Documenti di Didattica
Documenti di Professioni
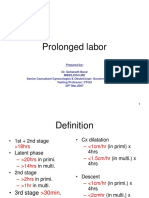
Documenti di Cultura
Milled Bar
Caricato da
jcbchleonDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Milled Bar
Caricato da
jcbchleonCopyright:
Formati disponibili
An implant-supported fixed-removable prosthesis with a milled tissue bar and Hader clip retention as a restorative option for the
edentulous maxilla
Aria Davodi, DDS, a Russell Nishimura, DDS, b and John Beumer III, DDS, MS c
University of Minnesota School of Dentistry, Minneapolis, Minn., and UCLA School of Dentistry, Los Angeles, Calif.
Restoration of the edentulous maxilla with implant retained and supported prosthesis is challenging because of inherent anatomic limitations present after the loss of teeth. A fixed-removable prosthesis is one treatment choice for restoration o f the edentulous maxilla with implants. This prosthesis meets the requirements for esthetics, phonetics, comfort, and hygiene, as well as favorable biomechanical stress distribution to the implants. This article presents a procedure for fabrication of a fixed-removable prosthesis with a precision milled bar, Hader clip attachments, and a superstructure prosthesis. The criteria for patient selection and the advantages and disadvantages of this prosthesis are discussed. (J Prosthet Dent 1997;78:212-17.)
The restoration of the edentulous maxilla with osseointegrated implants is challenging. The quantity of the residual alveolar ridge, its corticocancellous composition, resorptive patterns, presence of anatomic structures such as the incisive foramen, nasal floor, and maxillary sinuses, as well as the maxillomandibular relationship, limit the number, length, and anterior-posterior spread o f i m p l a n t s . A p r o s t h e s i s f a b r i c a t e d on osseointegrated implants must be rigid, provide adequate lip support for esthetics, allow for proper phonetics, and facilitate oral hygiene procedures. Several treatment options have been described for maxillary edentulous patients with implants. 1-8Prosthesis design is based on the amount of alveolar ridge resorption and fulfillment of prosthodontic criteria of support, stability, and retention. When considering the anatomic limitations of an edentulous maxilla, the nccd for a properly designed prosthesis that results in favorable biomechanical stress distribution and fulfillment of patient needs, in regard to esthetics, phonetics, c o m f o r t , and hygiene, an overdenture prosthesis is usually the prosthesis of choice. Wicks 3 described the variables to be considered in determining implant prosthodontic support as number, length, location of implants, and nature ofmucosal support. Typically, patients exhibit an adequate amount of bone in the premaxilla for placement of four implants and fabrication of an overdenture prosthesis supported anteriorly by implants and posteriorly by the residual alveolar ridge. Because of this dual nature of support, one must design an overdenture tissue bar that allows for rotation of the prosthesis along a fulcrum line and
seating of the overdenture base on denture bearing surfaces in function. However, there are patients who have an adequate amount of bone for placement of six or more implants in a curvilinear arrangement that extends beyond the premaxillary segment. A curvilinear arrangement of implants provides more prosthodontic support and stability than a linear arrangement. 9 In designing a prosthesis for these patients, an implant-supported prosthesis that does not derive support from denture bearing tissue may be considered. Prosthodontic treatment options for these patients include a fixed bone anchor partial denture or porcelain fused to metal (PFM) restoration. These prostheses are ideally suited for patients with minimal residual ridge resorption where proper esthetics and phonetics can be achieved. Another option, which has all the advantages of an overdenturc prosthesis in addition to support, stability, and retention characteristics similar to a fixed implantsupported prosthesis, is the hybrid or fixed-removable prosthesis. This concept of prosthesis design has been applied to implant prosthodontics. Lothigius et al. 1-12 have described techniques for fabrication of a hybrid maxillary prosthesis by using attachments. Van RoekeP 3 has described a technique for using electrical discharge machining (spark erosion), which was devised by Sillard, 14to fabricate a fixed-removable prosthesis. The purpose of this article is to describe the criteria and a design used for fabrication of an implant-supported fixed-removable prosthesis with a milled tissue bar and Hader clip retention. SELECTION CRITERIA
~Associate Clinical Professor, Division of Prosthodontics, School of Dentistry, University of Minnesota. bAssistant Professor, Section of Removable Prosthodontics, UCLA School of Dentistry. cprofessor and Chairman, Section of Removable Prosthodontics, UCLA School of Dentistry. 212 THE JOURNAL OF PROSTHETIC DENTISTRY
Careful clinical and radiographic evaluations are conducted to determine whether a patient is a candidate to receive a fixed-removable maxillary prosthesis. Clinical evaluation involves a preliminary diagnostic mounting of maxillary and mandibular casts in centric relation at the proper vertical dimension of occlusion on a
VOLUME 78 NUMBER 2
DAVODI, NISHIMURA, AND BEUMER
THE JOURNAL OF PROSTHETIC DENTISTRY
semiadjustable articulator with a face-bow transfer. For this purpose, the patient's existing denture or dentures can be duplicated if functionally and esthetically acceptable, otherwise, a preliminary arrangement of artificial teeth in wax may be necessary. Radiographic analysis of quantity, quality, and anatomic architecture of the residual bone should be performed with computerized t o m o g r a p h y (CT). On the basis of the patient's needs and the diagnostic information obtained, a decision to fabricate a fixed-removable prosthesis is made if the following criteria are met. Because support for this type of a prosthesis is derived primarily from implants, the placement of six or more implants is recommended. To design a restoration that is biomechanically sound, sufficient bone must exist for a curvilinear arrangement o f implants so that a 20 m m anterior-posterior spread o f implants is present. Superior biomechanical stress distribution patterns to the surrounding bone with greater anterior-posterior spread o f implants has been r e p o r t e d ) s 18 The length of the most distal implants bilaterally is important. Because of poor bone quality in the posterior maxilla and based on documentation o f higher failure rates for shorter implants in the posterior maxilla, I9-21 a m i n i m u m implant length of 1 3 mm is recommended for the most distal implants. Distal cantilevers are best avoided or confined to a minimum length. 22-2aThe determination of adequate interocclusal space is based on minimum prosthodontic requirements o f tissue bar height for rigidity, adequate thickness o f the superstructure casting, and the necessary a m o u n t of acrylic resin to encompass the artificial denture teeth and impart structural integrity and strength. CLINICAL PROCEDURES
Fig. 1. Mounted piaster index of arranged artificial teeth.
Fig. 2. Hader bar attachments positioned in between distal most implants bilaterally avoiding cantilevers.
LABORATORY 1.
PROCEDURES
The clinical procedures involved in fabricating a fixedremovable prosthesis are similar to fabrication of an implant and tissue-supported overdenture. 1. Assess the gingival tissue height circumscribing the implants at or after second stage implant surgery. Recontour any excessive gingival tissue that is coronal to the top of implants so that a maintainable periimplant gingival pocket is established. 2. After soft tissue healing, make a preliminary impression at the implant level with pick-up type impression copings. Fabricate a master cast. 3. Make a face-bow transfer and an interocclusal record at the proper vertical dimension of occlusion and in centric relation. M o u n t the maxillary and mandibular casts on a semiadjustable articulator. 4. Perform a wax try-in of the selected artificial teeth to ensure proper tooth position for lip support, esthetics, phonetics, and verification of the interocclusal record. Establish the position of the artificial teeth to allow for evaluation of the amount of space available for proper tissue bar fabrication.
AUGUST 1997
2.
3.
4.
Fabricate a plaster index incorporating the incisal edges and cusps of the artificial teeth. M o u n t the index to capture the spatial relationship of the artificial teeth to the residual alveolar ridge (Fig. 1). Remove the artificial teeth and lute them to the index with sticky wax (Kerr Manufacturing Co., Romulus, Mich.). Select the abutments and assemble on the master cast. [Typically, the U C L A abutment is selected because of its flexibility in solving angulation, proximity, and space problems. ] Wax the tissue bar to proper contours, allowing for access to peri-implant tissue for hygiene and approximation of the occlusal contacts of the artificial teeth along the long axis of the implants. Survey the bar to determine a path of insertion of the superstructure and tripodize the master cast. Incorporate Hader bar (Lifecore Biomedical Inc., Chaska, Minn.) plastic patterns within the tissue bar in line with the determined path of insertion, connecting the anterior most implants, and cantilevering distal to the posterior implants bilaterally. [If
213
THE JOURNAL OF PROSTHETIC DENTISTRY
DAVODI, NISHIMURA, AND BEUMER
Fig. 3. A, Tissue bar placed on milling machine and circumferentially milled at 2-degree taper.
B, Milled tissue bar, palatal contours. C, Milled tissue bar inserted.
sufficient space exists between the distal most implants, a cantilever segment is avoided by placing the Hader bar plastic patterns between the distal most implants parallel to the anterior Hader bar segment (Fig. 2).] 5. Perform a preliminary milling of the waxed tissue bar to create parallel labial and palatal walls that coincide with the path of insertion of the superstructure. Section, sprue, invest, and cast the wax pattern in a gold palladium alloy (250SL, Leach and Dillon, North Attleboro, Mass.). 6. Devest the casting, remove the sprues, and finish under magnification (10) to remove any casting irregularities such as blebs, nicks, or flash. Try-in the tissue bar segments and examine the fit clinically and radiographically.Additional sectioning may be necessary to ensure passive and accurate seating of all segments. 7. Assemble the s e g m e n t s i n t r a o r a l l y with autopolymerizing resin (GC Pattern Resin, GC Corp., Tokyo, Japan) and a type 2 piaster index (Kerr Manufacturing Corp.). Connect soldering analogs to the segments and fabricate an accurate soldering index with a type IV stone (Die Keen, Bayer Corp., South Bend, Ind.). Solder the sections together and verify the fit on the soldering index.
214
If any discrepancy or rocking exists, section and resolder the bar. When the soldered bar fits the soldering index accurately in all dimensions, perform a clinical try-in. Once satisfied with the accurate and passive fit of the tissue bar clinically and radiographically, substitute guide pins for seating screws. 9. Fabricate a custom impression tray, properly mold the labial and buccal contours in compound, and make an impression in light body polysulfide impression material (Kerr Manufacturing Co. ) incorporating the tissue bar. Connect laboratory analogs to the tissue bar and fabricate a master cast. Place the master cast tissue bar assembly on a milling machine (Degussa, Frankfurt, Germany) survey to the path of insertion of the superstructure casting and tripodize cast. Use a milling bur (Brassler USA, Savannah, Ca.) with a 2 - d e g r e e taper to circumferentially mill the tissue bar on palatal and labial surfaces (Fig. 3, A through C). 10. Once the tissue bar contours are finalized on the master cast, fabricate a tissue bar retained record base and make a face-bow transfer record, using all previous reference points. Mount the master cast against the plaster index that incorporated the previously arranged artificial teeth and assess the
VOLUME 78 NUMBER2
8.
DAVODI, NISHIMURA, AND BEUMER
THE JOURNAL OF PROSTHETIC DENTISTRY
Fig. 4. Completed superstructure prosthesis housing plastic Hader clips.
amount of space available for superstructure fabrication. 11. Position the master cast tissue bar assembly on a tripod to the set marks, block out all undercuts and screw access channels in wax, and make an impression in m e d i u m viscosity vinyl polysiloxane (Reprosil, Dentsply International Inc.) to provide a refractory cast for the development of the superstructure wax pattern. 12. Bead the refractory cast at the desired palatal extensions of the superstructure and complete the wax pattern. Incorporate wax beads (California Dental Products Inc., North Hollywood, Calif.) in the superstructure wax pattern to enhance mechanical retention for acrylic resin processing. 13. Sprue, invest, and cast the superstructure wax pattern in a metal similar to that of the tissue bar. Remove all casting irregularities under magnification (10x) and fit the cast superstructure to the tissue bar with a disclosing medium (Fit Checker, GC Corp.). 14. Carefully adjust the cast Hader clip housings, incorporated within the superstructure, to allow for easy placement and removal of the plastic Hader clips. Mount the master cast, tissue bar, superstructure assembly on the articulator against the plaster index that incorporates the arranged artificial teeth. 15. Transfer the artificial teeth to the superstructure with extra-hard set-up wax (Bayer Corp.) and perform a final clinical try-in to assess esthetics, phonetics, and verify vertical dimension and maxillomandibular relationships. 16. Condition the superstructure casting with a metal primer (GC Corp.) and process the overdenture in heat-polymerizing acrylic resin (Lucitone, Dentsply International Inc.). [ Opaquing of the metal superstructure is often necessary and is performed before pacldng of the acrylic resin with an opaquing medium ( D e n t a c o l o r Opaker, Heraeus Kulzer, Wehrheim, Germany). ] 17. After processing, perform a laboratory remount to
AUGUST 1997
Fig. 5. A, Incorporation of amalgam centric stops to reduce occlusal wear. B, Superstructure casting designed with custom metal occlusion to reduce occlusal wear.
correct processing errors. Complete all finishing and polishing procedures of the bar and overdenture, insert new plastic Hader clips, and deliver prosthesis to the patient (Fig. 4). PROSTHESIS DELIVERY On delivery of the prosthesis, care is taken to properly adjust the new plastic Hader clips to facilitate insertion and removal of the overdenture. The indirect retention provided by the engagement of the superstructure casting and the milled tissue bar and the direct retention provided by the Hader clips may make prosthesis insertion and removal difficult for some patients. Patients are asked to practice insertion and removal of the overdenture in the presence of the dentist. Patients are also given oral hygiene instructions for peri-implant plaque control and maintenance of the removable overdenture prosthesis. Patients are encouraged to remove the prosthesis at bedtime and keep the prosthesis hydrated.
DISCUSSION
Given the difficulties encountered in restoring the edentulous maxilla with an implant-supported prosthesis, a fixed-removable prosthesis with a precision milled
215
THE JOURNAL OF PROSTHETIC DENTISTRY
DAVODI, NISHIMURA, AND BEUMER
bar has proven to be an efficient, cost-effective treatment. Currently, such a prosthesis is prescribed for patients who meet the selection criteria described herein and for patients who have experienced severe bone loss in the maxillary arch where implant placement can only be accomplished after osseous grafting procedures. There are several advantages to such a prosthesis. The intimate adaptation of the secondary casting to the milled bar provides added retention and stability not available in implant- and tissue-supported prostheses. The prosthesis is rigid, it splints the implants, and is minimally cantilevered (or lacks cantilevering), which results in a favorable biomechanical design. Adequate esthetics and phonetics are achieved as a result of the ability to properly form labial and palatal contours in moldable compound. Proper oral hygiene procedures can be performed by patients, and minimal soft tissue coverage by the superstructure promotes mucosal health. The plastic replaceable clips can be removed and reinserted to provide easy serviceability of the attachment system. The laboratory procedures involved in fabricating this type of a prosthesis do not differ substantially from conventional implant laboratory techniques. A local dental laboratory with a milling machine can perform the mechanical milling procedures making prosthesis fabrication practical and economical. By comparison, a fixed-removable implant prosthesis fabricated with electrical discharge machining technology requires special equipment, which is not available to most dental laboratories and is significantly more expensive. The experience of the authors of this article has shown that this type of a prosthesis has been well-received by patients. The prosthesis function is similar to that of a fixed implant prosthesis because of its enhanced stability and retention and because the wear rate of the plastic Hader clips is significantly reduced, the need for prosthesis maintenance has been minimal. Although there are many advantages to this prosthesis, proper execution of all clinical and laboratory procedures requires lcnowledge of important laboratory techniques and clinical skills. The amount of tissue bar wear, as a result of engagement of the superstructure, must be critically investigated; however, initial observations have not revealed significant wear. Finally, special attention must be paid to the occlusal materials and scheme used in designing a fixed-removable prosthesis. A fixed-removable prosthesis functions in a manner similar to a fixed implant-supported prosthesis. Accelerated wear of artificial teeth has been observed when the prosthesis opposes natural or restored dentitions. Occlusal wear can be reduced by placement of amalgam plugs in the artificial teeth as centric stops, incorporation of custom metal occlusal surfaces on the superstructure, or use of porcelain artificial teeth if sufficient space is available for processing of acrylic resin (Fig. 5, A and B). The occlusal scheme selected for a fixed-removable prosthesis is group
216
function. The lateral and protrusive paths of excrusion of artificial teeth must be in coordination with condylar paths of movement. This coordination is important in reducing the transfer ofnonaxial loads to implants, especially when opposed by natural or restored dentition or fixed implant restorations. Hence, obtaining accurate condylar movement records, such as a stereographic recording, is recommended.
CONCLUSION
The application of a fixed-removable implant prosthesis with a milled tissue bar, Hader clip attachments, and a superstructure casting for treatment of complete maxillary edentulous jaw has been presented. Selection criteria, clinical and laboratory procedures, and advantages and disadvantages of this type of a prosthesis have been discussed. A fixed-removable prosthesis with a milled tissue bar and a superstructure casting can also be used for restoration of mandibular edentulous jaw, selected maxillofacial resection patients, and partially edentulous patients with proper patient selection and design criteria.
REFERENCES
1. Desjardins RP. Prosthesis design for osseointegrated implants in the edentu[ous maxilla. Int J Oral MaxiHofac Implants 1992;7:311-20. 2. Zarb GA, Schmitt A. Implant prosthodontic treatment options for the edentulous patient. J Oral Rehabil 1995;22:661-71. 3. Wicks RA. A systematic approach to definitive planning for osseointegrated implant prostheses. J Prosthodont 1994;3:237-42. 4. Taylor TD. Fixed implant rehabilitation for the edentulous maxilla, lnt J Oral Maxillofac Implants 1991;6:329-37. 5. DeBoer J. Edentulous implants: overdenture versus fixed. J Prosthet Dent 1993;69:386-90. 6. Laney WR. Selecting edentulous patients for tissue-integrated prostheses. Int J Oral Maxillofac Implants 1986;1:129-38. 7. Lekholm U, Zarb GA. Patient selection and preparation. In: Br~nemark PI, Zarb GA, Albrektssoon T, editors. Tissue-integrated prostheses: osseointegration in clinical dentistw. Chicago: Quintessence; 1985. p. 199-209. 8. Eckert SE, Laney WR. Patient evaluation and prosthodontic treatment planning for osseointegrated implants. Dent Clin North Am 1989;33:599-618. 9. Rangert B, Jemt T, Jorneus L. Forces and moments on Br~nemark implants. IntJ Oral Maxillofac Implants 1989;4:241-7. 10. Lothigius E, Smedberg JI, De Buck V, Nilner K. A new design for a hybrid prosthesis supported by osseointegrated implants: 1. Technical Aspects. Int J Oral Maxillofac Implants 1991 ;6:80-6. 11. Smedberg JK, Lothigius E, Nilner K, De Buck V. A new design for a hybrid prosthesis supported by osseointegrated implants: 2. Preliminary clinical aspects. Int J Oral Maxillofac Implants 199 I;6:154-9. 12. Kramer A, Weber H, Benzing U. Implant and prosthetic treatment of the edentulous maxilla using a bar-supported prosthesis. Int J Oral Maxillofac Implants 1992;7:251-5. 13. Van Roekel NB. Prosthesis fabrication using electrical discharge machining. Int J Oral Maxi[Iofac Implants 1992;7:56-61. 14. Sillard R. Fixed removable dental implants system. US Patent No. 4,931,016, June 5, 1990. 15. Benzing UR, Gall H, Weber H. Biomechanica[ aspects of two different implant-prosthetic concepts for edentulous maxillae. Int J Oral Maxillofac Implants 1995;10:188-98. 16. Brunski JB. Forces on dental implants and interfacial stress transfer. In: Laney WR, Tolman DE, editors. Tissue integration in oral, orthopedic, and maxillofacial reconstruction. Chicago: Quintessence; 1992. p. 108-24. 17. Brunski JB, Skalak R. Biomechanical considerations. In: Worthington P, Brfinemark P-I, editors. Advanced osseointegration surgery: applications in the maxillofacial region. Chicago: Quintessence; 1992. p. 15-39. 18. Davis DM, Zarb GA, Chao YL. Studies on frameworks for osseointegrated
V O L U M E 78
NUMBER2
DAVODI, NISHIMURA, AND BEUMER
THE JOURNAL OF PROSTHETIC DENTISTRY
19.
20. 21.
22. 23.
prostheses: part 1. The effect of varying the number of supporting abutments. Int J Oral Maxillofac Implants 1988;3:197-201. Friberg B, Jemt T, Lekholm U. Early failures in 4,641 consecutively placed Br~nemark dental implants: a study from stage 1 surgery to the connection of completed prostheses. Int J Oral Maxillofac Implants 1991 ;6:142-6. Moy P, Bain C. Relation between the fixture length and implant failure(Abstract). J Den Res 1992;72:637. ]emt T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Br~nemark implants in edentulous jaws: a study of treatment from the time of prosthesis placement to the first annual checkup. IntJ Oral Maxillofac Implants 1991;6:270-6. White SN, Caputo AA, Anderkvist T. Effect of cantilever length on stress transfer by implant-supported prosthesis. J Prosthet Dent 1994;71:493-9. Lewinstein I, Banks-Sills L, Eliasi R. Finite element analysis of a new system (IL) for supporting an implant-retained cantilever prosthesis. Int J Oral Maxillofac Implants 1995;10:355-66.
24. Tashkandi EA, Lang BR, Edge ME. Analysis of strain at selected bone sites of a cantilevered implant-supported prosthesis. J Prosthet Dent 1996;76:158-64. 25. Sertgoz A, Guvener S. Finite element analysis of the effect of cantilever and implant length on stress distribution in an implant-supported fixed prosthesis. J Prosthet Dent 1996;76:165-9. Reprint requests to: DR. ARIADAVODI 516 FIFTHST. SE-#4 M]NNEAPOUS,MN 55414 Copyright 1997 by The Editorial Council of The Journal of Prosthetic Den-
tistry.
0022-3913/97/$5.00 + 0. 10/1/82807
The single unit, single retainer, cantilever resin-bonded bridge Briggs P, Dnnne S, Bishop K. Br DentJ 1996;81:373-9. Purpose. Although resin-bonded bridges (RBBs) have become routinely used in clinical practice, several doubts remain about the long-term reliability of these restorations. These doubts include: clinical performance of RBBs is variable; "gray out" of metal wings are cosmetically unacceptable; unnoticed partial decementation can lead to dental caries; little agreement as to optimal RBB design; moisture control is difficult to achieve during cementation; temporization and occlusion is diffictflt to achieve; and the possibility exists of swallowing or inhaling a RBB if it debonds. This article describes the clinical function and the importance in clinical practice of the single abutment, single pontic cantilever resin-bonded bridge (CRRB) as an alternative to a fixed two abutment retained RBB. Material and Methods. Fifty-four single abutment, single pontic cantilever resin-bonded bridges (CRRB) were evaluated over time ranging from 1 to 82 months (mean 26.7 months). Forty-six (85%) where placed in the maxilla, while eight (15%) were placed in the mandible. Of the CRRB, 61% were cemented in the anterior region, 11% in the anterior/posterior region(canine/premolar), and 28% in the posterior region. Results. Eleven (20%) of the 54 CRRB debonded during the study period and the mean time before debond was 8 months. O f these debonds, eight (73%) were recemented and these restorations continued to be in clinical service to the end of the study. The remaining debonded CRRBs required remake or retreatment planning. O f the debonds, 91% (10) occurred in the maxillae and 9% (1) in the mandible. Discussion. The clinical performance of CRRBs in this study is comparable to other studies of RBBs, in that they tended to perform better than fixed two abutment retained RBBs. The authors discuss the factors affecting the clinical performance of the CRBB that included retainer design, abutment preparation, pontic features, occlusion, metal preparation and cementation, periodontal factors, and creation of sufficient interocclusal distance. Conclusions. This study highlights the good clinical potential for using the single unit, single abutment CRRB in dental practice. Results support other clinical studies. The authors stress the need for further clinical studies to compare the clinical performance of this design with other RBB designs and to evaluate the role of the full coverage retainer in terms of clinical performance of the CRRB. 28 references.--RPRenner
AUGUST 1997
217
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- WHO List of Books, 2006Documento161 pagineWHO List of Books, 2006Joenabie Andoy Encanto100% (1)
- Shi HeziDocumento54 pagineShi HeziDr-Mirza BaigNessuna valutazione finora
- Medical Record WikipediaDocumento4 pagineMedical Record WikipediaRisma KurniaNessuna valutazione finora
- Medicinos Anglu KnygaDocumento76 pagineMedicinos Anglu KnygaJigglypuff166Nessuna valutazione finora
- Obstetric Emergencies PDFDocumento15 pagineObstetric Emergencies PDFEdi BackyNessuna valutazione finora
- Research PaperDocumento14 pagineResearch Paperapi-455600000Nessuna valutazione finora
- The Pharmacist Guide To Implementing Pharmaceutical Care PDFDocumento502 pagineThe Pharmacist Guide To Implementing Pharmaceutical Care PDFLuis SosaNessuna valutazione finora
- Prolonged Labor Diagnosis and ManagementDocumento8 pagineProlonged Labor Diagnosis and ManagementMadhu Sudhan PandeyaNessuna valutazione finora
- ReportsDocumento2 pagineReportssawtulhassanNessuna valutazione finora
- Parecoxib PDFDocumento7 pagineParecoxib PDFawardani13Nessuna valutazione finora
- Penjagaan Temporary CatheterDocumento28 paginePenjagaan Temporary Catheterdev05_926413Nessuna valutazione finora
- Opthhalmology Examination ReviewDocumento12 pagineOpthhalmology Examination ReviewFaiq Syukri Bin SaparudinNessuna valutazione finora
- Oncology QuestionsDocumento3 pagineOncology QuestionsWilma BaludoNessuna valutazione finora
- Operative SurgeryDocumento119 pagineOperative SurgerySubhrajyoti Banerjee100% (2)
- 37-Pediatrics & NeonatologyDocumento11 pagine37-Pediatrics & NeonatologyIbrahimFikryNessuna valutazione finora
- Epidural AnaesthesiaDocumento18 pagineEpidural Anaesthesiarainbow rainNessuna valutazione finora
- Nurse's Role in Maternal-Child HealthcareDocumento2 pagineNurse's Role in Maternal-Child HealthcareHannaNessuna valutazione finora
- Final exam questions on obstetrics and gynaecologyDocumento1 paginaFinal exam questions on obstetrics and gynaecologySlashy HeugotNessuna valutazione finora
- AppendicitisDocumento7 pagineAppendicitisTim LuoNessuna valutazione finora
- Ra 9288Documento8 pagineRa 9288UlaysaNessuna valutazione finora
- 1 s2.0 S0007193505800223 MainDocumento12 pagine1 s2.0 S0007193505800223 Mainadamos1945Nessuna valutazione finora
- Cupping PointsDocumento9 pagineCupping PointsAna JacintaNessuna valutazione finora
- Primary Secondary Skin Lesions 2003Documento32 paginePrimary Secondary Skin Lesions 2003Louisa Abigail D'CruzNessuna valutazione finora
- Partogram CORRECTEDDocumento45 paginePartogram CORRECTEDjayasankariNessuna valutazione finora
- Medscape Hypovolemic ShockDocumento14 pagineMedscape Hypovolemic ShockSarah Ovinitha100% (1)
- Portable Oxygen - Use and Care GuidelinesDocumento4 paginePortable Oxygen - Use and Care GuidelinesMikeNessuna valutazione finora
- Baseball Diamond Concept for Optimal Port Placement in LaparoscopyDocumento27 pagineBaseball Diamond Concept for Optimal Port Placement in LaparoscopyAhsan Jamil100% (1)
- Pediatric Surgery Diagnosis and TreatmentDocumento460 paginePediatric Surgery Diagnosis and TreatmentPatricia Beznea100% (2)
- Bishwajit MazumderDocumento4 pagineBishwajit MazumderBishwajitMazumderNessuna valutazione finora
- Pregnancy Constipation and DiarrheaDocumento15 paginePregnancy Constipation and DiarrheaAry GuhtamaNessuna valutazione finora