Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
A Step-By-Step Guide To Performing A Complete Abdominal Examination
Caricato da
jojohnson250Descrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
A Step-By-Step Guide To Performing A Complete Abdominal Examination
Caricato da
jojohnson250Copyright:
Formati disponibili
clinicalskills clinical skills
A step-by-step guide to performing a complete abdominal examination
This clinical skills series is designed for the nursing professional as a basic overview on key clinical skills necessary for patient care, clearly presenting common clinical procedures and their rationale, together with the essential background theory. In this first article in the series, Carol Cox and Martin Steggall describe the process associated with abdominal assessment. It focuses on a systematic approach and highlights areas in which gastrointestinal nurses may enhance their knowledge and practice.
Carol Cox is Professor of Nursing, Advanced Clinical Practice, and Martin Steggall is Head of Department, Applied Biological Sciences, School of Community and Health Sciences, City University, London
Patients present with a variety of abdominal complaints and symptoms. Thus, it is important to have an understanding of the underlying problems that patients may have (Bickley and Szilagyi, 2007). The ability to undertake and document a clear, concise and systematic assessment of a patient is an essential skill for gastrointestinal nurses. In this article, a model of assessment (McGrath, 2004) is described, which gastrointestinal nurses can use to readily identify and prioritize patient care. By undertaking a full and systematic assessment of the abdomen, the gastrointestinal nurse is in a unique position to act upon findings from the assessment and ensure that appropriate medical or nursing intervention occurs. In this article, abdominal examination which is the first part of a 2-part series is presented. In part 2, digital rectal examination (DRE) is presented. DRE follows as the final element in a comprehensive abdominal examination.
Key words
!"Abdominal examination ! Clinical skills ! Inspection !"Palpation !"Percussion and auscultation This article has been subject to double-blind peer review
Background
For the purpose of review, the abdominal cavity is the centre for several of the bodys vital organs, including the liver, gallbladder, stomach, pancreas, spleen, small intestine, cecum, appendix, ascending, transverse, descending and sigmoid colon, kidneys, ureters, adrenal glands, abdominal aorta, inferior vena cava, bladder and rectum (Colbert et al, 2009; Marieb, 2009). The alimentary tract, or gastrointestinal tube, is
approximately 27 feet long (Colbert et al, 2009; Marieb, 2009). It begins at the mouth and ends at the anus. Its function is to ingest and digest food, absorb nutrients, electrolytes and water, and excrete waste. Peristalsis moves food and the products of digestion under the control of the autonomic nervous system (Colbert et al, 2009; Marieb, 2009). A patient with abdominal problems or disease may have a wide range of symptoms. Some problems may be dissociated from the abdominal system directly but impact upon organs in the abdomen, such as in diabetic gastroparesis and anticholinergic drug therapy in which the patient experiences unpleasant abdominal fullness after normal meals or early satiety and therefore has an inability to eat a full meal (Bickley and Szilagyi, 2007) or in pregnancy when, in the third trimester, there is upward displacement of the stomach. In approximately 1520% of pregnant women, the upper portion of the stomach herniates through the diaphragm. This is more common in older, obese and multiparous women after the seventh or eighth month of pregnancy (Seidel et al, 2006). In addition, increased progesterone production causes a decrease in motility and tone of smooth muscles. Therefore, there is a delayed emptying time of the stomach (Seidel et al, 2006; Swartz, 2006; Epstein et al, 2008). Conversely, there is a range of symptoms that are associated with abdominal problems and/or
10
gastrointestinal nursing vol 7 no 1 February 2009
clinical skills
Table 1. Symptoms of abdominal disease
Abdominal pain Anorexia Change in bowel habit Change in abdominal girth Constipation Dark urine Diarrhoea Dyspepsia and belching Dysphagia Haematemesis Jaundice Nausea Pain on swallowing (odynophagia) Pale faeces Bloody faeces Puritus Rectal bleeding Vomiting Weight loss Wind Heartburn Mesenteric angina From: McGrath (2004); Seidel et al (2006)
for diagnosing abdominal problems or disease (Epstein et al, 2008; Cox, 2004a).
Preparation for abdominal assessment
Assessment of the abdomen usually includes assessment of the mouth, abdomen and rectum and is best undertaken in a warm, quiet, welllit environment. Privacy should be provided so that a discrete interview can be conducted and the abdomen exposed for examination. The following equipment should be gathered: gloves, stethoscope, torch, measuring tape, felt-tip pen and a gown and drapes to cover the patient. Explain to the patient that the assessment should not be painful, although they may experience some discomfort at times. As with other forms of assessment, such as cardiac and respiratory assessment, selective listening must be employed during auscultation. Ensure that the patient urinates before beginning the assessment. Positioning of the patient is essential. The patient should be placed in a supine position with arms at their sides and their head on a pillow. To prevent abdominal muscle tensing, flex the patients knees slightly towards their chest. Putting a pillow under the patients knees promotes comfort particularly for patients who find it difficult to maintain flexion of the knees. Ask the patient to breathe quietly and slowly through their mouth. Then ask the patient to point to any areas that are tender and tell them that you will examine those areas last. Observe the patients facial expression as you undertake the assessment. A stoic patient may not admit to experiencing abdominal discomfort. Therefore, a change in facial expression may show when the patient is experiencing discomfort. Subsequently, the assessment can be modified accordingly. The order to be followed in an abdominal assessment is delineated in Table 2. Remember that unlike other forms of assessment, in abdominal assessment the gastrointestinal nurse always begins with inspection and follows this with auscultation so that the abdominal contents are not disturbed, which could alter bowel sounds during auscultation.
disease (Table 1), which should be explored fully if a tentative diagnosis is to be made (Seidel et al, 2006; Epstein et al, 2008; Jarvis, 2008). For example, ageing brings about changes in the functional ability of the gastrointestinal tract, motility of the intestine changes, and secretion and absorption are impacted. Bacterial flora in the intestine undergo changes and become less biologically active, which impairs digestion (Seidel et al, 2006). Older people, therefore, often complain of food intolerance and wind. Furthermore, some older people are unable to report abdominal pain. This, in association with blunted fever and leukocyte response, complicate the diagnosis of abdominal infection in older people (Seidel et al, 2006; Talley and OConnor, 2006). Assessment of abdominal pain in the older adult may be difficult because some of these patients can not communicate their pain (Cox, 2004a). Obtaining a good history from the family, or others who routinely care for the older adult, and using research-based pain assessment tools in association with behavioural cues, is the basis
Table 2. Order for examination of the abdomen
1. 2. 3. 4. Inspection Auscultation Percussion Palpation
Inspection
Begin the assessment by inspecting the patients entire abdomen. Since the liver and spleen lie
12
gastrointestinal nursing vol 7 no 1 February 2009
clinical skills
protected under the ribs, the lower half of the chest must also be inspected. Assess abdominal symmetry, noting overall contour and skin condition as well as the appearance of the umbilicus and any visible pulsations. Assess abdominal contour by standing at the feet of the patient first. Then move to the side of the patient and stoop so that the abdomen is at eye level. Look at the abdominal profile. Is the abdomen fully rounded or distended? Is the umbilicus inverted or everted? Is the abdomen scaphoid in appearance, or is it distended in the upper or lower half only? Normally, the abdomen is concave, symmetrical and moves gently with respiration (Epstein et al, 2008). A concave (scaphoid) abdominal contour may indicate malnutrition, whereas distension may indicate the presence of a tumour, ascites or the accumulation of air. In thin patients, the pulsation of the aorta may be seen in the midline epigastric area (Barkauskas et al, 2002; McGrath, 2004; Jarvis, 2008). Aortic pulsations may be pronounced due to increased intra-abdominal pressure related to the presence of a tumour or ascites. Peristalsis is not normally visible. Strong visible peristalsis indicates intestinal obstruction. Inspect the skin. It normally appears smooth and intact. Look for discolouration, striae, rashes, dilated veins, scars or other lesions. Skin abnormalities allude to underlying problems. Bulging around scars may indicate incisional hernias. Striae, in addition to resulting from pregnancy or obesity, may reflect the presence of an abdominal tumour or another disorder such as Cushings syndrome. Cushings syndrome characteristically causes thin-looking skin and purple striae to occur, which is due to the excessive secretion of cortisol (Seidel et al, 2006). Tortuous or dilated superficial abdominal veins may indicate inferior vena cava obstruction and cutaneous angiomas may indicate liver disease. A blue coloration around the umbilicus may be an early sign of intra-abdominal bleeding. Normally, abdominal veins are not prominent. If abdominal veins are prominent, the direction of flow should be assessed. This can be readily undertaken by placing two fingers at one section of a vein and applying occlusive pressure. Move one of your fingers further along the length of the vein so that this section of vein is flattened (emptied). Then remove the finger that has been moved
along the vein. Look to see in which direction the vein refills. In inferior vena cava obstruction, the blood flow below the umbilicus flows up towards the umbilicus, whereas in portal hypertension the blood flows downwards away from the umbilicus (McGrath, 2004).
Auscultation
Auscultation follows inspection and provides valuable information about gastrointestinal motility and underlying abdominal vessels and organs. Sounds heard upon auscultation can be characterized in the same fashion as in percussion (type of sound, pitch and location). It is preferable for the diaphragm of the stethoscope to be used to hear normal as well as abnormal bowel sounds. The diaphragm transmits high-pitched sounds and provides a broader area of sound whereas the bell transmits softer sounds (Cox, 2004b). When the bell is used, pressure on the bell will, by stretching the patients skin underneath the bell, create a diaphragm effect. Lightly place the stethoscope diaphragm on the abdominal skin in all four quadrants of the abdomen. The four quadrants of the abdomen (right lower quadrant, right upper quadrant, left upper quadrant, left lower quadrant) are divided horizontally and vertically at the umbilicus. Take care not to put pressure on the diaphragm as this may stimulate peristalsis and subsequently mask the usual sounds that would be heard. A systematic approach should be undertaken when listening. Before placing the diaphragm of the stethoscope on the patients abdomen, warm your hands and the diaphragm of the stethoscope in order to prevent muscular contraction. Muscular contraction can alter auscultation findings. Listen with the diaphragm for friction rubs in the area of the liver and spleen. Friction rubs are high pitched and, although in the abdomen are rare, it may indicate inflammation of the peritoneal surface of the organ from tumour, infection or infarction (Seidel et al, 2006; Swartz, 2006). Listen for bowel sounds. Note their frequency and character. Normally, bowel sounds occur irregularly and range 535 per minute. Borborygmi is loud, prolonged gurgles, such as with diarrhoea. Increased sounds occur with gastroenteritis and may indicate intestinal obstruction or hunger.
vol 7 no 1 February 2009 gastrointestinal nursing
13
clinical skills
Table 3. Abnormal auscultation sounds
Bowel sounds Bowel sounds: hyperactive or hypoactive sounds created by air and fluid movement through the bowel Location All four quadrants Possible indication Hyperactive = diarrhoea or early intestinal obstruction; hypoactive/then absent sounds = paralytic ileus of peritonitis; high pitched/ tinkling = intestinal fluid and air under tension in a distended bowel; high pitched/rushing with abdominal cramp = obstruction Partial arterial obstruction or dissecting abdominal aneurysm; renal artery; stenosis; hepatomegaly Hepatic cirrhosis
Systolic bruits: vascular blowing sounds resembling cardiac murmurs Venous hum: continuous, medium-pitched sound caused by blood flow in a large vascular organ
Abdominal aorta; renal artery/iliac artery Epigastric or umbilical
High-pitched sounds suggest intestinal fluid and air under pressure, which is frequently noted in early obstruction. Decreased bowel sounds, on the other hand, occur in peritonitis and paralytic ileus. Seidel et al (2006) indicate the absence of bowel sounds can only be established after 5 minutes of continuous listening. McGrath (2004) indicates that you should listen for up to 7 minutes before deciding that bowel sounds are absent. After listening with the diaphragm, use the bell to listen for vascular sounds. Listen in the epigastric region and each of the four quadrants for bruits in the aortic, renal, iliac and femoral arteries (see Figure 1). Bruits may indicate atherosclerosis (Barkauskas et al, 2002). Abnormal auscultation sounds are listed in Table 3.
Percussion
Abdominal percussion aids in determining the size and location of abdominal organs. Percussion also aids in the assessment of excessive accumulation of fluid and /or air in the abdomen. As in auscultation, a systematic approach should be used in percussing all four quadrants. Percussion sounds vary depending on the density of the organ and the underlying structures. Dull sounds are heard over dense structures, like the liver and spleen, and tympanic sounds are heard over air filled structures, such as the stomach and intestines (see Figure 2). In the obese patient, it may be difficult to discern percussion sounds. Percussion involves striking one object against another to produce percussion sounds (sound waves), which are termed forms of resonance. These arise from vibrations 46 cm deep in the bodys tissues (Seidel et al, 2006; Bickley and Szilagyi, 2007). In percussion, the finger of one hand functions as a hammer (plexor) and strikes the dorsal surface of the opposite hands finger on the interphalangeal joint. To perform this form of indirect percussion, as opposed to direct percussion which is when the hand strikes the patients abdomen directly, the non-dominant hand is placed on the surface of the patients abdomen with the fingers slightly spread. The distal phalanx of the middle finger is placed firmly on the abdominal surface of the patient while the other fingers are held slightly off the surface of the patients abdomen. The wrist
Friction rub: harsh Hepatic and spleen Inflammation of the grating sound that sounds peritoneal surface of an like two pieces of leather organ; liver tumour rubbing together From: McGrath (2004); Epstein et al (2008); Jarvis (2008)
Aorta Right renal artery Right iliac artery Right femoral artery Left renal artery Left iliac artery Left femoral artery
Figure 1. Ausculation sites.
14
gastrointestinal nursing vol 7 no 1 February 2009
clinical skills
of the other hand is snapped downward and the tip of the middle finger, which is being used as the hammer, sharply taps the interphalangeal joint of the finger that is pressing on the patients abdomen (see Figure 3). Refer to Table 4 for the classification of percussion sounds of the abdomen and where these may be heard. Remember, the quieter the percussion sound, the more dense the medium. Therefore, percussion sounds over air are loud and over fluid are less loud. Over solid areas, percussion sounds will be soft. There are several points to consider when percussing the abdomen. The tap of the striking finger (plexor) should be done quickly, lifting the finger to prevent dampening of the sound. Only one location should be percussed at a time, and this should be repeated several times, in each area, in order to facilitate interpretation of the sound. Keep in mind that percussion as well as palpation are contraindicated in patients with suspected abdominal aortic aneurysm and patients who have received organ transplants. Abnormal percussion findings occur in patients with abdominal distension either from the accumulation of air, ascites or masses. High-pitched tympanic sounds may indicate bowel distension associated with air. Ascites will produce shifting dullness. Shifting dullness can be assessed by having the patient lie supine. Percuss for areas of dullness and resonance and mark the borders with a felt-tip pen. Then have the patient lie on one side. Percuss for tympany and dullness and mark the borders again with a felt-tip pen. Ascites fluid settles with gravity. Therefore, you should expect to hear dullness in areas where the fluid has settled and tympany in the areas where the bowel has risen. In patients without ascites, the borders marked with a felt-tip pen will remain relatively the same, whereas in ascites the border of dullness will shift to the dependent side as the fluid resettles with gravity. Whenever the patient has abdominal distension, this should be assessed by taking serial measurements of the patients abdominal girth. To do this, wrap a tape measure around the patients abdomen at the level of the umbilicus and record the measurement. Mark the point of measurement on the patients abdomen. Then explain what you have done either to the patient, their family or others who
Figure 2. Percussion sites and hand placement.
Percussion sites Right upper quadrant Left upper quadrant
Hand placement for percussion
are caring for the patient so that they can measure in the same location when subsequent readings are taken. They can then report any changes to you. Ascites presents in liver failure, peritonitis and abdominal tumour.
Palpation
Palpation is the final component in an abdominal assessment and is used to assess the organs of
Table 4. Percussion sounds of the abdomen
Sound Tympany Hyperresonance Resonance Dullness Description Musical sound/high pitch, little resonance Pitch sounds between tympany and resonance Sustained sound of moderate pitch Short, high pitched sound with little resonance Location Air-filled viscera Base of left lung Vesicular lung tissue or the abdomen Solid organs
From: Seidel et al (2006)
vol 7 no 1 February 2009 gastrointestinal nursing
15
clinical skills
Figure 3. Percussion technique.
the abdominal cavity, to detect muscle spasm, tumours, fluid and areas of tenderness (Seidel et al, 2006; Epstein et al, 2008). It is a sophisticated skill that involves the use of the hands and fingers to gather information about the size, shape, mobility, consistency and tension of abdominal contents through the sense of touch. Touch is considered therapeutic, and is the actuality of laying on of hands. Palpation of the abdomen is a particularly sensitive matter; therefore, the gastrointestinal nurses approach should be gentle. Your hands should be warm and fingernails short, as this is not only practical in terms of the approach to the patient but is also symbolic of the respect you hold for the patient and the privilege the patient gives you in allowing you to examine the patients body. Begin with light palpation. Like auscultation and percussion, palpation should be systematic in assessing all four quadrants. Avoid palpating areas that have been identified by the patient as being tender or problematic. Various parts of the hands and fingers are used for specific types of palpation due to their variance in sensitivity associated with position,
Table 5. Areas of the hand used in palpation
Palmar surface of the hand and finger pads to assess size, consistency, texture, fluid, surgical emphysema and the texture and form of a mass or structure Ulnar surface of the hand and fingers to assess vibration Dorsal surface of the hands to assess temperature From: McGrath (2004)
vibration and temperature. Refer to Table 5 for the areas of the hands to use in palpation. The palmar surface of the hand and fingers is more sensitive than the fingertips and is used to discern size and shape. The back of the hand is used to discern hot and cold. The ulner surface of the hand is used to assess vibration. Gently rest the palm of your hand with the fingers extended on the patients abdomen. Use the palmar surface of your fingers to depress the abdominal wall approximately 12 cm. Employ a light even pressing motion as this helps to relax the patient. Avoid short quick jabs, which can frighten the patient and cause discomfort. If the patient is ticklish, ask the patient to rest their hand on the top of yours. This will often decrease the patients ticklish response. Move your hands in a circular fashion so that the abdominal wall moves over underlying organs. The patients abdomen should feel smooth and have a consistent softness throughout. When inflammation or tenderness is present, the patient will guard their abdomen (Barkauskas, 2002). When this resistance occurs, determine whether it is voluntary or involuntary by placing a pillow under the patients knees (if you have not already done so) and ask the patient to breathe slowly through their mouth. If guarding remains then it is probably an involuntary response. Board-like hardness of the abdominal wall is an indication of peritonitis and appendicitis. Deep palpation is required to assess abdominal organs and detect masses. Use the palmar surface of your extended fingers to press deeply into the abdominal wall, approximately 46 cm. Systematically assess all four quadrants. Be aware that deep palpation may evoke tenderness in healthy patients over the cecum, sigmoid colon and aorta. Identify any masses and determine whether they are superficial (located in the abdominal wall) or intra-abdominal by having the patient raise their head off the pillow. This action contracts the abdominal muscles; subsequently, masses in the abdominal wall will continue to be palpable whereas those in the abdominal cavity will be difficult to feel. In addition to assessing all four quadrants, particular attention should be paid to the umbilical ring. This area should be smooth and free of bulges, nodules or granulation. If the umbilical
16
gastrointestinal nursing vol 7 no 1 February 2009
clinical skills
ring is soft in the centre, this suggests a hernia. Specific structures, such as the liver, should be palpated as well. The liver is difficult to assess because it lies under the eleventh and twelfth ribs. To assess the liver, place your right hand on the patients abdomen with your fingers pointing towards the patients head. Ask the patient to breathe regularly a few times and then to take a deep breath. As the patient takes a deep breath, try to feel the liver edge as the diaphragm pushes the liver down. Normally, the liver is not palpable except in very thin people. When a tumour or cirrhosis is present, the edge of the liver will feel hard and irregular.
Bickley L, Szilagyi P (2007) Bates Guide to Physical Examination. 5th edn. Lippincott, Philadelphia Colbert B, Ankney J, Lee K, Steggall M, Dingle M (2009) The gastrointestinal system: fuel for the trip. In: Colbert B, Ankney J, Lee K, Steggall M, Dingle M (eds). Anatomy and Physiology for Nursing and Health Professionals. Pearson Education, Harlow Cox C (2004a) Assessment of Disability Including Care of the Older adult, Physical Assessment for Nurses. Blackwell Publishing, Oxford Cox C (2004b) Examination of the Cardiovascular System, Physical Assessment for Nurses. Blackwell Publishing, Oxford Epstein O, Perkin G, de Bono D, Cookson J (2008) Clinical Examination. 4th edn. Mosby, London Jarvis C (2008) Physical Examination & Health Assessment. 5th edn. Saunders, St. Louis Long MS (ed) (2002) History and examination. Gastrointestinal System. 2nd edn. Mosby, Edinburgh: 197202 Marieb E (2009) Essentials of Human Anatomy and Physiology. 9th edn. Benjamin Cummings, San Francisco Marsh AMA (2004) History and examination. Abdominal Examination. 2nd edn. Mosby, Edinburgh: 11936 McGrath A (2004) Abdominal examination. In: Cox C (ed). Physical Assessment for Nurses. Blackwell Publishing, Oxford Royal College of Nursing (2008) Advanced Nurse Practitioners: An RCN Guide to the Advanced Nurse Practitioner Role, Competencies and Programme Accreditation. RCN, London Royal College of Nursing (2003) Digital Rectal Examination and Manual Removal of Faeces: Guidance for Nurses. 3rd edn. RCN, London Seidel H, Ball J, Dains J, Benedict G (2006) Mosbys Guide to Physical Examination. 6th edn. Mosby, St. Louis Swartz M (2006) Physical Diagnosis, History and Examination. 5th edn. WB Saunders, London Talley N, OConnor S (2006) Clinical Examination: A Systematic Guide to Physical Diagnosis. 5th edn. Churchill Livingstone, London
Conclusion
In this article, the essentials of abdominal examination (excluding DRE) have been presented. The gastrointestinal nurse will find the information related to the processes of inspection, auscultation, percussion and palpation useful when examining patients at their first visit and subsequent visits when patient complaints occur or complications arise. Examination of the abdomen can tell the gastrointestinal nurse much about the overall health status of the patient and provides a baseline for diagnoses and treatment. In part 2, the process of undertaking a thorough DRE will be presented. As with abdominal examination, DRE aids in the identification of serious complications/pathology that prompt further clinical investigation. !
Barkauskas V, Baumann L, Darling-Fisher C (2002) Health and Physical Assessment. 3rd edn. Mosby, London
vol 7 no 1 February 2009 gastrointestinal nursing
17
Potrebbero piacerti anche
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Acute Abdominal Pain: Presented by Dr. Kolahdouzan Thoracic Surgen Alzahra HospitalDocumento77 pagineAcute Abdominal Pain: Presented by Dr. Kolahdouzan Thoracic Surgen Alzahra HospitalGraceline Margaretha Marsintauly SianiparNessuna valutazione finora
- A Simple Guide to Acalculous Cholecystopathy, Diagnosis, Treatment and Related ConditionsDa EverandA Simple Guide to Acalculous Cholecystopathy, Diagnosis, Treatment and Related ConditionsNessuna valutazione finora
- Bowel ObstructionDocumento6 pagineBowel ObstructionKryza Dale Bunado BaticanNessuna valutazione finora
- Gastrointestinal Diseases and Disorders Sourcebook, Fifth EditionDa EverandGastrointestinal Diseases and Disorders Sourcebook, Fifth EditionNessuna valutazione finora
- Thyroid SwellingDocumento8 pagineThyroid SwellingDn Ezrinah Dn Esham50% (2)
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Jaundice: Seminar Under The Guidance Of-Dr. Shiva NarangDocumento47 pagineJaundice: Seminar Under The Guidance Of-Dr. Shiva NarangMiguel MansillaNessuna valutazione finora
- Practical Gastroenterology and Hepatology Board Review ToolkitDa EverandPractical Gastroenterology and Hepatology Board Review ToolkitKenneth R. DeVaultNessuna valutazione finora
- Basic Thyroid ExaminationDocumento6 pagineBasic Thyroid ExaminationPalwasha MalikNessuna valutazione finora
- Obesity and Esophageal DisordersDa EverandObesity and Esophageal DisordersDhyanesh PatelNessuna valutazione finora
- Acute Abdominal Pain: Associate Professor, Dept. of Surgery Mti, KMC, KTHDocumento45 pagineAcute Abdominal Pain: Associate Professor, Dept. of Surgery Mti, KMC, KTHWaleed MaboodNessuna valutazione finora
- Gastrointestinal Bleeding, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandGastrointestinal Bleeding, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Acute Abdomen &peritonitisDocumento63 pagineAcute Abdomen &peritonitisSamar Ahmad100% (1)
- Abdominal Pain in ChildrenDocumento48 pagineAbdominal Pain in ChildrenSurin Jayawardene100% (1)
- Case Presentation Lump Right HypochondriumDocumento22 pagineCase Presentation Lump Right HypochondriumNANDAN RAINessuna valutazione finora
- Acute Abdominal Pain MS LectureDocumento63 pagineAcute Abdominal Pain MS Lectureheka_amrongNessuna valutazione finora
- Inflammatory Bowel DiseaseDocumento51 pagineInflammatory Bowel DiseaseTeena Chandran100% (1)
- Diverticular DiseaseDocumento30 pagineDiverticular Diseasept.mahmoudNessuna valutazione finora
- What Is A Cystoscopy?Documento3 pagineWhat Is A Cystoscopy?Harley Justiniani Dela Cruz100% (1)
- Large Bowel Obstruction by Nic MDocumento42 pagineLarge Bowel Obstruction by Nic MRisky OpponentNessuna valutazione finora
- The Acute AbdomenDocumento174 pagineThe Acute AbdomenHabibHusseinJasmanNessuna valutazione finora
- Managing The Bladder and Bowel in Spina BifidaDocumento77 pagineManaging The Bladder and Bowel in Spina BifidaSeptinaAyuSamsiati100% (1)
- Duodenal UlcerDocumento1 paginaDuodenal UlcerNeferterieManguinaoVillanueva100% (1)
- Investigation and Treatment of Surgical JaundiceDocumento38 pagineInvestigation and Treatment of Surgical JaundiceUjas PatelNessuna valutazione finora
- Abdominal Trauma: Dr. Sri Indah Aruminingsih, SP - RadDocumento135 pagineAbdominal Trauma: Dr. Sri Indah Aruminingsih, SP - RadwidyastutiNessuna valutazione finora
- 01 - Signs and Symptoms of Git DisordersDocumento51 pagine01 - Signs and Symptoms of Git DisordersRere AnugrahNessuna valutazione finora
- Peptic Ulcer Disease - EMEDICINE.2020Documento47 paginePeptic Ulcer Disease - EMEDICINE.2020qayyum consultantfpsc100% (1)
- Cholangitis: Reported By: R. DongaranDocumento18 pagineCholangitis: Reported By: R. DongaranVishnu Karunakaran100% (1)
- Rebound Tenderness TestDocumento2 pagineRebound Tenderness TestDesya100% (1)
- Acute AbdomenDocumento19 pagineAcute AbdomenNazmi Z. MehmetiNessuna valutazione finora
- 6 Imaging of Acute AbdomenDocumento73 pagine6 Imaging of Acute AbdomenAliyah Tofani PawelloiNessuna valutazione finora
- Breast Pain - History TakingDocumento6 pagineBreast Pain - History TakingValencia FooNessuna valutazione finora
- Colon Cancer: Risk FactorsDocumento3 pagineColon Cancer: Risk FactorsAshley VillanuevaNessuna valutazione finora
- Colon, Rectum and AnusDocumento121 pagineColon, Rectum and AnusCheng Mochi-MochikoNessuna valutazione finora
- Pyloric StenosisDocumento14 paginePyloric Stenosisgangguan hepatobilierNessuna valutazione finora
- Chapter 14. Abdominal PainDocumento10 pagineChapter 14. Abdominal PaindekergnpNessuna valutazione finora
- Inflammatory Bowel Disease: DefinitionDocumento4 pagineInflammatory Bowel Disease: Definitionkarl abiaadNessuna valutazione finora
- Compartment Syndrome: Sebelas Maret UniversityDocumento8 pagineCompartment Syndrome: Sebelas Maret Universitykhrisna satyaksaNessuna valutazione finora
- Ascitic Fluid AnalysisDocumento3 pagineAscitic Fluid AnalysisLohJNessuna valutazione finora
- Acute Chronic PancreatitisDocumento17 pagineAcute Chronic Pancreatitisjimjose antonyNessuna valutazione finora
- Intestinal Obstruction in Paediatrics - James GathogoDocumento21 pagineIntestinal Obstruction in Paediatrics - James GathogoMalueth Angui100% (1)
- Approach To The Surgical PatientDocumento51 pagineApproach To The Surgical Patientsanjivdas100% (1)
- Intestinal Atresia and StenosisDocumento7 pagineIntestinal Atresia and StenosisMichael NafarinNessuna valutazione finora
- Urinary Incontinence: By: Ayu SorayaDocumento23 pagineUrinary Incontinence: By: Ayu Sorayaandry setiawanNessuna valutazione finora
- Bowel Sounds: Jibran Mohsin Resident, Surgical Unit I SIMS/Services Hospital, LahoreDocumento58 pagineBowel Sounds: Jibran Mohsin Resident, Surgical Unit I SIMS/Services Hospital, LahoreMariajanNessuna valutazione finora
- Vitamin B12 Deficiency and A Patient Case StudyDocumento36 pagineVitamin B12 Deficiency and A Patient Case Studynherm6425100% (1)
- SG3 Paediatric Surgical EmergenciesDocumento69 pagineSG3 Paediatric Surgical EmergenciesDiyana ZatyNessuna valutazione finora
- Ileus MeconiumDocumento27 pagineIleus MeconiumDebby TamaraNessuna valutazione finora
- Function of G I System: The Primary Digestive Functions Are Break Down Food Particles "Documento113 pagineFunction of G I System: The Primary Digestive Functions Are Break Down Food Particles "cherryann_12100% (1)
- Gallbladder HydropsDocumento6 pagineGallbladder HydropsSaifulAnamNessuna valutazione finora
- Umbilical Hernia - Wikipedia PDFDocumento31 pagineUmbilical Hernia - Wikipedia PDFNeelamNessuna valutazione finora
- What Is AchalasiaDocumento6 pagineWhat Is AchalasiaDonnaliza Delos ReyesNessuna valutazione finora
- Nu'man AS DaudDocumento23 pagineNu'man AS DaudHidayat BazeherNessuna valutazione finora
- Powerpoint: Disorders of The EsophagusDocumento65 paginePowerpoint: Disorders of The Esophagusj.doe.hex_8782% (11)
- Abdominal Pain: Resources: Murtagh, John. General Practice 5 EdDocumento26 pagineAbdominal Pain: Resources: Murtagh, John. General Practice 5 EdDewanti PermatasariNessuna valutazione finora
- Upper Gi BleedDocumento20 pagineUpper Gi BleedNaeem Shehzad100% (1)
- Abdominal Compartment Syndrome in ChildrenDocumento12 pagineAbdominal Compartment Syndrome in Childrendian adiNessuna valutazione finora
- Crohn's DiseaseDocumento38 pagineCrohn's Diseasetintukmathew100% (1)
- SAGES Gallbladder CBDDocumento54 pagineSAGES Gallbladder CBDSAGESWeb100% (1)
- Ras Shastra PPT 6Documento10 pagineRas Shastra PPT 6Soham BhureNessuna valutazione finora
- Drug-Nutrient Interaction in Prescriptions ForDocumento7 pagineDrug-Nutrient Interaction in Prescriptions ForRafika DitaNessuna valutazione finora
- Home Composting SystemsDocumento8 pagineHome Composting Systemssumanenthiran123Nessuna valutazione finora
- API 510 Practise Question Nov 07 Rev1Documento200 pagineAPI 510 Practise Question Nov 07 Rev1TRAN THONG SINH100% (3)
- Senior Project RiceberryDocumento76 pagineSenior Project RiceberryIttisak PrommaNessuna valutazione finora
- "Next Friend" and "Guardian Ad Litem" - Difference BetweenDocumento1 pagina"Next Friend" and "Guardian Ad Litem" - Difference BetweenTeh Hong Xhe100% (2)
- Sustainable Development at British Petroleum: Presented by Amardeep Kulshrestha 09BS0000172 Section-EDocumento20 pagineSustainable Development at British Petroleum: Presented by Amardeep Kulshrestha 09BS0000172 Section-EAmar KulshresthaNessuna valutazione finora
- MajorProjects 202112 e 1Documento64 pagineMajorProjects 202112 e 1xtrooz abiNessuna valutazione finora
- Alugbati Plant Pigment Extraction As Natural Watercolor SourceDocumento6 pagineAlugbati Plant Pigment Extraction As Natural Watercolor SourceMike Arvin Serrano100% (1)
- 3 Activities For Adults To Practice Modeling SELDocumento10 pagine3 Activities For Adults To Practice Modeling SELDavid Garcia PerezNessuna valutazione finora
- The Emom Manual: 25 Kettlebell Conditioning WorkoutsDocumento14 pagineThe Emom Manual: 25 Kettlebell Conditioning WorkoutsguilleNessuna valutazione finora
- Comparative Pharmacology For AnesthetistDocumento162 pagineComparative Pharmacology For AnesthetistGayatri PalacherlaNessuna valutazione finora
- Assignment - Lab Accidents and PrecautionsDocumento6 pagineAssignment - Lab Accidents and PrecautionsAnchu AvinashNessuna valutazione finora
- Soil SSCDocumento11 pagineSoil SSCvkjha623477Nessuna valutazione finora
- Thesis ProposalDocumento19 pagineThesis Proposaldharmi subedi75% (4)
- Appendix B - Distance Tables - Metric Units PDFDocumento15 pagineAppendix B - Distance Tables - Metric Units PDFitisINessuna valutazione finora
- Heat Transfer ExampleDocumento4 pagineHeat Transfer Examplekero_the_heroNessuna valutazione finora
- Finite Element Analysis Project ReportDocumento22 pagineFinite Element Analysis Project ReportsaurabhNessuna valutazione finora
- Arsenal Strength Catalog 6.2-1Documento41 pagineArsenal Strength Catalog 6.2-1Mohammed NavedNessuna valutazione finora
- Gender, Slum Poverty and Climate Change in Flooded River Lines in Metro ManilaDocumento53 pagineGender, Slum Poverty and Climate Change in Flooded River Lines in Metro ManilaADBGADNessuna valutazione finora
- Neurocisticercosis PDFDocumento7 pagineNeurocisticercosis PDFFiorella Alexandra HRNessuna valutazione finora
- Chapter Three Liquid Piping SystemDocumento51 pagineChapter Three Liquid Piping SystemMelaku TamiratNessuna valutazione finora
- Latest Low NOx Combustion TechnologyDocumento7 pagineLatest Low NOx Combustion Technology95113309Nessuna valutazione finora
- Basics of Fire SprinklerDocumento21 pagineBasics of Fire SprinklerLeo_1982Nessuna valutazione finora
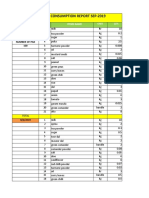
- Daily Staff Food Consumption Reports Sep-2019Documento4 pagineDaily Staff Food Consumption Reports Sep-2019Manjit RawatNessuna valutazione finora
- Carboset CA-600 - CST600 - CO - enDocumento3 pagineCarboset CA-600 - CST600 - CO - enNilsNessuna valutazione finora
- G1 Series User Manual Ver. 1.2Documento101 pagineG1 Series User Manual Ver. 1.2unedo parhusip100% (1)
- Intro To Psychological AssessmentDocumento7 pagineIntro To Psychological AssessmentKian La100% (1)
- Pengaruh Kualitas Anc Dan Riwayat Morbiditas Maternal Terhadap Morbiditas Maternal Di Kabupaten SidoarjoDocumento9 paginePengaruh Kualitas Anc Dan Riwayat Morbiditas Maternal Terhadap Morbiditas Maternal Di Kabupaten Sidoarjohikmah899Nessuna valutazione finora
- ISO - TR - 15608 - 2017 (En) - Pipe Grouping SystemsDocumento12 pagineISO - TR - 15608 - 2017 (En) - Pipe Grouping SystemsTeodor ProdanNessuna valutazione finora
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDa EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNessuna valutazione finora
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (28)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDa EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsValutazione: 5 su 5 stelle5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDa EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeValutazione: 2 su 5 stelle2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 5 su 5 stelle5/5 (81)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDa EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionValutazione: 4 su 5 stelle4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDa EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisValutazione: 4.5 su 5 stelle4.5/5 (42)
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (6)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDa EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDValutazione: 5 su 5 stelle5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDa EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsValutazione: 3.5 su 5 stelle3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDa EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisValutazione: 3.5 su 5 stelle3.5/5 (2)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Da EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Valutazione: 4.5 su 5 stelle4.5/5 (110)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDa EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDa EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsValutazione: 4.5 su 5 stelle4.5/5 (170)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDa EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityValutazione: 4 su 5 stelle4/5 (3)
- Gut: the new and revised Sunday Times bestsellerDa EverandGut: the new and revised Sunday Times bestsellerValutazione: 4 su 5 stelle4/5 (392)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDa EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningValutazione: 4 su 5 stelle4/5 (3)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosDa Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosValutazione: 4.5 su 5 stelle4.5/5 (207)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDa EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisValutazione: 4 su 5 stelle4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDa EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryValutazione: 4 su 5 stelle4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDa EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessValutazione: 4.5 su 5 stelle4.5/5 (328)
- The Marshmallow Test: Mastering Self-ControlDa EverandThe Marshmallow Test: Mastering Self-ControlValutazione: 4.5 su 5 stelle4.5/5 (58)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsDa EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsValutazione: 4.5 su 5 stelle4.5/5 (6)