Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Lecture 11 October 11th-Eating Disorders
Caricato da
api-26938624Descrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Lecture 11 October 11th-Eating Disorders
Caricato da
api-26938624Copyright:
Formati disponibili
1MEN’S AND WOMEN’S HEALTH – OCTOBER 11TH, 2007
NATUROPATHIC APPROACH TO EATING DISORDERS AND BODY IMAGE DISTURBANCES
LECTURE 11
• Slides are not in order.
• Anorexia: highest mortality rate of any psychiatric disorder.
Risk for death:
• Daily vomiting/binging: metabolic alkalosis, dehydration, electrolyte loss. Hard to find this out, guilt and shame around
eating disorders. Always check their BP, weight (if they don’t refuse).
• Bulemia: can get gastric dilation, stomach rupture.
• Vomiting can present in anorexia. If they eat more than they think they should, will compensate with vomiting,
laxatives.
Symptoms found in patients with Anorexia Nervosa
• Feeling of fullness: this is REAL. Stomach has shrunken, motility has slowed down. Slower transit time. Bitters
helpful with this.
• Leg pains: red flag. Related to electrolyte balance. Sign that their balance is off.
• Infertility: be aware of their weight. Women seen in fertility clinics: some that are not ovulating may have undiagnosed
eating disorder.
• Polyuria: don’t have strong kidneys: start to weaken. Will drink a lot of water, eating a lot of fruit and vegetables.
• “Refeeding syndrome”: if they take in too much food too quickly: increase blood volume, strain on KI, KI failure
Signs of Anorexia Nervosa:
• Sialadenosis: enlargement of parotid glands
• Lanugo: growth of fine hair due to hypothermia. Goes away with weight gain.
• Yellow skin, esp. on palms (more visible in Caucasians): Keratenemia, related to LV function. Will start to smell like
feces in later stages: bilirubin is coming through the pores.
Temperament of AN (generally speaking)
• Fearful of intimacy: or may be in relationship, but may not have enjoyment of sex
• Hesitant to have new experience,
Diagnostic criteria for Bulimia Nervosa
• Recurrent.
• May vomit/purge up to 15-20 times/day.
• Don’t have prolonged starvation/weight loss.
• Weight remains stable or can increase.
• Keep some food down, and calories are absorbed quickly.
• More violence/impulsive re: bulimia. May be linked with self-mutilation: cutting breasts, abdomen, arms, legs.
• May have impaired gag reflex: use other things like toothbrush, washcloth: risk of choking.
• “Dramatic”: very labile/reactive personality. Eg. : Dr. G did acupuncture on bulimic patient, LV3, jumped off table,
crying, ran out of office. Why? She wanted Dr. G to follow her, attention-seeking behaviour, guilt induction.
• Other behaviour: might repeatedly cancel appointments, frantic messages. Dr. G. won’t work with them unless they
also have a counsellor/MD. Know your limits. There are others that are trained to help them.
• Idea of letting go of behaviour is terrifying as well: relationship to addiction, can be “best friend”, part of identity.
Symptoms found in patients with Bulimia
Swollen cheeks: due to electrolyte imbalance (?)
Signs of bulimia nervosa
• Russell’s sign: callouses on hand from repeated trigerring of gag reflex
• Perimolysis: enamel erosion, will see this on the back of the teeth (acid is coming this way). Dentists and hygenists
will likely ID, but may not ask.
• Gingivitis, caries common
MEN’S AND WOMEN’S HEALTH OCTOBER 11TH, 2007 – PAGE 1
• Periorbital petechiae: due to force of vomiting
• Injected sclera: due to vomiting: usually see this within 1-2 hours after vomiting.
• Lots of signs, but most are non-specific.
Temperament of BN
• Need external acknowledgement. Anorexia, don’t care as much about what others think.
• High risk behaviours: drive fast, don’t care if they crash
• Dependent on praise, will give up easily. Perfectionist personality, will stop if they can’t do it right the first time.
• (Be careful to not use praise with anorexics: don’t tell them that they look good, have gained weight.)
Physical examination – suspected or known eating disorders
• Assess hydration through skin turgor
• Weight and height: ask patient if it is okay if you weigh them.
• Cardio-vascular, EKG, important in chronic cases. Auscultate the heart and palpate the wrist at the same time.
Check that they correspond. If there is a difference, irregularity, RED FLAG FOR EKG. Indicates that there is
irregularity. Assess by counting how often it is happening. Regular irregularity (eg. Every 10 seconds). Irregular
irregularity: happens randomly over time you are assessing.
• Abdominal exam
• Teeth and gums.
• ALWAYS DO VITALS
Case: Anorexic patient, female 27 years old. 80/60, 48bpm. Looked so weak. Hadn’t been to doctor in 6 years. Told her
she had to go that day, went to hospital and held for 3 days, risk of heart failure due to electrolyte imbalance.
Another case: anorexic patient, 82 lbs, will talk about it later. Is taking heroin, risk to heart.
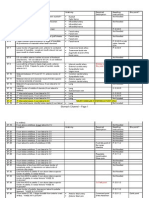
Recommended Lab Tests
• Starred ones: try to get these done if they have access to GP. If requesting, attach info: GP may not have specific
training in eating disorders.
• DEXA (bone density): they may have started to lose bone mass. Think of this if they haven’t menstruated in a year.
Cardiac Complications
• Acrocyanosis: cyanosis in extremities
• Calf pain: hypokalemia: major cation, small window, can supplement with potassium. Severity depends on frequency
of purging/vomiting.
• Dyspnea d/t alkalosis
Heart changes (picture)
• Overlap of valves, disproportionate. Don’t close properly, will start to hear clicks.
Factors for increased cardiac risk
• Co-morbid disorder (DM) increases risk
• Older age: if they have been bulemic for many years. Cumulative stress on body.
Effects on reproductive system
• GnRH release goes to “pre-pubetal” pattern (low intake of precursors?)
• Cysts on ovaries (Not PCOS). Body is shutting down reproductive system.
• Will lose secondary sex characteristics. “Boyish” body, flatter chest, less hair growth, hip development.
• 60% of women seen in infertility clinics with oligomenorrhea: had eating disorder. (study)
• Fats seem to be important factor in ovulation.
Factors contributing to the development of osteoporosis in AN.
• Cortisol is higher, esp. in AN.
• Even if they are doing weight bearing activity (eg. Running), may not be enough to compensate.
• Symptoms go away once they start eating again.
MEN’S AND WOMEN’S HEALTH OCTOBER 11TH, 2007 – PAGE 2
• Fracture risk, may present with bone pain.
• Thyroid: get euthyroid syndrome: normal thyroid that may start behaving abnormally due to low body weight.
GI system:
• Especially with use of laxatives, nerve plexi become numb, hypofunctioning. Cathartic colon syndrome: no function of
colon. Does not typically resolve.
• Slow-moving bowels, persistent. Very hard for them to know they have food sitting in their body.
Flow chart: re bulimia
• Disturbed satiety: sense of satisfaction. When they eat, there is a delayed response in feeling full. Don’t have a
sense of feeling full: keep eating.
• Binge eating gives a high. After eating, get depressed, vomit, get a high, then feel guilt.
• Study of control/bulimic individuals, look at CCK release: they have less released. Physiological change.
• Bulimia: open to psychoeducation: may want to know what it happening in their bodies and this may help them heal.
Anorexics may not be as open to this type of work: already have a lot of information.
• In practice, most likely seeing patients that WANT to change. See some with undisclosed disorder, start by
establishing trust. Then talk indirectly about how they relate to food, body image, they may start talking, feeling safe.
If you are very concerned for their health, may need to be more direct. Risk: they may not come back, although you
may have planted a seed. They may deny it, be offended.
• In family history, may inquire about history of eating disorders… may give them space to disclose.
• Toronto General: In-patient eating disorders clinic. Supervised meals. Food may not be healthy food… Supervised
afterwards to make sure they don’t purge. Monitor heart rate in/out of bathroom, not working out in bathroom.
Red Flags
• High frequency: if they say they purge, have to find out how often. Find out how they do it as well, other risks?
• Best way to get away from shame: talking about it. Painful at first, but gets lighter and starts to dissipate.
• Peripheral edema, especially around lower legs (d/t KI failure)
• Leg cramps, chest pains…
Where to start?
Disclosed:
• Assess stage of awareness of their condition, what the risk is, support system. Have they told anyone? See therapist,
GP? You might be the first person they have told.
PART II
Trauma: separation of spirit from body and mind.
CNC theory: confirmed negativity condition: Negative mind constantly punishing them telling them to exercise, not to eat.
“The secret language of eating disorders”: written by person who developed the CNC theory (being sued)
Trauma and the loss of spirit
• Dissociation: can feel the physical pain, but their mind leaves. Too painful to mentally experience so they separate.
Careful not to probe too deeply, may revert to this state.
• Mind/ego becomes a thing in itself.
• Ego: always wants more, is never satisfied. Nothing is ever good enough. Constantly judging and pushing. Negative
self-talk. (Taming the Monkey Mind –book). Avoidance strategy, to get away from pain.
Binges: an attempt to care for yourself when you don’t know how to. Not healthy, but a coping mechanism.
Effects of Trauma
• “prosecutor” should read “persecutor”
• Incredibly aggressive negative mind. Living with this.
MEN’S AND WOMEN’S HEALTH OCTOBER 11TH, 2007 – PAGE 3
• Flow chart
Theory behind etiology of eating disorders. Can substitute any addictive behaviour in the box that says “bulimia”
• How do you shift the pattern?
• Identification with trauma: if I am not thin, I won’t be liked. This will become what they live for.
• Like being attracted to people that match what you are used to (eg. Family relationships), even if they aren’t good for
you. Like relationship to addition, feels very comfortable, familiar, like home.
How do they relate to other people? This is a reflection of how they relate to themselves.
Inner beliefs:
• Food represents energy, yin energy, it is nurturing. Reject this. Feel that they need nothing/no one
• Deep belief that they aren’t worthy, don’t deserve anything
• Don’t believe they are attractive, have good qualities.
• Beliefs can come from parents, their attitudes to weight, food.
• Film: Through Thick and Thin: interviews with women with bulimia, anorexia. Dr. G. has a copy.
Energetic psychospiritual perspective of addiction
• If they are feeling low, will do something that will cause a spike: binge, purge, run, use drugs. Uncomfortable for them
to sit with their emotions. Technique: ask them to sit and see what happens, be with their emotions. Hard: have to
face where they are at, becoming present. Simple technique. Idea of meditation can be daunting for people. This
might be a good place to start.
• Immediate satisfaction: dissipation of uncomfortable feeling.
• There are layers of emotion: fear. What are they afraid of?
Recovery:
• If you have a good relationship with patient, this is key. Have to keep confidentiality, not disclose to parents, partner
unless they are okay about his. Patient needs to know you are on their side.
• No diets or restrictions! You are adding to their diet
Main treatment goals
• Assiste them to decrease fear of food/living.
• Increase connection to self. Make a list of things they want to do to be healthier and focus on one thing. Make it a
specific goal. They are usually vague to start. Can interpret this in many different ways, not concrete. Help them to
focus on one thing, they will feel better about themselves. Keep it simple and specific.
• Making a commitment to yourself. A vow to yourself.
Process of recovery
• Mourning is a part of the process of recovery. Don’t start with the disappearance of symptoms.
• Someone can spend much time in the early stages.
• May have most pain at beginning of process: they no longer have a distraction from the stuff they were distancing
themselves from.
• Reassure them that feeling bad at beginning is normal.
• Exercise might help, gentle yoga. Greater sense of self-worth, weight gain.
• In order to get better, they have to be willing to think differently.
• NLP: neurolinguistic
• Snakes and ladders: healing is not linear. Will have ups and downs.
• “Goal” may be daunting, try “intention” instead.
• Try to ground the goal. Concrete, specific.
• Journalling: Patients may not like it. Try writing letters, to body, from body.
• Addictions are around “hungers of the soul”. When you are not fed in other aspects, develop patterns that are not
healthy.
• What do you like doing, look at these things. Is there an area of life that is not being addressed?
• Try to stifle something, it pushes back harder. Don’t squelch the negative mind, just provide more positive thoughts.
MEN’S AND WOMEN’S HEALTH OCTOBER 11TH, 2007 – PAGE 4
• Gentle exercise is important. Movement is what is important. Dancing, stretching, run/walking
• Exercises to ground self: lie on grass, sitting, breathing.
Case #1: Weight gain is common in anorexia. Gained 2-3 pounds per week.
Cutting is big concern. Self-mutilation: the only way that they can get release from pain. Where is she cutting?
Case #2: Severe erosion of esophagus, potentially very serious.
Given Holter monitor for heart rate
Decreased exercise to 60 minutes.
Case #4: Parents academics, had lots of pressure to be a good student. Went to private school, high expectations. No
trauma/abuse. Perfection.
Really enjoys sex, likes touch.
Gets mad at boyfriend when he comes over and eats her food.
Carcinosum remedy: 30C in water. After remedy, ate in front of parents at wedding, potassium has increased. “Started to
realize that I’m wasting food, it is ethically wrong”, realized that her boyfriend is a mirror of her. They have attracted each
other. Realized how much pain she has given her mother. Starting to increase awareness.
MEN’S AND WOMEN’S HEALTH OCTOBER 11TH, 2007 – PAGE 5
Potrebbero piacerti anche
- B0dfbaf2 Beed 4ca7 99fb Ff3588d75dc0Documento3 pagineB0dfbaf2 Beed 4ca7 99fb Ff3588d75dc0api-26938624Nessuna valutazione finora
- Diabetes Mellitus and HypoglycemiaDocumento4 pagineDiabetes Mellitus and Hypoglycemiaapi-26938624Nessuna valutazione finora
- Endocrine System IDocumento2 pagineEndocrine System Iapi-26938624Nessuna valutazione finora
- Endocrine System IVDocumento3 pagineEndocrine System IVapi-26938624Nessuna valutazione finora
- Endocrine System IIIDocumento3 pagineEndocrine System IIIapi-26938624Nessuna valutazione finora
- c1fd6bbd Ff7a 480d A20e C93bd3a3cedfDocumento35 paginec1fd6bbd Ff7a 480d A20e C93bd3a3cedfapi-26938624Nessuna valutazione finora
- 13ffd1fa Eda0 4eb8 Bb3a 7802feec40daDocumento40 pagine13ffd1fa Eda0 4eb8 Bb3a 7802feec40daapi-26938624Nessuna valutazione finora
- Endorcine System IIDocumento4 pagineEndorcine System IIapi-26938624Nessuna valutazione finora
- Lecture 47 April 13th-EndocrineDocumento1 paginaLecture 47 April 13th-Endocrineapi-26938624Nessuna valutazione finora
- Lecture 50 April 20th-DiabetesDocumento2 pagineLecture 50 April 20th-Diabetesapi-26938624Nessuna valutazione finora
- Nervous System IIDocumento2 pagineNervous System IIapi-26938624Nessuna valutazione finora
- Lecture 46 April 11th-EndocrineDocumento3 pagineLecture 46 April 11th-Endocrineapi-26938624Nessuna valutazione finora
- Nervous System IDocumento4 pagineNervous System Iapi-26938624Nessuna valutazione finora
- Lecture 48 April 17th-Endocrine (Extra Class)Documento4 pagineLecture 48 April 17th-Endocrine (Extra Class)api-26938624Nessuna valutazione finora
- OP & OA ChartDocumento3 pagineOP & OA Chartapi-26938624100% (1)
- Lecture 49 April 18th-DiabetesDocumento3 pagineLecture 49 April 18th-Diabetesapi-26938624Nessuna valutazione finora
- Lecture 45 April 4th-EndocrineDocumento2 pagineLecture 45 April 4th-Endocrineapi-26938624Nessuna valutazione finora
- Lecture 43 March 28th-NervousDocumento3 pagineLecture 43 March 28th-Nervousapi-26938624Nessuna valutazione finora
- Lecture 39 March 9th-MSKDocumento3 pagineLecture 39 March 9th-MSKapi-26938624Nessuna valutazione finora
- Lecture 44 March 30th - NO NOTESDocumento1 paginaLecture 44 March 30th - NO NOTESapi-26938624Nessuna valutazione finora
- Lecture 42 March 23rd-NervousDocumento2 pagineLecture 42 March 23rd-Nervousapi-26938624Nessuna valutazione finora
- Lecture 41 March 16th-NervousDocumento2 pagineLecture 41 March 16th-Nervousapi-26938624Nessuna valutazione finora
- Conditions of The Musculoskeleltal SystemDocumento4 pagineConditions of The Musculoskeleltal Systemapi-26938624Nessuna valutazione finora
- Lecture 40 March 14th-MSKDocumento5 pagineLecture 40 March 14th-MSKapi-26938624Nessuna valutazione finora
- Extra DDX NotesDocumento1 paginaExtra DDX Notesapi-26938624Nessuna valutazione finora
- DDX - Gastrointestinal Disorders ChartDocumento21 pagineDDX - Gastrointestinal Disorders Chartapi-26938624100% (2)
- Lecture 36 February 28th-Male Genetalia and ReproductionDocumento3 pagineLecture 36 February 28th-Male Genetalia and Reproductionapi-26938624Nessuna valutazione finora
- Lecture 37 March 2nd-RenalDocumento2 pagineLecture 37 March 2nd-Renalapi-26938624Nessuna valutazione finora
- Lecture 35 February 16th-Male Genetalia and ReproductionDocumento3 pagineLecture 35 February 16th-Male Genetalia and Reproductionapi-26938624Nessuna valutazione finora
- Lecture 33 February 7th-Breast and AxillaDocumento4 pagineLecture 33 February 7th-Breast and Axillaapi-26938624Nessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Meralgia ParaestheticaDocumento4 pagineMeralgia ParaestheticaNatalia AndronicNessuna valutazione finora
- Introduction of Magic Rose UpDocumento21 pagineIntroduction of Magic Rose UpanggrainiNessuna valutazione finora
- Standardised Nomenclature of Animal Parasitic Diseases (Snopad)Documento67 pagineStandardised Nomenclature of Animal Parasitic Diseases (Snopad)Pwaveno BamaiyiNessuna valutazione finora
- Written Report Bio 150Documento7 pagineWritten Report Bio 150hyebibieNessuna valutazione finora
- Medical FlyerDocumento2 pagineMedical FlyerThana PalNessuna valutazione finora
- CATHETERIZATIONDocumento3 pagineCATHETERIZATIONrnrmmanphdNessuna valutazione finora
- Sample Questionnaire For Understanding The Self: For Private Use OnlyDocumento6 pagineSample Questionnaire For Understanding The Self: For Private Use Onlyirene ilustrisimo100% (1)
- 13) Technical Guideline On Irritation, Sensitization and Hemolysis Study For Chemical DrugsDocumento36 pagine13) Technical Guideline On Irritation, Sensitization and Hemolysis Study For Chemical DrugsAzam DanishNessuna valutazione finora
- Tap Presentation - Google SlidesDocumento12 pagineTap Presentation - Google Slidesapi-208317298Nessuna valutazione finora
- Systemic Complications of Iv Therapy Complications Assessment Nursing Management Fluid OverloadDocumento4 pagineSystemic Complications of Iv Therapy Complications Assessment Nursing Management Fluid OverloadMakagago And BruskoNessuna valutazione finora
- Why Jaggery? Is Jaggery Healthy? What Is Better: Jaggery or Sugar? Can Jaggery Cure Ailments?Documento5 pagineWhy Jaggery? Is Jaggery Healthy? What Is Better: Jaggery or Sugar? Can Jaggery Cure Ailments?satheb319429Nessuna valutazione finora
- Towards A Sociology of Health Discourse in AfricaDocumento172 pagineTowards A Sociology of Health Discourse in AfricaDavid Polowiski100% (2)
- 2018 Surgical Rescue in Medical PatientsDocumento11 pagine2018 Surgical Rescue in Medical PatientsgiseladlrNessuna valutazione finora
- Long-Term Survey of Tooth Loss in 600 PtsDocumento15 pagineLong-Term Survey of Tooth Loss in 600 PtsAndy HeNessuna valutazione finora
- Nursing Management of HypertensionDocumento152 pagineNursing Management of HypertensionEnfermeriaAncam100% (3)
- Cancer BulletsDocumento3 pagineCancer Bulletsraquel maniegoNessuna valutazione finora
- The Analysis and Reflection On That Sugar FilmDocumento2 pagineThe Analysis and Reflection On That Sugar FilmkkkkNessuna valutazione finora
- Bipolar Disorder - A Cognitive Therapy Appr - Cory F. NewmanDocumento283 pagineBipolar Disorder - A Cognitive Therapy Appr - Cory F. NewmanAlex P100% (1)
- Test Container Form Lab Process Remarks HKL (Hospital Appointment Date - Specialist's SignatureDocumento9 pagineTest Container Form Lab Process Remarks HKL (Hospital Appointment Date - Specialist's SignaturesyasyaNessuna valutazione finora
- Agarwal - Manual of Neuro OphthalmogyDocumento272 pagineAgarwal - Manual of Neuro Ophthalmogythycoon100% (4)
- National Geographic USA - January 2016Documento148 pagineNational Geographic USA - January 2016stamenkovskib100% (4)
- The Nadi Vigyan by DR - Sharda Mishra MD (Proff. in Jabalpur Ayurved College)Documento5 pagineThe Nadi Vigyan by DR - Sharda Mishra MD (Proff. in Jabalpur Ayurved College)Vivek PandeyNessuna valutazione finora
- University of Cambridge International Examinations General Certificate of Education Ordinary LevelDocumento16 pagineUniversity of Cambridge International Examinations General Certificate of Education Ordinary Levelmstudy123456Nessuna valutazione finora
- Bush y FrancisDocumento2 pagineBush y FrancisCarol Artigas100% (1)
- UC San Diego: Independent Study ProjectsDocumento21 pagineUC San Diego: Independent Study ProjectsSoha ShahidNessuna valutazione finora
- Biology Viral DiseasesDocumento11 pagineBiology Viral DiseasesPrasoon Singh RajputNessuna valutazione finora
- Cellular Aberration Acute Biologic Crisis 100 Items - EditedDocumento8 pagineCellular Aberration Acute Biologic Crisis 100 Items - EditedSherlyn PedidaNessuna valutazione finora
- Resource Material - Day 1 Primary Register Activity - ANC Register - 0Documento3 pagineResource Material - Day 1 Primary Register Activity - ANC Register - 0Ranjeet Singh KatariaNessuna valutazione finora
- Peoples of Cambodia 2nd EditionDocumento55 paginePeoples of Cambodia 2nd Editionsummit_go_team100% (1)
- Full Medical Examination Form For Foreign Workers: Work Pass DivisionDocumento1 paginaFull Medical Examination Form For Foreign Workers: Work Pass Divisionkarthik.swamyNessuna valutazione finora