Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Risk For Infection
Caricato da
Herrick MateoDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Risk For Infection
Caricato da
Herrick MateoCopyright:
Formati disponibili
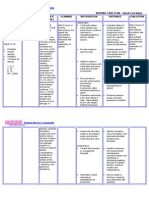
Need: Alteration in Safety
Diagnosis
Risk for infection R/T presence of favorable conditions for infections. 28 year old female Grav. 2, Para 2 4 degree laceration/episi otomy VBAC 6/19/02 Baby wt. 7lb 10oz Breast and bottle feeding Light lochiarubra Forceps attempted x2 WBC 12000 Vital Signs: T-99 BP-122/84 R-20
Goal & Goal Criteria
Patient will show no evidence of infection in 3-5 hours AEB:
Nursing Actions
Nursing student, from 1200-1700at Riverview Hospital will do the following: 1) Assess VS q4h (R,P,BP,T) R-increase in respirations and pulse indicate increased release of epinephrine and norepinephrine as a result of pain associated with inflammation and infection (Holman, lecture-Fall 2001) 2) Assess lab findings regarding Post Partum WBC. Ra total number of WBC exceeding 9000-30000 indicates an acute infection (Hols 532) 3) Monitor laceration/episiotomy for signs of infection such as increased redness, edema, pain, or a change to prurlent, foul smelling lochia. R-The body's cellular response to infection is inflammation-a protective vascular reaction that delivers fluid, blood products and nutrients to interstitial spaces in an area of injury (Potter-Perry 840) R-accumulation of fluid and dead tissue cells and WBC's forms an exudates at the site of inflammation (potter-perry 840)
Implementation
Evaluation
Over all goal was met 1. S within normal limits V
1) Normal VS P- 70-90 T- 97-99 R- 17-22 BP- 120/80-130/85 2) Episiotomy/laceration site will be without increased redness, tenderness, edema, drainage or foul odor. 3) Pt. Will not experience difficulty or increased discomfort related to urination. 4) Pt will demonstrate methods she will use to prevent infection. 5) WBC will be within normal Post Partum range
Assessed vital signs q4h
P--87 T--99 R-20 BP-120/82 2. l aceration/episiotomy site without increased redness, tenderness, edema, drainage or foul odor. 3. t able to urinate with no difficulty/discomfort. Stimulation not needed. p
2.
monitored laceration/episiotomy for signs of infection such as increased redness, edema, pain and change to purulent, foul smelling lochia. determined character of urine and whether pt experiences frequency, urgency or pain with urination.
3.
4. t demonstrated understanding of preventative hygiene practices / methods by return demonstration. 5. BC 12000
HR/P-87 Nipples without abrasion or lacerations States pain is a "3" on a 1-10 scale. States "everything is fine" States "I'm a little tired"
R-foul odor of lochia suggests endometrial infection. (murray 794) 4) Determine character of urine and whether pt experiences frequency, urgency or pain with urination. R-frequency, urgency or painful urination may indicate UTI (Murray 794) 5) Assess nutritional status R-pts with poor nutritional status may be anergic or unable to muster a cellular immune response to pathogens, and are therefore, more succeptible to infections (Nursing Diagnosis and Intervention 129) 6) Wash hands before and after pt contact R-The most important and most basic technique in preventing and controlling transmission of infections is hand-washing. (Potter-Perry 852) 7) Encourage intake of proteinrich foods such as poultry, meats, fish, legumes, soy products, peanut butter and yogurt. R-maintains optimal nutritional status, better enabling the body's natural defenses to fight invading organisms.(Nursing Diagnosis and 7. 4. assessed nutritional status and established that 95% of meals have been consumed.
5.
washed hands before and after pt. contact
6.
encouraged and explined the kinds of foods she should eat more of. (poultry, meat, fish, legumes, soy products, peanut butter, and yogurt) and explained the reasoning behind it. initiated measures to prevent UTI by:
*providing and encouraging fluid intake *monitoring for bladder distention
Intervention 130) 8) Initiate measures to reduce the risk of UTI provide and encourage increase in fluid intake monitor bladder distention to prevent overfilling use methods to promote bladder emptying (ie-running water in shower or sink and running warm water over perineum) R- adequate hydration and frequent voiding help prevent stasis of urine, which increases risk of UTI (Murray) 9) Instruct pt in hygienic practices to prevent infection: *Careful handwashing before and after perineal care. R-Hand washing is the most important defense against infection and its spread (Murray 794) *Perineal cleansing after elimination R-Perineal cleansing helps prevent growth of bacteria (Murray 794) *Change peripads frequently R-Frequent pad changes remove accumulated lochia, an excellent *stimulating urination when needed. 8. Instructed pt in hygiene practices to prevent infection.
culture medium for bacteria. (Murray 794) *Wipe perineum from front to back R-wiping from front to back prevents fecal contamination of the vagina (Murray 794)
REFERENCES: Gulanik, Klopp, Falanes, Gradishar and Puzas (1998) Nursing Diagnosis and Interventions (4th Edition) St. Louis, MO: Mosby, Inc. Potter and Perry (2001) Fundamentals of Nursing (5th Edition) St. Louis, MO: Mosby, Inc. Murray(2002) Foundations of Maternal-Newborn Nursing (3rd Edition) Philadelphia, PA: WB Saunders Company Shier (1999) Hole's Human Anatomy and Physiology (8th Edition) WCB/McGraw-Hill
NURSING CARE PLAN ANITA CLAPP
Wednesday June 19, 2002 INSTRUCTOR: P. Hart
Potrebbero piacerti anche
- Using The Glasgow Coma Scale For Patient AssessmentDocumento7 pagineUsing The Glasgow Coma Scale For Patient AssessmentJasmin Dela TorreNessuna valutazione finora
- Total Joint ReplacementDocumento10 pagineTotal Joint Replacementapi-3764215Nessuna valutazione finora
- Evidence-Based Nursing: I. Clinical QuestionDocumento4 pagineEvidence-Based Nursing: I. Clinical QuestionRay Jorge MarmetoNessuna valutazione finora
- CP - SoapieDocumento2 pagineCP - SoapieNikki GalveNessuna valutazione finora
- Fitrawati Arifuddin - Nursing Care Plan Deficiency of Fluid VolumeDocumento12 pagineFitrawati Arifuddin - Nursing Care Plan Deficiency of Fluid VolumefitrawatiarifuddinNessuna valutazione finora
- Delivery Room Performance Evaluation Tool: College of NursingDocumento2 pagineDelivery Room Performance Evaluation Tool: College of NursingIllya AnnesyNessuna valutazione finora
- BPH Case HistoryDocumento4 pagineBPH Case HistoryChino Dela CruzNessuna valutazione finora
- Otosclerosis Case StudyDocumento3 pagineOtosclerosis Case StudySana Anwar0% (2)
- Deficient Knowledge Related To Urinary Tract Infection: "Di Ako Aware About Sa UTI"as Verbalized by The ClientDocumento2 pagineDeficient Knowledge Related To Urinary Tract Infection: "Di Ako Aware About Sa UTI"as Verbalized by The ClientSeanmarie CabralesNessuna valutazione finora
- Intussusception: PathophysiologyDocumento8 pagineIntussusception: PathophysiologyNaufal AndaluNessuna valutazione finora
- Ladybelle P. Gototos Geriatric Nursing Bsn3 Set1 NCPDocumento2 pagineLadybelle P. Gototos Geriatric Nursing Bsn3 Set1 NCPLadybelle GototosNessuna valutazione finora
- Spinal Cord InjuryDocumento3 pagineSpinal Cord InjuryDan Leo UnicoNessuna valutazione finora
- Case Study, Chapter 70, Management of Patients WithOncologic or Degenerative Neurologic DisordersDocumento1 paginaCase Study, Chapter 70, Management of Patients WithOncologic or Degenerative Neurologic Disordersclyde i am100% (1)
- Nursing Diagnosis Analysis Goal/Objectives Intervention Rationale EvaluationDocumento3 pagineNursing Diagnosis Analysis Goal/Objectives Intervention Rationale EvaluationLorraine Punla PanganNessuna valutazione finora
- Application Balanced Skeletal TractionDocumento6 pagineApplication Balanced Skeletal TractionLorenz ChristopherNessuna valutazione finora
- Nursing Care in MR.X With Urinary Retention: Disusun OlehDocumento4 pagineNursing Care in MR.X With Urinary Retention: Disusun OlehHafin WardanaNessuna valutazione finora
- Clinical PaperDocumento18 pagineClinical PaperlhhjklllNessuna valutazione finora
- NCPDocumento10 pagineNCPCristina L. JaysonNessuna valutazione finora
- NCP ProperDocumento9 pagineNCP Properstephanie eduarteNessuna valutazione finora
- Nursing Care PlanDocumento3 pagineNursing Care PlanMae Therese AlabotNessuna valutazione finora
- Ramos - Pathophysiology PCOSDocumento1 paginaRamos - Pathophysiology PCOSLouwella RamosNessuna valutazione finora
- Assessment Nsg. Diagnosis Sci. Explanation Planning Intervention Rationale EvaluationDocumento6 pagineAssessment Nsg. Diagnosis Sci. Explanation Planning Intervention Rationale EvaluationRoMarie AbainzaNessuna valutazione finora
- Burns ActvityDocumento5 pagineBurns ActvityJoshua TercenoNessuna valutazione finora
- SBAR ToolDocumento2 pagineSBAR Toolpragya_devkota0% (1)
- Ca CHN Copar ReviewDocumento23 pagineCa CHN Copar Reviewapril punzalanNessuna valutazione finora
- GBS Nursing MangementDocumento21 pagineGBS Nursing MangementJoseph Namita SunnyNessuna valutazione finora
- Impaired Physical MobilityDocumento2 pagineImpaired Physical Mobilitygianne121391Nessuna valutazione finora
- 51 100Documento18 pagine51 100Jaessa Feliciano100% (1)
- Leptospirosis: Causes, Incidence, and Risk FactorsDocumento6 pagineLeptospirosis: Causes, Incidence, and Risk FactorsJackii DoronilaNessuna valutazione finora
- Balanoyos Geli Ortiz Santos Hypertension Case StudyDocumento76 pagineBalanoyos Geli Ortiz Santos Hypertension Case StudyElyse Ann Reyes100% (1)
- Imbalnce Nutrition Less Than Body RequirementsDocumento3 pagineImbalnce Nutrition Less Than Body RequirementselheezaNessuna valutazione finora
- Impaired Gas Exchange NCPDocumento3 pagineImpaired Gas Exchange NCPRomel BaliliNessuna valutazione finora
- Subjective Data: Baseline Data of Client.: Reference: Nurse's Pocket Guide: Diagnoses, Interventions, and RationalesDocumento4 pagineSubjective Data: Baseline Data of Client.: Reference: Nurse's Pocket Guide: Diagnoses, Interventions, and RationalesJor GarciaNessuna valutazione finora
- NCP PainDocumento2 pagineNCP PainApril_Ivy_Raga_3835Nessuna valutazione finora
- Assessment and Management of Preoperative AnxietyDocumento6 pagineAssessment and Management of Preoperative AnxietyFiorel Loves EveryoneNessuna valutazione finora
- 10 1056@NEJMcpc1913468 PDFDocumento10 pagine10 1056@NEJMcpc1913468 PDFAbdelkader HociniNessuna valutazione finora
- Assignment 5 - Fernandez, Dexter IvanDocumento1 paginaAssignment 5 - Fernandez, Dexter IvanIvan FernandezNessuna valutazione finora
- Acute TonsillopharyngitisDocumento39 pagineAcute TonsillopharyngitisCin AtianzarNessuna valutazione finora
- NCP DisturbedDocumento2 pagineNCP DisturbedTrixie Anne GamotinNessuna valutazione finora
- Essential New Born Care ScriptDocumento3 pagineEssential New Born Care ScriptShiela Joy DuquezNessuna valutazione finora
- Nursing Care PlanDocumento1 paginaNursing Care Planapi-248135371Nessuna valutazione finora
- Nursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term OutcomesDocumento2 pagineNursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term OutcomesDeanne Carla DalilisNessuna valutazione finora
- Proper Excreta Disposal, Food Safety Sanitation-Video LecDocumento15 pagineProper Excreta Disposal, Food Safety Sanitation-Video LecEden LacsonNessuna valutazione finora
- NCP Hip FractureDocumento5 pagineNCP Hip FractureCherry Ann BalagotNessuna valutazione finora
- FNCP On Elevated Blood Pressure 2Documento4 pagineFNCP On Elevated Blood Pressure 2Aaron EspirituNessuna valutazione finora
- Nursingcribcom Nursing Care Plan Spinal Cord InjuryDocumento2 pagineNursingcribcom Nursing Care Plan Spinal Cord InjuryJanine Erika Julom Brillantes100% (1)
- Acute Head InjuryDocumento5 pagineAcute Head InjuryRitesh KumarNessuna valutazione finora
- BSN 1 H Case Application Nursing Care PlanDocumento3 pagineBSN 1 H Case Application Nursing Care PlanAntonio EscotoNessuna valutazione finora
- NCP Proper CholecystectomyDocumento2 pagineNCP Proper CholecystectomyGail Lian SantosNessuna valutazione finora
- Post Stroke PamphletDocumento2 paginePost Stroke PamphletRgn McklNessuna valutazione finora
- Tonsilitis & Allergic Rhinitis NCPDocumento11 pagineTonsilitis & Allergic Rhinitis NCPJorgia SalardaNessuna valutazione finora
- Acute TonsillopharyngitisDocumento17 pagineAcute TonsillopharyngitisRachel Haide NaravalNessuna valutazione finora
- Assessment of The Peripheral Vascular SystemDocumento11 pagineAssessment of The Peripheral Vascular SystempatzieNessuna valutazione finora
- Pa Tho Physiology of PneumoniaDocumento6 paginePa Tho Physiology of PneumoniaPaula YoungNessuna valutazione finora
- Rheumatic Heart DiseaseDocumento13 pagineRheumatic Heart Diseasedy15Nessuna valutazione finora
- Oxytocin (Pitocin) : Slide 1Documento16 pagineOxytocin (Pitocin) : Slide 1Kalesha JonesNessuna valutazione finora
- EthicsDocumento1 paginaEthicsNadineNessuna valutazione finora
- NCP Acute PainDocumento3 pagineNCP Acute PainSian Grace AsadaNessuna valutazione finora
- Urinary Tract Infection (UTI)Documento13 pagineUrinary Tract Infection (UTI)BaDjed Willing100% (1)
- Case Study: Patient With Appendicitis: Submitted By: Farzaneh Yeganeh Submitted To: Ms. Amara SabriDocumento19 pagineCase Study: Patient With Appendicitis: Submitted By: Farzaneh Yeganeh Submitted To: Ms. Amara Sabrifarzaneh yeganehNessuna valutazione finora
- Cardiac Rehabilitation ProtocolDocumento5 pagineCardiac Rehabilitation Protocolmarkhabm100% (1)
- Neck Pain and Lower Back Pain. Med Clin N Am. 2019.Documento14 pagineNeck Pain and Lower Back Pain. Med Clin N Am. 2019.Jose Fernando Diez100% (1)
- "Undifferentiated Schizophrenia": A Case Study OnDocumento81 pagine"Undifferentiated Schizophrenia": A Case Study OnHomework Ping100% (1)
- Efficacy and Adverse Events of Oral Isotretinoin For Acne: A Systematic ReviewDocumento10 pagineEfficacy and Adverse Events of Oral Isotretinoin For Acne: A Systematic ReviewFerryGoNessuna valutazione finora
- Graseby 3100 Syringe Pump - Service ManualDocumento89 pagineGraseby 3100 Syringe Pump - Service ManualRamanjaneya goud100% (1)
- Chapter 15 - Autonomic Nervous System Course OutlineDocumento9 pagineChapter 15 - Autonomic Nervous System Course OutlineleoNessuna valutazione finora
- 2018 - Vitamine D Treatment Guidelines in India - JClinSciResDocumento10 pagine2018 - Vitamine D Treatment Guidelines in India - JClinSciResnagashayana gNessuna valutazione finora
- Psychologist Exam With AnswersDocumento13 paginePsychologist Exam With AnswersdrashishnairNessuna valutazione finora
- Intrathecal Morphine Single DoseDocumento25 pagineIntrathecal Morphine Single DoseVerghese GeorgeNessuna valutazione finora
- Soccer Programme U19 Pre in SeasonDocumento38 pagineSoccer Programme U19 Pre in SeasonJeffrey Peeko100% (1)
- Egyptian Hospital Accreditation Program: Standards: Sixth Edition May 2005Documento71 pagineEgyptian Hospital Accreditation Program: Standards: Sixth Edition May 2005khayisamNessuna valutazione finora
- Aravind Eye Care-ShubhDocumento7 pagineAravind Eye Care-ShubhShubha Brota RahaNessuna valutazione finora
- Avascular Necrosis - Causes, Symptoms, Prevention & TreatmentDocumento26 pagineAvascular Necrosis - Causes, Symptoms, Prevention & TreatmentSatrio Bangun NegoroNessuna valutazione finora
- What Is Personal HygieneDocumento4 pagineWhat Is Personal HygieneAnonymous 0FWhoTu100% (1)
- Teratogenic ItyDocumento8 pagineTeratogenic ItyValentin IanaNessuna valutazione finora
- Nursing Care Plan & Drug Study Set #1: PneumoniaDocumento6 pagineNursing Care Plan & Drug Study Set #1: PneumoniaBakushidoNessuna valutazione finora
- 1 BarashDP - Paradigms Lost AbridgedDocumento7 pagine1 BarashDP - Paradigms Lost AbridgedFABIONessuna valutazione finora
- National Congress of Veterinary Medicine Students HISTORYDocumento3 pagineNational Congress of Veterinary Medicine Students HISTORYRoyd Joseph R. MosasoNessuna valutazione finora
- Imperforate Anus PDFDocumento2 pagineImperforate Anus PDFGlyneth FranciaNessuna valutazione finora
- 40 Sa Hindi - LBDocumento6 pagine40 Sa Hindi - LBIrshad mohammedNessuna valutazione finora
- Viagra Connect Checklist - 4 PDFDocumento2 pagineViagra Connect Checklist - 4 PDFClarenceNessuna valutazione finora
- Overview He Most As IsDocumento20 pagineOverview He Most As IsManushi ChauhanNessuna valutazione finora
- Acute Limb Ischemia: Clinical PracticeDocumento9 pagineAcute Limb Ischemia: Clinical PracticeIndah MaulidawatiNessuna valutazione finora
- Thorax and Lungs SGDocumento2 pagineThorax and Lungs SGDestinee Caple100% (1)
- Photocatalysis PDFDocumento8 paginePhotocatalysis PDFLiliana GhiorghitaNessuna valutazione finora
- Fluids and Electrolytes Study GuideDocumento13 pagineFluids and Electrolytes Study GuideElizabeth McKeeNessuna valutazione finora
- Post PartumDocumento22 paginePost PartumShaira Mae Yante RomeroNessuna valutazione finora
- Kosmetik BatalDocumento5 pagineKosmetik BatalNurul AtikNessuna valutazione finora
- TableDocumento6 pagineTablemanuNessuna valutazione finora
- High Power Electrosurgery Review Update 2005Documento33 pagineHigh Power Electrosurgery Review Update 2005Ana ObradovicNessuna valutazione finora