Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
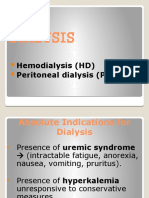
Indications For Initiation of Dialysis
Caricato da
Milton BenevidesDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Indications For Initiation of Dialysis
Caricato da
Milton BenevidesCopyright:
Formati disponibili
Official reprint from
UpToDate
Back | Print
www.uptodate.com
Indications for initiation of dialysis in chronic kidney disease
Author Nuhad Ismail, MD Section Editors Steve J Schwab, MD Jeffrey S Berns, MD Deputy Editor Theodore W Post, MD
Last literature review version 19.1: January 2011 | 2010 (More)
This topic last updated: October 5,
INTRODUCTION The decision to initiate dialysis in a patient with chronic kidney disease (CKD) involves the consideration of subjective and objective parameters by the physician and the patient. These parameters are often modulated by the patient's perception of his or her quality of life and by possible anxiety about starting new therapy that is technologically complex. INDICATIONS There are a number of clinical indications to initiate dialysis in patients with CKD. These include [ 1-3 ]: Pericarditis or pleuritis (urgent indication) Progressive uremic encephalopathy or neuropathy, with signs such as confusion, asterixis, myoclonus, wrist or foot drop, or, in severe cases, seizures (urgent indication) A clinically significant bleeding diathesis attributable to uremia (urgent indication) Fluid overload refractory to diuretics Hypertension poorly responsive to antihypertensive medications Persistent metabolic disturbances that are refractory to medical therapy; these include hyperkalemia, metabolic acidosis, hypercalcemia, hypocalcemia, and hyperphosphatemia Persistent nausea and vomiting Evidence of malnutrition However, these indications are potentially life-threatening and the patient is generally known to have advanced CKD. As a result, most nephrologists agree that delaying initiation of dialysis until one or more of these complications is present may put the patient at unnecessary jeopardy. Only one study has reported the outcomes of patients with CKD who initiated dialysis only after the onset of symptoms due to uremia. In this prospective cohort study of 233 consecutive patients with advanced uremia, 151 were elective starters on dialysis, while 82 initially declined dialysis [ 4]. Among the initial refusers, 55 percent developed a uremic emergency, while 48 percent were eventually established on maintenance dialysis. Compared with the elective starters, one year mortality was significantly higher among the initial refusers (18 versus 7 percent). However, these results are confounded by lack of randomization and by three deaths among the initial refusers, which resulted from treatment withdrawal.
Relative indications Since an important goal of dialysis is to enhance the quality of life as well as to prolong survival, it is therefore important to consider less acute indications for dialysis. These relative indications include decreased attentiveness and cognitive tasking, depression, persistent pruritus or the restless leg syndrome. Unfortunately, the expressions of these signs and symptoms are variable in patients with slowly progressive renal disease. The following are some of the factors that may contribute to this variability. Some patients accommodate to these symptoms and downgrade their sense of wellbeing as renal failure progresses. Many of the medications given to patients with CKD have side effects that mimic uremic symptoms. As examples, oral iron therapy often leads to nausea and centrally-acting antihypertensive drugs can induce drowsiness independent of the degree of renal failure. These factors illustrate the need to identify more objective markers of renal failure to lessen the subjective component of the decision to initiate dialysis. QUANTITATIVE MEASUREMENTS OF END-STAGE RENAL DISEASE The two most widely evaluated quantitative measurements of end-stage renal disease have been estimation of the glomerular filtration rate (GFR) and assessment of nutritional status. Estimation of GFR Although the filtration rate provides the best measure of functioning renal mass, there are problems with each of the available tests used to measure the GFR. As an example, many nephrologists previously used a target plasma creatinine concentration above 10 mg/dL (884 mol/L) [ 5,6 ]. However, progressive renal failure is frequently associated with marked changes in the generation and elimination of creatinine [ 7]. In particular, inadequate diet, increased tubular secretion of creatinine, and low muscle mass often limit the rise in the plasma creatinine concentration, thereby masking the true degree of renal failure. Use of the creatinine clearance is also limited in this setting. (See "Calculation of the creatinine clearance" .) The creatinine clearance generally overestimates the GFR due to increased tubular creatinine secretion. Some patients with a seemingly "normal" plasma creatinine concentration (<1.5 mg/dL or 132 mol/L) may have a GFR determined by 7]. One study, for example, inulin clearance as low as 20 to 25 mL/min/1.73 m [ evaluated 80 patients with CKD and a mean GFR of 22 mL/min [ 8]. The creatinine clearance was nearly twice the level of the inulin clearance. The urea clearance is an even less accurate measure of GFR. The urea clearance underestimates the rate of filtration due to a substantial degree of tubular reabsorption. It has been suggested that, when GFR is less than 15 mL/min, the mean of the creatinine and urea clearance provides a good estimate of GFR because the errors balance out. (See "Assessment of kidney function: Serum creatinine; BUN; and GFR" Because of the limitations of the conventionally used tests, many investigators have sought more accurate methods to measure the GFR. Although other markers of GFR, such as the clearance of 125-I-iothalamate, Cr-51-EDTA, 99m-Tc-DTPA, or inulin, are considered to be highly accurate, they are not widely available and cumbersome to use for regular monitoring of renal function. Several formulas that utilize easily obtained values have therefore been developed that
.)
help estimate the GFR. These include the Cockcroft-Gault and Modification of Diet in Renal Disease (MDRD) equations: The Cockcroft-Gault equation is: (140 - age) x lean body weight [kg] PCr [mg/dL] x 72
CCr, in mL/min
This formula takes into account the increase in creatinine production with increasing weight, and the decline in creatinine production with age. The value obtained must be calculator 1 ). multiplied by 0.85 in women who have a smaller muscle mass than men ( Using data from the MDRD study, the following is a simplified MDRD formula [ GFR, in mL/min per 1.73 m2 = 186.3 x ((serum creatinine) exp[-1.154]) x (Age exp[-0.203]) x (0.742 if female) x (1.21 if African American) where exp is the exponential. The K/DOQI clinical practice guidelines for CKD, as well as other K/DOQI guidelines, can be accessed through the National Kidney Foundation's web site at www.kidney.org/professionals/kdoqi/guidelines.cfm . Since the MDRD equations were derived from patients with renal failure, they can be reliably used in those with significant renal dysfunction. The MDRD and Cockroft-Gault equations, however, appear to generally overestimate the GFR in patients with stage 4 and 5 disease. Both the abbreviated MDRD formula and the Cockcroft-Gault equations provide similar values within a wide-range of patient ages. These formulas can only be used in patients with stable renal function. A detailed discussion of these formulas can be found elsewhere. (See "Assessment of kidney function: Serum creatinine; BUN; and GFR" .) A retrospective study in the United States found that the GFR at initiation of dialysis varied with patient age [ 10 ]. Based upon the United States Renal Data Systems database from 1995 to 1999, the creatinine clearance at initiation was 14.76, 13.38, 11.63, and 11.60 mL/min among those aged 20 to 44, 45 to 64, 65 to 74, and greater than 75 years, respectively. Nutritional status Many studies have shown an increased mortality risk associated with malnutrition in patients on maintenance dialysis [ 11,12 ]. As an example, an inverse relationship has been shown between the plasma albumin concentration and mortality risk in this setting [ 13,14 ]. The risk of death is increased when the plasma albumin concentration is below 3.5 to 4 mg/dL (35 to 40 g/L) ( figure 1 ). (See "Patient survival and maintenance dialysis" .) The United States Renal Data Systems analysis extended this observation by evaluating the relationship between the plasma albumin concentration at the time of initiation of dialysis and subsequent survival [ 14 ]. The risk of death in patients starting hemodialysis with hypoalbuminemia was substantially higher than in patients with a normal plasma albumin concentration ( figure 2 ). This relationship persisted even when diabetic patients, who may have significant proteinuria, were excluded from the analysis [ 15 ]. Worse outcomes in patients with lower plasma albumin concentrations at the initiation of dialysis 9]:
have also been noted in patients with continuous peritoneal dialysis [
16 ].
The significance of hypoalbuminemia in patients with nephrotic syndrome (other than diabetes) and end-stage renal disease is undetermined at present. In this setting, the low plasma albumin concentration may not reflect malnutrition. When interpreting the plasma albumin concentration, it is important to be aware of the specific assay used by the clinical laboratory. The two most commonly used methods are the bromcresol green (BCG) and bromcresol purple (BCP) dyebinding methods. BCG binds other proteins and therefore overestimates the albumin concentration. This error does not occur with the BCP method, the results of which compare closely with the reference immunonephelometric method [ 17,18 ]. Another marker of nutritional status at the time of dialysis initiation is the plasma creatinine concentration. The creatinine level reflects muscle mass as well as renal function. Thus, a patient requiring dialysis at a lower than usual plasma creatinine concentration has a reduced muscle mass and may be malnourished. Data from the USRDS are consistent with this hypothesis as the late mortality rate was increased in patients with a plasma creatinine concentration below 10 mg/dL (884 mol/L) at the start of dialysis ( figure 2 ) [ 14 ]. In comparison, the BUN level did not show a correlation with mortality risk. These data strongly suggest that malnutrition, as evidenced by a low plasma albumin and/or creatinine concentration at initiation of dialysis for symptomatic uremia, is an important prognostic variable. Other markers of malnutrition also may prove useful, including the plasma concentrations of transferrin, somatomedin C, prealbumin, and .) In cholesterol [ 19 ]. (See "Assessment of nutritional status in end-stage renal disease" patients treated with CAPD, for example, low serum prealbumin concentrations (<30 20 ]. A similar finding has mg/dL) have been associated with increased mortality risk [ been shown with maintenance hemodialysis (relative risk of mortality was 4.4 when the plasma prealbumin concentration was less than 15 mg/dL) [ 9]. A simple determinant of nutritional status that can be easily monitored is protein intake, assuming that the patient is not on a low protein diet. Patients with CKD on an unrestricted diet tend to decrease their protein intake as the renal failure progresses. The magnitude of this effect was demonstrated in a report that evaluated 90 patients with 21-23 ]. A direct correlation was noted between CKD who received no dietary intervention [ the dietary protein intake and the creatinine clearance (Ccr): 1.1 g/kg per day at a Ccr above 50 mL/min 0.85 g/kg per day between 25 and 50 mL/min 0.70 g/kg per day between 10 and 25 mL/min 0.54 g/kg per day below 10 mL/min These changes, which presumably reflect anorexia induced by renal failure, question the safety of restricting protein intake in patients with a creatinine clearance below 25 mL/min. These decrements in dietary protein intake can be followed by assessing daily urinary urea nitrogen and nonurea nitrogen losses. If daily intake is relatively constant and the patient is in a steady state (as evidenced by a stable BUN and body weight), then urinary nitrogen excretion is roughly equal to nitrogen intake. The former can be estimated from [24 ]: Urinary nitrogen excretion = Urine urea nitrogen + Nonurea nitrogen
Nonurea nitrogen excretion is relatively constant, averaging 30 mg/kg per day. Each gram of nitrogen is derived from 6.25 grams of protein. Thus, Estimated protein intake = 6.25 (Urine urea nitrogen + 30 mg/kg)
If, for example, 24-hour urine urea nitrogen excretion is 8.2 grams in a 60 kg woman excreting 3.5 g of protein per day, then: Estimated protein intake = 6.25 (8.2 + 1.8) = 62.5 grams
Thus, protein intake is approximately 1 g/kg per day. Moderate urinary protein loss can be ignored, but each gram excreted above 5 g/day should be added to the above formula. A useful measurement of protein metabolism is the protein equivalent of nitrogen appearance (eg, excretion) normalized using the ideal body weight (nPNA) which is equivalent to the normalized protein catabolic rate. Values below 0.8 g/kg per day are considered indicative of a malnourished state. (See "Protein catabolic rate in maintenance dialysis" .) Effect of dialysis Although the initiation of dialysis improves appetite in symptomatic uremia, there is a paucity of data showing that it is clearly associated with an improvement in nutritional status. Two observational studies reported that initiation of dialysis was associated with clear improvement in nutritional indices: Over a one year period, different nutritional indices were evaluated every three 25 ]. Marked months after dialysis initiation among 50 hemodialysis patients [ improvements were observed in the serum albumin, serum prealbumin, nPNA, fat mass, and others. The degree of improvement was dependent upon nutrition at baseline, with the lower the baseline value the lower its value at one year. Among 97 patients initiating maintenance dialysis therapy, multiple nutritional indices, including predialysis serum albumin, iron, transferrin saturation, creatinine, and the nPNA, significantly increased over the first six months of therapy, with many 26 ]. In addition, dietary intake, as shown indices continuing to increase at study end [ by the nPNA, directly correlated with serum albumin value. Given that dialysis was initiated based upon varying criteria, these two studies do not address the question of whether early or late initiation of dialysis is optimal. However, these results support the view that dialysis initiation improves nutritional parameters in the first year after beginning renal replacement therapy. DOES EARLY DIALYSIS OR REFERRAL IMPROVE SURVIVAL/OUTCOMES? Survival and dialysis complications There is conflicting evidence concerning the effect of the early initiation of dialysis on survival. Some retrospective and uncontrolled prospective studies have reported no survival benefits with early dialysis while others have 27-31 ]. found such benefits with early initiation [ The only randomized controlled trial that examined mortality and time of dialysis initiation, the IDEAL study, found NO difference in survival between early or late initiation of dialysis. In this study, 828 patients with progressive CKD and an estimated GFR between 10.0 and 15.0 mL/min per 1.73 m2 (as determined by the Cockcroft-Gault equation) were randomly assigned to dialysis initiation when the estimated GFR was either 10 to 14 mL/min per 1.73 m2 or 5 to 7 mL/min per 1.73 m2 [ 32 ]. The median
time to the initiation of dialysis was 1.8 and 7.4 months in the early and late start groups, respectively. At a median followup period of 3.6 years, the two groups had no significant difference in survival (38 and 37 percent mortality, hazard ratio of 1.05 with early initiation, 95% CI of 0.83 to 1.30) as well as no difference in cardiovascular events, infections, or dialysis complications. However, these results do NOT imply that the initiation of dialysis can be delayed until the GFR is between 5 to 7 mL/min per 1.73 m2 in all patients. The design of the IDEAL study permitted clinicians to initiate dialysis based upon the presence of symptoms due to uremia (such as uremic symptoms, volume overload, and other features) as well as on the estimated GFR. As a result, 76 percent of patients assigned to the late start arm initiated dialysis when the GFR was much greater than 5 to 7 mL/min per 1.73 m2. This resulted in a mean GFR of 9.8 mL/min per 1.73 m2 at the start of dialysis for the late start group, which was only 2.2 mL/min per 1.73 m2 less than the mean start GFR for the early group (12.0 mL/min per 1.72 m2). Thus, approximately 88 percent of all enrolled patients had initiated dialysis with an estimated GFR of approximately 10 mL/min per 1.73 m2 or more, either because of symptoms or enrollment in the early dialysis arm. An accompanying editorial to the IDEAL study stated that the results of this trial largely supports current practice that dialysis initiation should be based upon clinical factors 33 ]. Patients with progressive CKD require close rather than the estimated GFR alone [ followup, early nephrology referral, and adequate advance dialysis planning (including the presence of a functioning peritoneal or vascular access and referral for transplantation). In this study, for example, patients were followed by a nephrologist for approximately 2.5 years before dialysis was initiated. We suggest that, among patients with progressive CKD, clinicians must be vigilant for the presence of symptoms and/or signs of uremia and patients should also be fully informed of any symptoms of uremia to be able to contact their physicians appropriately. Dialysis should be considered based upon clinical factors plus the estimated GFR. Dialysis should be initiated in the patient with symptoms and/or signs due to uremia. (See 'Indications' above and 'Summary and recommendations' below and 'Relative indications' above.) Among asymptomatic patients with progressive CKD, the timing of initiation of dialysis is unclear and there is no specific threshold GFR level that has been established for the initiation of dialysis. To help avoid the onset of possible life-threatening complications of uremia, the initiation of dialysis should be considered in the asymptomatic patient with an extremely low GFR, such as an estimated GFR of approximately 8 to 10 mL/min per 1.73 m2. However, some clinicians may choose to closely monitor (weekly) asymptomatic patients with progressive CKD even when GFR is below this level, with the initiation of dialysis upon the onset of uremic signs/symptoms. Nevertheless, as noted in the IDEAL trial, the vast majority of patients are initiated on dialysis because of the onset of uremic symptoms at a GFR of approximately 10 mL/min per 1.73 m2 or above. The following are some of the more recent National and International Guidelines for the initiation of dialysis, which were published before the results of the IDEAL trial were reported: The 2006 National Kidney Foundation Dialysis Outcomes Quality Initiative (K/DOQI) for peritoneal dialysis and hemodialysis adequacy published guidelines concerning the initiation of dialysis among patients with renal insufficiency [ 2,3 ]. The work group suggested that the benefits and risks of initiating renal replacement therapy should
be considered in patients with GFR less than 15 mL/min per 1.73 m2 (stage 5 chronic kidney disease). Initiation of dialysis prior to stage 5 chronic kidney disease may also be required in patients with certain characteristics and/or complications, such as declining health due to the loss of kidney function. The 2005 European Best Practice Guidelines for peritoneal dialysis suggest that dialysis be initiated before the GFR is less than 6 mL/min per 1.73 m2, with consideration of initiation when the GFR is approximately 8 to 10 mL/min per 1.73 m2 [ 34 ]. There may be two additional advantages to early dialysis: control of hypertension and increased dietary intake [ 31 ]. Reversal of volume overload with dialysis often leads to a reduction in blood pressure, which is typically volume-dependent in CKD. (See "Hypertension in kidney disease" .) Perhaps more important, patients on dialysis patients require at least 1 g/kg of protein per day to replace dialysis losses and maintain nitrogen balance. Thus, early institution of dialysis can allow a more liberal diet in terms of both food and fluid. Possible value of early referral A related issue to the criteria for the initiation of dialysis is the timing of referral of patients with chronic renal failure to a nephrologist. Referral occurs at variable levels of renal function, but often late in the course of progressive renal failure, just before or even after the onset of symptomatic uremia. Late referral reflects in part the absence of clear criteria for the initiation of dialysis. However, early referral affords the opportunity to assess the rate of progression of renal disease, to exclude any reversible causes of a declining GFR, and to permit close followup and adequate advance dialysis planning. It may also improve patient outcomes. This is discussed in detail separately. (See "Late referral to nephrologists of patients with chronic kidney disease" .) INITIATION OF DIALYSIS AND DIALYSIS DISEQUILIBRIUM An important potential complication of the initiation of dialysis is the dialysis disequilibrium syndrome. This disorder, which appears to be related in part to a rapid reduction in the plasma osmolality due to urea removal, can produce a variety of symptoms including headache, nausea, vomiting, blurring of vision, muscle twitching, disorientation, tremor, and seizures. Patients with underlying neurologic disease or marked azotemia are at increased risk. .) (See "Dialysis disequilibrium syndrome" INFORMATION FOR PATIENTS Educational materials on this topic are available for patients. (See "Patient information: Dialysis or kidney transplantation which is right for me?" and "Patient information: Hemodialysis" and "Patient information: Peritoneal dialysis" .) We encourage you to print or e-mail these topic reviews, or to refer patients to our public web site, www.uptodate.com/patients , which includes these and other topics. SUMMARY AND RECOMMENDATIONS There are a number of clinical indications to 1-3 ]: initiate dialysis in patients with chronic kidney disease (CKD). These include [ Pericarditis or pleuritis (urgent indication) Progressive uremic encephalopathy or neuropathy, with signs such as confusion, asterixis, myoclonus, wrist or foot drop, or, in severe, cases, seizures (urgent indication) A clinically significant bleeding diathesis attributable to uremia (urgent indication) Fluid overload refractory to diuretics
Hypertension poorly responsive to antihypertensive medications Persistent metabolic disturbances that are refractory to medical therapy. These include hyperkalemia, metabolic acidosis, hypercalcemia, hypocalcemia, and hyperphosphatemia. Persistent nausea and vomiting Evidence of malnutrition Relative indications for the initiation of dialysis include decreased attentiveness and cognitive tasking, depression, persistent pruritus or the restless leg syndrome. We suggest that, among patients with progressive CKD, clinicians must be vigilant for the presence of symptoms and/or signs of uremia and patients should also be fully informed of any symptoms of uremia to be able to contact their physicians appropriately. Dialysis should be considered based upon clinical factors plus the estimated GFR. Dialysis should be initiated in the patient with symptoms and/or signs due to uremia. Among asymptomatic patients with progressive CKD, the timing of initiation of dialysis is unclear and there is no specific threshold GFR level that has been established for the initiation of dialysis. To help avoid the onset of possible life-threatening complications of uremia, the initiation of dialysis should be considered in the asymptomatic patient with an extremely low GFR, such as an estimated GFR of approximately 8 to 10 mL/min per 1.73 m2. However, some clinicians may choose to closely monitor (weekly) asymptomatic patients with progressive CKD even when the GFR is less than 8 to 10 mL/min per 1.73 m2, with the initiation of dialysis upon the onset of uremic signs/symptoms. Nevertheless, as noted in the IDEAL trial, the vast majority of patients are initiated on dialysis because of the onset of uremic symptoms at a GFR of approximately 10 mL/min per 1.73 m2 or above. All approaches require close follow-up, early nephrology referral, and adequate advance dialysis planning (including the presence of a functioning peritoneal or vascular access and referral for transplantation). The following are some of the more recent National and International Guidelines for the initiation of dialysis, which were published before the results of the IDEAL trial were reported: The 2006 National Kidney Foundation Dialysis Outcomes Quality Initiative (K/DOQI) for peritoneal dialysis and hemodialysis adequacy published guidelines concerning 2,3 ]. The work group the initiation of dialysis among patients with renal insufficiency [ suggested that the benefits and risks of initiating renal replacement therapy should be considered in patients with GFR less than 15 mL/min per 1.73 m2 (stage 5 chronic kidney disease). Initiation of dialysis prior to stage 5 chronic kidney disease may also be required in patients with certain characteristics and/or complications, such as declining health due to the loss of kidney function. The 2005 European Best Practice Guidelines for peritoneal dialysis suggest that dialysis be initiated before the GFR is less than 6 mL/min per 1.73 m2, with consideration of initiation when the GFR is approximately 8 to 10 mL/min per 1.73 m2 [ 34 ]. Use of UpToDate is subject to the Subscription and License Agreement
REFERENCES
1.
Pendse, S, Singh, A, Zawada, E. Initiation of dialysis in Handbook of Dialysis, 4th ed, Daugirdas, JT, Blake, PG, Ing, TS (Eds). Lippincott Williams & Wilkins, Philadelphia 2007. K/DOQI Clinical Practice Guidelines for Peritoneal Dialysis Adequacy. Am J Kidney Dis 2006; 47(Suppl 4):S1. K/DOQI Clinical Practice Guidelines and Clinical Practice Recommendations 2006 Updates Hemodialysis adequacy Peritoneal Dialysis Adequacy Vascular Access. Am J Kidney Dis 2006; 48(Suppl 1):S1. Tang SC, Ho YW, Tang AW, et al. Delaying initiation of dialysis till symptomatic uraemia--is it too late? Nephrol Dial Transplant 2007; 22:1926. Man NK. Initiation of dialysis: when? Nippon Jinzo Gakkai Shi 1992; 34:1. Obrador GT, Arora P, Kausz AT, et al. Level of renal function at the initiation of dialysis in the U.S. end-stage renal disease population. Kidney Int 1999; 56:2227. Levey AS. Measurement of renal function in chronic renal disease. Kidney Int 1990; 38:167. Shemesh O, Golbetz H, Kriss JP, Myers BD. Limitations of creatinine as a filtration marker in glomerulopathic patients. Kidney Int 1985; 28:830. Goldwasser P, Michel MA, Collier J, et al. Prealbumin and lipoprotein(a) in hemodialysis: relationships with patient and vascular access survival. Am J Kidney Dis 1993; 22:215. Balogun SA, Balogun RA, Evans J. Age-related differences in renal function at onset of renal replacement therapy in chronic kidney disease stage 5 patients. QJM 2006; 99:595. Acchiardo SR, Moore LW, Latour PA. Malnutrition as the main factor in morbidity and mortality of hemodialysis patients. Kidney Int Suppl 1983; 16:S199. Lowrie EG, Lew NL. Death risk in hemodialysis patients: the predictive value of commonly measured variables and an evaluation of death rate differences between facilities. Am J Kidney Dis 1990; 15:458. Owen WF Jr, Lew NL, Liu Y, et al. The urea reduction ratio and serum albumin concentration as predictors of mortality in patients undergoing hemodialysis. N Engl J Med 1993; 329:1001. Comorbid conditions and correlations with mortality risk among 3,399 incident hemodialysis patients. Am J Kidney Dis 1992; 20:32. Hakim, RM. Initiation of dialysis. In: Advances in Nephrology, vol 23, Grunfeld, JP, Back, JF, Kreis, H, Maxwell, MH (Eds), Mosby Yearbook, Chicago 1994. Misra M, Nolph KD, Khanna R, et al. Retrospective evaluation of renal kt/V(urea) at the initiation of long-term peritoneal dialysis at the University of Missouri: relationships to longitudinal nutritional status on peritoneal dialysis. ASAIO J 2003; 49:91. Blagg CR, Liedtke RJ, Batjer JD, et al. Serum albumin concentration-related Health Care Financing Administration quality assurance criterion is method-dependent: revision is necessary. Am J Kidney Dis 1993; 21:138. Wick. Albumin methodology. Dial Transplant 1994; 23:282. Hakim RM, Levin N. Malnutrition in hemodialysis patients. Am J Kidney Dis 1993; 21:125. Sreedhara R, Avram MM, Blanco M, et al. Prealbumin is the best nutritional predictor of survival in hemodialysis and peritoneal dialysis. Am J Kidney Dis 1996; 28:937. Hakim RM, Lazarus JM. Initiation of dialysis. J Am Soc Nephrol 1995; 6:1319.
2. 3.
4. 5. 6. 7. 8. 9.
10.
11. 12.
13.
14. 15. 16.
17.
18. 19. 20. 21.
22. 23. 24. 25. 26. 27. 28. 29. 30. 31.
Ikizler TA, Greene JH, Wingard RL, et al. Spontaneous dietary protein intake during progression of chronic renal failure. J Am Soc Nephrol 1995; 6:1386. Hakim RM, Lazarus JM. Biochemical parameters in chronic renal failure. Am J Kidney Dis 1988; 11:238. Maroni BJ, Steinman TI, Mitch WE. A method for estimating nitrogen intake of patients with chronic renal failure. Kidney Int 1985; 27:58. Pupim LB, Kent P, Caglar K, et al. Improvement in nutritional parameters after initiation of chronic hemodialysis. Am J Kidney Dis 2002; 40:143. Mehrotra R, Berman N, Alistwani A, Kopple JD. Improvement of nutritional status after initiation of maintenance hemodialysis. Am J Kidney Dis 2002; 40:133. Bonomini V, Feletti C, Scolari MP, Stefoni S. Benefits of early initiation of dialysis. Kidney Int Suppl 1985; 17:S57. Korevaar JC, Jansen MA, Dekker FW, et al. When to initiate dialysis: effect of proposed US guidelines on survival. Lancet 2001; 358:1046. Traynor JP, Simpson K, Geddes CC, et al. Early initiation of dialysis fails to prolong survival in patients with end-stage renal failure. J Am Soc Nephrol 2002; 13:2125. Kazmi WH, Gilbertson DT, Obrador GT, et al. Effect of comorbidity on the increased mortality associated with early initiation of dialysis. Am J Kidney Dis 2005; 46:887. Hakim, RM. Quand commencer la dialyze: Les bases de la decision. In: Actualites Nephrologiques, Funck Brentano, JL, Back, JF, Kreis, H, Grunfeld, JP (Eds), Jean Hamburger, Hospital Necker, Medecines Sciences/Flammarion, Paris 1993. Cooper BA, Branley P, Bulfone L, et al. A randomized, controlled trial of early versus late initiation of dialysis. N Engl J Med 2010; 363:609. Lameire N, Van Biesen W. The initiation of renal-replacement therapy--just-in-time delivery. N Engl J Med 2010; 363:678. European Best Practice Guidelines for peritoneal dialysis. Nephrol Dial Transplant 2005; 20(Suppl 9):3.
32. 33. 34.
GRAPHICS
Hypoalbuminemia and reduced survival in hemodialysis
Odds ratio for death, adjusted for age, sex, race, and underlying disease, according to the plasma albumin concentration in patients on maintenance hemodialysis. The likelihood of dying was inversely related to the plasma albumin concentration, being greatest at a plasma albumin concentration below 3.0 g/dL (30 g/L). All values are signficantly different (p<0.001 to 0.03) from the odds ratio of 1.0 at a normal plasma albumin concentration of 4.0 to 4.4 g/dL (40 to 44 g/L).
albumin concentration of 4.0 to 4.4 g/dL (40 to 44 g/L). Data from Owen, WF Jr, Lew, NL, Liu, Y, et al, N Engl J Med 1993; 329:1001.
Nutritional parameters predict relative mortality risk at initiation of dialysis
Relative mortality risk in new patients begun on maintenance hemodialysis in 1986-1987 according to the plasma albumin (left) and creatinine (right) concentrations. The mortality risk varied inversely with both parameters. Asterisks refer to values that are significantly different from the reference ranges of 3.6 to 4.0 g/dL (36 to 40 g/L) for albumin and 10 to 11.9 mg/dL [884 to 1052 mol/L]) for creatinine. Lower albumin and creatinine levels presumably reflect the negative impact of malnutrition on patient survival. Data from United States Renal Data Systems, Am J Kidney Dis 1992; 20(Suppl 2):32.
2011 UpToDate, Inc. All rights reserved. Licensed to: Harry Potter
| Subscription and License Agreement
Potrebbero piacerti anche
- Nephro - CVC Tip SheetDocumento6 pagineNephro - CVC Tip Sheetsam m0% (1)
- The Western and Eastern Concepts of SelfDocumento3 pagineThe Western and Eastern Concepts of SelfTakumi Shawn Hinata100% (3)
- Case Study HemodialysisDocumento5 pagineCase Study HemodialysisCharmaine del RosarioNessuna valutazione finora
- Caprini DVT Risk AssessmentDocumento2 pagineCaprini DVT Risk AssessmentAnonymous PjQxbsJQaNessuna valutazione finora
- Fresenius 2008T Dialysis System - User's Troubleshooting ManualDocumento20 pagineFresenius 2008T Dialysis System - User's Troubleshooting ManualCesar AlfaroNessuna valutazione finora
- ReagentsDocumento12 pagineReagentsKimscey Yvan DZ SulitNessuna valutazione finora
- 114 The Letter S: M 'TafontDocumento9 pagine114 The Letter S: M 'TafontHarry TLNessuna valutazione finora
- Bomber JacketDocumento3 pagineBomber JacketLaura Carrascosa FusterNessuna valutazione finora
- Hepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandHepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Hemodialysis Thesis - Analytical EssayDocumento4 pagineHemodialysis Thesis - Analytical EssayDianne LopezNessuna valutazione finora
- Hypertension in Dialysis PatientsDocumento16 pagineHypertension in Dialysis PatientsLiliana WoodNessuna valutazione finora
- Report2014 PDFDocumento332 pagineReport2014 PDFShareDialysis100% (1)
- Hemodialysis: NURSING DIAGNOSIS: Injury, Risk For (Loss of Vascular Access) Risk Factors May IncludeDocumento10 pagineHemodialysis: NURSING DIAGNOSIS: Injury, Risk For (Loss of Vascular Access) Risk Factors May IncludeChevelle Valenciano-GaanNessuna valutazione finora
- Hemodialysis in ChildrenDocumento28 pagineHemodialysis in ChildrenKarna Yuli sitanggangNessuna valutazione finora
- Increased Minimum Vein Diameter On PreoperativeDocumento40 pagineIncreased Minimum Vein Diameter On PreoperativeMikael AngelooNessuna valutazione finora
- Techniques To Improve Intradialytic Haemodynamic Stability: ReviewDocumento7 pagineTechniques To Improve Intradialytic Haemodynamic Stability: Reviewnelbut2Nessuna valutazione finora
- Dialysis TermsDocumento2 pagineDialysis TermsmagillaniNessuna valutazione finora
- Home Hemodialysis: A Guide For Patients and Their FamiliesDocumento28 pagineHome Hemodialysis: A Guide For Patients and Their FamiliesJJBMNessuna valutazione finora
- Decreased Cardiac OutputDocumento3 pagineDecreased Cardiac OutputSantana Janai Francisco100% (2)
- Peritoneal DialysisDocumento23 paginePeritoneal Dialysismakyofrancis20Nessuna valutazione finora
- JCAHO Medication Management Standards 2004Documento10 pagineJCAHO Medication Management Standards 2004Afdhal MawardinNessuna valutazione finora
- HEMODIALYSISDocumento108 pagineHEMODIALYSISDan™100% (2)
- Guidelines FOR Implementing Drug Utilization Review Programs IN HospitalsDocumento58 pagineGuidelines FOR Implementing Drug Utilization Review Programs IN HospitalsMuhammad Faris MahmudNessuna valutazione finora
- Literature Review DialysisDocumento14 pagineLiterature Review DialysisAnneNessuna valutazione finora
- Critical Care Nephrology Core Curriculum 2020 PDFDocumento18 pagineCritical Care Nephrology Core Curriculum 2020 PDFMartín FleiNessuna valutazione finora
- Picot Paper Summative FinalDocumento10 paginePicot Paper Summative Finalapi-291122174Nessuna valutazione finora
- Renal Replacement Therapy HD, PD, Renal TransplantationDocumento65 pagineRenal Replacement Therapy HD, PD, Renal TransplantationparciNessuna valutazione finora
- Seizures in Children JULIO 2020Documento29 pagineSeizures in Children JULIO 2020Elizabeth HendersonNessuna valutazione finora
- Clinical Practice Guidelines Critical Appraisal GuideDocumento2 pagineClinical Practice Guidelines Critical Appraisal GuideWijitha VarenniNessuna valutazione finora
- Guide To IV SolutionsDocumento1 paginaGuide To IV SolutionsKim BadillesNessuna valutazione finora
- What You Should Know About Dialyzer Reuse: A Guide For Hemodialysis Patients and Their FamiliesDocumento8 pagineWhat You Should Know About Dialyzer Reuse: A Guide For Hemodialysis Patients and Their FamiliesDewiyanti TodingNessuna valutazione finora
- Blood Transfusion On Dialysis Guidelines Aug 2017 PDFDocumento5 pagineBlood Transfusion On Dialysis Guidelines Aug 2017 PDFYolanda IrawatiNessuna valutazione finora
- Dialysisprescription2 161102121138Documento61 pagineDialysisprescription2 161102121138ZH. omg sar100% (1)
- Running Head: Scope of Practice Is State Regulated 1Documento7 pagineRunning Head: Scope of Practice Is State Regulated 1Carole MweuNessuna valutazione finora
- Blood Transfusion GuidelineDocumento402 pagineBlood Transfusion GuidelineAdam Razi0% (1)
- 2008T Hemodialysis Machine Operator's ManualDocumento285 pagine2008T Hemodialysis Machine Operator's ManualKarim AmerNessuna valutazione finora
- Formal ReflectionDocumento5 pagineFormal Reflectionapi-456592801Nessuna valutazione finora
- 3 Summary Guide Clinical Indicators 2012 (ACHS)Documento48 pagine3 Summary Guide Clinical Indicators 2012 (ACHS)Erniwati SilalahiNessuna valutazione finora
- Clinical Exemplar PcuDocumento7 pagineClinical Exemplar Pcuapi-430800277Nessuna valutazione finora
- Improving The Quality of Care in An Acute Care Facility Through RDocumento88 pagineImproving The Quality of Care in An Acute Care Facility Through RNor-aine Salazar AccoyNessuna valutazione finora
- Cherukuri Et Al. 2018 - Home Haemodialysis Treatment and Outcomes, Retrospective Analysis of KIHDNEyDocumento10 pagineCherukuri Et Al. 2018 - Home Haemodialysis Treatment and Outcomes, Retrospective Analysis of KIHDNEyShareDialysisNessuna valutazione finora
- A. Ward Round IPS Example FINALDocumento5 pagineA. Ward Round IPS Example FINALEzra Ledya Sevtiana SinagaNessuna valutazione finora
- Change InitiativeDocumento7 pagineChange InitiativeWajiha ShaikhNessuna valutazione finora
- 1 PDFDocumento94 pagine1 PDFJohn Louie SolitarioNessuna valutazione finora
- Falls Assessment in Continuing CareDocumento30 pagineFalls Assessment in Continuing CareIwan Purnawan100% (1)
- Observation Summary 2Documento5 pagineObservation Summary 2api-493028287Nessuna valutazione finora
- Dialysis: Hemodialysis (HD) Peritoneal Dialysis (PD)Documento66 pagineDialysis: Hemodialysis (HD) Peritoneal Dialysis (PD)joms_pasanoNessuna valutazione finora
- Patient Counselling - CPDocumento8 paginePatient Counselling - CPmrcopy xeroxNessuna valutazione finora
- Running Head: NURSING STANDARDS 1Documento20 pagineRunning Head: NURSING STANDARDS 1api-253509573Nessuna valutazione finora
- Outpt. Recommendation of Renal Transplant Patients.Documento86 pagineOutpt. Recommendation of Renal Transplant Patients.Nephrology On-DemandNessuna valutazione finora
- Interventional NephrologyDocumento5 pagineInterventional Nephrologyfouad tabet100% (1)
- Case 36 AscitesDocumento4 pagineCase 36 AscitesMichaelNessuna valutazione finora
- Adult Infusion StandardsDocumento11 pagineAdult Infusion StandardsJessica Torreglosa100% (1)
- Hemodialysis Adequacy DwiDocumento27 pagineHemodialysis Adequacy Dwiryo_ninukNessuna valutazione finora
- Hemodialysis 2nd Final 171120Documento94 pagineHemodialysis 2nd Final 171120jaime berces hospitalNessuna valutazione finora
- Quality Improvement Paper FinalDocumento11 pagineQuality Improvement Paper Finalapi-291740538Nessuna valutazione finora
- Advanced Airway Care: Intensive Care Unit PerspectiveDocumento42 pagineAdvanced Airway Care: Intensive Care Unit PerspectiveJeffery Samuel100% (1)
- Kdoqi Vasc Access Review2019 v2Documento163 pagineKdoqi Vasc Access Review2019 v2Humairah AnandaNessuna valutazione finora
- Introduction To Nursing Research Part 1Documento22 pagineIntroduction To Nursing Research Part 1Ciedelle Honey Lou DimaligNessuna valutazione finora
- Dialysis Licensing Requirment DC - LTO-LR12192006 PDFDocumento5 pagineDialysis Licensing Requirment DC - LTO-LR12192006 PDFal gulNessuna valutazione finora
- DialysisDocumento6 pagineDialysissakuraleeshaoranNessuna valutazione finora
- Sepsis: Fajar Yuwanto SMF Penyakit Dalam RS Abdul MoeloekDocumento58 pagineSepsis: Fajar Yuwanto SMF Penyakit Dalam RS Abdul MoeloekamirazhafrNessuna valutazione finora
- ICU Scoring Systems A Complete Guide - 2020 EditionDa EverandICU Scoring Systems A Complete Guide - 2020 EditionNessuna valutazione finora
- Chemistry Jun 2010 Mark Scheme Unit 3Documento15 pagineChemistry Jun 2010 Mark Scheme Unit 3dylandonNessuna valutazione finora
- Osce05ans 110918053819 Phpapp01Documento20 pagineOsce05ans 110918053819 Phpapp01masood alamNessuna valutazione finora
- Rezhna Hassan FarajDocumento2 pagineRezhna Hassan FarajchristoptNessuna valutazione finora
- Wet Chemical Pre E PresentationDocumento310 pagineWet Chemical Pre E PresentationEdwardAlexanderGarciaNessuna valutazione finora
- PANCREATITISDocumento38 paginePANCREATITISVEDHIKAVIJAYANNessuna valutazione finora
- WD 02Documento1 paginaWD 02Elezer BatchoNessuna valutazione finora
- MetDocumento41 pagineMetadityaNessuna valutazione finora
- Akshaya Vanam: Indian SandalwoodDocumento52 pagineAkshaya Vanam: Indian Sandalwoodprasadgss100% (4)
- Moldex Realty, Inc. (Linda Agustin) 2.0 (With Sound)Documento111 pagineMoldex Realty, Inc. (Linda Agustin) 2.0 (With Sound)Arwin AgustinNessuna valutazione finora
- Health Problems Vocabulary Esl Matching Exercise Worksheet For KidsDocumento2 pagineHealth Problems Vocabulary Esl Matching Exercise Worksheet For KidsTarisubhNessuna valutazione finora
- FP Lecture Midterm Exam Sec - Sem.2020Documento4 pagineFP Lecture Midterm Exam Sec - Sem.2020SAEEDA ALMUQAHWINessuna valutazione finora
- Introduction To Kalman FilterDocumento4 pagineIntroduction To Kalman FilterArghya MukherjeeNessuna valutazione finora
- SweetenersDocumento23 pagineSweetenersNur AfifahNessuna valutazione finora
- Bsi MD Ivdr Conformity Assessment Routes Booklet Uk enDocumento15 pagineBsi MD Ivdr Conformity Assessment Routes Booklet Uk enGuillaumeNessuna valutazione finora
- Advanced Aesthetics: The Definitive Guide For Building A Ripped and Muscular PhysiqueDocumento73 pagineAdvanced Aesthetics: The Definitive Guide For Building A Ripped and Muscular PhysiqueRoger murilloNessuna valutazione finora
- 1704 Broschuere Metal-Coating en EinzelseitenDocumento8 pagine1704 Broschuere Metal-Coating en EinzelseiteninterponNessuna valutazione finora
- Initiation in Pre-Tantrasamuccaya Kerala Tantric Literature PDFDocumento24 pagineInitiation in Pre-Tantrasamuccaya Kerala Tantric Literature PDFVenkateswaran NarayananNessuna valutazione finora
- Vegetable Rates - 02-01-2021Documento454 pagineVegetable Rates - 02-01-2021Saurabh RajputNessuna valutazione finora
- Biasing Opamps Into Class ADocumento11 pagineBiasing Opamps Into Class AsddfsdcascNessuna valutazione finora
- North Central Mindanao College: Maranding, Lala, Lanao Del NorteDocumento8 pagineNorth Central Mindanao College: Maranding, Lala, Lanao Del NorteAnalyn FielNessuna valutazione finora
- International Travel Insurance Policy: PreambleDocumento20 pagineInternational Travel Insurance Policy: Preamblethakurankit212Nessuna valutazione finora
- 3rd Stage ComplicationsDocumento84 pagine3rd Stage ComplicationsDream100% (1)
- ESM-4810A1 Energy Storage Module User ManualDocumento31 pagineESM-4810A1 Energy Storage Module User ManualOscar SosaNessuna valutazione finora
- Thermobaric Effects Formed by Aluminum Foils Enveloping Cylindrical ChargesDocumento10 pagineThermobaric Effects Formed by Aluminum Foils Enveloping Cylindrical ChargesAnonymous QFUEsUAnNessuna valutazione finora
- T 1246784488 17108574 Street Lighting Control Based On LonWorks Power Line CommunicationDocumento3 pagineT 1246784488 17108574 Street Lighting Control Based On LonWorks Power Line CommunicationsryogaaNessuna valutazione finora
- Lecture 1 1489485680Documento52 pagineLecture 1 1489485680Dato TevzadzeNessuna valutazione finora