Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Meningococcal Meningitis
Caricato da
April Kirstin Chua0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
59 visualizzazioni6 pagineMeningococcal meningitis is a severe bacterial infection of the bloodstream and meninges. The microorganism that causes this condition is called meningococcus or Neisseria meningitidis. Many people carry this particular bacteria in their nose and throat without any signs of illness, while others may develop serious symptoms. It is often found in young military recruits living together, or among college students living in close quarters in dormitories.
Descrizione originale:
Copyright
© Attribution Non-Commercial (BY-NC)
Formati disponibili
DOC, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoMeningococcal meningitis is a severe bacterial infection of the bloodstream and meninges. The microorganism that causes this condition is called meningococcus or Neisseria meningitidis. Many people carry this particular bacteria in their nose and throat without any signs of illness, while others may develop serious symptoms. It is often found in young military recruits living together, or among college students living in close quarters in dormitories.
Copyright:
Attribution Non-Commercial (BY-NC)
Formati disponibili
Scarica in formato DOC, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
59 visualizzazioni6 pagineMeningococcal Meningitis
Caricato da
April Kirstin ChuaMeningococcal meningitis is a severe bacterial infection of the bloodstream and meninges. The microorganism that causes this condition is called meningococcus or Neisseria meningitidis. Many people carry this particular bacteria in their nose and throat without any signs of illness, while others may develop serious symptoms. It is often found in young military recruits living together, or among college students living in close quarters in dormitories.
Copyright:
Attribution Non-Commercial (BY-NC)
Formati disponibili
Scarica in formato DOC, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 6
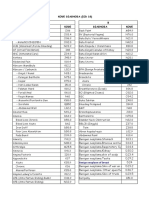
Definition of Meningococcal Meningitis Diagnosis of Meningococcal Meningitis • Are exposed to areas where the the meninges.
ed to areas where the the meninges. Infected fluid from the
Meningococcal meningitis is a severe bacterial A medical history and physical examination epidemic is occurring and the cases meninges then passes into the spinal cord,
infection of the bloodstream and meninges (a are useful but not specific enough to make the are due to Groups A, C, Y, and W-135 causing symptoms including stiff
thin lining covering the brain and spinal cord). diagnosis. Typically a lumbar puncture (also neck, fever andrashes. The meninges (and
The microorganism that causes this condition called a spinal tap) must be done. This • Are military recruits sometimes the brain itself) begin to swell,
is called meningococcus or Neisseria procedure is done by injecting local anesthetic • Have no spleen which affects the central nervous system.
meningitidis (N. meningitidis). (numbing medicine) into the skin of the lower
Description of Meningococcal Meningitis back, then inserting a hollow needle into the Even with antibiotics, approximately 1 in 10
The meningococcus bacteria is spread by lower part of the spinal canal and withdrawing victims of meningococcal meningitis will die;
direct close contact with nose or throat some cerebrospinal fluid. The fluid is then However, about as many survivors of the
discharge of an infected person. Many people stained and cultured to determine the disease lose a limb or their hearing, or suffer
Meningococcal disease describes infections
carry this particular bacteria in their nose and causative organism and to look for signs of permanent brain damage.[3] The sepsis type of
caused by the bacterium Neisseria
throat without any signs of illness, while infection (white blood cells, bacteria, protein). infection is much more deadly, and results in a
meningitidis (also termed meningococcus). It
others may develop serious symptoms. Cultures of blood, sputum and urine will also severe blood poisoningcalled meningococcal
carries a high mortality rate if untreated.
be obtained. In all patients with suspected sepsis that affects the entire body. In this
Whilst best known as a cause of meningitis,
meningitis, chest films and CT scans of the case, bacterial toxins rupture blood vessels
Causes and Risk Factors of Meningococcal widespread blood infection (sepsis) is more
brain are done to look for other sources of and can rapidly shut down vital organs. Within
Meningitis damaging and dangerous. Meningitis
infections and to rule out other diagnoses. hours, patient's health can change from
Meningococcal meningitis occurs as a and Meningococcemia are major causes of
Treatment of Meningococcal Meningitis seemingly good to mortally ill.[4]
communicable disease between humans. It is illness, death, and disability in both developed
often found in young military recruits living Bacterial meningitis is a medical and under developed countries worldwide. The N. meningitidis bacterium is surrounded
together, or among college students living in emergency. Every hour of delay in starting by a slimy outer coat that contains disease-
close quarters in dormitories. antibacterial (antibiotic) therapy increases the The disease's host/pathogen interaction is not
causing endotoxin. While many bacteria
When the cerebrospinal fluid is invaded by this risk of complications and permanent fully understood. The pathogen originates
produce endotoxin, the levels produced by
blood-borne organism. Originating in the neurological damage. Treatment with harmlessly in a large number of the general
meningococcal bacteria are 100 to 1,000
respiratory tract, the meningococcus bacteria intravenous antibiotics (such as penicillin G or population, but thereafter can invade the
times greater (and accordingly more lethal)
travels, via the blood, into the cerebrospinal ceftriaxone) should be started immediately, in blood stream and the brain, causing serious
than normal. As the bacteria multiply and
fluid (the watery liquid that surrounds the some cases even before the lumbar puncture. illness. Over the past few years, experts have
move through the bloodstream, it sheds
brain and spinal cord). During infection, the The regimen of intravenous antibiotics may be made an intensive effort to understand
concentrated amounts of toxin. The endotoxin
bacterium releases a toxin into the fluid continued for up to 7-10 days. specific aspects of meningococcal biology and
directly affects the heart, reducing its ability
causing an inflammatory reaction. Postexposure Prevention host interactions, however the development of
to circulate blood, and also causes pressure on
If the bacteria invades the blood it can lead Household members, close friends at school improved treatments and effective vaccines
blood vessels throughout the body. As some
to arthritis, heart infections and pneumonia. If and at home with intensive exposure, and - if will depend on novel efforts by workers in
blood vessels start to hemorrhage, major
it damages the nerves leading into the brain it the child attends child care - all preschool many different fields.[1]
organs like the lungs and kidneys are
could cause hearing loss, learning disabilities, children who are cared for in the same room, The incidence of endemic meningococcal damaged.
motor impairment or mental retardation. should receive an antibiotic such as rifampin, disease during the last 13 years ranges from 1
Symptoms of Meningococcal Meningitis ceftriaxone or ciprofloxacin as soon as Patients suffering from meningococcal disease
to 5 per 100,000 in developed countries, and
The most common symptoms possible (preferably within 24 hours of the are treated with a large dose of antibiotic. The
from 10 to 25 per 100,000 in developing
of meningococcal meningitis are: diagnosis) as a preventive measure. systemic antibiotic flowing through the
countries. During epidemics the incidence of
Prevention of Meningococcal Meningitis bloodstream rapidly kills the bacteria but, as
• Fever meningococcal disease approaches 100 per
A vaccine called meningococcal the bacteria are killed, even more toxin is
• Chills 100,000. There are approximately 2,600 cases
polysaccharide is used to prevent infection by released. It takes up to several days for the
of bacterial meningitis per year in the United
• Headache certain groups of meningococcal bacteria. The States, and on average 333,000 cases in
toxin to be neutralized from the body by using
• Vomiting vaccine works by causing the body to produce continuous liquid treatment and antibiotic
developing countries. The case fatality rate
its own antibodies against the disease. This therapy.[5]
• Stiff neck vaccine only applies to the Groups A, C, Y and
ranges between 10 and 20 per cent.[2]
• Rash W-135 of the meningococcal bacteria. The There are many mental signs of
While Meningococcal disease is not as
vaccine will not protect against Group B. The meningococcal such as paranoia and other
• Confusion contagious as the common cold (which is
mental instabilities.
Symptoms may also include: vaccine is recommended for persons who: spread through casual contact), it can be
• Seizures • Are age two (2) or older transmitted through saliva and occasionally [edit]Meningitis
through close, prolonged general contact with
• Coma • Are susceptible to certain conditions an infected person. The patient with meningococcal meningitis
that may cause meningococcal typically presents with high
• Inability to completely extend the meningitis Pathogenesis fever, meningism (stiff neck),Kernig's sign,
legs
• Are living in, working in, or visiting an severe headache, vomiting, purpura,
• Stiffness in knees and hips area where there is a high incidence Meningococcal disease causes life-threatening photophobia, and sometimes chills, altered
• Shock of meningococcal infection meningitis and sepsis conditions. In the case mental status, or seizures. Diarrhea or
The symptoms may appear 2 to 10 days after of meningitis, bacteria attack the lining respiratory symptoms are less common.
exposure, but usually within 5 days. between the brain and skull called Petechiae is often also present, but does not
always occur, so its absence should not be pneumonia, sometimes associated with septic [edit]Children and adolescents 11 years of Meningitis A,C,Y and W-135 vaccines and
used against the diagnosis of meningococcal shock. With prompt treatment with penicillin age or older those older than 55 years of age. Under
disease. Anyone with symptoms of or chloramphenicol, the prognosis is certain circumstances if unvaccinated health-
It is recommended that primary immunization
meningococcal meningitis should receive excellent. Pericarditis can appear, either as a care personnel cannot get vaccinated and who
against meningococcal disease with Meningitis
intravenus antibiotics pending results septic pericarditis with grave prognosis or as a have intensive contact with oropharyngeal
A,C,Y and W-135 vaccines for all young
of lumbar puncture, as delay in treatment rective pericarditis in the wake of meningitis secretions of infected patients and who do not
adolescents at 11–12 years of age and all
worsens the prognosis. or septicaemia. Myocarditis can be a use proper precautions should receive anti-
unvaccinated older adolescents at 15 years of
complication of meningococcemia and can be infective prophylaxis against meningococcal
[edit]Meningococcemia age. Although conjugate vaccines are the
contributive to shock seen in this form of infection (i.e., 2-day regimen of oral rifampin
preferred meningococcal vaccine in
disease. Pharyngitis and conjunctivitis can also or a single dose of IM ceftriaxone or a single
This section requires expansion. adolescents 11 years of age or older,
appear and can constitute the portal of entry dose of oral ciprofloxacin).[17][22]
polysaccharide vaccines are an acceptable
for the bacterium. Septic arthritis due to N.
alternative if the conjugated vaccine is [edit]Military recruits
Symptoms of meningococcemia are, at least meningitidis can be seen, usually
unavailable.[17][18][20][20]
initially, similar to those of influenza. Typically, accompanying disseminated infection. Other Because the risk of meningococcal disease is
the first symptoms include fever, nausea, forms of disease can rarely be seen, [edit]Adults increased among military recruits, all military
myalgia, headache, arthralgia, chills, diarrhea, like osteomyelitis,endophthalmitis and urethrit recruits routinely receive primary
is. College Students who plan to live in
stiff neck, and malaise. Later symptoms immunization against the disease.[23]
dormitories receive primary immunization with
include septic shock, purpura, hypotension, Prevention Meningitis A,C,Y and W-135 vaccines. [edit]Travelers and tourists
cyanosis, petechiae, seizures, anxiety, Although the risk for meningococcal disease
and multiple organ dysfunction Immunization against meningococcal disease
The most important form of prevention is a for is similar to 18–24 years of age that for the
syndrome. Acute respiratory distress is not a requirement for entry into any
vaccine against N. meningitidis. Different general population of similar age. The college
syndrome and altered mental status may also country, unlike Yellow fever. Only Saudi Arabia
countries have different strains of the bacteria students consider vaccination against
occur. Meningococcal sepsis has a higher require that travelers to their country for the
and therefore use different vaccines. Five meningococcal disease to reduce their risk for
mortality rate then meningococcal meningitis, annual Hajj and Umrah pilgrimage have a
serogroups, A, B, C, Y and W135 are the disease and stated that college health-
but the risk of neurologic sequelae is much certificate of vaccination against
responsible for virtually all cases of the care providers should take a proactive role in
lower.[citation needed] meningococcal disease issued not more than 3
disease in humans. Vaccines are currently providing information about meningococcal
available against four of the five strains, and a disease to students and their parents. years and not less than 10 days before arrival
[edit]Types of infection
vaccine against the B strain is in [21]
Routine primary immunization against in Saudi Arabia.
[edit]Meningococcemia development. Menactra,Menomune of Sanofi- meningococcal disease is recommended for Travelers to or residents of areas where N.
Aventis, Mencevax of GlaxoSmithKline and Nm most adults live in endemic areas and meningitidis is highly endemic or epidemic are
Meningococcemia, like many gram- Vac4-A/C/Y/W-135 (has not been licensed in planning to travel such areas. Although at risk of exposure should receive primary
negative blood infections, can the US) of JN-International Medical conjugate vaccines are the preferred immunization against meningococcal disease.
cause disseminated intravascular Corporation are the commonly used vaccines. meningococcal vaccine in adults 55 years of [18][24]
coagulation (DIC), a condition where blood Vaccines offer significant protection from age or younger, polysaccharide vaccines are
starts to clot throughout the body, sometimes three to five years (plain polysaccharide an acceptable alternative for adults in this age [edit]HIV-infected individuals
causingischemic tissue damage. DIC also vaccine Menomune, Mencevax and NmVac-4) group if the conjugated vaccine is unavailable.
causes bleeding, when the clotting factors are HIV-infected individuals are likely to be at
to more than eight years (conjugate vaccine Since safety and efficacy of conjugate
used up, causing the increased risk for meningococcal disease; HIV-
Menactra).[14][15] vaccines in adults older than 55 years of age
characteristic purpuric rash. infected individuals who wish to reduce their
have not been established to date,
[edit]Vaccinations risk of meningococcal disease may receive
polysaccharide vaccines should be used for
[edit]Meningitis primary immunization against meningococcal
[edit]Children primary immunization in this group.[17][18]
disease.[22] Although efficacy of Meningitis
Meningococcal meningitis is a consequence of
Children 2–10 years of age who are at high [edit]Medical staff and laboratory personnel A,C,Y and W-135 vaccines have not been
bacteria entering the cerebrospinal fluid (CSF)
risk for meningococcal disease such as certain evaluated in HIV-infected individuals to date,
and irritating the meninges - the membranes Health care people should receive routine
chronic medical conditions and travel to or HIV-infected individuals 11–55 years of age
that line the brain and spinal cord. Sub- immunization against meningococcal disease
reside in countries with hyperendemic or may receive primary immunization with the
Saharan Africa, Americas, Western Europe, UK for laboratory personnel who are routinely
epidemic meningococcal disease should conjugated vaccine.[22] Vaccination against
and Ireland face multifarious challenges, 200 exposed to isolates of N. meningitidis.
receive primary immunization. Although safety meningitis do not decrease CD4+ T-cell counts
years after the discovery of bacterial Laboratory personnel and medical staff are at
and efficacy of the vaccine have not been or increase viral load in HIV-infected
meningitis.[6] risk of exposure to N. meningitides or to
established in children younger than 2 years individuals and there has been no evidence
patients with meningococcal disease. Hospital that the vaccines adversely affect survival.[25]
[edit]Other types of age and under outbreak control, the
Infection Control Practices Advisory [26][27]
unconjugated vaccine can be considered....[16]
As with any gram negative bacterium, N. [17][18][19] Committee (HICPAC) recommendations
meningitidis can infect a variety of sites. regarding immunization of health-care workers
that routine vaccination of health-care
Meningococcal pneumonia can appear during personnel is recommended, Any individual 11–
influenza pandemics and in military camps. 55 years of age who wishes to reduce their
This is a multilobar, rapidly evolving risk of meningococcal disease may receive
[edit]Household and other close contacts of carrying the pathogenic strains. Vaccinations The first successful treatment of meningitis days in the nose and pharynx and for up to 24
individuals with invasive are the only answer for reducing the with intravenous and intrathecal penicillin was hours after starting antibiotics. Treatment with
meningococcal disease transmission of the Meningococcal disease.[32] reported in 1944, and the first clinical trials penicillin may not eradicate the bacteria from
[33]
using high doses of intravenous penicillin as the nasopharyngeal carriers.
Protective levels of anticapsular antibodies are
monotherapy for the treatment of meningitis
not achieved until 7–14 days following [edit]Treatment and prognosis were reported in 1950. Since then, penicillin
administration of a meningococcal vaccine, After adherence to the nasopharyngeal
has remained the drug of choice for the
vaccination cannot prevent early onset When meningococcal disease is suspected, mucosa, meningococci are transported to
treatment of meningococcal meningitis.1
disease in these contacts and usually is not treatment must be started immediately and membrane-bound phagocytic vacuoles. Within
recommended following sporadic cases of should not be delayed while waiting for 24 hours, they can be seen in the submucosa,
For related information, see eMedicine
invasive meningococcal disease. Unlike, investigations. Treatment in primary care close to vessels and local immune cells. In
article Meningococcal Infections.
developed countries, in sub-Saharan Africa usually involves prompt intramuscular most cases, meningococcal colonization of
and other under developed countries, entire administration of benzylpenicillin, and then an mucosal surfaces leads to subclinical infection
family live in a single room of a house.[28] urgent transfer to hospital for further care. Pathophysiology or mild symptoms. In approximately 10-20% of
[29]
Meningococcal infection is usually Once in hospital, the antibiotics of choice are cases, N meningitidis enters the bloodstream.
introduced into a household by an usually IV broad spectrum 3rd N meningitidis is a gram-negative, aerobic, In the vascular compartment, they may be
asymptomatic person. Carriage then spreads generationcephalosporins, encapsulated diplococcus that grows best on killed by bactericidal antibodies, complement,
through the household, reaching infants e.g. cefotaxime or ceftriaxone. Benzylpenicillin enriched media such as Mueller-Hinton or and phagocytic cells or may multiply, initiating
usually after one or more other household and chloramphenicol are also effective. chocolate agar, at 37° and in an atmosphere the bacteremic phase. Organisms replicate
members have been infected. Disease is most Supportive measures include IV fluids, oxygen, of 5-10% carbon dioxide. rapidly.
likely to occur in infants and young children inotropic support, e.g. dopamine or
who lack immunity to the strain of organism dobutamine and management of
circulating and who subsequently acquire raised intracranial pressure. Steroid therapy Meningococci comprise numerous serogroups Systemic disease appears with the
carriage of an invasive strain.[30] By preventing may help in some adult patients, but is that are based on the composition of their development of meningococcemia and usually
susceptible contacts from acquiring infection unlikely to affect long term outcomes. polysaccharide capsular antigens. They differ precedes meningitis by 24-48 hours. This can
by directly inhibiting colonization. Close in their agglutination reactions to sera lead to systemic infection in the form of
contacts are defined as those persons who Complications following meningococcal directed against polysaccharide antigens. At bacteremia, metastatic infection that
could have had intimate contact with the disease can be divided into early and late least 13 serogroups have been described: A, commonly involves the meninges (see Media
patient’s oral secretions such as through groups. Early complications include: raised B, C, D, E, H, I, K, L, W-135, X, Y, and Z. file 3), or severe systemic infection with
kissing or sharing of food or drink. The intracranial pressure, disseminated Serogroups B and C have caused most cases circulatory collapse and disseminated
importance of the carrier state in intravascular coagulation, seizures, circulatory of meningococcal meningitis in the United intravascular coagulation (DIC).
meningococcal disease is well known. In collapse and organ failure. Later complications States since the end of World War II; before Meningococcemia leads to diffuse vascular
developed countries the disease transmission are: deafness, blindness, lasting neurological that, group A was more prevalent. More than injury, which is characterized by endothelial
usually occurs in day care, schools and large deficits, reduced IQ, and gangrene leading to 99% of meningococcal infections are caused necrosis, intraluminal thrombosis, and
gatherings where usually disease transmission amputations. by serogroups A, B, C, 29E, or W-135. perivascular hemorrhage.
could occur. Because the meningococcal
organism is transmitted by respiratory
The natural habitat and reservoir for Invasive disease depends on host factors.
droplets and is susceptible to drying, it has
meningococci is the mucosal surfaces of the Infants are protected from meningococcal
been postulated that close contact is
human nasopharynx and, to a lesser extent, disease for the first few months of life by
necessary for transmission. Therefore, the
the urogenital tract and anal canal. transferred maternal antibodies and low rate
disease transmission to other susceptible
Approximately 5-10% of adults are of meningococcal acquisition. Subsequently,
person cannot be prevented. Meningitis occurs
Background asymptomatic nasopharyngeal carriers, but susceptibility peaks at age 6-12 months and
sporadically throughout the year, and since
that number increases to as many as 60-80% decreases again after colonization of closely
the organism has no known reservoir outside
Meningococcal meningitis (International of members of closed populations (eg, military related nonpathogenic bacteria such
of man, asymptomatic carriers are usually the
Classification of Disease-9 [ICD-9] code: recruits in camps). as Neisseria lactamica that have surface
source of transmission.[31] Additionally,
basic hygienemeasures, such as handwashing 036.0) has been recognized as a serious antigens in common with virulent strains.
and not sharing drinking cups, can reduce the problem for almost 200 years. It was first Colonization withN meningitidis gradually
identified definitely by Vieusseux in Geneva in The modes of infection include direct contact replaces the nonpathogenic bacteria and
incidence of infection by limiting exposure. or respiratory droplets from the nose and
When a case is confirmed, all close contacts 1805. The causative organism, Neisseria induces antibodies to the infecting strain, thus
meningitidis,was isolated first in 1887. throat of infected people. Meningococcal reinforcing natural immunity. Invasive disease
with the infected person can be disease most likely occurs within a few days of
offered antibiotics to reduce the likelihood of occurs if no protective bactericidal antibodies
acquisition of a new strain, before the are mounted against the infecting strain.
the infection spreading to other people. Meningococcal disease still is associated with development of specific serum antibodies.
However, rifampin-resistant strains have been a high mortality rate and persistent Meningococci that elaborate a capsule can
reported and the indiscriminate use of neurological defects, particularly among lead to invasive disease. The capsule protects
antibiotics contributes to this problem. infants and young children. The incubation period averages 3-4 days them from desiccation and from host immune
Chemoprophylaxis is commonly used to those (range 1-10 days), which is the period of mechanisms. Adhesins and endotoxins also
close contacts who are at highest risk of communicability. Bacteria can be found for 2-4 enhance their pathogenic potential.
Dysfunctional properdin (ie, component of the Projectile vomiting may purpura fulminans, when it usually is • Perform a neuroimaging study (either
alternative pathway of complement), HIV occur. associated with multiorgan failure (ie, MRI or CT scan) prior to lumbar
infection, functional or anatomical asplenia, o Seizures occur in 40% of Waterhouse-Friderichsen syndrome). puncture in all patients in whom
and congenital complement deficiencies also children with meningitis, meningitis is suspected. CT scan
predispose individuals to meningococcal typically during the first few findings are usually normal. However,
Workup
disease. days. The majority of imaging is an important cause
seizures have a focal onset. of delay of therapy.
o In infants, the illness may Laboratory Studies
Individuals acquire the infection if they are • MRI with contrast is preferred to CT
exposed to virulent bacteria and have no have an insidious onset; stiff scan because MRI better
protective bactericidal antibodies. Smoking neck may be absent. In • Laboratory examination of the demonstrates meningeal lesions,
and concurrent viral infection of the upper children, even when the cerebrospinal fluid (CSF) usually cerebral edema, and cerebral
respiratory tract diminish the integrity of the combination of convulsive confirms the presence of meningitis. ischemia. T1 may show obliterated
respiratory mucosa and increase the likelihood status epilepticus and fever Typical CSF abnormalities in cisterns. Contrast enhances the
of invasive disease. Crowding living conditions is present, the classic signs meningitis include the following: cisterns, and extension of enhancing
also facilitate disease spread, since individuals and symptoms of acute subarachnoid exudate deep into the
o Increased opening pressure
from different areas have different strains of bacterial meningitis may not sulci may be seen in severe cases.
be present.6 (>180 mm water)
meningococci. The risk of invasive disease is Strokes can be seen with the
o Pleocytosis of
development of vasculitis and
higher in the first few days after exposure to a
polymorphonuclear cerebritis. CNS complications that
new strain. Physical leukocytes (WBC counts can be visualized by MRI include
between 10 and 10,000 hydrocephalus, aqueductal
Clinical cells/µL, predominantly
• Neurological signs include nuchal
neutrophils)
obstruction, ventriculitis (especially in
rigidity, lethargy, delirium, coma, or neonates), choroid plexitis, subdural
convulsions. o Decreased glucose effusion, and empyema.
History
concentration (<45 mg/dL)
o Most adult patients have an • Indications for performing CT scan
altered mental state, clinical o Increased protein prior to lumbar puncture include
• In a 2008 published cohort study signs of nuchal rigidity (eg, concentration (>45 mg/dL) altered level of consciousness,
from Netherlands (the Meningitis Kernig sign, Brudzinski sign), • Gram stain and culture of CSF papilledema, focal neurological
Cohort Study), only 70% of the and fever. identify the etiological organism, N deficits, and/or focal or generalized
patients had the classic triad of fever, o Elderly patients are prone to meningitides. In bacterial meningitis, seizure activity.
neck stiffness, and change in mental Gram stain is positive in 70-90% of
have an altered mental state
status. If the presence of rash was untreated cases, and culture results
and a prolonged course with Other Tests
added, 89% of the patients had 2 of are positive in as many as 80% of
fever.
the 4 features.5 cases.
• Meningococcal meningitis is
• Patients older than 30 years were An electroencephalogram (EEG) study is
noted to have petechiae (62%) less • More specialized laboratory tests, sometimes useful to document irritable
characterized by acute onset of which may include culture of CSF and electrical patterns that may predispose the
frequently than younger patients
intense headache, fever, nausea, blood specimens, are needed for patient to seizures. Periodic complexes and
(81%).
vomiting, photophobia, and stiff neck. identification of N meningitidis and periodic lateralizing epileptiform discharges
• Lethargy or drowsiness frequently is
• A more severe but less common form
the serogroup of meningococci, as (PLEDs) may be suggestive of encephalitis
of meningococcal disease is
reported. Stupor or coma is less well as for determining its caused by herpes simplex virus.
meningococcal septicemia, which is
common. If coma is present, the susceptibility to antibiotics.
characterized by rapid circulatory
prognosis is poor.
collapse and a hemorrhagic rash. • Polymerase chain reaction (PCR)8 may
Histologic Findings
• Patients also may complain of skin
• The Waterhouse-Friderichsen
be used to complement standard
rash, which usually points to disease laboratory procedures for the During the first few days, the subarachnoid
syndrome may develop in 10-20% of
progression. diagnosis of meningococcal and ventricular exudate contains large
children with meningococcal
• The clinical pattern of bacterial meningitis.9 The IS1106 PCR is a rapid numbers of neutrophils and necrotic debris.
infection. This syndrome is
meningitis is quite different in young and sensitive test for confirmation of Intracellular and extracellular bacteria can be
characterized by large petechial
children: Bacterial meningitis usually the diagnosis; its sensitivity is not demonstrated. The exudate extends along the
hemorrhages in the skin and mucous
presents as a subacute infection that affected by prior antibiotic perivascular spaces into the cortex and
membranes, fever, septic shock, and
progresses over several days. treatment.10 PCR of the nspA gene cerebral cortex. Purulent material usually is
DIC.
was also reported to be a fast observed in the choroid plexus. With time, the
o Irritability is a common • A petechial or purpuric rash usually is diagnostic test.11 number of mononuclear leukocytes increases,
presenting feature, and found on the trunk, legs, mucous
headache and neck stiffness and they predominate by the end of the first
membranes, and conjunctivae.
may not be present. Imaging Studies week. Fibroblasts also proliferate.
Occasionally, it is on the palms and
soles. The rash may progress to
Inflammatory cells infiltrate leptomeningeal the beginning of sterilization of Therapy should be changed to ceftriaxone (or The infection occurs more often in winter or
and cortical arteries and veins and accumulate pneumococcus by 4 hours. cefotaxime) if the isolate is resistant to spring. It may cause local epidemics at
in the intima. Thrombosis of small vessels penicillin. boarding schools, college dormitories, or
leads to infarction. This pattern is common in military bases.
Surgical Care
autopsied cases.
The use of dexamethasone in the
Surgical interventions may be necessary for management of bacterial meningitis in adults Risk factors include recent exposure to
Treatment the management of complications such as remains controversial. It may be used in meningococcal meningitis and a recent upper
subdural effusions, empyema, and children, especially in those with meningitis respiratory infection.
hydrocephalus. caused by Haemophilus influenzae. In adults
Medical Care Symptoms
with suspected bacterial meningitis, especially
Meningococcal disease is potentially fatal and Medication in high-risk cases, the adjunctive use of
Symptoms usually come on quickly, and may
always should be viewed as a medical dexamethasone may be beneficial.
include:
emergency. Admission to a hospital is
At presentation, meningitis due to N
necessary. To prevent serious neurological Person-to-person transmission can be
meningitidis may be impossible to
morbidity and death, prompt institution of interrupted by chemoprophylaxis, which • Fever and chills
differentiate from other types of meningitis.
antibiotic therapy is essential when the
Thus, empirical treatment with an antibiotic eradicates the asymptomatic nasopharyngeal • Mental status changes
diagnosis of bacterial meningitis is suspected.
with effective CNS penetration should be carrier state. Rifampin, quinolones, and • Nausea and vomiting
based on age and underlying disease status, ceftriaxone are the antimicrobials used to
eradicate meningococci from the • Purple, bruise-like areas (purpura)
• Institute antimicrobial therapy as since delay in treatment is associated with
adverse clinical outcome. nasopharynx. • Rash, pinpoint red spots (petechiae)
soon as possible after the lumbar
puncture is performed. • Sensitivity to light (photophobia)
• If imaging studies are indicated Standard empirical therapy varies according Antibiotics • Severe headache
before lumbar puncture, draw blood to age, as follows: • Stiff neck (meningismus)
for culture and begin administration Penicillin is the drug of choice for the
of empiric antibiotics. Administration treatment of meningococcal meningitis and
septicemia. Chemoprophylactic antimicrobials Other symptoms that can occur with this
of empiric antibiotics is unlikely to • In infants younger than 4 weeks, it
disease:
decrease diagnostic sensitivity if CSF consists of ampicillin plus cefotaxime most commonly used to eradicate
is tested for bacterial antigens early or an aminoglycoside. meningococci include rifampin, quinolones
in the course of the illness. (eg, ciprofloxacin), and sulfonamides. (Also
• Infants aged 4-12 weeks should be included in this category are ceftriaxone, • Agitation
• Long delays may occur in the treated with ampicillin plus a third- minocycline, and spiramycin.) • Bulging fontanelles
emergency department before generation cephalosporin.
initiation of antibiotics in patients • Decreased consciousness
• In children aged 12 weeks to 18
with suspected bacterial meningitis. years, a third-generation • Poor feeding or irritability in children
In general, these delays appear to be cephalosporin or ampicillin plus • Rapid breathing
physician generated and, to a great Meningococcal meningitis is an infection
extent, potentially avoidable.12
chloramphenicol is an appropriate • Unusual posture with the head and
combination. that results in swelling and neck arched backwards
• In children and adults, the • Adults aged 18-50 years and irritation (inflammation) of the (opisthotonos)
recommended initial empiric therapy individuals with basilar skull fracture membranes covering the brain and
consists of third-generation should be treated with a third- spinal cord.
cephalosporins, but the addition of Exams and Tests
generation cephalosporin, while
ampicillin is required in patients in individuals older than 50 years should Causes Physical examination will show:
whom a Listeria species pathogen is be treated with ampicillin plus a
suspected (eg, patients older than 50 Meningococcal meningitis is caused by the
third-generation cephalosporin. bacteria Neisseria meningitidis (also known as
years, neonates). Once the organism • Fast heart rate
is identified, the antibiotic regimen meningococcus).
can be changed appropriately. Once the accurate diagnosis of meningococcal • Fever
• A recent study has suggested that at meningitis is established, appropriate changes Most cases of meningococcal meningitis occur • Mental status changes
least in children, CSF sterilization can be made. Currently, penicillin is the drug in children and adolescents. Meningococcus is • Rash
may occur more rapidly after of choice for the treatment of meningococcal the most common cause of bacterial
meningitis and septicemia. Unresponsiveness meningitis in children and the second most
• Stiff neck
initiation of parenteral antibiotics
than previously suggested, with to penicillin has not been observed in the common cause of bacterial meningitis in
complete sterilization of United States. Routine testing for adults. For any patient who is suspected of having
meningococcus within 2 hours and susceptibility of meningococcal isolates is not meningitis, it is important to perform a lumbar
necessary, unless the patient does not exhibit puncture ("spinal tap"), in which spinal fluid
appropriate clinical response.
(known as cerebrospinal fluid, or CSF) is • Myocarditis
collected for testing.
• Seizures
Tests that may be done include: • Subdural effusion (buildup of fluid
between the skull and brain)
• Blood culture When to Contact a Medical Professional
• Chest x-ray
Call the local emergency number (such as
• CSF examination for cell count, 911) or go to an emergency room if you
glucose, and protein suspect meningitis in a young child who has
• CT scan of the head the following symptoms:
• Gram stain, other special stains,
andculture of CSF
• Feeding difficulties
• White blood cell (WBC) count
• High-pitched cry
• Irritability
Treatment
• Persistent unexplained fever
Treatment with antibiotics should be started
as soon as possible. Ceftriaxone is one of the
Call the local emergency number if you
most commonly used antibiotics for
develop any of the serious symptoms listed
meningococcal meningitis. Penicillin in high
above. Meningitis can quickly become a life-
doses is almost always effective, too.
threatening illness.
If the antibiotic is not working and the health
Prevention
care provider suspects antibiotic resistance,
chloramphenicol may be used. Sometimes All family and close contacts (especially in
corticosteroids may be used, especially in health care or school settings) of people with
children. this type of meningitis should begin antibiotic
treatment as soon as possible to prevent
People in close contact with someone who has spread of the infection. Ask your health care
meningococcal meningitis should be given provider about this during the first visit.
antibiotics to prevent infection. Such people
include: Close contacts in the same household, school,
or day care center should be watched for early
signs of the disease as soon as the first case is
• Household members diagnosed. Always use good hygiene habits,
• Roommates in dormitories such as washing hands before and after
• Those who come into close and long- changing a diaper, or after using the
term contact with an infected person bathroom.
Vaccines are effective for controlling
Outlook (Prognosis)
epidemics. They are currently recommended
Early treatment improves the outcome. The for:
death rate ranges from 5% - 15%. Young
children and adults over 50 have the highest
risk of death. • College students in their first year
living in dormitories
Possible Complications • Military recruits
• Travelers to certain parts of the world
• Brain damage
• Hearing loss
• Hydrocephalus
Potrebbero piacerti anche
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Sputum Specimen CollectionDocumento14 pagineSputum Specimen CollectionHoneylouAzOpondaNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Invitation Letter With Written Pledge EnglishDocumento2 pagineInvitation Letter With Written Pledge EnglishADA ADA SAJANessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- HIV - Aids Lecture DR Nabil.1Documento25 pagineHIV - Aids Lecture DR Nabil.1Hannan AliNessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Hesi Exit RN 2021 v1 160 QuestionsDocumento4 pagineHesi Exit RN 2021 v1 160 Questionsqwivy.com33% (6)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Information On Botox Injection For Anal FissureDocumento2 pagineInformation On Botox Injection For Anal FissureNiyas Ahamed SNessuna valutazione finora
- CAGULADA (BSN 2 - NB) Expanded Program On Immunization ProjectDocumento1 paginaCAGULADA (BSN 2 - NB) Expanded Program On Immunization ProjectTrisha Mikaela CaguladaNessuna valutazione finora
- Shock and Its Nursing InterventionsDocumento3 pagineShock and Its Nursing InterventionsWendy EscalanteNessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Covid19 Rapid Guideline Pneumonia in Adults in The CommunityDocumento15 pagineCovid19 Rapid Guideline Pneumonia in Adults in The CommunityDusan OrescaninNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Discharge Planning: By: Chin V. UlamDocumento2 pagineDischarge Planning: By: Chin V. UlamChin Villanueva UlamNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- B.SC Nursing-2018-Question Papers-First Year-Microbiology FR PDFDocumento1 paginaB.SC Nursing-2018-Question Papers-First Year-Microbiology FR PDFSwapnil satputeNessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Transverse Myelitis - Johns Hopkins MedicineDocumento6 pagineTransverse Myelitis - Johns Hopkins MedicineHaykal Estu BhismoroNessuna valutazione finora
- Valencia Baribar Global Health InitiativesDocumento17 pagineValencia Baribar Global Health InitiativesKrisha Tañare-MalateNessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- M1 Intro To Disease IntroDocumento35 pagineM1 Intro To Disease IntrorealforgiveNessuna valutazione finora
- NSTPDocumento5 pagineNSTPlainrossNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Diabetes Patient Check ListDocumento2 pagineDiabetes Patient Check ListAbdirahman MusseNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Infection Control (Q & A)Documento27 pagineInfection Control (Q & A)Dr. Bimal Hospital Private LimitedNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- GHA 2020 Changes L Training MaterialDocumento42 pagineGHA 2020 Changes L Training MaterialJULIUS TIBERIONessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Klinik Kesihatan Sungai Asap Kertas Kerja Program Leprosy 2020 Prepared By: Dr. Liong Oey KitDocumento4 pagineKlinik Kesihatan Sungai Asap Kertas Kerja Program Leprosy 2020 Prepared By: Dr. Liong Oey KitSAMANTHA LIONG SAM YEE MoeNessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Jurnal Kritis 6 PDFDocumento5 pagineJurnal Kritis 6 PDFEndah Novianti SoenarsinNessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Week 6-MCQ in EBP-1Documento36 pagineWeek 6-MCQ in EBP-1Hasan KhawaldehNessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Diagnosa Icd 10 SilDocumento51 pagineDiagnosa Icd 10 SilinayaNessuna valutazione finora
- The EPIDocumento14 pagineThe EPIMartin Dazel Martin DazelNessuna valutazione finora
- Assignment On MycobacteriaDocumento7 pagineAssignment On MycobacteriaAlamgir HossainNessuna valutazione finora
- Cellulitis and Skin Abscess in Adults: TreatmentDocumento30 pagineCellulitis and Skin Abscess in Adults: TreatmentsebasNessuna valutazione finora
- GlomerulonephritisDocumento26 pagineGlomerulonephritissalsabr21Nessuna valutazione finora
- Niemann Pick DiseaseDocumento3 pagineNiemann Pick Diseaseडा. सत्यदेव त्यागी आर्यNessuna valutazione finora
- Ilovepdf MergedDocumento45 pagineIlovepdf Mergedacte minophenNessuna valutazione finora
- Multidrug-Resistant Tuberculosis: Disease PrimersDocumento27 pagineMultidrug-Resistant Tuberculosis: Disease PrimersErick HernandezNessuna valutazione finora
- New Insights Into The Treatment of Acute Otitis MediaDocumento13 pagineNew Insights Into The Treatment of Acute Otitis MediaAGUS DE COLSANessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Legal Issues CHNDocumento17 pagineLegal Issues CHNSamjhana NeupaneNessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)