Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Final Nursing Care Plan For Spirituality
Caricato da
Jerwelyn JoyDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Final Nursing Care Plan For Spirituality
Caricato da
Jerwelyn JoyCopyright:
Formati disponibili
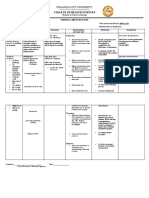
NURSING CARE PLAN FOR SPIRITUALITY CUES S-The client verbalized, Bakit ako nagkakanser?
Siguro pinaparusahan na ako ni Lord dahil sa paninigarilyo ko at pag-inom ng alak - The client also verbalized, Siguro dahil na rin hindi ako nakakapagsimba na pati hindi na rin ako nakakapagdasal. - The client also said, Natatakot talaga akong mamamatay. Sino mag-aalaga sa mga anak ko? O- during the interview, the client was emotional and tearful - There were no observed rosaries or other religious articles on the patients hands NURSING DIAGNOSIS Spiritual Distress related to chronic illness of self (cancer that metastasize) as evidenced by questioning why God has done this GOAL AND NURSING RATIONALE OBJECTIVES INTERVENTION Spiritual distress is Goal: an experience of After an 8 hour profound shift of nursing disharmony in the interventions, the persons belief or patient will value system that express meaning threatens the and purpose in life meaning of his or and a sense of her life. During connectedness spiritual distress with self and the patient loses others. hope, questions his or her belief Objectives: system, or feels After one hour of Determine clients Provides baseline separated from his nursing for planning care religious/spiritual or her personal interventions, the orientation, current and accessing source of comfort client will discuss involvement, and appropriate and strength. Pain, beliefs/values resources. presence of chronic or terminal about spiritual conflicts. illness, impending issues. surgery, and the Be aware of It is still possible death or illness of influence of affect to be helpful loved ones are to client while caregivers belief crises that may remaining neutral/ system. cause spiritual; not espousing own distress. beliefs. (Carpenito-Moyet, 2006; Gulanick, Promotes Establish 2007; Berman, et awareness and environment that al, 2008) identification of promotes free feelings so they expression of feelings and can be dealt with concerns. Provide calm, peaceful setting when ANALYSIS EVALUATION EFFECTIVENESS: Was the client able to express meaning and purpose in life and a sense of connectedness with self and others? ____ Yes ____ No If No, why? ________________
Was the client able to discuss beliefs/values about spiritual issues? ____ Yes ____ No If No, why? ________________
or near him. After 2 hours of nursing interventions, the client will verbalize acceptance of self as not deserving illness or no one is to blame.
possible. Be open to the Encourages clients feelings expression of inner about illness or fears and concerns death, and teaches the client to value of confronting issues. Listen to client/SOs reports/expressions of anger, concern, alienation from God, belief that situation is a punishment for wrongdoing, and so forth. Note sense of futility, feelings of hopelessness and helplessness, lack of motivation to help self. Helpful to understand client/SOs point of view and how they are questioning their faith in the face of tragedy. . Was the client able to verbalize acceptance of self as not deserving illness or no one is to blame.? ____ Yes ____ No If No, why? ________________
These thoughts and feelings can result in the client feeling paralyzed and unable to move forward to resolve the situation. May indicate need for further intervention to prevent suicide attempt.
Listen to expressions of inability to find meaning in life, reason for living. Evaluate for suicidal ideation. Help client find a reason for living.
Helps client find own solutions to
concerns. . Helps client to begin to look at basis for spiritual confusion. Note: There is a potential for care providers belief system to interfere with client finding own way. Therefore it is most beneficial to remain neutral and not espouse own beliefs. Blaming self for what has happened impedes dealing with the grief process and needs to be discussed and dealt with.
Make time for nonjudgmental discussion of philosophic issues/questions about spiritual impact of current events/situation.
Discuss difference between grief and guilt and help client to identify and deal with each, assuming responsibility for own actions, expressing awareness of the consequences of acting out of false guilt. Use therapeutic communication skills of reflection and ActiveListening. Discuss use
Can help to heal past and present pain.
Promotes trust and
of/provide opportunities for client/SO to experience meditation, prayer and forgiveness. Provide information that anger with God is a normal part of the grieving process. Develop therapeutic nurseclient relationship. Ask how you can be most helpful. Convey acceptance of clients spiritual beliefs/ concerns. After 2 hours of nursing intervention, the client will be able to identify resources appropriately.
comfort, encouraging client to be open about sensitive matters.
Promotes sense of hope and willingness to continue efforts to improve situation.
Determine support Presence or lack of systems available support systems to client/SO(s). can affect clients recovery. Identify and may refer to resources that can be helpful (e.g., pastoral/parish nurse or religious counselor, crisis counselor, psychotherapy) Assist client to identify SO(s) nad people who could Specific assistance may be helpful to recovery, (e.g., relationship problems, suicidal ideation).
Was the client able to identify resources? appropriately ____ Yes ____ No If No, why? ________________
Ongoing support is required to enhance sense of
provide support as needed.
connectedness and continue progress toward goals. Provides answers to spiritual questions, assist in the journey of selfdiscovery, and can help client learn to accept and forgive self.
Assist clients to identify spiritual resources that could be helpful (e.g., contact with spiritual advisor who has qualifications in dealing with terminal or chronic illness Encourage participation in support groups if possible.
Discussing concerns and questions with others can help client resolve feelings.
(Doenges et al, Nurses Pocket Guide Diagnoses, Prioritized Interventions and Rationales 11th Edition, page 646-651)
Submitted By: Campos, Jennilise C. Capistrano, Maria Marza Beverly B. Castillo, Hubert Ban M. Coronel, Romina G. De Luna, Alvin Michael M. Dejamco, Kristine Joy G. BSN 203 August 17, 2011
Potrebbero piacerti anche
- NCP Spiritual DistressDocumento3 pagineNCP Spiritual DistressEm Emer Emerson100% (1)
- Spiritual NCPDocumento12 pagineSpiritual NCPGayzel Dela CruzNessuna valutazione finora
- Nursing Care Plan For Readiness For Enhanced Spiritual Well Being NCPDocumento4 pagineNursing Care Plan For Readiness For Enhanced Spiritual Well Being NCPderic83% (6)
- NCP Spiritual DistressDocumento3 pagineNCP Spiritual DistressAngelo ArabejoNessuna valutazione finora
- FNCP Proper RevisedDocumento2 pagineFNCP Proper RevisedKevinNessuna valutazione finora
- Anticipatory GrievingDocumento2 pagineAnticipatory GrievingKM100% (5)
- NCP Self EsteemDocumento4 pagineNCP Self Esteemeinghel_24100% (2)
- Activity Schizophrenia: I. Case ScenarioDocumento3 pagineActivity Schizophrenia: I. Case ScenarioDan Hizon67% (3)
- A. Not My Job!: Ncmp109 Bioethics: Case StudyDocumento2 pagineA. Not My Job!: Ncmp109 Bioethics: Case StudyAudrey Ann Acob100% (1)
- NCPDocumento3 pagineNCPChrisTine M. MoralesNessuna valutazione finora
- Anxiety NCPDocumento2 pagineAnxiety NCPAnaleah MalayaoNessuna valutazione finora
- Anxiety Related To Hospitalization and Disease Condition As Manifested by Fiscal Expression and VerbalizationDocumento2 pagineAnxiety Related To Hospitalization and Disease Condition As Manifested by Fiscal Expression and VerbalizationmonaNessuna valutazione finora
- NCP AnxietyDocumento1 paginaNCP AnxietyGrace MellaineNessuna valutazione finora
- Nursing Care Process (NCP) Stress Overload PrepartumDocumento2 pagineNursing Care Process (NCP) Stress Overload PrepartumFrederene JavelonaNessuna valutazione finora
- NCP GrievingDocumento5 pagineNCP GrievingEllenare Racion33% (3)
- NCPDocumento6 pagineNCPhsiria100% (1)
- This Study Resource Was Shared Via: Fncp-Health Deficit: Diabetes MellitusDocumento3 pagineThis Study Resource Was Shared Via: Fncp-Health Deficit: Diabetes MellitusAlhadzra AlihNessuna valutazione finora
- NCPDocumento3 pagineNCPeun kyung shinNessuna valutazione finora
- Cognitive Perception Pattern of Nursing CareDocumento9 pagineCognitive Perception Pattern of Nursing CareGloria Khan100% (4)
- Assessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationDocumento4 pagineAssessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationTedd CamilingNessuna valutazione finora
- Nursing Care Plan For Rape Trauma Syndrome NCPDocumento5 pagineNursing Care Plan For Rape Trauma Syndrome NCPderic100% (4)
- Key Concepts Pre-Entry Phase of CoparDocumento2 pagineKey Concepts Pre-Entry Phase of CoparLegendXNessuna valutazione finora
- NCP Delayed Wound RecoveryDocumento5 pagineNCP Delayed Wound RecoveryDarkCeades100% (2)
- Nursing Care Plan: Phinma University of IloiloDocumento2 pagineNursing Care Plan: Phinma University of IloiloBeatrice ManingasNessuna valutazione finora
- Nursing Care Plan (ImpairedphyssicalDocumento5 pagineNursing Care Plan (ImpairedphyssicalkuroroexileNessuna valutazione finora
- Gout N C P BY BHERU LALDocumento1 paginaGout N C P BY BHERU LALBheru LalNessuna valutazione finora
- NCPDocumento2 pagineNCPsphinx809100% (2)
- Focus Diagnosis Action ResponseDocumento2 pagineFocus Diagnosis Action ResponseGrape JuiceNessuna valutazione finora
- NCP Anxiety Related To Unconscious Conflict About Essential Goals and Values of Life Into Financial Instability Causing DistressDocumento2 pagineNCP Anxiety Related To Unconscious Conflict About Essential Goals and Values of Life Into Financial Instability Causing DistressMa. Elaine Carla Tating0% (2)
- NCPDocumento1 paginaNCPEve DelosoNessuna valutazione finora
- Impaired Physical MobilityDocumento3 pagineImpaired Physical Mobilityvidagurl0% (1)
- NCP AnxietyDocumento3 pagineNCP AnxietyLord James De GuzmanNessuna valutazione finora
- NCP: Acute GastroenteritisDocumento3 pagineNCP: Acute GastroenteritishauteanicoleNessuna valutazione finora
- Risk For Disproportionate GrowthDocumento8 pagineRisk For Disproportionate GrowthRahajeng Intan HandayaniNessuna valutazione finora
- COURSE TASK 1 Increased ICP POLICIOS, SHARMAINE ANNE M. BSN 3Y2 - 3ADocumento2 pagineCOURSE TASK 1 Increased ICP POLICIOS, SHARMAINE ANNE M. BSN 3Y2 - 3ASHARMAINE ANNE POLICIOS100% (1)
- NCP LymphedemaDocumento1 paginaNCP Lymphedemayasira50% (2)
- Nutrition HTPDocumento3 pagineNutrition HTPAdriene Fay DominguezNessuna valutazione finora
- Developing Work Groups For Community Health DevelopmentDocumento4 pagineDeveloping Work Groups For Community Health DevelopmentStephanie Palma LladaNessuna valutazione finora
- NCPDocumento3 pagineNCPkristina_zamoraNessuna valutazione finora
- College of Health Sciences: Urdaneta City UniversityDocumento2 pagineCollege of Health Sciences: Urdaneta City UniversityDan Dan Manaois100% (1)
- Working With Groups Towards Community DevelopmentDocumento8 pagineWorking With Groups Towards Community DevelopmentAngel Joy CATALAN (SHS)Nessuna valutazione finora
- NCP Violence - OtherDocumento2 pagineNCP Violence - OtherRosean Venus SilangNessuna valutazione finora
- Learning Feedback DiaryDocumento1 paginaLearning Feedback DiaryRendel FernandezNessuna valutazione finora
- NCP-Impaired Social InteractionDocumento1 paginaNCP-Impaired Social InteractionopxNessuna valutazione finora
- Impaired Physical MobilityDocumento7 pagineImpaired Physical MobilityVianah Eve EscobidoNessuna valutazione finora
- Ineffective Role Perf Romance FinalDocumento1 paginaIneffective Role Perf Romance Finalasymptomaticcrisis0% (1)
- NCP StressDocumento2 pagineNCP StressWaqas Javed100% (7)
- Activity IntoleranceDocumento2 pagineActivity IntoleranceSenyorita KHaye100% (4)
- Situation 1Documento18 pagineSituation 1Maler De VeraNessuna valutazione finora
- Nursing Care Plan2 CVADocumento4 pagineNursing Care Plan2 CVAhermesdave1Nessuna valutazione finora
- Nursing Care PlanDocumento3 pagineNursing Care Planautoeroticasphaxia50% (8)
- MOriamin ForteDocumento1 paginaMOriamin Forteianecunar100% (3)
- Quiz 1 NCM 112 RLEDocumento3 pagineQuiz 1 NCM 112 RLEChriz Lech50% (2)
- Trichomonas Vaginalis NCPDocumento2 pagineTrichomonas Vaginalis NCP3S - JOCSON, DENESE NICOLE LEE M.Nessuna valutazione finora
- Impaired Ability To ExerciseDocumento3 pagineImpaired Ability To ExerciseKim Franzel M. RabeNessuna valutazione finora
- Unit 1:: Assessment, Diagnosis, Intervention, Evaluation and DocumentationDocumento29 pagineUnit 1:: Assessment, Diagnosis, Intervention, Evaluation and DocumentationRahil RajNessuna valutazione finora
- Nursing DiagnosisDocumento2 pagineNursing DiagnosisEvianne Jersey LofstedtNessuna valutazione finora
- hw420 Unit 9 AssignmentDocumento12 paginehw420 Unit 9 Assignmentapi-569132011Nessuna valutazione finora
- Collecting Subjective DataDocumento18 pagineCollecting Subjective DataNadia SolohNessuna valutazione finora
- Eating Disorder TreatmentDocumento24 pagineEating Disorder Treatmentpuchio100% (1)
- NCP AirwayDocumento2 pagineNCP AirwayJerwelyn JoyNessuna valutazione finora
- HYPERTHERMIADocumento5 pagineHYPERTHERMIAJerwelyn JoyNessuna valutazione finora
- Drugs BipoDocumento11 pagineDrugs Bipojerwelyn_joyNessuna valutazione finora
- BennyDocumento1 paginaBennyJerwelyn JoyNessuna valutazione finora
- NCP LessDocumento3 pagineNCP LessJerwelyn JoyNessuna valutazione finora
- Cooking Methods For ChickenDocumento2 pagineCooking Methods For ChickenJerwelyn JoyNessuna valutazione finora
- Edited NCP AnxietyDocumento6 pagineEdited NCP AnxietyJerwelyn Joy100% (6)
- DRUGSDocumento1 paginaDRUGSJerwelyn JoyNessuna valutazione finora
- Free Past Life Regression Report 1Documento21 pagineFree Past Life Regression Report 1Pav IvNessuna valutazione finora
- Caleb Parker-Johnson - 2017 Socialization-ReviewDocumento1 paginaCaleb Parker-Johnson - 2017 Socialization-Reviewapi-404482475Nessuna valutazione finora
- Personality and TeachingDocumento11 paginePersonality and TeachingJona AddatuNessuna valutazione finora
- The Intellectual and Emotional Traps by Harry BrowneDocumento3 pagineThe Intellectual and Emotional Traps by Harry BrownethankyouforthisNessuna valutazione finora
- CasesDocumento4 pagineCasesGrooming session with IqraNessuna valutazione finora
- History of Experimental PsychologyDocumento12 pagineHistory of Experimental PsychologyamrandomaNessuna valutazione finora
- Responding With Positive DisciplineDocumento34 pagineResponding With Positive DisciplineGladys100% (1)
- Introduction To SMART Objectives and SMART GoalsDocumento9 pagineIntroduction To SMART Objectives and SMART GoalsRandy ManaloNessuna valutazione finora
- MTA Cooperative GroupDocumento10 pagineMTA Cooperative GroupmatiasNessuna valutazione finora
- Counselling and Its Effect On Perceived Stress Among Young AdultsDocumento6 pagineCounselling and Its Effect On Perceived Stress Among Young AdultsTJPRC PublicationsNessuna valutazione finora
- Section 6 - Counseling PrinciplesDocumento31 pagineSection 6 - Counseling PrinciplesMALOU ELEVERANessuna valutazione finora
- Behaviorist TheoryDocumento2 pagineBehaviorist TheoryJeremiah Joshua JohnNessuna valutazione finora
- Disciplines in Social SciencesDocumento76 pagineDisciplines in Social SciencesDeanne Angeline L. AquinoNessuna valutazione finora
- Thomas Assessments India InfopagerDocumento1 paginaThomas Assessments India Infopagersachinthomas123Nessuna valutazione finora
- DocumentDocumento10 pagineDocumentCr Zaidi Abu HassanNessuna valutazione finora
- Existential TherapyDocumento41 pagineExistential TherapyBlack Rose100% (3)
- Components of Culture: A) Natural Knowledge B) Technological Knowledge C) Supernatural Knowledge D) Magical KnowledgeDocumento10 pagineComponents of Culture: A) Natural Knowledge B) Technological Knowledge C) Supernatural Knowledge D) Magical KnowledgealexNessuna valutazione finora
- Do Not Just Dream, Make It Happen Answer The Following Questions: 1.) Who Are You and What Would You BecomeDocumento3 pagineDo Not Just Dream, Make It Happen Answer The Following Questions: 1.) Who Are You and What Would You BecomeMickaella VergaraNessuna valutazione finora
- Role of Spiritual Intelligence in Enhancing Emotional Intelligence and Reducing Stress in An OrganizationDocumento9 pagineRole of Spiritual Intelligence in Enhancing Emotional Intelligence and Reducing Stress in An OrganizationMadhavi DeshpandeNessuna valutazione finora
- The Discipline of CounselingDocumento91 pagineThe Discipline of CounselingJohn Michael Bueno100% (3)
- Group Report Developing EthicsDocumento3 pagineGroup Report Developing Ethicsanton sabinoNessuna valutazione finora
- Determinants of Organizational Citizenship BehaviourDocumento11 pagineDeterminants of Organizational Citizenship BehaviourClaude JobNessuna valutazione finora
- Attachments FlashcardsDocumento39 pagineAttachments FlashcardsJay DaviesNessuna valutazione finora
- AutismDocumento9 pagineAutismAmr Ramazan IbrahimNessuna valutazione finora
- FTMendoza - FDD - Form1 - NBC - ENGR POCOT - JULY28, 2020Documento3 pagineFTMendoza - FDD - Form1 - NBC - ENGR POCOT - JULY28, 2020Eller-Jed Manalac MendozaNessuna valutazione finora
- Sex Trafficking ReflectionDocumento2 pagineSex Trafficking Reflectionapi-248999232Nessuna valutazione finora
- Speech and Oral Communication LessonsDocumento37 pagineSpeech and Oral Communication LessonsIrah LamosteNessuna valutazione finora
- Wilson Kiptonui Samoei PDFDocumento96 pagineWilson Kiptonui Samoei PDFEnelrejLeisykGarillosNessuna valutazione finora
- Impoving Suicide PreventionDocumento14 pagineImpoving Suicide PreventionClinica MonserratNessuna valutazione finora
- Clinical Assessment Marking and Interpretation FormDocumento2 pagineClinical Assessment Marking and Interpretation FormBob UyNessuna valutazione finora