receptor in cytoplasm Clucocorticoid receptor activation TRANSLOCATION activated hormone receptor complex enter nucleus Interact with glucocorticoid response element (GREs) & other regulatory proteins. Modulate transcription - Anti-inflammatory
- GIT disturbance: Flatulence Diarrhoea Bloating Abdominal discomfort
Adrenocorticosteroids Cortisol (glucocorticoid)
- Immunosuppressive
Hypersecretion cause abnormal deposition of fat - Face (moon-face) - Shoulder (buffalo hump) - Pendulous abdomen *cushings syndrome Others : - Osteoporosis - Thinning of skin - Increase capillary fragility (pecah) - Bruising - Striae **due to protein catabolism
- No abrupt withdrawal, always gradual withdrawal abrupt withdrawal may lead to suppression of hypothalamic/ pituitary/ adrenocortical feedback system severe mental depression.
Aldosterone (mineralocorticoid)
reabsorption of sodium from renal tubule followed by reabsorption of water Increase in ECF volume, blood volume & Blood Pressure
- Increase the absorption of sodium and water - Increase the renal excretion of potassium.
- Excessive use in sodium - water retention - loss of potassium Muscle weakness symptoms : - edema Congestive heart failure - Hypertension - Sweating - Bruising - Allergic skin rash
Contraindicate if the patient already receiving a potassium-sparing diuretic.
Analgesic-opioid (drug that relieve pain)-moderatesevere Pain: an unpleasant sensory & emotional experience associated with actual/potential tissue damage Nociceptive pain Neuropathic pain -tissue damage -damage/dysfunction of nerves (PNS/CNS) -acute: quick, excessive noxious stimulus /chronic: slow transmission Endogenous opioid (body synthesized) -somatic:localized visceral: internal organ Enkephalin, endorphin, dynorphin referred pain: sakit tmpt lain, rasa tmpt lain (endomorphin-1/-2)-new Opioid /narcotics Bind to opioid CNS: *histamine release asthmatic patient analgesic receptors (, ,,)*analgesia -urticaria Opiates (Morphine) coupled G-protein -exert effect at receptor -swearing -inhibit neuronal activity -bronchospasjm Less effective analgesia Inhibit adenylyl -inhibit release of cyclise neurotransmitter GIT: Codeine -activate descending motility Tramadol Activate receptorinhibitory system tone Methadone activated K+ currents *Sedation seretion K+ efflux doseconvulsion passage of fecal Antagonist: naloxone (hyperpolarization (muscles contract and relax mass Inhibit Ca2+ entry rapidly and repeatedly, water absorption resulting in an uncontrolled transmitter release shaking of the body) (anti-diarrheal effect) & excitability *euphoria -delay gastric (sense of well-being) emptying Inhibit transmission *respiratory suppression nociceptive impulse -depress respiratory center (overdose) CO2 sensitivity arterial PCO2 Cerebral vascular dilatation *cough suppression -anti-tussive -codeine,pholcodeine *nausea & vomiting -stimulate chemoreceptor trigger zone (CTZ) *miosis -pin-point pupil (constriction of pupil) NSAIDs (non-opioid) mildmoderate (inflammation) NSAIDs Inhibiting Non-selective COX *Anti-inflammatory #GIT #Renal COX-1>COX-2 (can inhibit both COX- *Analgesic effect -- peptic ulcer insufficenency 1,COX-2) inhibit *Antipyretic effect -nausea #hepatic Indomethacin prostaglandin # platelet dysfunction Sulindac synthesis aggregation #peptic ulcer Piroxicam #hepatic #renal failure Phospholipid (hepatoxicity) #NSAID allergy Phospholipase #renal #anticoagulant Arachidonic acid (glumorukopathy) #thrombocytopenia Cyclooxygenase #CNS (hallucinations) Prostaglandin #Hypersensitivity Salicylates (Aspirin) A:Well absorbed in + Anti platelet effect #Renal: derived from Salicylic GIT *PG (renal acid (SA) rectal absorption vasodilatior) M:Rapid hydrolysed * PG: blood flow SA *Na & H2O retention Glycine bp conjugateinactivate *GFR: renal failure ions #Salicylism: tinnitus, E:kidney headach, confuse #Allergy:urticaria #Reyes syndrome: detrimental effects
to organs NSAIDs Inhibiting COX-1 = COX-2 Ibuprofen Highly selective COX-2 Celecoxib Paracetamol (Acetaminophen) (not NSAIDs) Non-selective COX (can inhibit both COX1,COX-2) inhibit prostaglandin synthesis Selective COX-2 Inhibitors Inhibit PG synthesis in CNS (maybe via COX3) A:well absorb (GIT) M: conjugate as glucoronide & sulphate Brochial Asthma 2-receptor agonist Non-selective: Adrenaline Selective: *Short -salbutamol -terbutaline -fernoterol *Long -salmeterol -fomoterol Methylxanthine -Theophylline -Amophylline cAMP Stimulate adenyl cyclase [x] SM contraction [x] mast cell mediator release
#analgesic effect #anti-pyretic effect
-lack GIT effect -not produce Reyes syndrome Overdose: -hepatoxicity -slow death (liver damage) (B1 receptor-effects) -tachycardia -palpitation -peripheral vasodilation -hypokalemia
Relief acute attack of asthma
Anticholinergic (antimuscarinic) -ipratropium bromide -tiotropium Corticosteroid *systemic -hydrocortisone (IV) -prednisolone *inhaled -beclomethasone -budesonide Mast cell stabilizers -sodium cromoglycate -nedocromil Leukotrienes Pathway Inhibitors *Leukotriene synthesis inhibitor -zileuton *Leukotriene receptor antagonist -zafirlukast -montelukast Anti-IgE monoclonal ab Opioids
[x] phosphodiesterase enzyme cAMP Relax SM [x] adenosine receptor (X) AcH at muscarnic receptor (X) bronchoconstriction (X) phospholipase A2 (X) COX-2 arachidonic acid D inflammatory mediators (leukotrienes) (X) mast cell degranulation Arachidoic acid (X) 5-lipoxygenase Leukotrienes
Chronic treatment Nocturnal cough prophylaxis IV acute asthma Oral chronic asthma
Vomiting, nausea Headache, anxiety, tremor, seizures, dysrhythmmias
Effective in COPD
Prophylactic Prevent broncoconstriction Moderate asthma Maintenance prophylaxis Mild Git upset headache
-blockCysLT (leukotriene receptor) contraction of SM (x) igE binding (X) igE synthesis Block medullary -
ANTI-TUSSIVE
-morphine -codeine -methadone H-receptor antagonist st -1 generation *promethazine *pheniramine
nd
cough center cough reflex
-2 generatiomn
Expectorants
Mucolytics -Carbocysteine, mecysteine
-dornase alfa
-bromhexine, ambroxol
Peptic Ulcer -triple therapy for 14days is considered the treatment of choice. - 1 PPI + 2 antibiotics -can substitute Flagyl 500mg PO for 14d if allergic to PCN -in active peptic ulcer, continue qd PPI for additional 2 weeks - goal: complete elimination of H. Pylori Histamine/H2 receptor -Block the H2 Relieves heartburn and antagonist receptor of histamine functional dyspepsia pain -cimetidine(tagamet) in parietal cells and promotes ulcer healing -ranitidine (zantac) -Inhibit the cAMPby decreasing stomach acid -famotidine(peptid) dependent pathway -nizatidine (axid) from activating the proton pump -Inhibit HCl secretion Proton pump receptor (PPI) - omeprazole (prilosec) -lansoprazole (prevacid) -rabeprazole (aciphex) -Esomeprazole (nexium) Exist in inactive form prodrugs -readily converted to active form in low pH(acidic) -become thiolreactive - Inhibits H+/K+ ATPase enzyme irreversibly Results in more complete acid suppression in comparison to H2 blockers
-Headache -Dizziness -Diarrhoea..etc
Antibiotic -clarithromycin -amoxycillin -tetracycline
A single antibiotic is not sufficient, combination of 2 antibiotics are required (synergistic effect)
Elimination of H. Pylori
Antibiotic (AMA) B-lactam antibiotics *Penicillin *Cephalosporins *Carbapenems
Inhibition of cell wall synthesis -prevent cross-linkage (inhibit transpeptidase) -prevent cross-linkage (bind D-alanine) Disrupt cell membrane Bind to phospholipids Inhibit protein synthesis Change 30S rRNA shape mRNA read incorrectly Bind to 50S rRNA X movement on mRNA Interfere tRNA anticodon reading Bind to 50s rRNA X peptide bond form Inhibit N.A synthesis
Glycopeptide *Vancomycin *Teicoplanin Polymyxin
*Prophylaxis (prevention of serious infection) *Empirical therapy (therapy before lab result) *Directed therapy *Combine use of AMAs? -to achieve synergism effects (-cidal/-static) - adverse effect -X resistance -broaden spectrum of AMA action
*Toxicity (Local/Systemic) *Hypersensitivity *Superinfection (disruption of normal microflora) *Nutritional deficiencies
CHOICES OF AMA -PATIENT Age, drug allergy, immune status Eg: bacteriostatic immune system OK -ORGANISM Clinical diagnosis, culture & sensitivity, severity
Aminoglycosides *streptomycin
Drug Resistance 1. natural (lack of specific target site for the drug) 2.acquired (mutation) *X entrance of drug,change in CM permeability *alter drug binding site (acquire new gene) *pump out drug/efflux pump *inactive the drug *use alternative p/way:metabolite
-DRUG Spectrum (narrowgram +/-) (broadboth) Toxicity, route, pharmacokinetics
Macrolides *Erythromycin Tetracycline Chloramphenicol Rifampin Quinolones Nalidixic acids Rifamycin
Antifungal Polyene Amphothericin B (AMB) Liposomal Ampho B Ampho B in lipid delivery vehicle toxicity tolerability of infusion
Interact with ergosterol (fungi cell membrane) Produce hydrophilic channels(micropore) Electrolytes,cell contents move out
-for oral, vaginal, cutaneous candidiasis -otomycis -systemic mycoses #broad spectrum eg: (against candida spp,aspergillus,
Highly toxic a) acute reaction occur in each infusion: chills, fevers, hypotension,nausea #: add hydrocortisone
Pharmacokinetics * I.V administration *poor CSF absorbintrathecal *slow release *slow excrete *protein-bound Nystatin Azoles: Imidazole -Ketoconazole -Miconazole -Clotrimazole Triazoles affinity toxic *topical Lanoesterol (14-demethylase/ P450 enzyme) (-) Ergosterol Abnormal fungi membrane Superficial candidiasis Less toxic than ampho B Broad: Candida sp., c. Neoformans, aspergillus
b) chronic reaction -nephrotoxic -electrolyte disturbance -CNS toxicity
-nausea -bad taste in mouth -GIT Upset -hepatitis
Drug interaction: Affect mammalian P450
-flucanazole -itraconazole -voriconazole Flucytosine (5-FC) (narrow spectrum) Griseofulvin Echinocandis -caspofungin -micsfungin -anidulafungin Antivirals Anti-Herpes virus (HPV-1,HPV2,CMV,EpsteinBarr,Varicella zoster) Acyclovir
Pharmacokinetics: Oral & i.v Good absorption Inhibitor of thymidylate synthesis P/kinetic: oral Mitotic inhibitor Block synthesis 1,3--D-glucan (cell wall p/kinetic: i.v Deoxyguanosine analog Acyclovir v.l thymidine kinase Acyclovir monophosphate Acyclovir triphosphate x viral DNA pol x lengthening DNA strands
Chromoblasto Mycosis Synergestic with AMB Dermatophyte Protect skin For Resistant infection
Marrow suppression hepatitis Headache, git disturbance Not much side effects
Foscarnet
Inhibit v. DNA pol, reverse transcriptase
Anti-CMV Gancyclovir (analogue Acyclovir, more active)
Pharmacokinetics: I.V, oral, intraocular
Anti-influenza virus Adamantanamine -amantadine -rimantadine Sialic acid Oseltamavir (oral) Zanamivir (inhaler) Anti-hepatitis Interferon
Inhibit replication of influenza A virus Prevent uncoating of viral RNA Inhibit neuraminidase enzyme (for viral release) Inhibit all steps of viral infection (i.v / i.m) PEGylated interferon Slow absorb Sustained effects Guanosine analogue Inhibit GTP synthesis Reverse transcriptase inhibitor (X) viral RNADNA
Low toxicity on normal host cell Preferentially taken up by virus infected cell Active aginst all herpes v. except CMV Uses: -genital herpes simplex (HPV2) -mucutaneous H. Simplex (HPV1) -H.simplex encephalitis (HPV1) -H.simplex I keratitis -Herpes zoster -Chicken pox *CMV retinitis & other CMV infections *Acyclovir-resistant mucocutaneous Active aginst all HPV Congenital & severe CMV -delay progession of retinitis risk of Karposis sarcoma i n HIV CMV infection -prophylaxis of influenza A2 (epidemic) -treatment Prophylaxis & treatment of Influenza A, B, H5N1 -chronic hepatitis B,C -Kaposis sarcoma -chronic myeloma leukemia
Headache Nausea Rashes Low BP Reduce GFR
Toxicity: Damage kidney Anemia Convulsions,tremor Rash, fever Bone marrow depression Retinal detachment Neuro psychiatric probs. Nausea, anorexia, insomnia, dizziness, nightmares Nausea, abdominal pain, headache, diarrhoea,cough Flu-like symptoms, fatigue, aches, anorexia, neurotoxicity, myelosuppression, hypotension, thyroid dysfunction Haemolytic anemia Psychiatric problem Toxicity: Anaemia, neutropenia Epilepsy, CNS disease, gastric ulcer, pregnancy
Ribavirin
Antiretrovirals Nucleoside RTI -Zidovudine -Didanosine -Lamivudine
-chronic hepatitis C -severe Respiratory Syncytical Virus (RSV) Combination therapy -reduce vertical transmission -symptomatic AIDS -infants with HIV
Non-nucleoside RTI -Nevirapine -Efavirenz -saquinavir -indinavir -ritonavir Enfuvirtude
-low CD4
Protease Inhibitors (X) aspartyl transferase Inhibit fusion of viral and cell membrane
Potrebbero piacerti anche
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsDa EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNessuna valutazione finora
- Cardiovascular PharmacologyDocumento61 pagineCardiovascular PharmacologyTeeOne920% (1)
- Revising basic and clinical pharmacology: eBookDa EverandRevising basic and clinical pharmacology: eBookNessuna valutazione finora
- Pharmacology Charts PDFDocumento88 paginePharmacology Charts PDFMohamad Samir90% (10)
- Clinical Physiology and Pharmacology: The EssentialsDa EverandClinical Physiology and Pharmacology: The EssentialsValutazione: 4 su 5 stelle4/5 (1)
- Pharmacology Complete Drug TableDocumento6 paginePharmacology Complete Drug Tableninja-2001100% (4)
- Drug ChartDocumento8 pagineDrug Chartstudentalwaysstudy100% (1)
- Pharmacology Chart 3Documento2 paginePharmacology Chart 3Omar ClorNessuna valutazione finora
- Anti Infective Drug ChartDocumento1 paginaAnti Infective Drug ChartJessica100% (1)
- Drugs MnemonicsDocumento6 pagineDrugs MnemonicsDarrylJavier100% (1)
- Pharmacology Drug Chart: Drug Name Receptor Therapeutic Uses Adverse EffectsDocumento18 paginePharmacology Drug Chart: Drug Name Receptor Therapeutic Uses Adverse EffectsPadmavathy Naidu Chokkapu100% (2)
- Drug SuffixesDocumento3 pagineDrug SuffixesjeromeasuncionNessuna valutazione finora
- Drug Nomenclature HintsDocumento1 paginaDrug Nomenclature HintsJordynNessuna valutazione finora
- Mechanism of Action For Each Class of AntiDocumento146 pagineMechanism of Action For Each Class of AntiReynaldo RiveraNessuna valutazione finora
- Antibiotics 9Documento11 pagineAntibiotics 9Beth Morales100% (1)
- Lang 10 EditionDocumento235 pagineLang 10 Editionraju niraulaNessuna valutazione finora
- Antiinfectives Drug TableDocumento5 pagineAntiinfectives Drug Tablecdp1587100% (3)
- Antibiotics Chart 2Documento10 pagineAntibiotics Chart 2Vee MendNessuna valutazione finora
- Antiepileptic Drugs AED: D' DI Disadv SE AdvDocumento1 paginaAntiepileptic Drugs AED: D' DI Disadv SE Advrayooona88Nessuna valutazione finora
- Pharmacology MapsDocumento18 paginePharmacology MapsPERUBATAN Cawangan Zagazig100% (1)
- Pain and Inflammation Med ChartsDocumento4 paginePain and Inflammation Med Chartssurviving nursing school100% (1)
- Pharmacology SummaryDocumento16 paginePharmacology Summaryshenric16Nessuna valutazione finora
- Git Drugs TablesDocumento3 pagineGit Drugs TablesSulochan Ssplendid Splinterr Lohani100% (1)
- Mnemonics For Antibiotics-2Documento10 pagineMnemonics For Antibiotics-2totallyfakeusernameNessuna valutazione finora
- Pharmacology of Adrenergic AgonistsDocumento9 paginePharmacology of Adrenergic Agonistsfiena92Nessuna valutazione finora
- Drug Name Mechanism Application Side Effects Contraindication Drug-Drug InteractionsDocumento3 pagineDrug Name Mechanism Application Side Effects Contraindication Drug-Drug Interactionsazhar hussinNessuna valutazione finora
- Generic Name Brand Names Common Uses Possible Side Effects Mechanism of ActionDocumento13 pagineGeneric Name Brand Names Common Uses Possible Side Effects Mechanism of Actionangel3424Nessuna valutazione finora
- Pharmacology MnemonicsDocumento19 paginePharmacology MnemonicsAl-nazer Azer Al100% (5)
- Endocrine Drug ChartDocumento1 paginaEndocrine Drug ChartJessicaNessuna valutazione finora
- AntimicrobialsDocumento1 paginaAntimicrobialsRomaine Barrett100% (1)
- Antihypertensives Drug ChartDocumento3 pagineAntihypertensives Drug Chartinfirmarydude100% (2)
- Pharmacology FirecrackerDocumento37 paginePharmacology FirecrackerRehan Usman100% (1)
- Musculoskeletal PharmacologyDocumento18 pagineMusculoskeletal PharmacologyBLEEMAGE100% (2)
- Drug Interactions: What Is An Interaction?Documento4 pagineDrug Interactions: What Is An Interaction?Leyla MajundaNessuna valutazione finora
- Diabetes Mellitus Drug ChartDocumento3 pagineDiabetes Mellitus Drug Chartlui.stephanie1751100% (1)
- Pharmacology Mnemonics (Part 01) by M IhtishamDocumento32 paginePharmacology Mnemonics (Part 01) by M Ihtishammuhammad ihtisham ul hassan100% (1)
- Pharmacology Mnemonic DoctorsHungoutDocumento20 paginePharmacology Mnemonic DoctorsHungoutJiaYee GoNessuna valutazione finora
- Pharmacology ChartDocumento6 paginePharmacology ChartPaula67% (3)
- Pharmacology Notes (Chapter 20 and 21)Documento2 paginePharmacology Notes (Chapter 20 and 21)graycorypNessuna valutazione finora
- Whole Pharmacology Classification: Adrenergic Antagonists Alpha Adrenergic Antagonists Alpha 1 AntagonistsDocumento17 pagineWhole Pharmacology Classification: Adrenergic Antagonists Alpha Adrenergic Antagonists Alpha 1 AntagonistsFlorina TrutescuNessuna valutazione finora
- DiureticsDocumento4 pagineDiureticsBill John100% (1)
- MS2 USMLE Pharm ReviewDocumento25 pagineMS2 USMLE Pharm ReviewAnna ArtyNessuna valutazione finora
- Complete Drug GuideDocumento225 pagineComplete Drug GuideJessica 'Baker' IsaacsNessuna valutazione finora
- Drug SummaryDocumento5 pagineDrug Summarybriancripe100% (2)
- Drugs of ChoiceDocumento3 pagineDrugs of ChoiceReeti R. Bhat100% (1)
- KDT Only ClassificationsDocumento72 pagineKDT Only ClassificationsDebashis ParidaNessuna valutazione finora
- Antibiotics Chart 1Documento7 pagineAntibiotics Chart 1Vee MendNessuna valutazione finora
- Pharm-Drugs ChartsDocumento21 paginePharm-Drugs ChartsCandace Flowers100% (3)
- Drugs Acting On The Gastrointestinal TractDocumento27 pagineDrugs Acting On The Gastrointestinal TractJames PerianayagamNessuna valutazione finora
- Pharm Drugs + Classes (All)Documento28 paginePharm Drugs + Classes (All)Tom WuNessuna valutazione finora
- A-Autonomic Drugs: 1) CholinergicDocumento28 pagineA-Autonomic Drugs: 1) CholinergicMahmoud Ahmed MahmoudNessuna valutazione finora
- Adrenergic Receptors ChartDocumento1 paginaAdrenergic Receptors ChartLeon ChenNessuna valutazione finora
- Pharmacology of The GITDocumento31 paginePharmacology of The GITmarviecute22Nessuna valutazione finora
- Cardiovascular Pharmacology OutlineDocumento11 pagineCardiovascular Pharmacology OutlineLhay de OcampoNessuna valutazione finora
- ATI Prototype DrugsDocumento11 pagineATI Prototype Drugsjinnyduong100% (1)
- Pharmacology SlidesDocumento114 paginePharmacology Slidesbrandon15000100% (9)
- Medicatia antiHTADocumento67 pagineMedicatia antiHTALizuka_92Nessuna valutazione finora
- Drenergic AND Anti Adrenergic Drugs: Shabib AkhtarDocumento21 pagineDrenergic AND Anti Adrenergic Drugs: Shabib AkhtarDeepa ShaiekhNessuna valutazione finora
- Drug ListDocumento30 pagineDrug ListKristineNessuna valutazione finora
- BIOSTATISTICSDocumento8 pagineBIOSTATISTICSMaisarah Ab SamadNessuna valutazione finora
- Normal Cell Physiology, Cell Growth & Cell MetabolismDocumento12 pagineNormal Cell Physiology, Cell Growth & Cell MetabolismMaisarah Ab SamadNessuna valutazione finora
- Practical 2Documento10 paginePractical 2Maisarah Ab SamadNessuna valutazione finora
- GTB 204 Molecular Tech Technic OSPE 2002/2003Documento3 pagineGTB 204 Molecular Tech Technic OSPE 2002/2003Maisarah Ab SamadNessuna valutazione finora
- Dissolution Method Development For Soft Gelatin CapsulesDocumento30 pagineDissolution Method Development For Soft Gelatin Capsulesbanapte599706Nessuna valutazione finora
- Practice Problems ADocumento2 paginePractice Problems ACrystal LynaeNessuna valutazione finora
- FILE 28 June QDocumento45 pagineFILE 28 June QHanan HejaziNessuna valutazione finora
- A. Pharmacodynamic: Mcu-Fdtmf Colloge of Medicine Department of Pharmacology Board QuestionsDocumento14 pagineA. Pharmacodynamic: Mcu-Fdtmf Colloge of Medicine Department of Pharmacology Board QuestionsJo Anne100% (1)
- Jurnal UveitisDocumento5 pagineJurnal UveitisAnna ApsariNessuna valutazione finora
- Antibiotics PDFDocumento8 pagineAntibiotics PDFSarah JaneNessuna valutazione finora
- Retention Sample Tracking 2017Documento2 pagineRetention Sample Tracking 2017MITON CHOWDHURYNessuna valutazione finora
- B PharmaSyllabusDocumento178 pagineB PharmaSyllabusKirthi Kanth NNessuna valutazione finora
- Droperidol (Inapsine)Documento1 paginaDroperidol (Inapsine)ENessuna valutazione finora
- Oral Medication Written ReportDocumento53 pagineOral Medication Written ReportOliver DiamaeNessuna valutazione finora
- Indigenous Health Information and Knowledge SystemsDocumento20 pagineIndigenous Health Information and Knowledge SystemsDexter Abrenica AlfonsoNessuna valutazione finora
- Mekanisme Kerja Obat Anestesi Lokal: Ratno Samodro, Doso Sutiyono, Hari Hendriarto SatotoDocumento14 pagineMekanisme Kerja Obat Anestesi Lokal: Ratno Samodro, Doso Sutiyono, Hari Hendriarto Satotoumar sahidNessuna valutazione finora
- 3 RdeditonDocumento387 pagine3 RdeditonHamza shoaib100% (1)
- PCNE Classification Scheme For Drug Related Problems-1 (Revised)Documento3 paginePCNE Classification Scheme For Drug Related Problems-1 (Revised)Alan HobbitNessuna valutazione finora
- Revised WTP Leaflet FinalDocumento3 pagineRevised WTP Leaflet FinalShrutangi VaidyaNessuna valutazione finora
- Antiepileptiki in Hipnotiki: (Antiepileptics and Hypnotics)Documento60 pagineAntiepileptiki in Hipnotiki: (Antiepileptics and Hypnotics)api-3814389Nessuna valutazione finora
- Chapter 2 New Drug and DevelopmentDocumento152 pagineChapter 2 New Drug and DevelopmentMeriam JuanNessuna valutazione finora
- Tatay Nick TranscriptDocumento9 pagineTatay Nick TranscriptSherwin LingatingNessuna valutazione finora
- Stock Obat BPJS Desember 2017Documento16 pagineStock Obat BPJS Desember 2017Vika FujiNessuna valutazione finora
- E-Catalog 2021Documento33 pagineE-Catalog 2021fiannysjahjadiNessuna valutazione finora
- Tamsulosin Tablets. Tamsulosin For Enlarged Prostate - PatientDocumento7 pagineTamsulosin Tablets. Tamsulosin For Enlarged Prostate - PatientXtineNessuna valutazione finora
- Lippincot Farma Ilustrata Ed5 - OCR - CompressedDocumento317 pagineLippincot Farma Ilustrata Ed5 - OCR - CompressedMaria PopescuNessuna valutazione finora
- Usp DC Pub 2023 Release 2.0 Updated FinalDocumento2.032 pagineUsp DC Pub 2023 Release 2.0 Updated FinalMerry AlveraNessuna valutazione finora
- AntihistaminesDocumento2 pagineAntihistaminesmercywicherNessuna valutazione finora
- Biopharmaceuticals Availability, Diffusion, Sustainability: Massimo Riccaboni University of Florence & CERM, RomeDocumento28 pagineBiopharmaceuticals Availability, Diffusion, Sustainability: Massimo Riccaboni University of Florence & CERM, RomeNoor hossainNessuna valutazione finora
- Faculty of Pharmacy Student CouncilDocumento14 pagineFaculty of Pharmacy Student CouncilFish BallNessuna valutazione finora
- William H. Soine - Clandestine Drug SynthesisDocumento34 pagineWilliam H. Soine - Clandestine Drug SynthesisAnonymous Gb9EyW83% (6)
- UPenn Foreign Donations For Fiscal Year 2021Documento9 pagineUPenn Foreign Donations For Fiscal Year 2021JoeSchoffstallNessuna valutazione finora
- Insulin Therapy in Critically IllDocumento2 pagineInsulin Therapy in Critically IllNisbet SamuelNessuna valutazione finora
- Nonhuman Primate FormularyDocumento25 pagineNonhuman Primate Formularymel Cid0% (2)