Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Typhoid Diet
Caricato da
Ashwini TeegalaDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Typhoid Diet
Caricato da
Ashwini TeegalaCopyright:
Formati disponibili
Objectives
To maintain adequate nutrition To provide relief from symptoms To correct and maintain water and electrolyte balance To provide enough proteins
Dietary modifications Energy: In fevers the basal metabolic rate (BMR) increases, thus enhancing the energy needs. Restlessness also increases the energy expenditure. Therefore, it is recommended to increase the energy intake. But initially, a patient may be able to consume only 1000 1200 kcal/day. But it should be gradually increased with recovery and improved tolerance. Protein: Protein intake should be increased with the use of foods such as milk and eggs. Carbohydrates: A liberal intake of carbohydrates is suggested to meet the increased energy intake. Well cooked, easily digestible carbohydrates like starches, glucose, honey and cane sugar. should be included as they are easily digestedand are well absorbed by the body. Dietary fibre: In typhoid since there is injury to the digestive tract, all forms of irritants and harsh foods should be restricted from the diet. Fats: Fats are required mainly to increase the energy intake. In case diarrhoea is present, fats need to be restricted. It is the quality of fat that is more important than the quantity. Emulsified fats such as butter, cream and milk fat are easily digested. Minerals: There is excessive loss of electrolytes like sodium, potassium and chloride due to increased sweating. Salty soups, broths, fruit juices and milk help compensate the loss. Vitamins: Infection and fevers increase the requirement for vitamin A, B and C. Moreover, the use of antibiotics and drugs interferes with the synthesis of vitamin B in the intestines. So, vitamin supplements may have to be given along with other medicines. Fluids: In order to compensate for the losses through the sweat and also to ensure adequate volume of urine for excreting waste, a liberal intake of fluids is very essential. A daily intake of 34 litres is desirable. Fluids may be taken as water, tea, milk, juices and soups. Sample diet plan Meal Early morning Breakfast Menu Milk / tea in milk Biscuits / rusk Suji porridge / sewian kheer Boiled egg
Mid morning Lunch Evening tea Dinner Bedtime To remember
Paneer sandwich Vegetable khichri Potato raita / plain curd Milk Biscuits / bread butter / bread jam Tomato soup / chicken soup Chapatti / boiled rice Washed moong dal Custard with soft fruits
Small meals should be given at frequent intervals. Sufficient intake of fluids and salt should be ensured. Diet should be bland, low fibre, soft diet (easy to digest and absorbed). As the condition improves larger meals may be given.
Foods to be restricted or avoided
High fibre foods like whole grain cereals and their products, whole pulses and pulses with husk. All raw vegetables and fruits excluding banana and papaya. Fried and fatty foods such as samosas, pakoras, ladoos and halwas. Irritants such as spices, pickles, chutneys and strongly flavoured vegetables like cabbage, capsicum, turnip, radish, onion and garlic.
Foods to be included
Plenty of fluids like juices and soups. Milk and milk based beverages. Low fibre foods such as refined cereals (maida, suji, etc.) and their products, washed pulses, well-cooked vegetables in soft puree form and boiled potatoes. Foods providing proteins such as eggs, soft cheese, paneer, fish and chicken.
Potrebbero piacerti anche
- The 5x5 ProgramDocumento13 pagineThe 5x5 ProgramSMO979Nessuna valutazione finora
- Seismic Design and Construction of Retaining WallDocumento21 pagineSeismic Design and Construction of Retaining WallManojit Samanta100% (1)
- Railway Structures Chapter8 AREMA 2003Documento9 pagineRailway Structures Chapter8 AREMA 2003hawarihaithamNessuna valutazione finora
- Parkinson'S Disease What Is Parkinson's Disease?Documento6 pagineParkinson'S Disease What Is Parkinson's Disease?FadhilaKPNessuna valutazione finora
- Physiologic Value of FoodDocumento46 paginePhysiologic Value of FoodMICHELLE FACTONessuna valutazione finora
- Diet For Diabetes Step by Step Guide - 636b5747Documento69 pagineDiet For Diabetes Step by Step Guide - 636b5747vrunda shahNessuna valutazione finora
- Physics Formula Sheet by MedAngleDocumento17 paginePhysics Formula Sheet by MedAngleShahab SarwarNessuna valutazione finora
- Paper Tablets EXPDocumento4 paginePaper Tablets EXPRosales Gemson Lyster100% (2)
- Oral Rehydration TherapyDocumento12 pagineOral Rehydration TherapypasambalyrradjohndarNessuna valutazione finora
- Frcs General Surgery Mcqs Pdfsdocuments2comwwwpdfsdocuments2comf54frcs General Surgery MCQSPDFPDFDocumento2 pagineFrcs General Surgery Mcqs Pdfsdocuments2comwwwpdfsdocuments2comf54frcs General Surgery MCQSPDFPDFAbbas Ali0% (1)
- Nutrition PDFDocumento22 pagineNutrition PDFskNessuna valutazione finora
- Standardized Curriculum in General Surgery 2012Documento102 pagineStandardized Curriculum in General Surgery 2012Martin EscasuraNessuna valutazione finora
- Informatica BasicsDocumento253 pagineInformatica BasicsAshwini TeegalaNessuna valutazione finora
- SOPs Handling First AidDocumento2 pagineSOPs Handling First AidsridharNessuna valutazione finora
- Nursing Care PlanDocumento10 pagineNursing Care PlanmariasomorayNessuna valutazione finora
- Health Promotion and EducationDocumento2 pagineHealth Promotion and EducationBobet Reña100% (1)
- Dingcong, Phoebe Joy M. BSN 1 - A Fundamentals of NursingDocumento6 pagineDingcong, Phoebe Joy M. BSN 1 - A Fundamentals of NursingDee JeonNessuna valutazione finora
- Index: AntacidsDocumento24 pagineIndex: AntacidsaaajjpNessuna valutazione finora
- NCP and Problems FinalDocumento8 pagineNCP and Problems FinalRina CebreroNessuna valutazione finora
- Nutritional Management in Respiratory DiseasesDocumento23 pagineNutritional Management in Respiratory DiseasesRafia KhalilNessuna valutazione finora
- 8 Week Programme 1 PDFDocumento28 pagine8 Week Programme 1 PDFEsly Roman100% (1)
- Professional Nursing Research PaperDocumento6 pagineProfessional Nursing Research Paperapi-357132774Nessuna valutazione finora
- Nursing Math Conversions ONLINEDocumento2 pagineNursing Math Conversions ONLINEerinNessuna valutazione finora
- Dietary Guidelines For Indians-NINDocumento138 pagineDietary Guidelines For Indians-NINsaradhi26Nessuna valutazione finora
- Heat StrokeDocumento15 pagineHeat StrokesofiatidianNessuna valutazione finora
- Food Production AssignmentDocumento26 pagineFood Production AssignmentHarshit BhasinNessuna valutazione finora
- Workshop FlyerDocumento2 pagineWorkshop FlyerbhathiyaengNessuna valutazione finora
- Kerala: "God's Own Country"Documento13 pagineKerala: "God's Own Country"Muhammed AlwaniNessuna valutazione finora
- Hep B Lesson PlanDocumento42 pagineHep B Lesson PlanBea Bianca CruzNessuna valutazione finora
- HaematinicsDocumento20 pagineHaematinicsGeetika Mehta100% (1)
- Basic Concept in Nursing LessonsDocumento214 pagineBasic Concept in Nursing LessonsIlaw100% (1)
- DiabetesDocumento32 pagineDiabetesaneeshajaiswalNessuna valutazione finora
- Nuts Oil Seeds and Sugar UnitDocumento16 pagineNuts Oil Seeds and Sugar UnitIyappan SubramaniNessuna valutazione finora
- Different Types of IV FluidsDocumento6 pagineDifferent Types of IV FluidsnicoleNessuna valutazione finora
- Sheena Khan: Biochemistry Generiic Bs NursingDocumento22 pagineSheena Khan: Biochemistry Generiic Bs NursingsharmeenNessuna valutazione finora
- Nursing DiagnosisDocumento9 pagineNursing Diagnosiskhikmatul mu'jizahNessuna valutazione finora
- 2 Temperature RegulationDocumento46 pagine2 Temperature RegulationAlaa ElbedriNessuna valutazione finora
- Cam TherapyDocumento31 pagineCam TherapyHemantNessuna valutazione finora
- UNIT II Blood Pressure MeasurementDocumento50 pagineUNIT II Blood Pressure MeasurementDr.K. AyyarNessuna valutazione finora
- Data Visualisation Slides 1-6Documento318 pagineData Visualisation Slides 1-6Jasper van TuijlNessuna valutazione finora
- Clinical Learning Skills Laboratory: College of NursingDocumento3 pagineClinical Learning Skills Laboratory: College of NursingBeverly DatuNessuna valutazione finora
- Diabetic Foot Care: ReviewDocumento7 pagineDiabetic Foot Care: ReviewRavi HardjumadyNessuna valutazione finora
- Weaning in NepalDocumento16 pagineWeaning in Nepalbuddhaeyes098Nessuna valutazione finora
- Drug Study - Ncp.regDocumento7 pagineDrug Study - Ncp.reghaynakoewankosayoNessuna valutazione finora
- Isolationbarrier Nursing, ZoningDocumento29 pagineIsolationbarrier Nursing, ZoningSangeeta KamatchiNessuna valutazione finora
- Presentation Social IsolationDocumento20 paginePresentation Social IsolationMariagmzNessuna valutazione finora
- MSCDFSM Prog. GuideDocumento108 pagineMSCDFSM Prog. Guidesamraju1Nessuna valutazione finora
- Aquatic Therapy Services in Women HealthDocumento21 pagineAquatic Therapy Services in Women HealthMohammad Ajmal MadniNessuna valutazione finora
- No Dues CertificateDocumento1 paginaNo Dues Certificatereddy rajaNessuna valutazione finora
- The Community Client: Assessment Diagnosis: As andDocumento43 pagineThe Community Client: Assessment Diagnosis: As andAbid HussainNessuna valutazione finora
- Ragi Idli RecipeDocumento2 pagineRagi Idli RecipePradiba RaajkumaarNessuna valutazione finora
- Drug Name Mechanism of Action Indication Side Effects Nursing Responsibilities Generic Name: Occasional: DuringDocumento2 pagineDrug Name Mechanism of Action Indication Side Effects Nursing Responsibilities Generic Name: Occasional: Duringhahaha100% (1)
- Chapter 2 NutritionDocumento20 pagineChapter 2 NutritionLee Care GeneNessuna valutazione finora
- TnA (ICU)Documento1 paginaTnA (ICU)Danica Joy Christelle L. PilarNessuna valutazione finora
- Dermatological PharmacologyDocumento53 pagineDermatological PharmacologyDesta BelachewNessuna valutazione finora
- Bronchitis: Week 5 1Documento5 pagineBronchitis: Week 5 1jessNessuna valutazione finora
- NUTRIDocumento20 pagineNUTRIJinnijinniNessuna valutazione finora
- Body Posture & Lifting-8Documento89 pagineBody Posture & Lifting-8Shafiq Mohd NorNessuna valutazione finora
- IvtDocumento32 pagineIvtArlhona Juana RagoNessuna valutazione finora
- Demand Side ManagementDocumento67 pagineDemand Side ManagementLemdy AnwunaNessuna valutazione finora
- CBSE Class 12 Maths HOTs - IntegrationDocumento8 pagineCBSE Class 12 Maths HOTs - Integrationjagannivas100% (1)
- Soil Pollution and Noise Pollution 2Documento31 pagineSoil Pollution and Noise Pollution 2RajeshNessuna valutazione finora
- Women EntrepreneurshipDocumento24 pagineWomen EntrepreneurshipvincentrjkmrNessuna valutazione finora
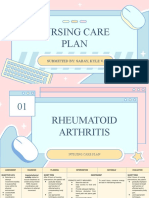
- Nursing Care Plan: Submitted By: Sabay, Kyle VDocumento11 pagineNursing Care Plan: Submitted By: Sabay, Kyle VKYLE SABAYNessuna valutazione finora
- Alternative MEDICINESDocumento21 pagineAlternative MEDICINESMoromi RongpeeNessuna valutazione finora
- DiabetesDocumento25 pagineDiabetesLawrence LarsonNessuna valutazione finora
- Acute and Chronic GastritisDocumento6 pagineAcute and Chronic GastritisAnn CanNessuna valutazione finora
- Dietary Management For TyphoidDocumento3 pagineDietary Management For Typhoidkeshav1980Nessuna valutazione finora
- Typhoid Is An Infectious DiseaseDocumento10 pagineTyphoid Is An Infectious DiseaseStephen MadridNessuna valutazione finora
- Mullins Cove Loop - EveryTrailDocumento15 pagineMullins Cove Loop - EveryTrailAshwini TeegalaNessuna valutazione finora
- Signal & Edwards Points SectionDocumento8 pagineSignal & Edwards Points SectionAshwini TeegalaNessuna valutazione finora
- The Luck FactorDocumento0 pagineThe Luck FactorFrederico GodinezNessuna valutazione finora
- Soil Mechanics Full Course Notes and LecturesDocumento125 pagineSoil Mechanics Full Course Notes and LecturesmehboobullahNessuna valutazione finora
- InformaticaDocumento162 pagineInformaticaAshwini TeegalaNessuna valutazione finora
- Design of Self-Centering Moment Resisting Frame and Experimental Loading SystemDocumento17 pagineDesign of Self-Centering Moment Resisting Frame and Experimental Loading SystemAshwini TeegalaNessuna valutazione finora
- Engineering Properties of SoilDocumento6 pagineEngineering Properties of Soilpapilolo2008Nessuna valutazione finora
- Assign 5Documento3 pagineAssign 5Ashwini TeegalaNessuna valutazione finora
- Artificial Generation of Spatially Varying Seismic Ground Motion Using AnnsDocumento8 pagineArtificial Generation of Spatially Varying Seismic Ground Motion Using AnnsAshwini TeegalaNessuna valutazione finora
- Extractions in Orthodontics PDFDocumento2 pagineExtractions in Orthodontics PDFJohnNessuna valutazione finora
- Icf PDFDocumento576 pagineIcf PDFŁukaszNessuna valutazione finora
- Medical Treatment Recuperation Convalescence With HomoeopathyDocumento4 pagineMedical Treatment Recuperation Convalescence With HomoeopathyEditor IJTSRDNessuna valutazione finora
- Drexel University: Commencement Ceremonies College of MedicineDocumento25 pagineDrexel University: Commencement Ceremonies College of MedicineChimpNessuna valutazione finora
- Mo2vate Issue 15 - March 2022Documento74 pagineMo2vate Issue 15 - March 2022Mo2vate MagazineNessuna valutazione finora
- Project Proposal Outline Form (Ppof)Documento5 pagineProject Proposal Outline Form (Ppof)Raging PotatoNessuna valutazione finora
- Exploring The Multifaceted Dimensions of Placemaking: From Theory To PracticeDocumento33 pagineExploring The Multifaceted Dimensions of Placemaking: From Theory To Practiceecho10131105Nessuna valutazione finora
- Romany Lofty: Prepare byDocumento27 pagineRomany Lofty: Prepare bySupekshya ShresthaNessuna valutazione finora
- SikaProof Membrane PDFDocumento6 pagineSikaProof Membrane PDFbetterthandrugsNessuna valutazione finora
- First Aid Training 1-2-3Documento2 pagineFirst Aid Training 1-2-3Christian Makande0% (1)
- Medical Claim Form (Reimbursement Only)Documento2 pagineMedical Claim Form (Reimbursement Only)Muhammad Rizwan Tariq100% (1)
- Activity Completion Report: District of Basey IDocumento2 pagineActivity Completion Report: District of Basey IRyan Adona GaddiNessuna valutazione finora
- Burning Mouth SyndromeDocumento28 pagineBurning Mouth SyndromeMelissa KanggrianiNessuna valutazione finora
- Breastfeeding ManagementDocumento12 pagineBreastfeeding ManagementtitisNessuna valutazione finora
- DRAFT - HIRARC REGISTER (45637)Documento6 pagineDRAFT - HIRARC REGISTER (45637)Leliance Ann BillNessuna valutazione finora
- City Health Office 2 PDFDocumento2 pagineCity Health Office 2 PDFSeth CastilloNessuna valutazione finora
- 6 Depression in ChildrenDocumento4 pagine6 Depression in ChildrenMirza ShaplaNessuna valutazione finora
- Arcon Engineering and Services ProfileDocumento30 pagineArcon Engineering and Services ProfilearconsteelNessuna valutazione finora
- Clinical Effectiveness of Conservative ManagementDocumento77 pagineClinical Effectiveness of Conservative ManagementD2S In'tl Business SolutionNessuna valutazione finora
- 10 Physical and Mental Benefits of BasketballDocumento4 pagine10 Physical and Mental Benefits of BasketballJohn Kenzo NavatoNessuna valutazione finora
- Mind FitnessDocumento9 pagineMind FitnessFit DealsNessuna valutazione finora
- ทิพยมนต์กับการบำบัดโรคDocumento7 pagineทิพยมนต์กับการบำบัดโรคtachetNessuna valutazione finora
- FW02 Phy ActivitiesDocumento13 pagineFW02 Phy Activitiesjojo basenNessuna valutazione finora
- Posttraumatic Stress Disorder Epidemiology, Pathophysiology, Clinical Manifestations, and DiagnosisDocumento9 paginePosttraumatic Stress Disorder Epidemiology, Pathophysiology, Clinical Manifestations, and Diagnosisisa_horejsNessuna valutazione finora