Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Renal Tubular Acidosis Evaluaion
Caricato da
Shailesh Badole Shailesh BadoleDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Renal Tubular Acidosis Evaluaion
Caricato da
Shailesh Badole Shailesh BadoleCopyright:
Formati disponibili
83
Symposium on New Diagnostics
Evaluation of Renal Tubular Acidosis
Arvind Bagga and Aditi Sinha
Division of Nephrology, Department of Pediatrics, All India Institute of Medical Sciences, New Delhi, India
ABSTRACT
Renal tubular acidoses (RTA) comprises of a group of disorders characterized by a low capacity for net acid excretion and persistent hyperchloremic, metabolic acidosis. The RTAs are classified into chiefly three types (types 1,2 and 4) based on clinical and laboratory characteristics. Correct diagnosis involves careful evaluation, including exclusion of other entities causing acidosis. A variety of tests are required to be administered in a stepwise fashion for the diagnosis and characterization of RTA. [Indian J Pediatr 2007; 74 (7) : 679-686] E-mail : arvindbagga@ hotmail.com
Key words : Renal tubular disorders; Metabolic acidosis
Renal tubular acidosis (RTA) is a group of transport defects secondary to reduced proximal tubular reabsorption of bicarbonate (HCO 3-), the distal secretion of protons (hydrogen ion, H +) or both, resulting in impaired capacity for net acid excretion and persistent hyperchloremic metabolic acidosis. In this review, we discuss the pathophysiological basis and clinical and laboratory diagnosis of this condition. Physiology The proximal renal tubule is the site of the bulk of solute and water reabsorption in the nephron. Approximately 60% of the filtered sodium (Na +) is reabsorbed in the proximal segments, along with water, potassium (K +), bicarbonate (HCO3-), phosphate, amino acids and low molecular weight proteins. In contrast, the distal tubule has a specialized role in the final modification of urine concentration and pH. Specialized transporters are involved in the regulation of Na + and K+ reabsorption and H+ secretion, which are shown in Figs. 1-3. Classification of RTA Based on pathophysiology, RTA has been classified into three types: type 1 (distal) RTA; type 2 (proximal) RTA; and type 4 RTA secondary to true or apparent hypoaldosteronism. The above conditions are either secondary to other causes,1 or primary, with or without known genetic defects.
Pathophysiological basis The proximal tubule is the major site for reabsorption of filtered HCO 3 (Fig. 1). The primary defect in proximal RTA is reduced renal threshold for HCO 3, resulting in bicarbonaturia. The proposed mechanisms include defective pump secretion or function of the H + ATPase, the Na+/H+ antiporter, the Na+/K+ ATPase or deficiency of carbonic anhydrase in the brush-border membrane. Proximal RTA may represent isolated or generalized proximal tubular dysfunction, the latter (Fanconi syndrome) characterized by tubular proteinuria and aminoaciduria and variable degrees of bicarbonaturia, phosphaturia, Na + and K+ wasting and glucosuria. K+ wasting is enhanced due to increased distal tubular delivery of Na + and hyperaldosteronism secondary to volume contraction.
Correspondence and Reprint requests : Dr. Arvind Bagga, Department of Pediatrics, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110029, India. [Received January 24, 2007; Accepted February 2, 2007]
Fig. 1. Bicarbonate absorption in the proximal tubule. The secreted H+ combines with luminal HCO 3- to form H 2CO 3, which, under the action of carbonic anhydrase (CA) dissociates to H2O and CO2. The CO2 travels across the membrane into the cell where it combines with OH- to generate HCO3-; HCO3and Na + cross the basolateral membrane using the Na +/ HCO3 - symporter. Na+ also exits the cell via the Na +/K + ATPase.
Indian Journal of Pediatrics, Volume 74July, 2007
679
84
A. Bagga and A. Sinha However, with a severe rate defect, the time spent in tubule lumen may be insufficient for acidification, and there is failure to maximally decrease the urine pH. The defect in secretory distal RTA may be secondary to defective function of H+ ATPase, H+/K+ ATPase, or the Cl - /HCO 3 - exchanger. Patients with the gradient (permeability) defect show normal secretory capacity of H+ but an increased backleak resulting in dissipation of the pH gradient. A subtype exists, where the backleak is due to enhanced membrane permeability to HCO3-, as seen with amphotericin induced RTA. In distal RTA, the titrable acidity and NH4 + secretion is low resulting in systemic acidosis. The cause of hypokalemia is attributed to increased K+ loss in the tubular lumen, urinary Na+ loss and volume contraction leading to aldosterone stimulation that increases tubular K + secretion, and decreased proximal K+ reabsorption.2 Incomplete distal RTA is a variant or milder form of classic distal RTA, in which there is defective tubular H + secretion but plasma HCO3 - levels are normal. Daily net acid excretion is maintained by enhanced ammoniagenesis. Hypercalciuria and hypocitraturia are present, and there is a risk for nephrolithiasis and nephrocalcinosis. Distal RTA associated with hyperkalemia may occur due either to a voltage-defect or rate-defect due to aldosterone deficiency or resistance. The voltage-defect is uncommon and caused by an insufficient negative intratubular potential at the level of cortical collecting duct (Fig. 3), which results in reduced secretion of H+ and K+, with decreased trapping and excretion of NH 4+ and hyperkalemia. Inadequate voltage generation may be due to drugs such as amiloride that inhibit Na+ transport in the cortical collecting tubules, structural defects that inhibit active Na + reabsorption in the tubules such as sickle cell nephropathy and obstructive uropathy, and increased epithelial permeability to Cl - causing its reabsorption and attenuating the negative voltage linked to Na+ reabsorption. The laboratory parameters in the voltage-defect (hyperkalemic distal RTA) resemble classic distal RTA, except for the presence of normo- or hyperkalemia (Table 2). More commonly, hyperkalemia with distal RTA is due to aldosterone resistance or deficiency (type 4 RTA). Aldosterone increases Na + absorption and results in a negative intratubular potential (Fig. 3). It also increases luminal membrane permeability to K+ and stimulates basolateral Na+/K+/ATPase, causing increased urinary K+ losses. Since aldosterone also directly stimulates the proton pump, aldosterone deficiency or resistance is expected to cause hyperkalemia and acidosis. Another major factor in decreasing net H+ excretion in type 4 RTA is the inhibition of ammoniagenesis due to hyperkalemia. In type 4 RTA, maximally acidic urine (<5.5) can be formed, indicating the ability to establish a maximal H+ gradient. However, despite the maximally acidic urine, the rate of ammonium excretion is low.2
Indian Journal of Pediatrics, Volume 74July, 2007
Fig. 2. Mechanism of distal acidification. Intercalated cells in distal tubule mediate HCO3 - absorption through secretion of H+ through H+ ATPase and H+/K+ ATPase. The hydroxyl (OH-) ions generated in the cell through H+ secretion exit the cell by the HCO3 -/Cl- exchanger. The secreted H+ is buffered by luminal ammonia forming NH4 + and phosphate (titrable acids), to prevent a drop in luminal pH that would prevent further H+ secretion.
Fig. 3. Sodium transport in the principal cells. The apical membrane of the principal cells contains an amiloride sensitive Na + channel, which transports Na + into the cell that exits basolaterally via Na+/K + ATPase. Na+ transport creates a lumen negative transepithelial potential that increases the rate of H + secretion (by intercalated cells). (Fig. 2). Aldosterone enhances Na+ absorption and increases H + and K+ secretion.
Metabolic acidosis secondary to decreased secretion of H + ions in the absence of marked decrease in the glomerular filtration rate is characteristic of distal RTA. Patients with distal RTA are unable to excrete ammonium (NH 4+) ions in amounts adequate to keep pace with a normal rate of acid production. In hypokalemic distal RTA, urine pH cannot reach maximal acidity (i.e., remains >5.5) despite systemic acidemia indicating low H+ concentration in the collecting duct. In hypokalemic distal RTA, also known as classic RTA or type 1 RTA, the deficiency is secondary to either a secretory (rate) defect or a gradient (permeability) defect. In the secretory defect, the rate of secretion of H+ is low for the degree of acidosis. Ideally, with a rate defect the ability to maximally acidify the urine should be retained.
680
85
Evaluation of Renal Tubular Acidosis When should RTA be suspected? Clinical features that suggest RTA include growth retardation, failure to thrive, polyuria, polydipsia, preference for savory foods and refractory rickets. Children with proximal RTA often present with stunted growth. Rickets and/or osteomalacia may be associated, and suggest the presence of Fanconi syndrome. Nephrocalcinosis and urolithiasis are not seen. Symptoms related to hypokalemia including weakness and paralysis are uncommon. In children, proximal RTA occurs either as a primary isolated defect or as part of Fanconi syndrome secondary to cystinosis, galactosemia, fructose intolerance, tyrosinemia, Wilson disease or Lowe syndrome.1,3 Clinical features in distal RTA include impairment of growth, polyuria, nephrocalcinosis, nephrolithiasis and symptoms due to hypokalemia. Progression of nephrocalcinosis may lead to chronic renal failure. In children, distal RTA is almost always observed as a primary entity. Rarely, it occurs as a complication of systemic lupus erythematosus or Sjogren syndrome. A proportion of cases with sporadic or autosomal recessive distal RTA show sensorineural deafness, which may be present from birth or manifest in late childhood. Type 4 RTA is associated with hypoaldosteronism or resistance to the action of aldosterone, either isolated or in the context of chronic kidney disease, for example obstructive uropathy. Nephrocalcinosis and urolithiasis are absent and bone lesions are rare. Older children may develop type 4 (RTA) due to advanced tubulointerstitial renal diseases leading to mineralocorticoid resistance, drugs, or with mineralocorticoid deficiency. Pseudo hypo aldosteronism (PHA) type 1 is characterized by saltwasting, hyperkalemia and metabolic acidosis in the presence of markedly elevated plasma renin activity and aldosterone concentration. PHA type 2 is an autosomal dominant syndrome of arterial hypertension, hyperkalemia, metabolic acidosis, and suppressed plasma renin activity.4 Evaluation of RTA Metabolic acidosis may result from extra-renal processes, which result in either increased endogenous acid synthesis (e.g., ketoacidosis) or enhanced extra-renal bicarbonate wasting (diarrhea). Intestinal and pancreatic secretions and bile have considerable quantities of HCO3; therefore, conditions like diarrhea, removal of pancreatic or intestinal secretions or bile by tube drainage or fistula leads to loss of HCO 3 - and metabolic acidosis. 5 Hyperchloremic metabolic acidosis may also result from ureterosigmoidostomy due to presence in the colon of an anion exchange pump that absorbs luminal Cl- (of urinary origin) and exchanges it for HCO3-, and due to colonic absorption of NH4+ (of urinary origin), which releases H+ when metabolized in the liver. Drugs like cholestyramine
Indian Journal of Pediatrics, Volume 74July, 2007
also cause metabolic acidosis by acting as anion exchange resins, where colonic luminal HCO 3 - is absorbed in exchange for Cl- released by the resin.6 RTA may be due to either HCO 3- wasting (proximal RTA) or inability to generate new HCO 3- to buffer endogenous acid (distal RTA). Na+ wasting (as NaHCO3 or as salt of other acids) results in volume contraction and increased avidity of renal Cl- absorption, causing hyperchloremia and normal anion gap acidosis. Since all types of RTA are associated with normal anion gap, the initial step in the evaluation of metabolic acidosis is to determine the plasma anion gap. Step 1. Determine plasma anion gap Plasma anion gap is calculated as follows: Anion gap = [Na+] {[Cl] + [HCO3]} The normal plasma anion gap is 8-16 mEq/L. Important causes of metabolic acidosis with normal anion gap include RTA and diarrhea (Fig. 4). An elevated anion gap suggests conditions associated with excess unmeasured anions, e. g., diabetic ketoacidosis, lactic acidosis due to shock or poor peripheral perfusion, some inborn errors of metabolism, poisonings and uremia. While advanced renal failure with GFR <15 ml/min results in metabolic acidosis with elevated anion gap, normal anion gap (hyperchloremic) acidosis is not infrequent at GFR 20-50 ml/min, especially in patients with tubulointerstitial diseases.7 Step 2. Estimate urine anion gap (UAG) Having established the presence of metabolic acidosis with a normal plasma anion gap, the next step is to distinguish renal (RTA) from extra-renal causes. Halperin, et al proposed UAG (or urine net charge) for estimating NH 4 + excretion in patients with hyperchloremic metabolic acidosis.8 The test is based on the assumption that while metabolic acidosis due to extrarenal HCO3 losses (diarrhea) is associated with high urinary NH4+ excretion, the excretion is low in patients with RTA. Since the sum of charges on cations and anions is equal, Na + + K + + NH 4+ + unmeasured cations = Cl + unmeasured anions The difference between urinary unmeasured anions (sulfates, phosphates, organic anions) and cations (calcium, magnesium) is relatively constant at an approximate value of 80, therefore Na+ + K+ + NH4+ = Cl- + 80, or NH4+ = 80 (Na+ + K+ - Cl-) UAG or urine net charge is the difference between the sum of urinary Na+ and K+ and Cl. Hence, the UAG gives an approximate estimate of urinary NH4+ excretion.
681
86
A. Bagga and A. Sinha
Anion Gap
High anion gap
Normal anion gap (hyperchloremic)
Renal origin
Extrarenal origin
Renal origin
Extrarenal origin
Uremic acidosis Lactic acidosis GFR <15-20 ml/min Diabetic ketoacidosis Starvation ketoacidosis Poisoning by ethylene glycol, methanol or salicylates
Renal tubular acidosis Mild renal insufficiency GFR >15 ml/min
Diarrhea Ureterosigmoidostomy Pancreatic or biliary losses Drugs e.g., cholestyramine,
Fig. 4. Differential diagnosis of the causes of metabolic acidosis. GFR glomerular filtration rate
NH = 80 UAG Under normal circumstances, the UAG is positive due to the presence of dissolved anions. Metabolic acidosis with normal mechanism of renal acidification causes the UAG to become negative due to an increase in the NH4+ synthesis and excretion with the Cl ion. Thus in patients with hyperchloremic metabolic acidosis with preserved mechanism of renal acidification a negative UAG implies adequately increased NH 4+ excretion. A positive UAG indicates inappropriately low renal NH4+ excretion, as in RTA. While initial reports suggested normal excretion of urinary NH4+ (negative UAG) in subjects with proximal RTA, recent studies show that both proximal and distal RTA are characterized by inappropriate levels of urinary NH4+, and thus a positive UAG. There are two caveats in the above approximations. First, the UAG approximates NH 4+ excretion only in patients with chronic hyperchloremic metabolic acidosis. Second, the validity of this value in estimating NH 4+ excretion is limited if the urine pH>6.5, since HCO3 is then a significant urinary anion (but is not included in calculation of the UAG). In presence of significant other anions (e.g., ketones, HCO3) or cations (e.g., lithium) the reliability of UAG is limited. Here, the measurement of urine osmolal gap is more useful than the UAG in estimating urinary NH4+ excretion. The osmolal gap is determined as follows: Urine osmolal gap = measured osmolality calculated osmolality The early morning urine osmolality is measured directly by an osmometer and calculated as given below:
Calculated urine osmolality = 2 [Na+ + K+] + urea + glucose
+ 4
and glucose are in mg/dl). Urinary NH4+ excretion, estimated at half the urine osmolal gap, is considered appropriately increased if the gap >100 mOsm/Kg. Step 3. Determine urine pH Urine pH is useful for assessing the overall integrity of distal urinary acidification. In the presence of systemic acidosis, present spontaneously or induced by ammonium chloride load, the urine pH is normally <5.5. Presence of urine pH >5.5 during metabolic acidosis suggests defective distal secretion of H +. It should however be appreciated that the urine pH measures the concentration of free H+ in the urine. This constitutes <1% of the total amount of H+ secreted in the distal nephron during systemic acidosis, since most protons are excreted as NH4+ or titrable acidity. Urine pH values < 5.5 are seen in subjects with proximal RTA during systemic acidosis and low filtered load (plasma HCO 3 <15 mEq/L), or in patients with selective aldosterone deficiency. If systemic acidosis is absent, an oral ammonium chloride challenge (0.1 mg/Kg) might be given, followed by the measurement of urine pH every hr for the next 28 hr. If the plasma total CO2 content falls by 3-5 mEq/L, the urine pH should fall to <5.5. Another protocol involves giving the same dose of ammonium chloride daily for 3-5 days, followed by measurement of urine pH and urinary NH4+ excretion; the latter should increase 35 times the baseline by the third day of induced acidosis. In patients with liver disease, calcium chloride may be used as an acidifying agent at a dose of 2 mEq/Kg. The pH is measured electrometrically on fresh voided, early morning urine specimen. The use of dipstick is not recommended. Urine kept standing is likely to get contaminated or infected with urea-splitting organisms,
Indian Journal of Pediatrics, Volume 74July, 2007
18
(Urinary levels of electrolytes are in mEq/l and urea
682
87
Evaluation of Renal Tubular Acidosis resulting in high urine pH. The urine pH must be evaluated in conjunction with the urinary NH4+ content to assess the acidification process. Low urine pH does not always imply an intact urinary acidification mechanism, if excretion of NH4+ is low, as might occur in proximal RTA. Patients with chronic metabolic acidosis (e.g., after chronic diarrhea) show increased ammoniagenesis that consumes most distally secreted H + ions, resulting in enhanced urine NH 4 + excretion. The urine pH in this instance may therefore be high despite appropriate H+ excretion. Urine pH should also be interpreted in relation to urine Na+ levels. When urine Na+ level is <5-10 mEq/l, distal H+ secretion is low; high urine pH therefore might not imply a defect in distal urinary acidification in subjects with low urinary Na+ concentration. Step 4. Bicarbonate loading test Sodium bicarbonate is administered as half-strength IV infusion (0.5 mEq/ml) at the rate of 3 ml/minute through a peripheral vein, while measuring urine pH in timed samples taken 30-60 minutes apart. The urine should be collected under mineral oil, with the child voiding in the upright position. A steady state is usually achieved after 3 to 4 hr of start of infusion, and the test is terminated when three samples of timed urine collections show urine pH >7.5. The medication may also be given orally at a dose of 2-4 mEq/Kg/day for 2-3 days, with the aim to achieve a similar urine pH and/or normal plasma pH and HCO 3 -. Interpretation of this test allows characterization of the type of RTA. Urine to blood CO2 gradient In alkaline urine, such as after a load of sodium bicarbonate, urine PCO 2 increases because of distal H+ secretion and is considered a sensitive indicator of distal acidification. The secreted H+ in the distal tubule reacts with luminal HCO 3 - to form carbonic acid, which dehydrates slowly in the medullary collecting duct to form CO2 that is trapped in the renal tubule. If urine pH is >7.5 and plasma HCO3- concentration >23-25 mEq/L, the urine PCO2 should exceed 70 mm Hg and the urineto-blood PCO2 gradient should be greater than 20 mm Hg in normal individuals. Patients with decreased rates of tubular H + secretion (classical type 1 RTA) show subnormal values, with urine PCO 2 less than 50 mm Hg and U-B PCO2 <10 mm Hg. Those with backleak distal RTA retain the ability to generate high urinary PCO2, because the proton pump function is normal and the H+ gradient does not favor back-diffusion during alkaline diuresis. Normal results are also observed in hypoaldosteronism associated RTA and reversible voltage-dependent defects. Urine PCO2 also augments markedly after neutral phosphate administration, providing that urine pH is close to the pK of the phosphate buffer system (i.e., 6.8).
Indian Journal of Pediatrics, Volume 74July, 2007
With a urine phosphate concentration above 20 mmol/L, normal subjects should achieve a urine-to-blood PCO 2 gradient above 40 mmHg. Fractional excretion of bicarbonate (FEHCO3) This is an important index of proximal tubular handling of HCO 3 . The FEHCO 3 is calculated after adequate alkalization. The proximal tubule normally reabsorbs almost all filtered bicarbonate (fractional excretion <5%).
urine bicarbonate plasma creatinine
FEHCO3 (%) = 100
plasma bicarbonate urine creatinine
When the serum bicarbonate is normal (>22 mEq/l), a value >15% indicates proximal RTA. Levels are in the normal range (<5%) in classic distal RTA although HCO3absorption is incomplete at low levels of plasma HCO 3-, its absorption increases with increasing levels. In hyperkalemic distal RTA, the FEHCO3 varies from 5-10%. Despite normal proximal HCO3- reabsorption, variable degrees of fixed bicarbonaturia may occur in type 1 RTA due to the high urine pH, because the urine HCO3- varies with the urine pH as per the Henderson Hasselbach equation. log HCO3Urine pH = pKa + 0.03 pCO2 Thus, even in type 1 RTA with urine pH <6, the FEHCO3 is 3%, while at urine pH >7 it may exceed 5-10%. This is referred to as type 3 RTA; it does not indicate the co-presence of a proximal defect in HCO3- reabsorption, unlike previously proposed. Step 5. Additional Investigations Tests for phosphate handling The plasma phosphate level indicates proximal tubular function. The fractional excretion of phosphate determined on a timed (6-hr, 12-hr, 24-hr) urine specimen, is useful for detecting phosphate wasting, which provides supportive evidence for presence of proximal RTA, as in Fanconi syndrome. Normally 5-12% of the ultrafiltered phosphate is excreted and the tubular reabsorption is 88-95%.
Fractional excretion = of phosphate urine phosphate plasma creatinine 100 plasma phosphate urine creatinine
Tubular reabsorption = 100 - fractional excretion The tubular reabsorption of phosphate depends on plasma phosphate and GFR and is not the optimal indicator of tubular phosphate handling, especially in patients with hypophosphatemia. This has led to increasing use of the index, tubular maximum for phosphate, corrected for GFR (TmP/GFR), a factor independent of plasma phosphate and renal functions for assessment of phosphate handling. TmP/GFR, or Bijvoet index,
683
88
A. Bagga and A. Sinha represents the concentration above which most phosphate is excreted and below which most is reabsorbed. 9 It can be calculated from the plasma phosphate and TRP (on timed urine samples) using Bijvoet nomogram (Fig. 5) or directly:
0. 00
0.0 0.0 2.0 1.8 1.6 4.0 0.6 2.0 0.8 1.0 3.0 1.2 1.4 1.0 1.6 1.8 2.0 1.4 5.0
1.0
Actual plasma phosphate concentration (mg/dL)
0.4
Renal threshold phosphate concentration (TmP/GFR)
0.2
Briefly, secretion of K + in the cortical and outer medullary collecting ducts accounts for the majority of its excretion in the urine that is influenced by aldosterone, plasma K+ concentration and anion composition of the luminal fluid. Negligible amounts of K + are secreted or reabsorbed distal to these sites. The final urinary K+ concentration then depends on water reabsorption in the medullary collecting ducts, which results in a rise in the final urinary K+ concentration. TTKG is determined as follows: TTKG = urine K+ x plasma osmolality plasma K+ x urine osmolality
0. 00
0. 01 0. 05 0. 0. 10 99 0 0. 0. .20 95 0. 30 0. 90 0. 40 0 50 0. .80 0. 70 60 0. 0. 0. 60 70 50 0. 0. 80 40 0. 30 0. 90 0. 20 0. 10 0. 00
1.2
3.0
1.0 0.8
2.0
0.6
The ratio of urine to plasma osmolality allows for correction of the final urinary K+ concentration for the water reabsorbed in the medullary collecting duct. The TTKG is an index of the gradient of K + in the distal tubular lumen and interstitial blood capillaris, independent of urine flow rate. The urine must at least be iso-osmolal with respect to serum if the TTKG is to be meaningful. The TTKG in normal persons varies but is generally within the range of 6-12. Hypokalemia from extrarenal causes results in renal K+ conservation and a TTKG <2. A higher value suggests renal K + losses, as in hyperaldosteronism. During hyperkalemia, the expected TTKG is >10. An inappropriately low TTKG (< 8) in hyperkalemia suggests hypoaldosteronism or renal tubular resistance to aldosterone. Administration of the mineralocorticoid, fludrocortisone (0.05 mg) enables TTKG to rise to >7 in patients with hypoaldosteronism. When the TTKG does not increase after mineralocorticoid challenge, tubular resistance to aldosterone is suspected.10 Frusemide test Response to frusemide and sodium sulfate help determine the mechanism of defect in type 1 RTA (Table 1). Responses to frusemide or sodium sulfate help elucidate the possible site and mechanism of acidification defect in type 1 RTA. Both agents tend to increase the luminal electronegativity by increasing Na+ delivery to and reabsorption in the cortical collecting tubule. The changes that these agents induce in H+ and K+ excretion in normal subjects, and in those with various defects of distal RTA, are shown in Table 1. In healthy individuals
0.4
1.0
5.0
0.0
0.0
Fig. 5. Assessment of TmP/GFR involves estimation of plasma phosphate (left y-axis) and tubular reabsorption (TRP) (or fractional excretion, C p/Ccr ). The straight line joining these values is extended to obtain TmP/GFR (right y-axis). TmP/GFR (mg/dL) = plasma phosphate urine phosphate plasma creatinine urine creatinine
The normal value of TmP/GFR is 2.8-4.4 mg/dL, with lower values in older children. Transtubular potassium gradient (TTKG) While spot and 24-hr urinary excretion of K+ is useful for evaluating patients with hypokalemia, its role in evaluating subjects with hyperkalemia is limited. In patients with hyperkalemia and normal glomerular function, the TTKG provides an accurate estimate of aldosterone effect on late distal and cortical collecting tubules, as explained below.
TABLE 1. Response of Urine pH and Potassium (K+) Excretion Following Frusemide Administration in Normal Subjects and Various Defects Causing Distal RTA. Defect Site of defect Urine pH During acidosis After frusemide <5.5 >5.5 >5.5 >5.5 Further decline >5.5 <5.5 >5.5 K+ excretion Baseline After frusemide Normal Normal Normal Decreased Increased Increased Increased Unchanged
Normal H+ ATPase defect H+ ATPase defect Voltage defect CT collecting tubule
None Diffuse, cortical CT Medullary CT alone Cortical CT
684
1. 00
Indian Journal of Pediatrics, Volume 74July, 2007
89
Evaluation of Renal Tubular Acidosis administration of either of these agents results in decrease in urine pH to <5.5 and increased K+ excretion. In patients with hypokalemic distal RTA, due to defect in the H+ ATPase, the urine pH does not fall but the urine K+ excretion increases, in response to frusemide since the function of principal cells is intact. Patients with H + ATPase pump defect limited to the medulla show a relatively normal increase in both H + and K+ secretion because cortical tubule function is stimulated appropriately by a rise in luminal electronegativity. Patients with primary defect in cortical Na+ reabsorption (voltage defect) have baseline hyperkalemia and no posttherapy increase in H + or K + excretion, since luminal electronegativity is not enhanced. A normal response is observed in patients with type 4 RTA, hypoaldosteronism (where voltage sensitive activity is retained), reversible voltage dependent defects (as with lithium-induced RTA) and proximal RTA.6 The sodium sulfate test is limited to research settings. The frusemide test is practical and can be done using the agent at a single oral dose of 2 mg/Kg body weight, after collecting baseline sample of urine. Hourly urine samples are collected and urine pH and K + concentration determined. Some protocols involve the administration of an oral dose of fludrocortisone (1 mg) the evening prior to testing.2 Table 2 summarizes the results of invertigations in different forms of RTA. Proximal RTA The diagnosis of proximal RTA calls for study of other proximal tubular functions. Assessment of phosphate excretion has been discussed above. Evaluation for aminoaciduria, glucosuria and rickets is important. Disorders that are associated with proximal RTA and Fanconi syndrome should be specifically screened for, including cystinosis, Lowes syndrome, galactosemia and Wilsons disease.1 Distal RTA When a diagnosis of distal RTA is made the diagnostic work-up should always include ultrasonography for nephrocalcinosis and renal calculi, and measurement of urinary calcium and citrate excretion. Hypercalciuria and hyperphosphaturia occur due to the release of calcium phosphate from bone in order to buffer excess H + during acidosis, and the direct effects of acidosis on tubular reabsorption of these ions. Hypocitraturia results from increased citrate utilization in proximal tubule cells due to intracellular acidosis, resulting in an increased gradient for tubular reabsorption, and due to the high luminal pH favoring conversion of citrate3- to the readily reabsorbable citrate2-. Hypercalciuria, hypocitraturia and high urine pH contribute to occurrence of calcium phosphate renal stones. Hypercalciuria is suspected when the value of urinary calcium to creatinine ratio is above the age related norm, and diagnosed in the presence of 24-hr calcium excretion exceeding 4 mg/Kg/day. Hypocitraturia is said to be present when the 24 hr urinary citrate is below 2 mg/Kg/day.9 All patients with idiopathic distal RTA should undergo a formal hearing evaluation, in view of the association of sensorineural deafness with recessively inherited disease; deafness may not be present in infancy and develop later. Since type 1 RTA in older children may be associated with systemic lupus erythematosus, Sjogren syndrome or chronic hepatitis, appropriate evaluation for these entities should be undertaken. A subtype of type 1 RTA, caused by deficiency of carbonic anhydrase type II isoenzyme, is associated with osteopetrosis.2 Type 4 RTA In children, aldosterone unresponsiveness is a more common cause of type IV RTA than aldosterone deficiency, and is commonly associated with obstructive uropathy. Diagnostic work-up should thus include investigations for an underlying nephropathy, including ultrasound to identify structural abnormalities and renal function tests for parenchymal dysfunction. TTKG is useful in diagnosing type 4 RTA, and when done before and after a mineralocorticoid challenge helps distinguish between deficiency and resistance to aldosterone. Plasma renin activity and aldosterone levels are necessary.
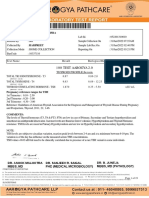
Distal RTA Classic Plasma K+ Urine pH Urine anion gap Urine NH 4+ Fractional HCO3- excretion U-B PCO 2 mm Hg Urine Ca 2+ Other tubular defects Nephrocalcinosis Bone disease Normal/low < 5.5 Positive Low >10-15% >20 Normal Often present Absent Common Normal/low > 5.5 Positive Low <5% < 20 High Absent Present Often present Hyperkalemic High > 5.5 Positive Low <5% </>20 High Absent Present Uncommon High < 5.5 Positive Low 5-10% >20 Normal/low Absent Absent Absent Type 4 RTA
TABLE 2. Investigations to Differentiate Types of Renal Tubular Acidosis (RTA) Proximal RTA
U-B PCO 2 urine to blood PCO2 gradient.
Indian Journal of Pediatrics, Volume 74July, 2007
685
90
A. Bagga and A. Sinha
Hyperchloremic (normal anion gap) Metabolic Acidosis
Urine anion gap
Negative
Positive
Gastrointestinal losses Acid intake
Suspect RTA
Urine pH Serum K+ Sodium bicarbonate loading
Urine pH <5.5 Serum K+ low normal UB CO2 >20 mm Hg FEHCO3 >10-15% Proximal RTA
Urine pH >5.5 Serum K+ low/normal UB CO2 <20 mm Hg FEHCO3 < 5% Classic type 1 RTA (Secretory defect)
Urine pH >5.5 Serum K+ high/normal UB CO2 </>20 mm Hg FEHCO3 <5%
Urine pH <5.5 Serum K+ high/ normal UB CO2 >20 mm Hg FEHCO3 5-10 % Type 4 RTA
Hyperkalemic type 1 RTA (Voltage defect)
Screen for other proximal tubular defects
Screen for hypercalciuria & nephrocalcinosis
Screen for renal parenchymal disease Plasma renin & aldosterone
Fig. 6. Evaluation of a patient with renal tubular acidosis. GI: gastrointestinal, U-B CO2: urine to blood PCO2 gradient, FEHCO3 fractional excretion of HCO3-
Genetic studies Recently, mutations have been identified in the genes encoding a number of transporters involved in pathogenesis of RTA and PHA types 1 and 2. 2,11,12 Identification of these mutations provides insights into the pathogenesis of RTA, but are currently available only as research tools. The evaluation of patients with RTA requires understanding of basic concepts and a methodological approach, as outlined in Fig. 6. REFERENCES
1. Dell KM, Avner ED. Renal tubular acidosis. In Behrman RE, Kliegman RM, Jenson HB, ed. Nelson Textbook of Pediatrics. Philadelphia; WB Saunders, 2003; 1758-1762. 2. Soriano JR. Renal tubular acidosis, the clinical entity. J Am Soc Nephrol 2002; 13: 2160-2170. 3. Bagga A, Bajpai A, Menon S. Approach to renal tubular disorders. Indian J Pediatr 2005; 72: 771-776. 4. Sayer JA, Pearce SHS. Diagnosis and clinical biochemistry of
inherited tubulopathies. Ann Clin Biochem 2001; 38: 459-470. 5. Unwin RJ. The renal tubular acidosis. J Royal Soc Med 2001; 94: 221-225. 6. Rose BD, Post TW. Metabolic acidosis. In Rose BD, Post TW, ed. Clinical Physiology of Acid Base and Electrolyte Disorders. Boston; Mc Graw Hills, 2001; 578-646. 7. Palmer BF, Alpern RJ. Normal acid-base balance and metabolic acidosis. In Johnson RJ, Feehally J, eds. Comprehensive Clinical Nephrology. London; Harcourt Publishers, 2000; 12.1-12.13. 8. Goldstein MB, Bear R, Richardson RMA, Marsden PA, Halperin ML. The urine anion gap: a clinically useful index of ammonium excretion. Am J Med Sci 1986; 292: 198-199. 9. Drueke TB, Lacour B. Disorders of calcium, phosphate and magnesium metabolism. In Johnson RJ, Feehally J, eds. Comprehensive Clinical Nephrology. London; Harcourt Publishers, 2000; 11.1-11.16. 10. DuBose TD Jr. Hyperkalemic hyperchloremic metabolic acidosis: pathophysiologic insights. Kidney Int 1997; 51: 591602. 11. Igarashi T, Sekine T, Inatomi J, Seki G. Unraveling the molecular pathogenesis of isolated proximal renal tubular acidosis. J Am Soc Nephrol 2002; 13 : 2171-2177. 12. Karet FE. Inherited distal renal tubular acidosis. J Am Soc Nephrol 2002; 13: 2178-2184.
686
Indian Journal of Pediatrics, Volume 74July, 2007
Potrebbero piacerti anche
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Multiple MyelomaDocumento10 pagineMultiple MyelomaFadina RizkiNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Interpretation of The eGFR Jul 07Documento8 pagineInterpretation of The eGFR Jul 07Danielcc LeeNessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Arcipe Iccu Case 5Documento98 pagineArcipe Iccu Case 5Maria Charis Anne Indanan100% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- HWProblemsDocumento21 pagineHWProblemsJonny Paul DiTroiaNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Mayo Clinic Laboratories Critical Values / Critical Results ListDocumento4 pagineMayo Clinic Laboratories Critical Values / Critical Results ListCarl DonaireNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Mydhili Recent Blood Test Reports 22.11.2021 PDFDocumento13 pagineMydhili Recent Blood Test Reports 22.11.2021 PDFHOD (MVGR Civil)Nessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Laboratory and Diagnostic TestDocumento3 pagineLaboratory and Diagnostic TestKristine Artes AguilarNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Acute On Chronic Liver Failure: Ulva Yogia GuslafDocumento19 pagineAcute On Chronic Liver Failure: Ulva Yogia GuslafSyahrul AdzimNessuna valutazione finora
- Exit FOR University Students 18/ /2011: WolloDocumento9 pagineExit FOR University Students 18/ /2011: WolloFikir AtalayNessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Neonatal Acute Kidney InjuryDocumento58 pagineNeonatal Acute Kidney InjuryRadhika BatraNessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Analyte Stability & Freeze-Thaw Information-1Documento8 pagineAnalyte Stability & Freeze-Thaw Information-1Yusuf Indra SentosaNessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Evaluation of Roselle (Hibiscus - Agbabiaka L. A., G.A. Nkwocha.Documento8 pagineEvaluation of Roselle (Hibiscus - Agbabiaka L. A., G.A. Nkwocha.dcollot8026Nessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Pathogenesis of Renal Failure in Multiple Myeloma: Any Role of Contrast Media?Documento10 paginePathogenesis of Renal Failure in Multiple Myeloma: Any Role of Contrast Media?Link BuiNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Reproductive Performance and Blood Constituents of Damascus Goats As Affected by YeastDocumento18 pagineReproductive Performance and Blood Constituents of Damascus Goats As Affected by YeastRaj CellaNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Boyd 2015Documento8 pagineBoyd 2015Fede0Nessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- MSDS Reaksi JaffeDocumento2 pagineMSDS Reaksi JaffeRossa A.G.PNessuna valutazione finora
- 100 Test Aarogya 2.0:: Mrs - Gunjan MisraDocumento19 pagine100 Test Aarogya 2.0:: Mrs - Gunjan Misramomo misraNessuna valutazione finora
- Creatinine (Alkaline Picrate) PDFDocumento1 paginaCreatinine (Alkaline Picrate) PDFatul pandey100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Iris A4 PosterDocumento2 pagineIris A4 PosterAndrea Gil Flaño0% (1)
- Chronic Kidney DiseaseDocumento283 pagineChronic Kidney DiseaseloisebadNessuna valutazione finora
- Ravel - Clinical Laboratory MedicineDocumento1.151 pagineRavel - Clinical Laboratory MedicineWiLaGatchaLianNessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Case Study ClinicalDocumento15 pagineCase Study ClinicalJane FlorendoNessuna valutazione finora
- Fenofibrate-Associated Nephrotoxicity: A Review of Current EvidenceDocumento8 pagineFenofibrate-Associated Nephrotoxicity: A Review of Current EvidencefevianaNessuna valutazione finora
- CKDCKD 37Documento60 pagineCKDCKD 37Jar JarNessuna valutazione finora
- Kidney Functions in Wister Rats Treated WTH Artesunate and AmodiaquineDocumento5 pagineKidney Functions in Wister Rats Treated WTH Artesunate and Amodiaquinesandeep raiNessuna valutazione finora
- Indapamide: M. Chajjman, R.C. Heel, R.N. Brogden, T.M. SpeightDocumento47 pagineIndapamide: M. Chajjman, R.C. Heel, R.N. Brogden, T.M. SpeightFitria SalsabilaNessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Urinalysis Specific GravityDocumento7 pagineUrinalysis Specific GravityOchima Walichi PrameswariNessuna valutazione finora
- Full ReportDocumento22 pagineFull ReportSadhu DasNessuna valutazione finora
- Effect of Storage Time and Temperature On Some Serum Analytes8.21 PDFDocumento4 pagineEffect of Storage Time and Temperature On Some Serum Analytes8.21 PDFyunitaNessuna valutazione finora
- Management of Proteinuria in Dogs and CaDocumento35 pagineManagement of Proteinuria in Dogs and Cajuan carlos white yepezNessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)