Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Adult: PO HTN Initial: 50-100 Mg/day in Single or Divided Doses Increase Slowly
Caricato da
Joanna Marie Lumbre BalbiranDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Adult: PO HTN Initial: 50-100 Mg/day in Single or Divided Doses Increase Slowly
Caricato da
Joanna Marie Lumbre BalbiranCopyright:
Formati disponibili
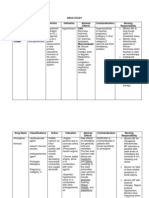
Indications Dosage
Listed in Dosage. Adult: PO HTN Initial: 50-100 mg/day in single or divided doses; increase slowly according to response. Maintenance: 100-200 mg/day. Extended-release 25-100 mg once daily. Angina pectoris 50-100 mg 2-3 times/day. Cardiac arrhythmias 50 mg 2-3 times/day; up to 300 mg/day in divided doses if needed. Adjunct inhyperthyroidism 50 mg 4 times/day. Migraine prophylaxis 100-200 mg/day in divided doses. Adjunct in the early management of acute MI 100 mg twice daily once clinical condition of patient is stable. Stable symptomatic heart failure As succinate: Extended release Initial: 12.5-25 mg of equiv metoprolol tartrate dose. Increase slowly as needed. Max: 20 mg once daily. IV Emergency treatment of cardiac arrhythmias Initial: 5 mg at a rate of 1-2 mg/min; repeat at 5-min intervals if needed up to a total of 10-15 mg. Maintenance via oral therapy: 50 mg 3 times/day 4-6 hr after IV regimen. Prevention or control of arrhythmias on induction of anesth2-4 mg as slow inj; repeat as needed. Max total: 10 mg. Adjunct in the early management of acute MI Administer w/in 12 hr of the onset of chest pain, 5 mg at 2-min intervals to a total of 15 mg, if tolerated. After 15 mins, initiate oral therapy at 50 mg 6 hrly for 2 days for patients who received the full IV dose. Subsequent maintenance: 100 mg PO twice daily. Click to view metoprolol Dosage by Indications May be taken with or without food. For action to be taken in the event of accidental overdose ... click to view metoprolol 2nd or 3rd degree AV block; sick sinus syndrome; decompensated heart failure; clinically relevant sinus bradycardia. Severe peripheral arterial circulatory disorders. Cardiogenic shock. Asthma. Phaeochromocytoma (without -blockade), systolic BP <100 mmHg. Metabolic acidosis. Pregnancy (2nd and 3rd trimesters). Compensated heart failure, bronchospastic disease, hepatic impairment, AV conduction disorders, bradycardia, peripheral arterial circulatory disorders. An blocker should be given concurrently in patients with phaeochromocytoma. May mask signs of acute hypoglycaemia. May mask symptoms of hyperthyroidism. Caution when used in patients with history of cardiac failure or those with minimal cardiac reserve. Avoid using anaesthetic agents that may depress the myocardium. May impair ability to drive or operate machinery. Myasthenia gravis; history of psychiatric disorder. Lactation. Avoid abrupt drug withdrawal. Bradycardia, hypotension, arterial insufficiency, chest pain, CHF, oedema, palpitation, syncope, gangrene; dizziness, fatigue, depression, confusion, headache, insomnia, short-term memory loss, nightmares, somnolence; pruritus, rash, increased psoriasis, reversible alopecia; sexual dysfunction/impotence, Peyronie's disease; diarrhoea, constipation, flatulence, GI pain, heartburn, nausea, xerostomia; agranulocytosis (rare); musculoskeletal pain; blurred vision, dry eyes, oculomucocutaneous syndrome; tinnitus; dyspnoea, bronchospasm, wheezing, rhinitis; cold extremities. Potentially Fatal: Heart failure, heart block, bronchospasm. Additive effect with catecholamine-depleting drugs e.g. reserpine and MAOIs. May antagonise 1-adrenergic stimulating effects of sympathomimetics. Additive negative effects on SA or AV nodal conduction with cardiac glycosides, nondihydropyridine calcium-channel blockers. Increased oral bioavailability with aluminium/magnesiumcontaining antacids. Paradoxical response to epinephrine may occur. Increased plasma concentrations with CYP2D6 inhibitors (e.g. bupropion, cimetidine, diphenhydramine, fluoxetine, hydroxycholoquine, paroxetine, propafenone, quinidine, ritonavir, terbinafine, thioridazine). Increased risk of hypotension and heart failure with myocardial depressant general anaesthetics (e.g. diethyl ether). Risk of pulmonary hypertension
Administration Overdosage Contraindications
Special Precautions
Adverse Drug Reactions
Drug Interactions
with vasodilators e.g. hydralazine in uraemic patients. Reduced plasma levels withrifampicin. May increase negative inotropic and negative dromotropic effect of anti-arrhythmic drugs e.g. quinidine and amiodarone. Propafenone may increase serum levels of metoprolol. Concurrent use with indomethacin may reduce the antihypertensive efficacy of -blocker. May reduce clearance of lidocaine. May increase effects of hypoglycaemics. Efficacy may be reduced by isoprenaline. Concurrent use with digoxin may lead to additive bradycardia. Potentially Fatal: Additive or synergistic effects with verapamil; increased oral bioavailability with verapamil. Exacerbation of rebound hypertension during abrupt clonidine withdrawal. Click to view more metoprolol Drug Interactions Food Interaction Pregnancy Category (US FDA) Category C: Either studies in animals have revealed adverse effects on the foetus (teratogenic or embryocidal or other) and there are no controlled studies in women or studies in women and animals are not available. Drugs should be given only if the potential benefit justifies the potential risk to the foetus. For caution against potential drug-food interactions ... click to view metoprolol
in 2nd & 3rd trimesters. Category D: There is positive evidence of human foetal risk, but the benefits from use in pregnant women may be acceptable despite the risk (e.g., if the drug is needed in a life-threatening situation or for a serious disease for which safer drugs cannot be used or are ineffective). MIMS Class ATC Classification Beta-Blockers / Antimigraine Preparations C07AB02 - Metoprolol ; Belongs to the class of selective beta-blocking agents. Used in the treatment of cardiovascular diseases. MOA = Metoprolol selectively inhibits -adrenergic receptors but has little or no effect on 2-receptors except in high doses. It has no membrane-stabilising nor intrinsic sympathomimetic activity. Indications Dosage Listed in Dosage. Adult: PO Benign gastric and duodenal ulceration 40 mg/day at bedtime for 4-8 wk. GERD 20 mg twice daily for 6-12 wk. May continue to prevent recurrence. Zollinger-Ellison syndrome Initial: 20 mg 6 hrly, up to 800 mg/day if needed. Dyspepsia 10 mg twice daily. IV Benign gastric and duodenal ulceration 20 mg 12 hrly. Click to view famotidine Dosage by Indications May be taken with or without food. Hypersensitivity; lactation. Impaired renal function, liver cirrhosis; pregnancy. Possibility of malignancy should be considered prior to initiating treatment as drug may mask symptoms and delay diagnosis. No safety and efficacy data is available for children <1 yr. Headache, dizziness, constipation, diarrhoea, nausea, rash, GI discomfort, fatigue, gynaecomastia, impotence. Reduced absorption of famotidine with antacids hence admin should be separated by 2 hr. Reduced absorption of ketoconazole and itraconazole. Avoid ethanol (may cause gastric mucosal irritation).
Administration Contraindications Special Precautions
Adverse Drug Reactions Drug Interactions
Pregnancy Category
(US FDA) Category B: Either animal-reproduction studies have not demonstrated a foetal risk but there are no controlled studies in pregnant women or animal-reproduction studies have shown an adverse effect (other than a decrease in fertility) that was not confirmed in controlled studies in women in the 1 st trimester (and there is no evidence of a risk in later trimesters). MIMS Class ATC Classification Antacids, Antireflux Agents & Antiulcerants A02BA03 - Famotidine ; Belongs to the class of H2-receptor antagonists. Used in the treatment of peptic ulcer and gastro-oesophageal reflux disease (GERD). MOA - Famotidine competitively blocks histamine H2-receptors thus reducing basal, nocturnal and stimulated gastric acid secretion. Pepsin secretion is reduced resulting in decreased peptic activity. It effectively heals duodenal and gastric ulcers and prevents recurrence. Indications Dosage Listed in Dosage. Adult: PO Allergic conditions As HCl: 25-50 mg 3-4 times/day. Max: 300 mg/day. Prevention and treatment of motion sickness As diphenhydramine di (acefyllinate): Usual: 90-135 mg, may repeat if needed at intervals of at least 6 hr. Max: 540 mg/day. IV/IM Allergic conditions As 1 or 5% soln: As HCl: 10-50 mg, up to 100 mg. Not more than 400 mg/24 hr. Click to view diphenhydramine Dosage by Indications May be taken with or without food. For action to be taken in the event of accidental overdose ... click to view diphenhydramine Hypersensitivity ; neonates, lactation. Epilepsy; elderly; performing tasks which require mental alertness; angle-closure glaucoma; pyroduodenal obstruction; urinary tract obstruction; hyperthyroidism; raised intraocular pressure; CV disease; acute asthma; pregnancy. CNS depression, dizziness, headache, sedation; paradoxical stimulation in children; dryness of mouth, thickened respiratory secretion, blurring of vision, urinary retention; GI disturbances; blood dyscrasias. Masks ototoxicity produced by aminoglycosides. Increases gastric degradation of levodopa and decreases its absorption by reduction of gastric emptying. Antagonises therapeutic effects of cholinergic agents e.g. tacrine, donezepil and neuroleptics. Valerian, St. John's wort, Kava Kava and gotu kola may increase CNS depression. Potentially Fatal: Potentiates CNS depression with alcohol, barbiturates, analgesics, sedatives and neuroleptics. Additive antimuscarinic action with MAOIs, atropine and TCAs. Click to view more diphenhydramine Drug Interactions
Administration Overdosage Contraindications Special Precautions
Adverse Drug Reactions Drug Interactions
Pregnancy Category (US FDA) Category B: Either animal-reproduction studies have not demonstrated a foetal risk but there are no controlled studies in pregnant women or animal-reproduction studies have shown an adverse effect (other than a decrease in fertility) that was not confirmed in controlled studies in women in the 1 st trimester (and there is no evidence of a risk in later trimesters). MIMS Class Antihistamines & Antiallergics MOA - Diphenhydramine blocks histamine H1-receptors on effector cells of the GI tract, blood vessels and respiratory tract. It also causes sedation and has some anticholinergic action.
Potrebbero piacerti anche
- Drug Study TramadolDocumento14 pagineDrug Study TramadolBianca Freya Porral85% (13)
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesDa EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesValutazione: 4 su 5 stelle4/5 (2)
- Microbiology CaseDocumento3 pagineMicrobiology Caseclower112100% (2)
- Wound Documentation TipsDocumento4 pagineWound Documentation TipsLaura Hernandez100% (1)
- RiteMED MetoprololDocumento7 pagineRiteMED MetoprololAngie MandeoyaNessuna valutazione finora
- Drug StudyDocumento10 pagineDrug StudyFranco ObedozaNessuna valutazione finora
- Drugs AufDocumento6 pagineDrugs AufBrian OballoNessuna valutazione finora
- Drug StudyDocumento4 pagineDrug Studyjazmine_caritos100% (2)
- 8 Drug StudyDocumento19 pagine8 Drug StudyLoyloy D ManNessuna valutazione finora
- Hemostan, Methergine CA Gluconate2Documento4 pagineHemostan, Methergine CA Gluconate2Stacy MC PelitoNessuna valutazione finora
- Drug StudyDocumento3 pagineDrug Studyanon_11638632Nessuna valutazione finora
- LI Case 2 (Pharmacological Properties of Propanolol)Documento2 pagineLI Case 2 (Pharmacological Properties of Propanolol)adtyadaviaNessuna valutazione finora
- Solian SMPCDocumento20 pagineSolian SMPCyanal.bisharat.mspharmaNessuna valutazione finora
- Adrenergic Blockers AtenololDocumento3 pagineAdrenergic Blockers AtenololPoinsithia OrlandaNessuna valutazione finora
- Ipratropium BromideDocumento20 pagineIpratropium BromideAngelique Ramos PascuaNessuna valutazione finora
- Metformin Hydrochloride PDFDocumento4 pagineMetformin Hydrochloride PDFHannaNessuna valutazione finora
- Labs Drug Study 1Documento17 pagineLabs Drug Study 1Drei LanuzoNessuna valutazione finora
- Formulary 3rd Shifing AudsDocumento81 pagineFormulary 3rd Shifing AudsSheila Lyn LacsonNessuna valutazione finora
- Furosemide Mims EngDocumento17 pagineFurosemide Mims EngNur Ilmi SofiahNessuna valutazione finora
- Drug 25Documento17 pagineDrug 25carol_gigliotti24100% (1)
- Drug Study Ko ToDocumento4 pagineDrug Study Ko ToGian Carlo FernandezNessuna valutazione finora
- Drug StudyDocumento4 pagineDrug StudyTeanu Jose Gabrillo TamayoNessuna valutazione finora
- Drug Profile (Bisoprolol)Documento16 pagineDrug Profile (Bisoprolol)Maryam KhushbakhatNessuna valutazione finora
- Emergency MedsDocumento24 pagineEmergency MedsNursyNurse100% (1)
- Drugs AnalysisDocumento6 pagineDrugs AnalysisPauline CarenNessuna valutazione finora
- Drug Study JrodDocumento8 pagineDrug Study JrodGaez ﭢ UlpindoNessuna valutazione finora
- Drug Study Drug Name Classifications Action Indication Adverse Effects Contraindication Nursing Responsibility CnsDocumento4 pagineDrug Study Drug Name Classifications Action Indication Adverse Effects Contraindication Nursing Responsibility CnsMarielle SorianoNessuna valutazione finora
- Lisinopril PDFDocumento3 pagineLisinopril PDFHannaNessuna valutazione finora
- Drug StudyDocumento16 pagineDrug StudyCharm TanyaNessuna valutazione finora
- Drug Study PlasilDocumento2 pagineDrug Study PlasilPatrisha PatawaranNessuna valutazione finora
- CVA Drug StudyDocumento51 pagineCVA Drug StudyKarel LuNessuna valutazione finora
- Pharmacards CompilationDocumento53 paginePharmacards CompilationchristianfcualNessuna valutazione finora
- Dosage: Route:: Mycobacterium TuberculosisDocumento21 pagineDosage: Route:: Mycobacterium TuberculosisLyn ConsingNessuna valutazione finora
- Diazepam, Lanoxin, Hemostan, NaprexDocumento6 pagineDiazepam, Lanoxin, Hemostan, NaprexRene John Francisco100% (1)
- Drug StudyDocumento9 pagineDrug StudyEzshkha OngueNessuna valutazione finora
- Drug StudyDocumento16 pagineDrug Studyalice_lim01Nessuna valutazione finora
- Pedia Drug StudyDocumento11 paginePedia Drug StudyPeetah PanNessuna valutazione finora
- Motilium: ® Domperidone DatasheetDocumento11 pagineMotilium: ® Domperidone DatasheetAurungzaib BhattiNessuna valutazione finora
- B BlockersDocumento11 pagineB BlockersIRINANessuna valutazione finora
- Metoclopromide Drug StudyDocumento4 pagineMetoclopromide Drug Studymarklesterdeguzman087Nessuna valutazione finora
- Haloperidol 2mg-ml DropsDocumento15 pagineHaloperidol 2mg-ml Dropsddandan_2Nessuna valutazione finora
- Metformin 1 METFORMIN (500mg, 850mg and 1000mg Tablets) : New Zealand Data SheetDocumento11 pagineMetformin 1 METFORMIN (500mg, 850mg and 1000mg Tablets) : New Zealand Data SheetAfifa ZainNessuna valutazione finora
- Drug Study CCUDocumento5 pagineDrug Study CCUKrishna Faith P. DelaraNessuna valutazione finora
- Obat Tugas Dokter PhathimhaDocumento6 pagineObat Tugas Dokter PhathimhaMegan LewisNessuna valutazione finora
- LalalalaaaaDocumento6 pagineLalalalaaaaRobert LeblancNessuna valutazione finora
- Drug StudiesDocumento3 pagineDrug StudiesSteve PerezNessuna valutazione finora
- Drugstudy For ElderlyDocumento14 pagineDrugstudy For ElderlyJenniferP.BarrosoNessuna valutazione finora
- MM MM MM MM MMM MMMMM M MM M MMMM MMMMM MMM MM MMM MM!M M!"M#MM MM M $M M %MMM MM "M "MM M MMM MDocumento9 pagineMM MM MM MM MMM MMMMM M MM M MMMM MMMMM MMM MM MMM MM!M M!"M#MM MM M $M M %MMM MM "M "MM M MMM M배기숭Nessuna valutazione finora
- RamiprilDocumento3 pagineRamiprilNovi YulianaNessuna valutazione finora
- DRUG STUDY - SpironolactoneDocumento4 pagineDRUG STUDY - SpironolactoneMarianne Claire P. Bartolome50% (2)
- CHN Drug StudyDocumento10 pagineCHN Drug StudyJoshua Cyryll ComiaNessuna valutazione finora
- Amdocal Final PDFDocumento5 pagineAmdocal Final PDFSaifur Rahman SuzonNessuna valutazione finora
- Haldol 5mg: (Haloperidol)Documento17 pagineHaldol 5mg: (Haloperidol)ddandan_2Nessuna valutazione finora
- Drug StudyDocumento3 pagineDrug StudyGail SantosNessuna valutazione finora
- Drug StudyDocumento11 pagineDrug StudyHennah Reblando100% (3)
- ZolmitriptanDocumento3 pagineZolmitriptanjulieNessuna valutazione finora
- Metoprolol (Lopressor, Toprol-XL) Considerations For Use : Mechanism of Action DosingDocumento1 paginaMetoprolol (Lopressor, Toprol-XL) Considerations For Use : Mechanism of Action DosingB PNessuna valutazione finora
- mebendazole-WPS OfficeDocumento6 paginemebendazole-WPS OfficeDenvicNessuna valutazione finora
- Timolol MaleateDocumento3 pagineTimolol MaleateAP TOROBXNessuna valutazione finora
- The Efects of a Plant-Based Diet on Diabetes MellitusDa EverandThe Efects of a Plant-Based Diet on Diabetes MellitusNessuna valutazione finora
- REVIEWDocumento31 pagineREVIEWJoanna Marie Lumbre BalbiranNessuna valutazione finora
- Grow For The Perfect Exit Event-March 30-April1Documento4 pagineGrow For The Perfect Exit Event-March 30-April1Joanna Marie Lumbre BalbiranNessuna valutazione finora
- Behavior and Mental Status Can Be Early Signs of Impaired Gas ExchangeDocumento2 pagineBehavior and Mental Status Can Be Early Signs of Impaired Gas ExchangeJoanna Marie Lumbre BalbiranNessuna valutazione finora
- Capitol University College of NursingDocumento7 pagineCapitol University College of NursingJesus Carlo Adalla QuirapNessuna valutazione finora
- Chapter 1Documento1 paginaChapter 1Joanna Marie Lumbre BalbiranNessuna valutazione finora
- Regulation of Fluid Loss HypothalamusDocumento3 pagineRegulation of Fluid Loss HypothalamusJoanna Marie Lumbre BalbiranNessuna valutazione finora
- Ten Minutes Could Prevent One-Third of Road Deaths, Spanish Study FindsDocumento3 pagineTen Minutes Could Prevent One-Third of Road Deaths, Spanish Study FindsJoanna Marie Lumbre BalbiranNessuna valutazione finora
- Hazel Journal 2Documento1 paginaHazel Journal 2Joanna Marie Lumbre BalbiranNessuna valutazione finora
- Viii - Diagnostics Date Procedure Description Purpose/ Significance Normal Ranges Result Indication/Impr EssionDocumento9 pagineViii - Diagnostics Date Procedure Description Purpose/ Significance Normal Ranges Result Indication/Impr EssionChristian Karl B. LlanesNessuna valutazione finora
- UC Davis Koret Shelter Medicine Program - Feline Leukemia Virus (FeLV) - 2012-04-25Documento3 pagineUC Davis Koret Shelter Medicine Program - Feline Leukemia Virus (FeLV) - 2012-04-25Kitt KaosNessuna valutazione finora
- Embun Feby - Tugas Bahasa Inggris Untill II 3-4Documento4 pagineEmbun Feby - Tugas Bahasa Inggris Untill II 3-4Zibda UlyaNessuna valutazione finora
- Role of LABACS Provides A Simple and Effective For COPD and Asthma ManagementDocumento74 pagineRole of LABACS Provides A Simple and Effective For COPD and Asthma ManagementHans WinardiNessuna valutazione finora
- Laryngeal CleftDocumento4 pagineLaryngeal CleftjuicyprunesNessuna valutazione finora
- Psyche 4 AnxietyDocumento37 paginePsyche 4 AnxietysimplyrosalynNessuna valutazione finora
- Trastuzumab MonographDocumento11 pagineTrastuzumab MonographAmeliaNessuna valutazione finora
- Breast CancerDocumento129 pagineBreast CancerHope LeeNessuna valutazione finora
- Hs TroponinDocumento6 pagineHs TroponinNerhis Sydney WisakaNessuna valutazione finora
- MS Musculoskeletal ReviewDocumento12 pagineMS Musculoskeletal ReviewShayesra-Radina Laja SahibadNessuna valutazione finora
- Rodney Vs Death Rabies RadioLab Homework AssignmentDocumento1 paginaRodney Vs Death Rabies RadioLab Homework AssignmentLula Sims 14Nessuna valutazione finora
- Dental Treatment Considerations in The Chemotherapy PatientDocumento12 pagineDental Treatment Considerations in The Chemotherapy PatientAdeel TahirNessuna valutazione finora
- Pregnancy Induced Urinary Tract Changes Urinary Tract InfectionsDocumento5 paginePregnancy Induced Urinary Tract Changes Urinary Tract InfectionsDilausan B MolukNessuna valutazione finora
- UDID What Medical Doctors May Need To KnowDocumento37 pagineUDID What Medical Doctors May Need To KnowdrhareeshNessuna valutazione finora
- MAPEHDocumento3 pagineMAPEHGermaine Guimbarda MiguelesNessuna valutazione finora
- Use of CoQ10 To Treat MalignanciesDocumento2 pagineUse of CoQ10 To Treat MalignanciesTUartistNessuna valutazione finora
- Amit ReportDocumento3 pagineAmit ReportXlramitNessuna valutazione finora
- ENDOMETRIOSISDocumento33 pagineENDOMETRIOSISpriyanka bhowmikNessuna valutazione finora
- Neuro-Oncology Explained Through Multiple Choice Questions: Joe M DasDocumento243 pagineNeuro-Oncology Explained Through Multiple Choice Questions: Joe M Dasalistair90100% (2)
- Mouth Paste-Kenalog OrabaseDocumento3 pagineMouth Paste-Kenalog OrabaseKashif2008Nessuna valutazione finora
- 113959Documento19 pagine113959Andrea San AntonioNessuna valutazione finora
- Eczema, Immunity & The Skin Microbiome: Heidi H. Kong Dermatology Branch, CCR, NCIDocumento38 pagineEczema, Immunity & The Skin Microbiome: Heidi H. Kong Dermatology Branch, CCR, NCIrafdiaz2Nessuna valutazione finora
- Collateral Ligament Injuries - OrthoInfo - AAOSDocumento4 pagineCollateral Ligament Injuries - OrthoInfo - AAOSgermanda yepezNessuna valutazione finora
- DOLICHOCOLONDocumento6 pagineDOLICHOCOLONCassNessuna valutazione finora
- AXR Made EasyDocumento13 pagineAXR Made EasycswathikanNessuna valutazione finora
- First Level Assessment (SAMPLE)Documento2 pagineFirst Level Assessment (SAMPLE)Cooby Gempesaw100% (1)
- Erb'S Palsy: Definition/DescriptionDocumento10 pagineErb'S Palsy: Definition/DescriptionGuhan SubramaniamNessuna valutazione finora