Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Bacillary Dysentry
Caricato da
Khevin ZabalaDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Bacillary Dysentry
Caricato da
Khevin ZabalaCopyright:
Formati disponibili
VIII.
Period of Communicability Bacillary dysentery is communicable during the acute phase and until the microorganism is absent from the bowel discharges. This can last as long as four weeks. Asymptomatic carriers have the ability to transmit disease. The duration of carriage may be reduced with the use of antibiotics. A few individuals became carriers for a year or two. IX. Treatment Anyone with bloody diarrhea needs immediate medical help. Treatment often starts with an oral rehydrating solution, water mixed with salt and carbohydrates to prevent dehydration. Liquid or soft diet until diarrhea stops, then returns to normal diet. The medical treatment for dysentery includes the administration of antibiotics to treat and cure the infection caused by the agents; antihelminthic caused by parasitic worms; cases of schistosomiasis may be treated with medications which are specific to the agents causing the disease or infection. If Shigella is suspected and it is not too severe, the doctor may recommend letting it run its course, usually less than a week. The patient will be advised to replace fluids lost through diarrhea. If the Shigella is severe, the doctor may prescribe antibiotics for adults and children, if the strai is susceptible, such as Ciloxan and Cipro, which contains ciprofloxacin, TMP-SMX or Bactrim and Septra, containing trimethoprim-sulfamethoxazole, and NegGram which has nalidixic acid. Also, antibiotics such as, Ampicillin, Tetracycline or Cotrimoxazole is useful in severe cases or when the spread of infection to other people is likely and when the patient is very young. For adults and children, if the strain is susceptible, are ciprofloxacin or TMP/SMX or azithromycin. Unfortunately, many strains of shigella are becoming resistant to common antibiotics, and effective medications are often in short supply in developing countries. If necessary, a doctor may have to reserve antibiotics for those at highest risk for death, including young children, people over 50, and anyone suffering from dehydration or malnutrition. Antibiotic resistance frequently develops after treatment. Use of antibiotics will shorten the period of fecal excretion of the infecting strain and will shorten the clinical course of disease often to a few days. Antibiotics are often helpful for those with symptoms but resistance is becoming a problem. Although fluoroquinolones are currently effective in treating adults, resistance to fluoroquinolones among Shigella spp. is emerging, and their use in children is subject to limitations. Azithromycin and third-generation cephalosporins are also effective in the treatment of shigellosis, but monitoring of Shigella spp. isolates to detect the emergence of resistance is essential. Treatment consists mainly of replacing fluids and salts lost because of diarrhea. Oral replacement is satisfactory for most people, but some may need to receive fluids intravenously. In most cases, the disease resolves within 4 to 8 days without antibiotics. Severe infections may last 3 to 6 weeks. Antibiotics such as trimethoprim-sulfamethoxazole, norfloxacin, ciprofloxacin, or furazolidone may be
given when the person is very young or very old, when the disease is severe, or when there is a high risk of the infection spreading to other people. The severity of the symptoms and the length of time the stool contains Shigella are reduced with antibiotics. Anti-diarrheal drugs (such as diphenoxylate or loperamide) may prolong the infection and should not be used since they delay fecal excretion. More recent expert advice is that antimotility agents are contraindicated. One of the most common ways of dealing with dysentery is ORS therapy or intravenous replacement of fluid. This is done in order to bring down the electrolyte of the body to normalcy. Specially made ORS such as pedialyte and infalyte have been prepared for dehydration in children. IV might be infused with normal saline (with electrolyte) to prevent dehydration. Fluids and electrolyte are replaced if excessive fluid loss through diarrhea or vomiting. Dysentery is initially managed by maintaining fluid intake using oral rehydration therapy. If this treatment cannot be adequately maintained due to vomiting or the profuseness of diarrhea, hospital admission may be required for intravenous fluid replacement. Ideally, no antimicrobial therapy should be administered until microbiological microscopy and culture studies have established the specific infection involved. When laboratory services are not available, it may be necessary to administer a combination of drugs, including an amoebicidal drug to kill the parasite and an antibiotic to treat any associated bacterial infection. Dysentery caused by parasitic worms is treated with the help of anthelminthic medications like mebendazole, available in the name of Vermox. Cases of schistosomiasis may be treated with medications which are specific to the agents causing the disease or infection such as oxamniquine, metrifonate and praziquantel. Advancement of medical science has led to the development of drugs and medicines which cannot be outrivaled by the viruses or bacteria. One of the antiprotozoal drugs developed is known as tinidazole, which is available by the name of Fasigyn and Tindamax. But it is harmful for pregnant women who suffer from dysentery. Another recent addition is nitazoxanide, available as Alinia. Dysentery is actually not so dangerous except caused by amoeba or bacteria which have the resistance to even outdo medications or drug treatment. A proper treatment ensures a fast and easy recovery within 10 to 15 days. But the prognosis of the disease may depend on the immune status of the patient, the kind of dysentery that one suffers from and the severity of the disease. However, with proper treatment and the maintenance of both personal and public hygiene shall help in the cure from dysentery and prevent the risk of contracting the same. In children especially, antipyretic medicines can reduce temperature and help to prevent convulsions. X. Prognosis/Outcome/Complications
Most shigella infections are mild and don't require drastic treatment. However, in a severe attack, excessive dehydration can be fatal (especially in infants and young children) if treatment is unsuccessful. Bacteraemia occurs primarily in malnourished children and carries a mortality rate of 20% as a result of acute renal failure, haemolysis, thrombocytopenia, gastrointestinal haemorrhage, and shock. Hemolytic uremic syndrome may complicate infections with Shigella spp. and E. coli, and it carries a mortality rate in excess of 50%. Hemolytic uremic syndrome is characterized by acute hemolysis, renal failure, uraemia, and disseminated intravascular coagulation. Reactive arthritis (ReA), previously known as Reiter's syndrome, is an autoimmune condition that develops in response to an infection in another part of the body. Coming into contact with bacteria and developing an infection can trigger reactive arthritis. It is commonest in men aged 20 to 40 and with the HLAB27 antigen. It starts 2 to 4 weeks after infection and may be chronic and relapsing. The disease tends to last from 1 day to 1 month with an average of 1 week. Mortality is rare but can occur in malnourished children and the elderly. XI. Preventive/ Control Measures, Vaccines If you have the infection, you can protect others around you by washing your hands regularly with soap and water, especially after using the toilet, after changing diapers, and before preparing food. While you are suffering from diarrhea you should not go to work/school. Simple precautions can be taken to prevent getting Shigellosis: Good personal hygiene; Toilet hygiene; Wash soiled clothing and bed linen; Handling food; Sanitation of food utensils. There are currently no vaccines against shigella although trials are underway in America. Sanitation and clean water is important in developing countries. In developed nations the concern is hand washing and personal hygiene. Preparation of fresh produce is also important. In addition to improved sanitation and hygiene, several vaccine candidates for Shigella are in various stages of development. According to the World Health Organization, candidates include live attenuated, conjugate, ribosomal, and proteosome vaccines are in development. There are promising results for a vaccine against serotype 1, which otherwise show large resistance against antibiotics. Epidemiology and volunteer studies have shown that protective immunity to Shigellas is directed to the O-somatic antigen and is narrowly type-specific, which has hampered the development of an effective Shigella vaccine. Strong mucosal sIgA anti-O-antigen antibody responses follow wild-type infection and experimental challenge. Passive administration of cow's milk immunoglobulin that contained hightiter anti S flexneri 2a antibodies protected volunteers from experimental challenge with wild type S flexneri, whereas cow's milk with low titers of such antibodies did
not . In addition, cell-mediated immunity mechanisms, including IFN-secreting T cells, seem to play a role in recovery and immunity. Candidate shigellosis vaccines currently in advanced development include both polysaccharide conjugate and live attenuated vaccines and mostly focus on the most frequently isolated S flexneri 2a and S sonnei, as well as on Sd1, due to the severity of cases.
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- 5113 P Facial WeaknessDocumento12 pagine5113 P Facial WeaknessHarish Radhi DipocaksonoNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- D Physiology of RespirationDocumento45 pagineD Physiology of RespirationValluri Mukesh100% (1)
- Chemotherapy Protocols V 101Documento42 pagineChemotherapy Protocols V 101Charm TanyaNessuna valutazione finora
- MethergineDocumento2 pagineMethergineJulie May33% (3)
- IV FluidsDocumento3 pagineIV FluidsEvangeline San Jose83% (6)
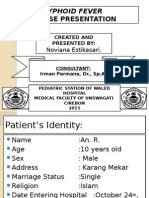
- Typhoid Case PresentationDocumento17 pagineTyphoid Case PresentationAbdulMazidZabir0% (1)
- CSS Airway Management RickyDocumento53 pagineCSS Airway Management RickyArtha PutuNessuna valutazione finora
- Eurasia Research Pharma Corporation Standard Operatig ProcedureDocumento1 paginaEurasia Research Pharma Corporation Standard Operatig ProcedureKhevin ZabalaNessuna valutazione finora
- Sodium Ascorbate BoxDocumento2 pagineSodium Ascorbate BoxKhevin ZabalaNessuna valutazione finora
- Mefenamic Acid BoxDocumento2 pagineMefenamic Acid BoxKhevin ZabalaNessuna valutazione finora
- Module III-H Principles of Permitted EvilDocumento11 pagineModule III-H Principles of Permitted EvilKhevin ZabalaNessuna valutazione finora
- 1 Christian Concept of The Human PersonDocumento9 pagine1 Christian Concept of The Human Personmar234Nessuna valutazione finora
- Health and Wellness Calendar 2020Documento1 paginaHealth and Wellness Calendar 2020CHARMAINE ACEVEDONessuna valutazione finora
- 4 EL Husseinys Essentials of Cardiovascular System @eduwaves360Documento236 pagine4 EL Husseinys Essentials of Cardiovascular System @eduwaves360ahmed_abu_alrobNessuna valutazione finora
- BF Builders and Construction Corporation Hiv/Aids Workplace Policy and ProgramDocumento4 pagineBF Builders and Construction Corporation Hiv/Aids Workplace Policy and Programglenn dalesNessuna valutazione finora
- Unit 3 Part 2 Rheumatoid ArthritisDocumento10 pagineUnit 3 Part 2 Rheumatoid ArthritisReman AlingasaNessuna valutazione finora
- Daily-Inpatient-Care-Checklist 112118 346713 284 45189 v1Documento5 pagineDaily-Inpatient-Care-Checklist 112118 346713 284 45189 v1Andrew McGowanNessuna valutazione finora
- SOP For Staphylococcus AureusDocumento4 pagineSOP For Staphylococcus AureusDr. StormNessuna valutazione finora
- Composite Hemangioendothelioma An Unusual Presentation of A Rare Vascular TumorDocumento5 pagineComposite Hemangioendothelioma An Unusual Presentation of A Rare Vascular TumorTian Nopita SariNessuna valutazione finora
- Special Chemistry: Test Name Current Result Previous Result Unit Normal RangeDocumento1 paginaSpecial Chemistry: Test Name Current Result Previous Result Unit Normal RangeddssNessuna valutazione finora
- USMLE Step 1 Study Plan 2Documento3 pagineUSMLE Step 1 Study Plan 2BenHansonNessuna valutazione finora
- Κατάσταση Πρωτοτύπων-Αντιγράφων φαρμάκων - Απρίλιος 2011Documento121 pagineΚατάσταση Πρωτοτύπων-Αντιγράφων φαρμάκων - Απρίλιος 2011nosfarNessuna valutazione finora
- Skin ConditionsDocumento11 pagineSkin ConditionsElza ShainidzeNessuna valutazione finora
- Amboss CACES-EcuadorDocumento44 pagineAmboss CACES-EcuadorStorage Liz0% (1)
- Plastic SurgeryDocumento5 paginePlastic Surgeryhasif21Nessuna valutazione finora
- Brochure XN-L 550 450 350 330 - MNDocumento8 pagineBrochure XN-L 550 450 350 330 - MNarkoudelosNessuna valutazione finora
- Surgical Management of Fourniers Gangrene A Seven Year Experience at The Philippine General HospitalDocumento6 pagineSurgical Management of Fourniers Gangrene A Seven Year Experience at The Philippine General HospitalGian PagadduNessuna valutazione finora
- BrochureDocumento2 pagineBrochureZubair ShaikhNessuna valutazione finora
- Immunization Schedule in India 2017 (Latest !!)Documento13 pagineImmunization Schedule in India 2017 (Latest !!)rajNessuna valutazione finora
- Elevated BilirubinDocumento5 pagineElevated BilirubinNovita ApramadhaNessuna valutazione finora
- Vaginal MicrobiomeDocumento9 pagineVaginal MicrobiomeRika Yulizah GobelNessuna valutazione finora
- Aplikasi Terapi Generalis Dalam Pemberian Asuhan Keperawatan Jiwa Pada Nn. R Dengan HalusinasiDocumento13 pagineAplikasi Terapi Generalis Dalam Pemberian Asuhan Keperawatan Jiwa Pada Nn. R Dengan Halusinasicindy veronikaNessuna valutazione finora
- PEH 3 Lesson 2Documento3 paginePEH 3 Lesson 2ShaineMaiko MarigocioNessuna valutazione finora
- Prudential BSN Takaful Berhad Investment-Linked Plan IllustrationDocumento19 paginePrudential BSN Takaful Berhad Investment-Linked Plan IllustrationhilmiyaidinNessuna valutazione finora
- Use of Chlorhexidine Varnishes in Preventing and Treating Periodontal DiseaseDocumento4 pagineUse of Chlorhexidine Varnishes in Preventing and Treating Periodontal Diseasetaher adelNessuna valutazione finora