Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
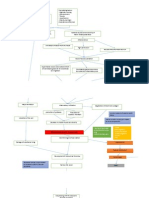
Pathophysiology Headinjury
Caricato da
K.b. DequiñaDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Pathophysiology Headinjury
Caricato da
K.b. DequiñaCopyright:
Formati disponibili
Pathophysiology
Brain function may be immediately impaired by direct damage (eg, crush, laceration) of brain tissue. Further
damage may occur shortly thereafter from the cascade of events triggered by the initial injury.
TBI of any sort can produce cerebral edema and decrease brain blood flow. The cranial vault is fixed in size
(constrained by the skull) and filled by noncompressible CSF and minimally compressible brain tissue;
consequently, any swelling from edema or an intracranial hematoma has nowhere to expand and thus increases
ICP. Cerebral blood flow is proportional to the cerebral perfusion pressure (CPP), which is the difference
between mean arterial pressure (MAP) and mean ICP. Thus, as ICP increases (or MAP decreases), CPP
decreases. When CCP falls below 50 mm Hg, the brain may become ischemic. Ischemia and edema may trigger
various secondary mechanisms of injury (eg, release of excitatory neurotransmitters, intracellular Ca, free
radicals, and cytokines), causing further cell damage, further edema, and further increases in ICP. Systemic
complications from trauma (eg, hypotension, hypoxia) can also contribute to cerebral ischemia and are often
called secondary brain insults.
Excessive ICP initially causes global cerebral dysfunction. If excessive ICP is unrelieved, it can push brain tissue
across the tentorium or through the foramen magnum, causing herniation (see Coma and Impaired
Consciousness: Pathophysiology) and increased morbidity and mortality. If ICP increases to equal MAP, CPP
becomes zero, resulting in complete brain ischemia and brain death; absent cranial blood flow is objective
evidence of brain death (see Coma and Impaired Consciousness: Brain Death).
Hyperemia and increased brain blood flow may result from concussive injury in adolescents or children. Second
impact syndrome is a rare and debated entity defined by sudden increased ICP and death after a second traumatic
insult that follows a minor head injury. It is attributed to loss of autoregulation of cerebral blood flow that leads
to vascular engorgement, increased ICP, and herniation.
Symptoms and Signs
Initially, most patients with moderate or severe TBI lose consciousness (usually for seconds or minutes),
although with minor injuries, some have only confusion or amnesia (amnesia is usually retrograde and lasts for
seconds to a few hours). Young children may simply become irritable. Some patients have seizures, often within
the first hour or day. After these initial symptoms, patients may be fully awake and alert, or consciousness and
function may be altered to some degree, from mild confusion to stupor to coma. Duration of unconsciousness and
severity of obtundation are roughly proportional to injury severity but are not specific.
The Glasgow Coma Scale
Neurologic function may continue to improve for a few yr after TBI, most rapidly during the initial 6 mo.
Diagnosis
• Initial rapid trauma assessment
• Glasgow coma scale and neurologic examination
• CT scan
The vast majority of patients with mild TBI retain good neurologic function. With moderate or severe TBI, the
prognosis is not as good but is much better than is generally believed. The most commonly used scale to assess
outcome in TBI patients is the Glasgow Outcome Scale. On this scale the possible outcomes are:
• Good recovery (return to previous level of function)
• Moderate disability (capable of self-care)
• Severe disability (incapable of self-care)
• Vegetative (no cognitive function)
• Death
Treatment
Multiple noncranial injuries, which are likely with motor vehicle crashes and falls, often require simultaneous
treatment. Initial resuscitation of trauma patients is discussed elsewhere (see Approach to the Trauma Patient).
At the injury scene,a clear airway is secured and external bleeding is controlled before the patient is moved.
Particular care is taken to avoid displacement of the spine or other bones to protect the spinal cord and blood
vessels. Proper immobilization should be maintained with a cervical collar and long spine board until stability of
the entire spine has been established by appropriate examination and imaging (see Spinal Trauma: Diagnosis).
After the initial rapid neurologic assessment, pain should be relieved with a short-acting opioid (eg, fentanyl
Some Trade Names
Traumatic Brain Injury (TBI): Management of Traumatic Brain Injury Based on Severity of Injury ).
Potrebbero piacerti anche
- Pathophysiology of Head TraumaDocumento12 paginePathophysiology of Head TraumaMohammad ZianuddinNessuna valutazione finora
- Ischemic Stroke Guide: Symptoms, Diagnosis & TreatmentDocumento7 pagineIschemic Stroke Guide: Symptoms, Diagnosis & TreatmentAlly Juaneza100% (1)
- Non-Modifiable, Partially Modifiable, and Modifiable Risk Factors for Atherothrombotic DiseaseDocumento15 pagineNon-Modifiable, Partially Modifiable, and Modifiable Risk Factors for Atherothrombotic DiseaseWiljohn de la CruzNessuna valutazione finora
- General Pathophysiology: Predisposing Factors: Precipitating FactorsDocumento2 pagineGeneral Pathophysiology: Predisposing Factors: Precipitating FactorsIrish Nicole DCNessuna valutazione finora
- Pathophysiology of StrokeDocumento22 paginePathophysiology of StrokeKingman844100% (3)
- NCP CvaDocumento4 pagineNCP CvaMariquita BuenafeNessuna valutazione finora
- PPPDocumento3 paginePPPJack BangcoyoNessuna valutazione finora
- Clinical Worksheet for Stroke PatientDocumento6 pagineClinical Worksheet for Stroke PatientJackie GriffisNessuna valutazione finora
- Lacunar Stroke Guide - Causes, Symptoms and Treatment OptionsDocumento6 pagineLacunar Stroke Guide - Causes, Symptoms and Treatment OptionsRismanto TorsioNessuna valutazione finora
- Pathophysiology of Brain Injury: Predisposing Factors: Precipitating FactorsDocumento4 paginePathophysiology of Brain Injury: Predisposing Factors: Precipitating FactorsHoney Lorie D. Simbajon100% (2)
- Nursing Care of Stroke - NewDocumento4 pagineNursing Care of Stroke - Newninda saputriNessuna valutazione finora
- Pathophysiology of Ischemic Stroke - UpToDateDocumento11 paginePathophysiology of Ischemic Stroke - UpToDateKarla AldamaNessuna valutazione finora
- Human Diseases Case Study 18 ADocumento4 pagineHuman Diseases Case Study 18 Aairickann100% (1)
- A Subdural HematomaDocumento12 pagineA Subdural HematomaGina Irene IshakNessuna valutazione finora
- Organophosphrous PoisoningDocumento53 pagineOrganophosphrous Poisoningpriyashu78100% (1)
- Aneurysmal Subarachnoid Hemorrhage.6Documento19 pagineAneurysmal Subarachnoid Hemorrhage.6Aldy Setiawan PutraNessuna valutazione finora
- Predisposing and precipitating factors of abdominal aortic aneurysmDocumento6 paginePredisposing and precipitating factors of abdominal aortic aneurysmSandrine BarredoNessuna valutazione finora
- Patho Sheet For Hypovolemic ShockDocumento3 paginePatho Sheet For Hypovolemic ShockAnnie JohnsonNessuna valutazione finora
- PATHOPHYSIOLOGYDocumento1 paginaPATHOPHYSIOLOGYJeroham CoNessuna valutazione finora
- Head Trauma: Yoon Seung-Hwan, M.DDocumento53 pagineHead Trauma: Yoon Seung-Hwan, M.DAhmed ZahranNessuna valutazione finora
- Nephrotic Syndrome PathophysiologyDocumento1 paginaNephrotic Syndrome PathophysiologyKrisianne Mae Lorenzo FranciscoNessuna valutazione finora
- MIDocumento22 pagineMIGagauz SiliviaNessuna valutazione finora
- Pathophysiology HPN CvaDocumento1 paginaPathophysiology HPN Cvatresdos09Nessuna valutazione finora
- Animal and Insect Bites DiseasesDocumento28 pagineAnimal and Insect Bites DiseasesAditya PrabawaNessuna valutazione finora
- Pathophysiology of TetanusDocumento2 paginePathophysiology of TetanusAnitha SuprionoNessuna valutazione finora
- Addison'sDocumento4 pagineAddison'sKoRnflakesNessuna valutazione finora
- Pulmonary Contusion - WikipediaDocumento15 paginePulmonary Contusion - WikipediaRony OktarizalNessuna valutazione finora
- Introduction - MIDocumento10 pagineIntroduction - MIkhimiiiNessuna valutazione finora
- Cerebrovascular AccidentDocumento79 pagineCerebrovascular AccidentKathy B. AbuanNessuna valutazione finora
- 403 Full PDFDocumento10 pagine403 Full PDFKuroto YoshikiNessuna valutazione finora
- Basilar Skull Fractures DiagnosisDocumento16 pagineBasilar Skull Fractures DiagnosisRindahMDNessuna valutazione finora
- BurnsDocumento9 pagineBurnsVincentus BinNessuna valutazione finora
- Pa Tho Physiology of Hemorrhagic StrokeDocumento2 paginePa Tho Physiology of Hemorrhagic StrokeMerlash MerlaNessuna valutazione finora
- Predisposing and precipitating factors leading to ESRD, DM, atherosclerosis, and pneumoniaDocumento11 paginePredisposing and precipitating factors leading to ESRD, DM, atherosclerosis, and pneumoniaJonathan CuaNessuna valutazione finora
- Stroke: Abyot From Harrison, DR Belachew and DR Yared HandoutDocumento32 pagineStroke: Abyot From Harrison, DR Belachew and DR Yared HandoutashuNessuna valutazione finora
- Raynaud's DISEASEDocumento3 pagineRaynaud's DISEASEkondame aisheeNessuna valutazione finora
- NCPDocumento3 pagineNCPErica Denice CastilloNessuna valutazione finora
- Drowning: David Slocum MD Albany Medical CenterDocumento39 pagineDrowning: David Slocum MD Albany Medical CenterPawan SujaneNessuna valutazione finora
- Pathophysiology of Brain Abscess Secondary To Chronic Otitis MediaDocumento5 paginePathophysiology of Brain Abscess Secondary To Chronic Otitis Mediafufulabrador100% (1)
- Case Presentation 1Documento70 pagineCase Presentation 1shadow gonzalezNessuna valutazione finora
- Pa Tho Physiology of ParkinsonDocumento2 paginePa Tho Physiology of Parkinsoncuriosity_killsNessuna valutazione finora
- Esophagea L Cancer: By: Krizzia S. Bunagan-Legasi, RNDocumento20 pagineEsophagea L Cancer: By: Krizzia S. Bunagan-Legasi, RNAnn SalvatierraNessuna valutazione finora
- Hemorrhagic Cerebro Vascular DiseaseDocumento37 pagineHemorrhagic Cerebro Vascular Diseasejbvaldez100% (1)
- Nursing Care Plan For Angina Pectoris NCPDocumento2 pagineNursing Care Plan For Angina Pectoris NCPkarthi karthi100% (1)
- Head Injury: Manali H. Solanki F.Y. M.Sc. Nursing J G College of NursingDocumento31 pagineHead Injury: Manali H. Solanki F.Y. M.Sc. Nursing J G College of NursingWaqar AhmedNessuna valutazione finora
- Types, Causes and Treatments of ComasDocumento3 pagineTypes, Causes and Treatments of ComasgcsNessuna valutazione finora
- Drug Study (AGN)Documento10 pagineDrug Study (AGN)kristineNessuna valutazione finora
- Schematic Diagram: Signs and Symptoms: Headache, Unconsciousness, Nausea and Vomiting, Visual DisturbancesDocumento3 pagineSchematic Diagram: Signs and Symptoms: Headache, Unconsciousness, Nausea and Vomiting, Visual DisturbancesJosett RomanoNessuna valutazione finora
- NSTEMIDocumento33 pagineNSTEMIwaazalimahwahidNessuna valutazione finora
- LA Myxoma Case PresentationDocumento34 pagineLA Myxoma Case PresentationWiwik Puji LestariNessuna valutazione finora
- Rhabdomyolysis Case Study WeeblyDocumento18 pagineRhabdomyolysis Case Study Weeblyapi-241865788Nessuna valutazione finora
- Buerger's DiseaseDocumento13 pagineBuerger's DiseaseJoan JuradoNessuna valutazione finora
- Nursing Care Plan On HyperthermiaDocumento4 pagineNursing Care Plan On HyperthermiaAleah JayaganNessuna valutazione finora
- Burn Injury PathophysiologyDocumento1 paginaBurn Injury PathophysiologyMonique Ann DanoyNessuna valutazione finora
- Tramautic Brain InjuryDocumento95 pagineTramautic Brain InjuryCAROL ANN PATITICONessuna valutazione finora
- Cerebral Concussion (Mini Case Study)Documento8 pagineCerebral Concussion (Mini Case Study)Airalyn Chavez AlaroNessuna valutazione finora
- Traumatic Brain InjuryDocumento81 pagineTraumatic Brain InjuryShine JyothNessuna valutazione finora
- Opiana Christian Joseph - ReseachassignmenttraumaDocumento42 pagineOpiana Christian Joseph - ReseachassignmenttraumaChristian Joseph OpianaNessuna valutazione finora
- Head Trauma Guide: Concussions, Hematomas & CT InterpretationDocumento193 pagineHead Trauma Guide: Concussions, Hematomas & CT InterpretationhanimozaghiNessuna valutazione finora
- Traumatic Brain InjuryDocumento39 pagineTraumatic Brain InjuryDung Nguyễn Thị MỹNessuna valutazione finora
- Drucker Difference Chapter PDFDocumento15 pagineDrucker Difference Chapter PDFantonioNessuna valutazione finora
- Hirstein - Brain Fiction - Self-Deception and The Riddle of Confabulation (MIT, 2005) PDFDocumento303 pagineHirstein - Brain Fiction - Self-Deception and The Riddle of Confabulation (MIT, 2005) PDFAbraao Zuza CostaNessuna valutazione finora
- Organon of Medicine and Principles of Homoeopathic Philosophy & PsychologyDocumento40 pagineOrganon of Medicine and Principles of Homoeopathic Philosophy & PsychologyAmit BangiaNessuna valutazione finora
- Cranial Nerves For NUR 2249Documento1 paginaCranial Nerves For NUR 2249Janine Aytria SaleNessuna valutazione finora
- Aids To The Examination of The Peripheral Nervous System PDFDocumento67 pagineAids To The Examination of The Peripheral Nervous System PDFAdolfoBreaAndrade100% (1)
- LP For Co1Documento5 pagineLP For Co1Rosevie SabillanoNessuna valutazione finora
- Intracranial Pressure Monitoring ReportingDocumento26 pagineIntracranial Pressure Monitoring ReportingMary Johna PancrudoNessuna valutazione finora
- 0PIOIDDocumento77 pagine0PIOIDDipti PatilNessuna valutazione finora
- Cognitive Drill TherapyDocumento148 pagineCognitive Drill Therapydrrakesh4jain100% (1)
- Neurology Past Years Before EhsanDocumento345 pagineNeurology Past Years Before EhsanMohammad AlrefaiNessuna valutazione finora
- Mondriaan Aura CollegeDocumento4 pagineMondriaan Aura CollegeCamae Snyder GangcuangcoNessuna valutazione finora
- Contoh Soal Skenario 4Documento2 pagineContoh Soal Skenario 4NoNessuna valutazione finora
- The Development of Hand Preference in ChildrenDocumento9 pagineThe Development of Hand Preference in Childrenapi-26018051Nessuna valutazione finora
- Chapter 4Documento21 pagineChapter 4muhammad syamimNessuna valutazione finora
- Ion Channels as Drug TargetsDocumento71 pagineIon Channels as Drug TargetsQonita NitaNessuna valutazione finora
- Experience Psychology 3rd Edition King Test BankDocumento36 pagineExperience Psychology 3rd Edition King Test BankAlexandriaBarajasrnaxb100% (14)
- Table 59-5 - Clinical Features of Common DementiasDocumento1 paginaTable 59-5 - Clinical Features of Common DementiasDragutin PetrićNessuna valutazione finora
- The Human Body: An Orientation: © 2018 Pearson Education, IncDocumento44 pagineThe Human Body: An Orientation: © 2018 Pearson Education, IncShana AquinoNessuna valutazione finora
- Pattern of Neurologic Emergencies in Tikur Anbessa Specialized Hospitalemergency Department in Addis Ababa EthiopiaDocumento5 paginePattern of Neurologic Emergencies in Tikur Anbessa Specialized Hospitalemergency Department in Addis Ababa EthiopiaHelen NeguseNessuna valutazione finora
- To Hell and BackDocumento12 pagineTo Hell and Backmelamin1980janNessuna valutazione finora
- ABNORMAL Drill Week2Documento8 pagineABNORMAL Drill Week2MS Zhou Si ViolonNessuna valutazione finora
- Cushing and CheyneDocumento2 pagineCushing and CheyneMirna Ayu Permata SariNessuna valutazione finora
- Kagan Structures Are Brain-BasedDocumento10 pagineKagan Structures Are Brain-BasedYanpinginbkk100% (1)
- Coetzer (2003) The - Development - of - A - Holistic - Community - Based - NeurDocumento6 pagineCoetzer (2003) The - Development - of - A - Holistic - Community - Based - Neurhoranvera10Nessuna valutazione finora
- Pex 02 03 PDFDocumento6 paginePex 02 03 PDFCourtney Sims83% (6)
- Keerthana Kamboji Research Assesment 4 3a 10Documento7 pagineKeerthana Kamboji Research Assesment 4 3a 10api-353150081Nessuna valutazione finora
- 1 Gcse Aqa BiologyDocumento43 pagine1 Gcse Aqa Biologycharlotteamy10Nessuna valutazione finora
- Performance Task in Personal Development (Depression) : Submitted By: Submitted ToDocumento6 paginePerformance Task in Personal Development (Depression) : Submitted By: Submitted ToJanea Arinya100% (1)
- Fasd - A ChecklistDocumento3 pagineFasd - A Checklistapi-287219512Nessuna valutazione finora
- PowerPoint Cognitive DisordersDocumento22 paginePowerPoint Cognitive Disordersiqra-j100% (2)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDa EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionValutazione: 4 su 5 stelle4/5 (402)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingDa EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingValutazione: 5 su 5 stelle5/5 (4)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (13)
- The Happiness Trap: How to Stop Struggling and Start LivingDa EverandThe Happiness Trap: How to Stop Struggling and Start LivingValutazione: 4 su 5 stelle4/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDa EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNessuna valutazione finora
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDa EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsValutazione: 3.5 su 5 stelle3.5/5 (3)
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 5 su 5 stelle5/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 5 su 5 stelle5/5 (78)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDa EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisValutazione: 4 su 5 stelle4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDa EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityValutazione: 3.5 su 5 stelle3.5/5 (2)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDa EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNessuna valutazione finora
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDa EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsValutazione: 4.5 su 5 stelle4.5/5 (169)
- The Ultimate Guide To Memory Improvement TechniquesDa EverandThe Ultimate Guide To Memory Improvement TechniquesValutazione: 5 su 5 stelle5/5 (34)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsDa EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNessuna valutazione finora
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingDa EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingValutazione: 3.5 su 5 stelle3.5/5 (31)
- Techniques Exercises And Tricks For Memory ImprovementDa EverandTechniques Exercises And Tricks For Memory ImprovementValutazione: 4.5 su 5 stelle4.5/5 (40)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisDa EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisValutazione: 5 su 5 stelle5/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Da EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Valutazione: 4.5 su 5 stelle4.5/5 (110)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDa EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDa EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeValutazione: 4.5 su 5 stelle4.5/5 (253)
- Secure Love: Create a Relationship That Lasts a LifetimeDa EverandSecure Love: Create a Relationship That Lasts a LifetimeValutazione: 5 su 5 stelle5/5 (17)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDa EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessValutazione: 4.5 su 5 stelle4.5/5 (327)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDa EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryValutazione: 4 su 5 stelle4/5 (44)