Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Antioxidants, Diabetes and Endothelial Dysfunction: Review
Caricato da
Mustafa Ali HassanDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Antioxidants, Diabetes and Endothelial Dysfunction: Review
Caricato da
Mustafa Ali HassanCopyright:
Formati disponibili
Cardiovascular Research 47 (2000) 457464 www.elsevier.com / locate / cardiores www.elsevier.
nl / locate / cardiores
Review
Antioxidants, diabetes and endothelial dysfunction
D.W. Laight*, M.J. Carrier, E.E. Anggard
The William Harvey Research Institute, St. Bartholomew s and the Royal London School of Medicine and Dentistry, Charterhouse Square, London EC1 6 BQ , UK Received 3 January 2000; accepted 8 February 2000
Abstract While a damaged endothelium is recognised to be a key accessory to diabetic macroangiopathy, awareness is developing that impairments concerning endothelium- and nitric oxide (NO)-dependent microvascular function, may contribute to several other corollaries of diabetes, such as hypertension, dyslipidaemia and in vivo insulin resistance. There are now several reports describing elevations in specic oxidant stress markers in both insulin resistance syndrome (IRS) and diabetes, together with determinations of reduced total antioxidant defence and depletions in individual antioxidants. Such a pro-oxidant environment in diabetes may disrupt endothelial function through the inactivation of NO, resulting in the attenuation of a fundamental anti-atherogenic and euglycaemic vascular inuence. Indeed, experimental and clinical data suggest that the supplementation of insulin resistant or diabetic states with antioxidants such as vitamin E, normalises oxidant stress and improves both endothelium-dependent vasodilation and insulin sensitivity. However, the promising potential efcacy of antioxidant therapy in cardiovascular disease and diabetes, in either a primary or secondary preventative role, awaits denitive clinical demonstration. 2000 Elsevier Science B.V. All rights reserved.
Keywords: Blood ow; Diabetes; Endothelial function; Free radicals; Nitric oxide
Downloaded from cardiovascres.oxfordjournals.org by guest on July 2, 2011
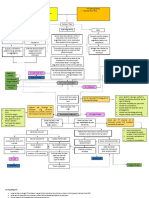
1. Introduction Insulin resistance syndrome (IRS) or metabolic syndrome X [1,2], is characterised by a group of metabolic and haemostatic abnormalities, most of which represent independent risk factors for the development of type II diabetes (see Fig. 1). These include impaired glucose tolerance, hyperinsulinaemia, hypertension, dyslipidaemia, a pro-thrombotic / hypo-brinolytic state, oxidant stress and endothelial dysfunction [13]. This cluster also generates an increased risk of macroangiopathy in both diabetes and the prediabetic state represented by IRS, resulting principally from atherosclerotic and thrombotic pathologies [4]. Such macroangiopathy is often present at the diagnosis of type II diabetes [5] and the associated coronary artery,
cerebrovascular and peripheral vascular disease are leading causes of diabetic morbidity and mortality. Given the central pathogenic role of the dysfunctional endothelium in the atherosclerosis of large and mediumsized arteries [6,7], it is increasingly clear that endothelial cells are the ultimate target of pro-atherogenic mediators in IRS and diabetes such as oxidant stress [79]. Furthermore, a more disseminated endothelial dysfunction possibly mediated by reactive oxygen species (ROS), for example in resistance and microvascular beds, may even underlie the parallel development of some of the principal facets of IRS such as hypertension, insulin resistance, dyslipidaemia and altered haemostasis [10]. This notion is lent credence by ndings that in common with atherosclerosis, endotheliopathy is an early abnormality and precedes the development of type II diabetes [11]. The pathological role of the endothelium as both a target and mediator of diabetic macroangiopathy, has been the
*Corresponding author. Tel.: 144-171-982-6037; fax: 144-171-9826016. E-mail address: d.w.laight@mds.qmw.ac.uk (D.W. Laight).
Time for primary review 25 days.
0008-6363 / 00 / $ see front matter 2000 Elsevier Science B.V. All rights reserved. PII: S0008-6363( 00 )00054-7
458
D.W. Laight et al. / Cardiovascular Research 47 (2000) 457 464
insulin resistance in the development of essential hypertension. However, the role of this phenomenon in the maintenance of hypertension is less clear since, while the endothelial NO pathway is thought to be defective in this condition [15,24], insulin may still be able to potentiate endothelium-dependent vasodilation by what appears to be a compensatory, hyperpolarising mechanism in established essential hypertension [15]. Of course, endothelium-derived endothelin-1 and angiotensin II, two powerful vasoconstrictor and pro-mitogenic agents, are also clearly implicated in the progression of endothelial dysfunction and hypertension in diabetes [2530].
3. Endothelial dysfunction and in vivo insulin resistance
3.1. Blood ow and insulin-mediated glucose disposal
Fig. 1. Hypothetical scheme linking oxidant stress, endothelial dysfunction and insulin resistance in the setting of type II diabetes.
subject of a recent review by us [12]. The present review examines how endothelial dysfunction associated with oxidant stress, may help generate a number of risk factors for diabetic macroangiopathy, including vascular and metabolic insulin resistance, before considering evidence of an altered antioxidant status in diabetes and the potential of antioxidant therapy.
2. Endothelial dysfunction, vascular insensitivity to insulin and hypertension
2.1. Vasodilator activity of insulin
Insulin per se elicits nitric oxide (NO)-dependent vasodilation in human skeletal muscle [13,14], possibly by enhancing agonist-stimulated endothelial vasodilator function [15,16]. This vasodilator action of insulin can be shown to be blunted in insulin resistant states such as obesity, hypertension and type II diabetes [1719]. Moreover, the recent report by Tack et al. [20] that impaired insulin-mediated endothelium-dependent vasodilation in obesity may be independent of frank endothelial vasodilator dysfunction, raises the fascinating possibility of a discrete vascular insensitivity to insulin or vascular insulin resistance at the level of the endothelium [21]. Such a defect in the putative tonic modulation of endothelial vasodilator function in resistance vessels by insulin, has already been suggested to contribute to hypertension in a genetic model of insulin resistance, the obese Zucker rat [22]. Studies in insulin resistant, hypertensive patients and spontaneously hypertensive rats by Lembo et al. [23] support a causative or permissive role of such vascular
Endothelial vasodilator dysfunction at the level of metabolically important arterioles such as those of skeletal muscle, may not only precede but also play a role in the development of IRS [10,31]. This is because a decit in endothelium-dependent vasodilation described in insulin resistant states including type II diabetes [19,3234], may impair the postprandial increase in blood ow in insulinsensitive tissues such as skeletal muscle, now considered to be a signicant determinant of glucose disposal, at least in insulin-sensitive individuals [17,3537]. This could explain the relationship between insulin sensitivity and NO-mediated, endothelial vasodilator function reported in normal subjects [3739], although such a link is not a universal nding [40]. Furthermore, as mentioned above, insulin is itself an endothelium-dependent vasodilator and this vascular effect in insulin-sensitive tissue is diminished in insulin resistant states [1719]. Indeed, impaired insulin-stimulated NO-mediated vasodilation in skeletal muscle has been accorded a major role in the pathogenesis of the in vivo insulin resistance associated with type I diabetes [41]. Furthermore, a defective insulin-mediated, endothelium-dependent regulation of blood ow in adipose tissue has itself been suggested to pose a signicant cardiovascular risk, since this may contribute to postprandial hyperlipidaemia [42].
Downloaded from cardiovascres.oxfordjournals.org by guest on July 2, 2011
3.2. Role of endothelial transcytosis of insulin
Another aspect of endothelial dysfunction to consider in insulin resistant individuals is the delay in the endothelial transport of insulin to the interstitial space [35,43] which, although probably insufcient to account for poor insulin action under steady-state conditions [44], may nonetheless impose a rate-limiting step in glucose disposal in response to rapidly changing blood-borne insulin levels [45].
D.W. Laight et al. / Cardiovascular Research 47 (2000) 457 464
459
3.3. Signicance of endothelial dysfunction to in vivo insulin resistance
Defects in both metabolically relevant endothelial vasoactive and transport function coupled with a reported reduction in skeletal muscle capillarisation in insulin resistant individuals [46], may all contribute to in vivo insulin resistance in man [47] and thus conceivably promote hyperglycaemia and hyperinsulinaemia and generate an enhanced cardiovascular risk. However, despite the identication of defects in endothelium-dependent vasodilation and the adverse implications for glycaemic control in insulin resistant states, reports in type II diabetic patients so far indicate that simply normalising skeletal muscle blood ow does not overcome established in vivo insulin resistance [39,48,49]. While this may not seem surprising in view of the fact that insulin resistance predominantly concerns a cellular defect in insulin-stimulated glucose uptake [50], it is important to distinguish between nutritive and non-nutritive microvascular ow in such studies; since only a rise in the former, which indeed may occur independently of a change in total blood ow, can be expected to enhance glucose and insulin delivery and therefore facilitate glucose disposal in insulin-sensitive tissue such as skeletal muscle [35].
vulnerability to an environmental pro-oxidative insult in established insulin resistance. Although the cellular source(s) of ROS is still unknown in such studies on the relationship between oxidant stress and insulin resistance, it is clear that endothelium-derived ROS potentially make a key contribution to poor insulin action at metabolically relevant sites (see above). Indeed, part of this contribution could concern a ROS-mediated reduction in trans-endothelial insulin transport [63]. Furthermore, the rapid inactivation of the endothelium-derived nitrovasodilator NO by vascular superoxide anion [6466], may account for the impaired endothelium-dependent vasodilation observed in type II diabetic patients [6769] and therefore contribute to a haemodynamic component of in vivo insulin resistance as well as more directly promoting atherogenesis [12]. It is interesting to note in this regard that our novel pro-oxidant model of type II diabetes in the obese Zucker rat [62], is also associated with evidence of a lesion in the NO signalling pathway in vivo (unpublished observation).
Downloaded from cardiovascres.oxfordjournals.org by guest on July 2, 2011
4.2. ROS and dyslipidaemia
In addition to the inactivation of NO, a ROS-mediated loss of glycosaminoglycan may lead to reductions in capillary endothelium-bound lipoprotein lipase action and thereby help to account for the prole of plasma hypertriglyceridaemia and reduced high density lipoprotein levels in IRS and type II diabetes [10]. Furthermore, in addition to encouraging platelet aggregation by limiting the release of prostacyclin from the endothelium, dyslipidaemia and in particular elevated levels of very low density lipoprotein, contributes to the generation of a pro-thrombotic environment via an increase in circulating levels of the anti-brinolytic factor plasminogen activator inhibitor 1, derived from the endothelium [3]. In addition, the ability of the endothelium to oxidatively modify low density lipoprotein particles [12], which are small and dense in diabetes and particularly vulnerable to oxidation [70,71], creates the environment for enhanced foam cell formation in diabetic atherogenesis [72].
4. Endothelium and oxidant stress
4.1. ROS and insulin action
Oxidant stress is associated with type II diabetes [51,52]and has recently been identied in our laboratory in the insulin resistant, obese Zucker rat [53]. While the origin(s) of this oxidant stress remains to be fully dened, it is clear that the generation of ROS including superoxide anion may be elevated in type II diabetes and even during impaired glucose tolerance [54], due in part to glucose auto-oxidation and non-enzymatic protein glycation [55]. ROS generation has also been associated with the interaction of advanced glycation endproducts (AGE) with specic receptors (RAGE), present on endothelium [56]. In addition, hyperglycaemia has been demonstrated to generate superoxide anion via the stimulation of endothelial cyclo-oxygenase activity in vitro [57]. Other potential endothelial sources of ROS include the activity of NADPH oxidase and uncoupled NO synthase activity [58,59]. Oxidant stress contributes to insulin resistance in man [60] and we have made a similar observation in the obese Zucker rat, based on the ability of a lipophilic antioxidant, vitamin E, to improve insulin action in vivo while reducing elevated plasma levels of a lipid peroxidation marker [61]. Moreover, we have very recently shown that a pro-oxidant challenge in this insulin resistant animal in vivo, provokes a further deterioration in insulin action leading to a type II diabetic state [62]. This is the rst demonstration of such a
5. Antioxidants and diabetes
5.1. Antioxidants and endothelial function in diabetes
There is a great deal of evidence to support a role for ROS in the impaired endothelium-dependent vasodilation observed in a variety of vascular preparations isolated from experimental diabetic animals [7380]. This dysfunction is thought to principally involve the reduced bioavailability of NO resulting from its rapid inactivation by superoxide radical [64,65]. Such a disruptive inuence of ROS in diabetes is supported by the demonstration of a comparable endothelial dysfunction in vitamin E-deprived rats [81,82].
460
D.W. Laight et al. / Cardiovascular Research 47 (2000) 457 464
Similarly, defective endothelium-dependent vasodilation in type II diabetic subjects [3234,69] can be reversed by dietary ascorbic acid [67]. This is also the case in type I diabetics [83]. Interestingly, ascorbic acid has recently also been demonstrated to reduce blood pressure in hypertensives [84]. These benecial actions of ascorbic acid may feasibly result from an enhanced bioavailability of vascular NO but could also conceivably arise from a stimulation of endothelial NO synthesis [85]. A reduction in NO formation could conceivably arise in diabetes following hyperglycaemia-dependent pseudohypoxia, since this condition is associated with the depletion of NADPH and tetrahydrobiopterin, which act as co-factors for NO synthase activity [12,86,87]. Furthermore, another result of pseudohypoxia, diacylglycerol formation, may activate protein kinase C and lead to the stimulation of vascular oxidase systems [8688]. This, together with the production of superoxide anion by uncoupled NOS, may generate signicant sources of endothelial superoxide anion (see above). Reductions in vascular NO signalling mediated by ROS, may be accompanied in diabetes by a reduced synthesis of prostacyclin [88,89] coupled with an undiminished or even enhanced formation of vasoconstrictor agents, which is also a factor in restricted vasodilation [79,80]. In particular, hyperglycaemia leads to endothelium-derived prostaglandin G 2 and thromboxane A 2 formation [90] and in common with hyperinsulinaemia, stimulates endothelin-1 (ET-1) synthesis in endothelial cells [91]. Indeed, ET-1 and another potent vasoconstrictor and pro-mitogenic peptide, angiotensin II derived from the vascular renin angiotensin system [92,93], have been linked with the development of clinical diabetic macroangiopathy [25,94]. In this regard, the angiotensin-converting enzyme inhibitor ramipril, has very recently been demonstrated to signicantly reduce the risk of myocardial infarction, stroke and cardiovascular death in a major clinical trial involving diabetics [95]. In addition, these vasoconstrictor peptides may also play a local role in the aetiology of microangiopathy, especially in the kidney, by maintaining post-capillary resistance in the face of diabetic arteriolar vasodilation and so facilitating capillary hypertension [96]. Ironically, superoxide anion may help mediate this paradoxical arteriolar vasodilation and increase in microvascular blood ow, which is an early feature of diabetes attendant on hyperglycaemia, by enhancing the calcium signalling pathway involved in agonist-stimulated NO synthesis [97,98]. An enhanced endothelial uptake of L-arginine, the substrate for NO synthase, has also been implicated in an effect of hyperglycaemia to stimulate basal NO synthesis [88]. NO per se has important antioxidant activities in the vessel wall, including the direct scavenging of superoxide anion and the inhibition of lipid peroxidation [99101]. Indeed, the efciency of NO in its antioxidant role, may make basal endothelium-dependent, NO-mediated vasodi-
lator function especially vulnerable to inhibition during an oxidative insult. Conversely, the loss of basal endotheliumderived NO in this manner, may also serve to help preserve vasodilator responses to endothelial agonists and NO donors [102]. However, any lesion in the endogenous NO signalling pathway has major pathological implications for macroangiographic disease progression in diabetes, resulting from a dysregulation of vascular tone, proliferation, platelet aggregation, coagulation, brinolysis, leukocyte adhesion, vascular permeability and lipoprotein oxidation [12]. Many of these pro-atherogenic sequelae may be triggered by hyperglycaemia via the formation of AGE, which been shown to inactivate NO and generate endothelial intracellular oxidant stress [9,12,56].
5.2. Antioxidant status in diabetes
There are several lines of evidence to suggest that antioxidant defences may be lower in diabetes. These include reports of reduced plasma / serum total antioxidant status or free radical scavenging activity and increased plasma oxidisability in type II diabetics, together with demonstrations of reduced levels of specic antioxidants such as ascorbic acid and vitamin E [54,103109]. In addition, the activities of the antioxidant enzymes catalase, superoxide dismutase and glutathione peroxidase, have been described as reduced in diabetics [34,109,110]. A diminution in the endothelial synthesis of NO has also been suggested in type II diabetics [69], which apart from detracting from vascular antioxidant defence (see above), would of course compound any defect in the antiatherogenic signalling role of NO [12].
Downloaded from cardiovascres.oxfordjournals.org by guest on July 2, 2011
5.3. The potential of antioxidant therapy
Antioxidant therapy, achieved by supplementation with pharmaceutical preparations of antioxidant nutrients and / or non-nutrients [111113], may conceivably confer both cardiovascular and metabolic benets in diabetes. This notion is well grounded in the theory surrounding the role of oxidative stress in disease [114]. In addition, it is supported by evidence of reduced antioxidant defences in diabetes and also by experimental ndings that antioxidants improve endothelium-dependent vasodilation and insulin sensitivity (see above). Indeed, epidemiological data provide strong associations between the dietary intake of antioxidant nutrients and protection against cardiovascular disease [113,115117]. Furthermore, a recent report has suggested a role for low serum carotenoid status in the development of insulin resistance and diabetes [118]. However, despite some early indications from clinical trials that vitamin E could protect against coronary artery disease [116,117,119], including that associated with diabetes [120], more recent studies with vitamin E, vitamin C and beta-carotene supplements have failed to clearly demonstrate a retardation in cardiovascular disease progression [119,121]. The reasons for these disappointing
D.W. Laight et al. / Cardiovascular Research 47 (2000) 457 464
461
results are unclear; but may simply highlight the need to intervene at a suitable moment in disease progression in patients at specic risk, using the most appropriate balance of harmonised and correctly targeted antioxidants at an optimal dose and for an adequate duration [122]. A more comprehensive evaluation of the cardiovascular benets of a range of naturally occurring antioxidants, including vitamin E, vitamin C, beta-carotene and selenium as potential nutriceuticals, awaits the outcome of a number of ongoing clinical trials [119]. However, a preliminary report from one of these, the Heart Outcomes Prevention Evaluation (HOPE) study, indicates that vitamin E supplementation did not reduce the incidence of cardiovascular endpoints after 4.5 years of use [95].
6. Conclusions A multifaceted endothelial dysfunction, involving the generation of oxidant stress, is conceivably central to the
principal manifestations of IRS, including insulin resistance and associated macrovascular disease (see Fig. 2). Indeed, the parallel development of atherosclerotic, diabetic macroangiopathy and the metabolic corollaries of insulin resistance [10], can be considered as manifestations of endothelial dysfunction at distinct vascular sites. This would then account for the commonality of vascular endothelial dysfunction and relative resistance to insulinmediated glucose uptake in metabolic disorders such as type II diabetes and cardiovascular disease such as atherosclerosis, essential hypertension, congestive heart failure and cardiac syndrome X (microvascular angina) [123]. Furthermore, it is apparent that antioxidant intervention in both experimental and clinical diabetes, can reverse endothelial dysfunction which may itself be related to an insufcient antioxidant defence [34]. However, while antioxidants are proving essential tools in the investigation of oxidant stress-related diabetic pathologies and despite the obvious potential merit of a replacement style therapy, the safety and efcacy of antioxidant supplementation in any future treatment, remains to be established.
Downloaded from cardiovascres.oxfordjournals.org by guest on July 2, 2011
Fig. 2. Hypothesised central role for a multifaceted, disseminated endothelial dysfunction in the development of insulin resistance syndrome, macroangiopathy and type II diabetes.
462
D.W. Laight et al. / Cardiovascular Research 47 (2000) 457 464 circulating endothelin-1 levels in type 2 diabetic patients. Acta Diabetol 1995;32:263267. Sarman B, Toth M, Somogyi A. Role of endothelin-1 in diabetes mellitus. Diabetes Metab Rev 1998;14:171175. Velasquez MT, Bhathena SJ, Strifer JS et al. Role of angiotensinconverting enzyme inhibition in glucose metabolism and renal injury in diabetes. Metabolism 1998;47:711. Anderson S. Physiologic actions and molecular expression of the reninangiotensin system in the diabetic rat. Miner Electrolyte Metab 1998;24:406411. Giugliano D, Marfella R, Acampora R et al. Effects of perindopril and carvedilol on endothelium-dependent vascular functions in patients with diabetes and hypertension. Diabetes Care 1998;21:631636. ODriscoll G, Green D, Maiorana A et al. Improvement in endothelial function by angiotensin-converting enzyme inhibition in NIDDM. J Am Coll Cardiol 1999;33:15061511. Ganrot PO. Insulin resistance syndrome: possible key role of blood ow in resting muscle. Diabtologia 1993;36:876879. McVeigh GE, Brennan GM, Johnston GD et al. Impaired endothelium-dependent and independent vasodilation in patients with Type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia 1992;35:771776. Hogikyan RV, Halter JB, Galecki AT et al. Specic impairment of endothelium-dependent vasodilation in subjects with type II diabetes independent of obesity. J Clin Endocrinol Metab 1998;83:1946 1952. Mohan IK, Das UN. Oxidant stress, antioxidants and nitric oxide in non-insulin dependent diabetes mellitus. Med Sci Res 1997;25:55 57. Wiernsperger N. Vascular defects in the aetiology of peripheral insulin resistance in diabetes. A critical review of hypotheses and facts. Diabetes Metab Rev 1994;10:287307. Baron AD, Steinberg HO, Chaker H et al. Insulin-mediated skeletal muscle vasodilation contributes to both insulin sensitivity and responsiveness in lean humans. J Clin Invest 1995;96:779786. Baron AD. The coupling of glucose metabolism and perfusion in human skeletal muscle. The potential role of endothelium-derived nitric oxide. Diabetes 1996;45:S105S109. Petrie JR, Ueda S, Webb DJ et al. Endothelial nitric oxide production and insulin sensitivity. A physiological link with importance for pathogenesis of cardiovascular disease. Circulation 1996;93:13311333. Avogaro A, Piarulli F, Valerio A et al. Forearm nitric oxide balance, vascular relaxation and glucose metabolism in NIDDM patients. Diabetes 1997;46:10401046. Utriainen T, Makimattila S, Virkamaki A et al. Dissociation between insulin sensitivity of glucose uptake and endothelial function in normal subjects. Diabetologia 1996;39:14771482. Baron AD, Laakso M, Brechtel G et al. Mechanism of insulin resistance in IDDM: a major role for reduced skeletal muscle blood ow. J Clin Endocrinol Metab 1991;73:637643. Summers LKM, Samra JS, Frayn KN. Impaired postprandial tissue regulation of blood ow in insulin resistance: a determinant of cardiovascular risk? Atherosclerosis 1999;147:1115. Miles PDG, Li S, Hart M et al. Mechanism of insulin resistance in experimental hyperinsulinaemic dogs. J Clin Invest 1998;101:202 211. Castillo C, Bogardus C, Bergman R et al. Interstitial insulin concentrations determine glucose uptake rates but not insulin resistance in lean and obese men. J Clin Invest 1994;93:1016. Miles PDG, Levisetti M, Reichart D et al. Kinetics of insulin action in vivo: identication of rate limiting steps. Diabetes 1995;44:947 953. Lillioja S, Young AA, Culter CL et al. Skeletal muscle capillary density and ber type are possible determinants of in vivo insulin resistance in man. J Clin Invest 1987;80:415424.
References
[1] Reaven GM. Role of insulin resistance in human disease. Physiol Rev 1995;75:473486. [2] Chisholm DJ, Campbell LV, Kraegen EW. Pathogenesis of the insulin resistance syndrome (syndrome X). Clin Exp Pharmacol Physiol 1997;24:782784. [3] McCarty MF. Haemostatic concomitants of syndrome X. Med Hypotheses 1994;44:179193. [4] Stamler J, Vaccaro O, Neaton JD et al. The multiple risk factor intervention trial research group: diabetes, other risk factors and 12-year cardiovascular mortality for men screened in the multiple risk factor intervention trial. Diabetes Care 1993;16:434444. [5] Tooke JE, Shore AC, Cohen RA et al. Diabetic angiopathy: tracking down the culprits. J Diabetes Complications 1996;10:173181. [6] Vanhoutte PM. Endothelial dysfunction and atherosclerosis. Eur Heart J 1997;18:E19E29. [7] Ross R. The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature 1990;362:801809. [8] Hsueh WA, Quinones MJ, Creager MA. Endothelium in insulin resistance and diabetes. Diebetes Rev 1997;5:343352. [9] Stehouwer CDA, Lambert J, Donker AJM et al. Endothelial dysfunction and pathogenesis of diabetic angiopathy. Cardiovasc Res 1997;34:5568. [10] Pinkney JH, Coen DA, Stehouwer CDA et al. Endothelial dysfunction: cause of the insulin resistance syndrome. Diabetes 1997;16:S9S13. [11] Tooke JE, Goh KL. Endotheliopathy precedes type 2 diabetes. Diabetes Care 1998;21:20472048. [12] Laight DW, Carrier MJ, Anggard EE. Endothelial cell dysfunction and the pathogenesis of diabetic macroangiopathy. Diabetes Metab Res Rev 1999;15:274282. [13] Steinberg HO, Brechtel G, Johnson A et al. Insulin-mediated skeletal muscle vasodilation is nitric oxide dependent. J Clin Invest 1994;94:11721179. [14] Scherrer U, Randin D, Vollenweider P et al. Nitric oxide release accounts for insulins vascular effects in humans. J Clin Invest 1994;94:25112515. [15] Taddei S, Virdis A, Mattei P et al. Effect of insulin on acetylcholineinduced vasodilation in normotensive subjects and patients with essential hypertension. Circulation 1995;92:147152. [16] Laight DW, Kaw AV, Carrier MJ et al. Pharmacological modulation of endothelial function by insulin in the rat aorta. J Pharm Pharmacol 1998;50:11171120. [17] Laakso M, Edelam SV, Brechtel G et al. Impaired insulin-mediated skeletal muscle blood ow in patients with NIDDM. Diabetes 1992;41:10761083. [18] Steinberg HO, Chaker H, Leaming R et al. Obesity / insulin resistance is associated with endothelial dysfunction. J Clin Invest 1996;97:26012610. [19] Shoemaker JK, Bonen A. Vascular actions of insulin in health and disease. Can J App Physiol 1995;20:127154. [20] Tack CJ, Ong MK, Lutterman JA et al. Insulin-induced vasodilation and endothelial function in obesity / insulin resistance. Effects of troglitazone. Diabetologia 1998;41:569576. [21] Vischer UM. Insulin resistance and the regulation of vascular tone: is insulin a vasodilator? Eur J Endocrinol 1998;138:262263. [22] Walker AB, Dores J, Buckingham RE et al. Impaired insulin induced attenuation of noradrenaline-mediated vasoconstriction in insulin-resistant obese Zucker rats. Clin Sci 1997;93:235241. [23] Lembo G, Morella A, Lanni F et al. Vascular insulin resistance in hypertension. Nutr Metab Cardiovasc Dis 1997;7:124126. [24] Panza JA, Casino PR, Kilcoyne CM et al. Role of endotheliumderived nitric oxide in the abnormal endothelium-dependent vascular relaxation of patients with essential hypertension. Circulation 1993;87:14681474. [25] Perfetto F, Tarquini R, de Leonardis V et al. Angiopathy affects [26] [27]
[28]
[29]
[30]
[31] [32]
[33]
Downloaded from cardiovascres.oxfordjournals.org by guest on July 2, 2011
[34]
[35]
[36]
[37]
[38]
[39]
[40]
[41]
[42]
[43]
[44]
[45]
[46]
D.W. Laight et al. / Cardiovascular Research 47 (2000) 457 464 [47] Wascher TC. Endothelial transport processes and tissue metabolism: evidence for microvascular endothelial dysfunction in insulin-resistant diseases? Eur J Clin Invest 1997;27:831835. [48] Natali A. Skeletal muscle blood ow and insulin action. Nutr Metab Cardiovasc Dis 1997;7:105109. [49] Laine H, Yki-Jarvinen H, Kirvela O et al. Insulin resistance of glucose uptake in skeletal muscle cannot be ameliorated by enhancing endothelium-dependent blood ow in obesity. J Clin Invest 1998;101:11561162. [50] Bloomgarden ZT. Insulin resistance: current concepts. Clin Ther 1998;20:216231. [51] Wolff SP. Diabetes mellitus and free radicals. Br Med Bull 1993;49:642652. [52] Gopaul NK, Mallet AI, Betteridge DJ et al. Plasma 8-epi-PGF 2a levels are elevated in individuals with NIDDM. FEBS Lett 1995;368:225229. [53] Laight DW, Kengatharan KM, Gopaul NK et al. Investigation of oxidant stress and vasodepression to glyceryl trinitrate in the obese Zucker rat in vivo. Br J Pharmacol 1998;125:895901. [54] Ceriello A, Bortolotti N, Crescentini A et al. Antioxidant defences are reduced during the oral glucose tolerance test in normal and non-insulin-dependent diabetic subjects. Eur J Clin Invest 1998;28:329333. [55] Giugliano D, Paolisso G, Ceriello A. Oxidative stress and diabetic vascular complications. Diabetes Care 1996;19:257267. [56] Taniguchi NH, Asahi M, Takahashi M et al. Involvement of glycation and oxidative stress in diabetic macroangiopathy. Diabetes 1996;45:S81S83. [57] Tesfamariam B. Free radicals in diabetic endothelial cell dysfunction. Free Radic Biol Med 1993;16:383391. [58] Bult H. Nitric oxide and atherosclerosis: possible implications for therapy. Mol Med Today 1996;2:510518. [59] Pritchard KAJ, Groszek L, Smalley DM et al. Native low-density lipoprotein increases endothelial cell nitric oxide synthase generation of superoxide anion. Circ Res 1994;77:354357. [60] Paolisso G, DAmore A, Volpe C et al. Evidence for a relationship between oxidative stress and insulin action in NIDDM patients. Metabolism 1994;43:14261429. [61] Laight DW, Desai KM, Gopaul NK et al. F 2 -isoprostane evidence of oxidant stress in the insulin resistant obese Zucker rat: effects of vitamin E. Eur J Pharmacol 1999;377:8992. [62] Laight DW, Desai KM, Gopaul NK et al. Pro-oxidant challenge in vivo provokes the onset of NIDDM in the insulin resistant obese Zucker rat. Br J Pharmacol 1999;128:269271. [63] Bertelsen M, Andersson MB, Anggard EE et al. Role of reactive oxygen species on tans-endothelial insulin transport. Br J Pharmacol 1998;125:P120. [64] Gryglewski RJ, Palmer RM, Moncada S. Superoxide anion is involved in the breakdown of endothelium-derived relaxing factor. Nature 1986;329:454458. [65] Darley-Usmar V, White R. Disruption of vascular signalling by the reaction of nitric oxide with superoxide: implications for cardiovascular disease. Exp Physiol 1997;82:305316. [66] Laight DW, Kaw AV, Carrier MJ et al. Interaction between superoxide anion and nitric oxide in the regulation of vascular endothelial function. Br J Pharmacol 1998;124:238244. [67] Ting HH, Timimi FK, Boles KS et al. Vitamin C improves endothelium-dependent vasodilation in patients with non-insulindependent diabetes mellitus. J Clin Invest 1996;97:2228. [68] Levine GN, Frei B, Koulouris SN et al. Ascorbic acid reverses endothelial vasomotor dysfunction in patients with coronary artery disease. Circulation 1996;93:11071113. [69] Makimattila S, Liu M-L, Vakkilainen J et al. Impaired endotheliumdependent vasodilation in type 2 diabetes. Diabetes Care 1999;22:973981. [70] Anderson JW, Gowri MS, Turner J et al. Antioxidant supplementation effects on low density lipoprotein oxidation for indi-
463
[71] [72] [73]
[74]
[75]
[76]
[77]
[78]
[79]
[80] [81]
[82] [83]
[84] [85]
[86] [87]
[88]
[89]
[90]
[91]
[92]
[93]
[94]
viduals with type 2 diabetes mellitus. J Am Coll Nutr 1999;18:451 461. Verges BL. Dyslipidaemia in diabetes mellitus. Diabetes Metab 1999;25:3240. Witztum JL. The oxidation hypothesis of atherosclerosis. Lancet 1994;344:793795. Pieper GM, Gross GJ. Oxygen free radicals abolish endotheliumdependent relaxation in diabetic rat aorta. Am J Physiol 1988;255:H825H833. Langenstroer P, Peiper GM. Regulation of spontaneous EDRF release in diabetic rat aorta by oxygen free radicals. Am J Physiol 1992;263:H257H265. Diederich D, Skopec J, Diederich A et al. Endothelial dysfunction in mesenteric resistance arteries of diabetic rats: role of free radicals. Am J Physiol 1994;266:H1153H1161. Hattori Y, Kawasaki H, Abe K et al. Superoxide dismutase recovers altered endothelium-dependent relaxation in diabetic rat aorta. Am J Physiol 1991;261:H1086H1094. Keegan A, Walbank H, Cotter MA et al. Chronic vitamin E treatment prevents defective endothelium-dependent relaxation in diabetic rat aorta. Diabetologia 1995;38:14751478. Rosen P, Ballhausen T, Bloch W et al. Endothelial relaxation is disturbed by oxidative stress in the diabetic rat heart: inuence of tocopherol as antioxidant. Diabetologia 1995;38:11571168. Dai F-X, Diederich A, Skopec J et al. Diabetes-induced endothelial dysfunction in STZ-treated rats: role of prostaglandin endoperoxides and free radicals. J Am Soc Nephrol 1993;4:13271336. Tesfamariam B. Free radicals in diabetic endothelial cell dysfunction. Free Radic Biol Med 1993;16:383391. Ralevic V, Milla PJ, Burnstock G. Effects of chronic vitamin E deciency on vascular function a study of sympathetic nerves, smooth muscle and endothelium of the mesenteric arterial bed of the rat. Br J Pharmacol 1995;116:29832988. Davidge ST, Ojimba J, McLaughlin MK. Vascular function in the vitamin E-deprived rat. Hypertension 1998;31:830835. Timimi FK, Ting HH, Haley M et al. Vitamin C improves endothelium-dependent vasodilation in IDDM. J Am Coll Nephrol 1998;31:552557. Duffy SJ, Gokce N, Holbrook M et al. Treatment of hypertension with ascorbic acid. Lancet 1999;354:20482049. Heller R, Munscher-Paulig F, Grabner R et al. L-Ascorbic acid potentiates nitric oxide synthesis in endothelial cells. J Biol Chem 1999;274:82548260. Honing MJH, Morrison PJ, Banga JD et al. Nitric oxide availability in diabetes mellitus. Diabetes Metab Rev 1998;14:241249. Giugliano D, Paolisso G, Coppla L. Hyperglycaemia and endothelial dysfunction in human diabetes: does oxidative stress play a role? Nutr Metab Cardiovasc Dis 1997;7:100104. Sobrevia L, Mann GE. Dysfunction of the endothelial nitric oxide signalling pathway in diabetes and hyperglycaemia. Exp Phyisol 1997;82:423452. Ono H, Umeda F, Inoguchi T et al. Glucose inhibits prostacyclin production by cultured aortic endothelial cells. Thromb Haemost 1988;60:174177. Tesfamariam B, Brown ML, Deykin D et al. Elevated glucose promotes generation of endothelium-derived vasoconstrictor prostanoids in rabbit aorta. J Clin Invest 1990;85:929932. Yamaguchi T, Ohnaka K, Takayanagi R et al. Enhanced secretion of endothelin 1 by elevated glucose levels from cultured endothelial cells. FEBS Lett 1990;267:1618. Falkenhahn M, Gohlke P, Paul M et al. The reninangiotensin system in the heart and vascular wall: new therapeutic aspects. J Cardiovasc Pharmacol 1994;24:S6S13. Schalekamp MADH. Reninangiotensin system components and endothelial proteins as markers of diabetic microvascular disease. Clin Invest 1993;71:S3S6. Hsueh WA, Anderson PW. Systemic hypertension and the renin
Downloaded from cardiovascres.oxfordjournals.org by guest on July 2, 2011
464
D.W. Laight et al. / Cardiovascular Research 47 (2000) 457 464 [109] Ashour M, Salem S, Hassaneen H et al. Antioxidant status and IDDM. J Clin Biochem Nutr 1999;26:99107. [110] Tuzun S, Girgin FK, Sozmen EY et al. Antioxidant status in experimental type 2 diabetes mellitus: effects of glibenclamide and glipizide on various rat tissues. Exp Toxicol Pathol 1999;51:436 441. [111] Vendemiale G, Grattagliano I, Altomare E. An update on the role of free radicals an diabetes antioxidant defense in human disease. Int J Clin Lab Res 1999;29:4955. [112] Patel M, Day BJ. Metalloporphyrin class of therapeutic catalytic antioxidants. Trends Pharmacol Sci 1999;20:359364. [113] Nuttall SL, Kendall MJ, Martin U. Antioxidant therapy for the prevention of cardiovascular disease. Q J Med 1999;92:239244. [114] Maxwell SRJ. Prospects for the use of antioxidant therapies. Drugs 1995;49:345361. [115] Palace VP, Khaper N, Qin Q et al. Antioxidant potentials of vitamin A and carotenoids and their relevance to heart disease. Free Radic Biol Med 1999;26:746761. [116] Kendall MJ, Nuttall SL, Martin U. Antioxidant therapy a new therapeutic option for reducing mortality from coronary artery disease. J Clin Pharm Ther 1998;23:323325. [117] Gaziano JM. Antioxidant vitamins and cardiovascular disease. Proc Assoc Am Phys 1999;111:29. [118] Ford ES, Will JC, Bowman BA et al. Diabetes mellitus and serum carotenoids: ndings from the Third National Health and Nutrition Survey. Amount J Epidemiol 1999;149:168176. [119] Marchioli R. Antioxidant vitamins and prevention of cardiovascular disease: laboratory, epidemiological and clinical trial data. Pharmacol Res 1999;40:227238. [120] Jain SK, McVie R, Jaramillo JJ et al. The effect of modest vitamin E supplementation on lipid peroxidation products and other cardiovascular risk factors in diabetic patients. Lipids 1996;31:S87S90. [121] Maxwell SRJ. Antioxidant vitamin supplements. Drug Safety 1999;21:253266. [122] Bellomo G. Is it really time to perform large intervention trials with antioxidant vitamins to prevent cardiovascular disease? Pharmacol Res 1999;40:207208. [123] Stern MP. Do NIDDM and cardiovascular disease share common antecedents? Ann Intern Med 1996;124:110116.
angiotensin system in diabetic vascular complications. Am J Cardiol 1993;72:14H21H. [95] Kleinert S. HOPE for cardiovascular disease prevention with ACEinhibitor ramipril. Lancet 1999;354:841. [96] Jaap AJ, Tooke JE. Pathophysiology of microvascular disease in NIDDM. Clin Sci 1995;89:312. [97] Graier WF, Posch K, Wascher TC. Role of superoxide anions in changes of endothelial vasoactive response during acute hyperglycaemia. Horm Metab Res 1997;29:622626. [98] Graier WF, Simecek S, Hoebel BG et al. Antioxidants prevent high-D-glucose-enhanced endothelial Ca 21 / cGMP response by scavenging superoxide anions. Eur J Pharmacol 1997;322:113122. [99] Kanner J, Harel S, Granit R. Nitric oxide as an antioxidant. Arch Biochem Biophys 1991;289:130136. [100] Halliwell B. Oxidative stress, nutrition and health. Experimental strategies for optimization of nutritional antioxidant intake in humans. Free Radic Res 1996;25:5774. [101] Hogg N, Kalyanaraman B. Nitric oxide and lipid peroxidation. Biochim Biophys Acta 1999;1411:378384. [102] Laight DW, Kaw AV, Carrier MJ et al. Interaction between superoxide anion and nitric oxide in the regulation of vascular endothelial function. Br J Pharmacol 1998;124:238244. [103] Ceriello A, Bortolotti N, Falleti E et al. Total radical-trapping antioxidant parameter in NIDDM patients. Diabetes Care 1997;20:194197. [104] Ceriello A, Bortolotti N, Pirisi M et al. Total plasma antioxidant capacity predicts thrombosis-prone status in NIDDM patients. Diabetes Care 1997;20:15891593. [105] Aguirre F, Martin I, Grinspon D et al. Oxidative damage, plasma antioxidant capacity and glycaemic control in elderly patients. Free Radic Biol Med 1998;24:580585. [106] Haffner SM, Agil A, Mykkanen L et al. Plasma oxidisability in subjects with normal glucose tolerance, impaired glucose tolerance and NIDDM. Diabetes Care 1995;18:646653. [107] Maxwell SRJ, Thomason H, Sandler D et al. Poor glycaemic control is associated with reduced serum free radical scavenging (antioxidant) activity in NIDDM. Ann Clin Biochem 1997;34:638 644. [108] Paolisso G, DAmore A, Balbi V et al. Plasma vitamin C affects glucose homeostasis in healthy subjects and in NIDDM. Am J Physiol 1994;266:E261E268.
Downloaded from cardiovascres.oxfordjournals.org by guest on July 2, 2011
Potrebbero piacerti anche
- NIH Public Access: Author ManuscriptDocumento15 pagineNIH Public Access: Author ManuscriptIrma KurniawatiNessuna valutazione finora
- B51 FullDocumento7 pagineB51 FullAna LevcencoNessuna valutazione finora
- RosuvastatinDocumento13 pagineRosuvastatinZahid MahmoodNessuna valutazione finora
- Oxidative Stress and Diabetes: Antioxidative StrategiesDocumento18 pagineOxidative Stress and Diabetes: Antioxidative StrategiesClaudia DoloresNessuna valutazione finora
- Insulin Resistance and Atherosclerosis: Julie Nigro, Narin Osman, Anthony M. Dart, and Peter J. LittleDocumento18 pagineInsulin Resistance and Atherosclerosis: Julie Nigro, Narin Osman, Anthony M. Dart, and Peter J. LittlekatyaraujoNessuna valutazione finora
- Zozulinska, 2006Documento5 pagineZozulinska, 2006wanda oktariaNessuna valutazione finora
- Advances in Secondary Prevention Mechanisms of Macrovascular Complications in Type 2 Diabetes Mellitus Patients: A Comprehensive ReviewDocumento20 pagineAdvances in Secondary Prevention Mechanisms of Macrovascular Complications in Type 2 Diabetes Mellitus Patients: A Comprehensive Reviewabenavides39Nessuna valutazione finora
- Abel 2012Documento10 pagineAbel 2012pamela gaitanNessuna valutazione finora
- Pathogenesisof Cardiovasculardiseasein Diabetes: Andrea V. Haas,, Marie E. McdonnellDocumento13 paginePathogenesisof Cardiovasculardiseasein Diabetes: Andrea V. Haas,, Marie E. McdonnellPaulina DiazNessuna valutazione finora
- Diabetes and Hypertension Physiopathology and Therapeutics: Journal of Human Hypertension May 2000Documento7 pagineDiabetes and Hypertension Physiopathology and Therapeutics: Journal of Human Hypertension May 2000chandra9000Nessuna valutazione finora
- Jurnal 1Documento8 pagineJurnal 1Alya AlphiyantiNessuna valutazione finora
- Diabetes and Vascular Disease: Pathophysiology, Clinical Consequences, and Medical Therapy: Part IDocumento11 pagineDiabetes and Vascular Disease: Pathophysiology, Clinical Consequences, and Medical Therapy: Part IHeather PorterNessuna valutazione finora
- Effects of Insulin On The Vasculature: Danna M. Breen and Adria GiaccaDocumento12 pagineEffects of Insulin On The Vasculature: Danna M. Breen and Adria GiaccaAndrea Natalia Palma SilvaNessuna valutazione finora
- Oxidative Stress in The Cardiorenal Metabolic Syndrome: The Therapeutic Trials (G Mancia and TD Giles, Section Editors)Documento6 pagineOxidative Stress in The Cardiorenal Metabolic Syndrome: The Therapeutic Trials (G Mancia and TD Giles, Section Editors)filema2000Nessuna valutazione finora
- Atherosclerosis en DiabetesDocumento11 pagineAtherosclerosis en DiabetesAlexis Jesus GomezNessuna valutazione finora
- Jurnal 1 AcidDocumento15 pagineJurnal 1 AcidawaloeiacidNessuna valutazione finora
- 331 FullDocumento15 pagine331 FullsaravabioNessuna valutazione finora
- Keywords: Diabetes, Hypertension, Obesity, Metabolic Syndrome, Metabolic PathwayDocumento6 pagineKeywords: Diabetes, Hypertension, Obesity, Metabolic Syndrome, Metabolic PathwayFATHICHAHNessuna valutazione finora
- Review Article Oxidative Stress As The Main Target in Diabetic Retinopathy PathophysiologyDocumento22 pagineReview Article Oxidative Stress As The Main Target in Diabetic Retinopathy PathophysiologyAriNessuna valutazione finora
- Pathophysiology of Cardiovascular Disease in Diabetes MellitusDocumento6 paginePathophysiology of Cardiovascular Disease in Diabetes MellitusAnatomska CentralaNessuna valutazione finora
- Ni Hms 765147Documento38 pagineNi Hms 765147pamela gaitanNessuna valutazione finora
- Ijms 23 06500Documento16 pagineIjms 23 06500Aiz IlhanaNessuna valutazione finora
- Inflammation in Metabolic and Cardiovascular Disorders - Role of Oxidative Stress (2021)Documento12 pagineInflammation in Metabolic and Cardiovascular Disorders - Role of Oxidative Stress (2021)Ajeng Shanaz SantyaNessuna valutazione finora
- NIH Public Access: Author ManuscriptDocumento15 pagineNIH Public Access: Author ManuscriptM Nizarwan IslamyNessuna valutazione finora
- Protein Oxidation in Diabetes Mellitus: January 2006Documento34 pagineProtein Oxidation in Diabetes Mellitus: January 2006AdelaKalstumAdiibahNessuna valutazione finora
- Articulo de Como Flavonoides Disminuyen La Aterosclerosi EtcDocumento9 pagineArticulo de Como Flavonoides Disminuyen La Aterosclerosi EtcSandra Marcela PabónNessuna valutazione finora
- Hyper Tension and Diabetes Mellitus: Gurushankar Govindarajan James R Sowers Craig S StumpDocumento7 pagineHyper Tension and Diabetes Mellitus: Gurushankar Govindarajan James R Sowers Craig S StumpAdina StoianNessuna valutazione finora
- Jurnal 2Documento14 pagineJurnal 2Alya AlphiyantiNessuna valutazione finora
- Obesity and Endhotelial DysfuncDocumento19 pagineObesity and Endhotelial DysfuncMumtaz MaulanaNessuna valutazione finora
- Zinc As A Potential Coadjuvant in Therapy For Type 2Documento7 pagineZinc As A Potential Coadjuvant in Therapy For Type 2Ida YulianaNessuna valutazione finora
- Diabetes and Hyperlipidemia: A Direct Quantitative AnalysisDocumento6 pagineDiabetes and Hyperlipidemia: A Direct Quantitative AnalysisAnonymous Kc2tM8Nessuna valutazione finora
- Review Article: Endothelial Dysfunction: The Early Predictor of AtherosclerosisDocumento10 pagineReview Article: Endothelial Dysfunction: The Early Predictor of Atherosclerosisijeoma alumNessuna valutazione finora
- Diabetes Mellitus Is A Group of Metabolic Diseases Characterized byDocumento67 pagineDiabetes Mellitus Is A Group of Metabolic Diseases Characterized byBivek TimalsinaNessuna valutazione finora
- Serum Ferritin and Diabetes Mellitus Type LLDocumento21 pagineSerum Ferritin and Diabetes Mellitus Type LLM.PRASAD NAIDUNessuna valutazione finora
- Literature Review On Diabetes Mellitus Type 2Documento4 pagineLiterature Review On Diabetes Mellitus Type 2qtbghsbnd100% (1)
- Haematological Parameters and Lipid Profile AbnormDocumento10 pagineHaematological Parameters and Lipid Profile AbnormPhelix O DaniyanNessuna valutazione finora
- Dyslipidaemia in Rheumatological Autoimmune Diseases: Tracey E. Toms, Vasileios F. Panoulas and George D. KitasDocumento12 pagineDyslipidaemia in Rheumatological Autoimmune Diseases: Tracey E. Toms, Vasileios F. Panoulas and George D. KitasMithun CbNessuna valutazione finora
- Rheumatological Manifestation in Type 2 Diabetes MellitusDocumento7 pagineRheumatological Manifestation in Type 2 Diabetes MellitusIJAR JOURNALNessuna valutazione finora
- Nitric Oxyde and HypertensionDocumento26 pagineNitric Oxyde and HypertensionSuciatikarahmi AtikarahmiNessuna valutazione finora
- Revisiones: La Disfunción Endotelial en La Angiopatía Diabética. El Factor de Crecimiento Del Endotelio VascularDocumento4 pagineRevisiones: La Disfunción Endotelial en La Angiopatía Diabética. El Factor de Crecimiento Del Endotelio VascularIvan Hernandez FloresNessuna valutazione finora
- Diabetes Mellitus in Patients With Cirrhosis: Clinical Implications and ManagementDocumento15 pagineDiabetes Mellitus in Patients With Cirrhosis: Clinical Implications and ManagementEduardoNessuna valutazione finora
- Diabetes and Vascular Disease: Pathophysiology, Clinical Consequences, and Medical Therapy: Part IDocumento11 pagineDiabetes and Vascular Disease: Pathophysiology, Clinical Consequences, and Medical Therapy: Part IdentheloNessuna valutazione finora
- Eid2019 Article NewInsightsIntoTheMechanismsOf PDFDocumento11 pagineEid2019 Article NewInsightsIntoTheMechanismsOf PDFStella UrdinolaNessuna valutazione finora
- Nativel2018 Article LowerExtremityArterialDiseaseIDocumento14 pagineNativel2018 Article LowerExtremityArterialDiseaseIRaynier GuerreroNessuna valutazione finora
- Type 2 Diabetes MellitusDocumento24 pagineType 2 Diabetes Mellitusdr. M.F. Romdhoni100% (1)
- Disfunctii Vaculare, Ateroscleroza Si Calcificari VasculareDocumento24 pagineDisfunctii Vaculare, Ateroscleroza Si Calcificari VasculareMikaela W. Marcu100% (1)
- Alzheimer's Disease and Type 2 Diabetes Mellitus: Molecular Mechanisms and SimilaritiesDocumento12 pagineAlzheimer's Disease and Type 2 Diabetes Mellitus: Molecular Mechanisms and SimilaritiesMarco MerazNessuna valutazione finora
- Imune DeseaseDocumento6 pagineImune DeseaseGeorge NicoloiuNessuna valutazione finora
- Cardiovascular Disease and Diabetes: The Vulnerable Patient: Katharina Hess, Nikolaus Marx, and Michael LehrkeDocumento10 pagineCardiovascular Disease and Diabetes: The Vulnerable Patient: Katharina Hess, Nikolaus Marx, and Michael Lehrkekrungi21Nessuna valutazione finora
- Biomarker For The Association Between Body Mass Index and Lipid Peroxidation in T2DM With and Without Microvascular ProblemsDocumento7 pagineBiomarker For The Association Between Body Mass Index and Lipid Peroxidation in T2DM With and Without Microvascular ProblemsEditor IJTSRDNessuna valutazione finora
- Bab 10Documento14 pagineBab 10Anonymous uGI8l9zMsNessuna valutazione finora
- Endothelial Dysfunction in DiabetesDocumento26 pagineEndothelial Dysfunction in DiabetesVera CiobanuNessuna valutazione finora
- Anti Oxidant and DMDocumento1 paginaAnti Oxidant and DMBima BaikuniNessuna valutazione finora
- Diabetes Dan HipertrofiDocumento10 pagineDiabetes Dan HipertrofiHanif FakhruddinNessuna valutazione finora
- Hyperglycemia in Acute StrokeDocumento4 pagineHyperglycemia in Acute StrokeDewi PratiwiNessuna valutazione finora
- Physical Exercise Is A Potential "Medicine" For AtherosclerosisDocumento18 paginePhysical Exercise Is A Potential "Medicine" For AtherosclerosisJesusNavarrete97Nessuna valutazione finora
- Endothelial Dysfunction in Type 2 Diabetes MellitusDocumento7 pagineEndothelial Dysfunction in Type 2 Diabetes MellitusKwame YeboahNessuna valutazione finora
- Pathophysiology 30 00026Documento19 paginePathophysiology 30 00026Ogwal EmmanuelNessuna valutazione finora
- COVID-19 - The Spartacus LetterDocumento41 pagineCOVID-19 - The Spartacus Lettervihkr950689% (9)
- Introduction To Operations and Supply Chain Management 3rd Edition Bozarth Test BankDocumento26 pagineIntroduction To Operations and Supply Chain Management 3rd Edition Bozarth Test BankCaseyBrownaoqn100% (55)
- Stroke in CovidDocumento13 pagineStroke in CovidAbdul AzeezNessuna valutazione finora
- CACAOAMARGODocumento12 pagineCACAOAMARGOVianney Casta¥Eda MonroyNessuna valutazione finora
- Effect of The Rho-Associated Kinase Inhibitor Eye Drop (Ripasudil) On Corneal Endothelial Wound HealingDocumento9 pagineEffect of The Rho-Associated Kinase Inhibitor Eye Drop (Ripasudil) On Corneal Endothelial Wound HealingRaúl Plasencia SaliniNessuna valutazione finora
- Covid19 HypercoagulabilityDocumento22 pagineCovid19 Hypercoagulability陳瑞豐Nessuna valutazione finora
- Neurological Complications of COVID-19: Underlying Mechanisms and ManagementDocumento21 pagineNeurological Complications of COVID-19: Underlying Mechanisms and ManagementAngelita Torres LlacsahuangaNessuna valutazione finora
- A - Covid 19Documento3 pagineA - Covid 19JESUS YOBALNessuna valutazione finora
- Baru Standar 7 S3ffkuh9brs1219brDocumento191 pagineBaru Standar 7 S3ffkuh9brs1219brjumrainiNessuna valutazione finora
- Refresh Pathology 3rd Ed. 2022-Dr. Shiva MDDocumento220 pagineRefresh Pathology 3rd Ed. 2022-Dr. Shiva MD147-haricharan voduri100% (1)
- Cardiovascular DiseaseDocumento5 pagineCardiovascular DiseaseJohn SammutNessuna valutazione finora
- 2019 Raynaud's PhenomenonDocumento21 pagine2019 Raynaud's PhenomenonGerman Gustavo Salgado TapiaNessuna valutazione finora
- Concept MapDocumento4 pagineConcept MapDud AccNessuna valutazione finora
- Primer: AtherosclerosisDocumento18 paginePrimer: AtherosclerosisLeonardoCampanelliNessuna valutazione finora
- 2018 CNGold Nanoparticlesandtheir Applicationsin Cancer TreatmentDocumento19 pagine2018 CNGold Nanoparticlesandtheir Applicationsin Cancer TreatmentShinyNessuna valutazione finora
- Age-Related Impairment of Vascular Structure and FunctionsDocumento21 pagineAge-Related Impairment of Vascular Structure and FunctionsSomnis VeritasNessuna valutazione finora
- Chapter 19 Anatomy and Physiology NotesDocumento11 pagineChapter 19 Anatomy and Physiology NotesZachary WatsonNessuna valutazione finora
- Medical Nutrition Therapy For Cardiovascular DiseaseDocumento210 pagineMedical Nutrition Therapy For Cardiovascular DiseaseBok MatthewNessuna valutazione finora
- Microparticle Clearence Theory of Mechansim of Wet Cupping Therapy (Al-Hijama)Documento5 pagineMicroparticle Clearence Theory of Mechansim of Wet Cupping Therapy (Al-Hijama)AdmirNessuna valutazione finora
- Rina AmeliaDocumento12 pagineRina AmeliaDerison MarsinovaNessuna valutazione finora
- PEDIS Classification in Diabetic Foot Ulcers Patients PDFDocumento5 paginePEDIS Classification in Diabetic Foot Ulcers Patients PDFDeo ValendraNessuna valutazione finora
- Inflammation and RepairDocumento16 pagineInflammation and RepairSuhan HasanNessuna valutazione finora
- Volibris MOA Storyboard v1 1Documento4 pagineVolibris MOA Storyboard v1 1shyamchepurNessuna valutazione finora
- Glucocorticoid Effects On The Immune System - UpToDateDocumento23 pagineGlucocorticoid Effects On The Immune System - UpToDatedita novia maharani100% (1)
- Fistula ArteriovenosaDocumento14 pagineFistula ArteriovenosaJoshua CajinaNessuna valutazione finora
- Ramji 2015Documento13 pagineRamji 2015AlexandraNessuna valutazione finora
- COVID 19 Is A Systemic Vascular HemopathyDocumento34 pagineCOVID 19 Is A Systemic Vascular HemopathyYuri YogyaNessuna valutazione finora
- Introducing Neolife Upbeat Drink MixDocumento7 pagineIntroducing Neolife Upbeat Drink MixRobert BennettNessuna valutazione finora
- Hackam 2022 - Bench To Bedside - New Insights Into The Pathogenesis of Necrotizing EnterocolitisDocumento12 pagineHackam 2022 - Bench To Bedside - New Insights Into The Pathogenesis of Necrotizing EnterocolitisBee GuyNessuna valutazione finora
- Mechanism of Tissue RepairDocumento22 pagineMechanism of Tissue RepairWalidad AarbiNessuna valutazione finora