Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Deep Vein Thrombosis
Caricato da
Gina FasoloDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Deep Vein Thrombosis
Caricato da
Gina FasoloCopyright:
Formati disponibili
CHAPTER 33 / Nursing Care of Clients with Peripheral Vascular and Lymphatic Disorders 1017
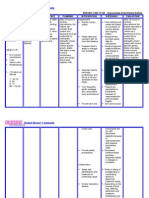
CHART 33–3 NANDA, NIC, AND NOC LINKAGES
The Client with Venous Thrombosis
NURSING DIAGNOSES NURSING INTERVENTIONS NURSING OUTCOMES
• Impaired Physical Mobility • Exercise Therapy: Joint Mobility • Joint Movement: Active
• Environmental Management: Safety • Ambulation: Walking
• Ineffective Health Maintenance • Teaching: Prescribed Activity / Exercise • Knowledge: Health Behaviors
• Teaching: Prescribed Medication • Knowledge: Treatment Regimen
• Ineffective Protection • Bleeding Precautions • Coagulation Status
• Ineffective Tissue Perfusion: Peripheral • Circulatory Care: Venous Insufficiency • Tissue Integrity: Skin and Mucous
• Positioning Membranes
• Tissue Perfusion: Peripheral
• Pain • Heat / Cold Application • Comfort Level
• Coping Enhancement • Pain: Disruptive Effects
Note. Data from Nursing Outcomes Classification (NOC) by M. Johnson & M. Maas (Eds.), 1997, St. Louis: Mosby; Nursing Diagnoses: Definitions & Classification 2001–2002 by
North American Nursing Diagnosis Association, 2001, Philadelphia: NANDA; Nursing Interventions Classification (NIC) by J.C. McCloskey & G. M. Bulechek (Eds.), 2000, St. Louis:
Mosby. Reprinted by permission.
• Initiate oxygen therapy, elevate the head of the bed, and re- tended period of time following hospital discharge. Include the
assure the client who is experiencing manifestations of pul- following topics when teaching for home care.
monary embolism. Oxygen therapy and elevating the head of
• Explanation of the disease process
the bed promote ventilation and gas exchange in those alve-
• Treatment measures, including laboratory tests and their
oli that are well perfused, helping maintain tissue oxygena-
purposes, medications and adverse effects that should be
tion. Reassurance helps reduce anxiety and slow the respira-
reported
tory rate, promoting greater respiratory depth and alveolar
• Appropriate methods of heat application
ventilation.
• Prescribed activity restrictions
Using NANDA, NIC, and NOC • Measures to prevent future episodes of venous thrombosis
• The importance of follow-up visits and laboratory tests as
Chart 33–3 shows links between NANDA nursing diagnoses,
scheduled
NIC (McCloskey & Bulechek, 2000), and NOC (Johnson et al.,
2000) for the client with venous thrombosis. Refer clients for community nursing services for contin-
ued assessment and reinforcement of teaching. Provide refer-
Home Care rals for assistance with ADLs and home maintenance serv-
Treatment measures for venous thrombosis may be initiated ices as indicated. Consider referral for physical therapy if
and carried out on an outpatient basis or continued for an ex- needed.
Nursing Care Plan
A Client with Deep Vein Thrombosis
Mrs. Opal Hipps, age 75, lives alone with her dog, Chester, in her ASSESSMENT
family home in the suburbs. She retired from her job as a postal Mr. Cookson notices that Mrs. Hipps was admit-
clerk 10 years ago and now spends a lot of time reading and ted 14 months ago for repair of a fractured femur. Mrs. Hipps says,
watching television. Over the past week she has developed a “This business about a blood clot really has me worried.” She also
vague aching pain in her right leg. She ignored the pain until last tells Mr. Cookson that she is worried about who will care for her
night when it developed into a much more severe pain in her dog while she is in the hospital. Physical findings include: height
right calf. She noticed that her right lower leg seemed larger 62 inches (157 cm), weight 149 lb (68 kg), T 99.2 F (37.3°C); vital
than the left, and it was very tender to the touch. After seeing her signs within normal limits otherwise.Her left leg is warm and pink,
physician and undergoing Doppler ultrasound studies, Mrs. with strong peripheral pulses and good capillary refill. Her right
Hipps is admitted to the hospital with the diagnosis of deep vein calf is dark red, very warm, and dry to touch. It is tender to palpa-
thrombosis in the right leg. She is placed on bed rest, and intra- tion. The right femoral and popliteal pulses are strong, but the
venous heparin. Michael Cookson, RN, is assigned to admit and pedal and posterior tibial pulses are difficult to locate. The right
care for Mrs. Hipps. calf diameter is 0.5 inch (1.27 cm) larger than the left.
(continued)
1018 UNIT IX / Responses to Altered Peripheral Tissue Perfusion
Nursing Care Plan
A Client with Deep Vein Thrombosis (continued)
DIAGNOSIS • Monitor laboratory values to assess effect of anticoagulant
Mr. Cookson makes the following nursing diag- therapy; report values outside desired range.
noses for Mrs. Hipps. • Assist with progressive ambulation when allowed.
• Pain related to inflammatory response in affected vein • Inspect legs and feet and record findings every 8 hours.
• Anxiety related to unexpected hospitalization and uncertainty
about the seriousness of her illness
EVALUATION
Seven days after admission, the pain in Mrs. Hipps’s right leg has
• Ineffective tissue perfusion: Peripheral related to decreased ve-
subsided and the diameter of her right calf is equal to her left calf.
nous circulation in the right leg
Mrs. Hipps admits to Mr. Cookson that her fears really relate to a
• Risk for impaired skin integrity related to pooling of venous
cousin who was hospitalized for a similar problem and had his leg
blood in the right leg
amputated. After talking about her condition and the steps she
EXPECTED OUTCOMES can take to prevent its recurrence, she is much less anxious. Before
The expected outcomes of the plan of care are that Mrs.Hipps will: discharge, Mr. Cookson reviews instructions for antiembolism
• Verbalize relief of right leg pain by day of discharge. stockings, daily walking, warfarin schedule, and scheduled follow-
• Verbalize reduced anxiety by the second day of her hospitaliza- up appointment. Her neighbor, Kate, came to pick her up. As Mr.
tion. Cookson was helping Mrs. Hipps into the car, Kate handed her a
• Demonstrate reduced right leg diameter by 0.25 inch (0.64 cm) small brown dog and said,“I took good care of Chester for you, but
by the fifth day of hospitalization. he’s missed you.” Mrs. Hipps smiled, and assured Mr. Cookson that
• Maintain intact skin in the right foot throughout the hospital she would call the number he provided if she had any questions.
stay.
Critical Thinking in the Nursing Process
PLANNING AND IMPLEMENTATION 1. Describe the pathophysiologic reasons for the pain in Mrs.
The following interventions are planned and implemented for Hipps’s right leg.
Mrs. Hipps. 2. How would you respond if Mrs. Hipps tells you she does not
• Elevate legs, maintaining slight knee flexion, while in bed. have the money to buy the prescribed anticoagulant when
• Apply warm, moist compresses to right leg using a 2-hour-on, she goes home?
2-hour-off schedule around the clock. 3. How would you change your teaching and discharge plan-
• Administer prescribed analgesics and evaluate effectiveness. ning if Mrs. Hipps had difficulty caring for herself?
• Spend time with Mrs. Hipps to explain venous thrombosis and 4. Design a plan of care for Mrs. Hipps for the diagnosis, Activity
its treatment. intolerance.
• Arrange for a friend or neighbor to care for Mrs. Hipps’s dog.
• Apply antiembolism stockings as ordered; remove for 30 min- See Critical Thinking in the Nursing Process in Appendix C.
utes every 8 hours.
THE CLIENT WITH CHRONIC VENOUS When venous valves are incompetent, the muscle-pumping
INSUFFICIENCY action produced during activity cannot propel blood back to
the heart. Venous blood collects and stagnates in the lower leg
(venous stasis). Venous pressures in the calf and lower leg in-
Chronic venous insufficiency is a disorder of inadequate ve- crease, particularly during ambulation. This increased pres-
nous return over a prolonged period. Deep vein thrombosis is sure impairs arterial circulation to the lower extremities as
the most frequent cause of chronic venous insufficiency. Other well. The body’s ability to provide sufficient oxygen and nu-
conditions, such as varicose veins or leg trauma, may con- trients to the cells and remove metabolic waste products di-
tribute; in some instances, it develops without an identified minishes. Eventually, there is so little oxygen and nutrients
precipitating cause (Braunwald et al., 2001; Tierney et al., that cells begin to die. The skin atrophies, and subcutaneous
2001). fat deposits necrose. Breakdown of red blood cells in the con-
gested tissues causes brown skin pigmentation (Porth, 2002).
Venous stasis ulcers develop. Congested tissues impair the
PATHOPHYSIOLOGY body’s ability to increase the supply of oxygen, nutrients, and
Following DVT, large veins may remain occluded, increasing metabolic energy to heal the ulcer. As a result, the condition
the pressure in other veins of the extremity. This increased pres- worsens and, over time, the ulcers enlarge. The congested ve-
sure distends the veins, separating valve leaflets and impairing nous circulation also prevents the blood from mounting effec-
their ability to close. DVT also damages valve leaflets, causing tive inflammatory and immune responses, significantly in-
them to thicken and contract. The result is impaired unidirec- creasing the risk for infection in the ulcerated tissue (McCance
tional blood flow and deep vein emptying (Porth, 2002). & Huether, 2002).
Potrebbero piacerti anche
- Nursing Care Plan for Postpartum HemorrhageDocumento5 pagineNursing Care Plan for Postpartum HemorrhageDanica Yen PagalNessuna valutazione finora
- Urinary CalculiDocumento2 pagineUrinary CalculiJayceeniPatricia CoronelNessuna valutazione finora
- Baheti CABG PainDocumento49 pagineBaheti CABG PainneareastspineNessuna valutazione finora
- The Effectiveness of Deep Oscillation Therapy On Reducing Swelling and Pain in Athletes With Acute Lateral Ankle SprainsDocumento4 pagineThe Effectiveness of Deep Oscillation Therapy On Reducing Swelling and Pain in Athletes With Acute Lateral Ankle SprainsNyLa LibertyNessuna valutazione finora
- Guillermo Clinical PathwayDocumento5 pagineGuillermo Clinical PathwayLemuel Glenn Bautista100% (1)
- 3-0 Extravasation Injuries FESSH 2022Documento43 pagine3-0 Extravasation Injuries FESSH 2022Professeur Christian DumontierNessuna valutazione finora
- Using NANDA, NIC, and NOC: A Client Having SurgeryDocumento2 pagineUsing NANDA, NIC, and NOC: A Client Having Surgeryinno so qtNessuna valutazione finora
- Chapter 3 Wound HealingDocumento85 pagineChapter 3 Wound HealingShahbaz Sherry 7777Nessuna valutazione finora
- Managing Diverticulitis with Diet and RestDocumento2 pagineManaging Diverticulitis with Diet and RestAhmad RizkiNessuna valutazione finora
- 11 Lumbosacral Radicular PainDocumento3 pagine11 Lumbosacral Radicular PainchairulNessuna valutazione finora
- Surgery SNIDocumento28 pagineSurgery SNIMr Soman Nadim IqbalNessuna valutazione finora
- Nursing The Icu PatientsDocumento31 pagineNursing The Icu PatientsInnocentNessuna valutazione finora
- Tuberculosis of SpineDocumento19 pagineTuberculosis of SpinemelittaaNessuna valutazione finora
- Medical Surgical Nursing Module 12Documento45 pagineMedical Surgical Nursing Module 12weissNessuna valutazione finora
- Msn-Pain - SurgeryDocumento45 pagineMsn-Pain - SurgeryweissNessuna valutazione finora
- Plasma Disc Decompression /nucleoplasty: What Is PDD/Nucleoplasty?Documento7 paginePlasma Disc Decompression /nucleoplasty: What Is PDD/Nucleoplasty?Ijaz KhanNessuna valutazione finora
- Comfort nursing relieves pain and improves ability after spine surgeryDocumento8 pagineComfort nursing relieves pain and improves ability after spine surgeryBella FebriantiNessuna valutazione finora
- Randomized Clinical Study To Compare Negative Pressure Wound Therapy With Simultaneous Saline Irrigation and Traditional Negative Pressure Wound Therapy For Complex Foot InfectionsDocumento8 pagineRandomized Clinical Study To Compare Negative Pressure Wound Therapy With Simultaneous Saline Irrigation and Traditional Negative Pressure Wound Therapy For Complex Foot InfectionsAsmat BurhanNessuna valutazione finora
- Tachycardia PDFDocumento2 pagineTachycardia PDFubaidillah ubaiNessuna valutazione finora
- 02 Patient Safety Bedah Anestesiologi WEBINARDocumento73 pagine02 Patient Safety Bedah Anestesiologi WEBINARSiti AisyahNessuna valutazione finora
- NEW INJECTION PALSY PRTDocumento25 pagineNEW INJECTION PALSY PRTChidube UkachukwuNessuna valutazione finora
- Medi 96 E6490Documento4 pagineMedi 96 E6490TheEdgeNessuna valutazione finora
- Modul KFR Peripheral NeuropathyDocumento68 pagineModul KFR Peripheral NeuropathyHasna Diyani SalamahNessuna valutazione finora
- Physiotherapy Guide for Pain Relief and RehabilitationDocumento42 paginePhysiotherapy Guide for Pain Relief and Rehabilitationakheel ahammedNessuna valutazione finora
- Day 1 - Common Session 2 - Palliative Care and Its Concept - DR Sushma BhatnagarDocumento39 pagineDay 1 - Common Session 2 - Palliative Care and Its Concept - DR Sushma Bhatnagarm debNessuna valutazione finora
- Abandon the "tendinitisDocumento42 pagineAbandon the "tendinitisSAKAI69Nessuna valutazione finora
- The Intraoperative Patient: by Lisa M. Dunn RN, MSN/ED, CCRNDocumento52 pagineThe Intraoperative Patient: by Lisa M. Dunn RN, MSN/ED, CCRNrahmaya100% (1)
- Acute GlomerulonephritisDocumento2 pagineAcute GlomerulonephritisdesaatibagosNessuna valutazione finora
- Perioperative Concepts and Nursing ManagementDocumento28 paginePerioperative Concepts and Nursing ManagementXia WeiNessuna valutazione finora
- English For Doctors - SyllabusDocumento2 pagineEnglish For Doctors - SyllabusEdward AvlTNessuna valutazione finora
- Ask The Experts: Evidence-Based Practice: Percussion and Vibration TherapyDocumento3 pagineAsk The Experts: Evidence-Based Practice: Percussion and Vibration Therapysebastian arayaNessuna valutazione finora
- Chronic venous insufficiency clinical presentation and treatmentDocumento3 pagineChronic venous insufficiency clinical presentation and treatmentAlex Andrés Cuevas UrriolaNessuna valutazione finora
- Epidural AnestesiDocumento28 pagineEpidural AnestesiNur AidahNessuna valutazione finora
- Lumbar Lateral ShiftDocumento8 pagineLumbar Lateral Shiftiretama_Nessuna valutazione finora
- Carpal Tunnel Syndrom Rustam 2024Documento42 pagineCarpal Tunnel Syndrom Rustam 2024white.bear251102Nessuna valutazione finora
- Pain N TensDocumento19 paginePain N TensHimanshu YadavNessuna valutazione finora
- Mirana BSN2-7 NCPDocumento3 pagineMirana BSN2-7 NCPCrystal MiranaNessuna valutazione finora
- Peripheral Receptor Targets for Analgesia: Novel Approaches to Pain ManagementDa EverandPeripheral Receptor Targets for Analgesia: Novel Approaches to Pain ManagementNessuna valutazione finora
- Postoperative Pain Management IMADocumento53 paginePostoperative Pain Management IMAashok_jadonNessuna valutazione finora
- Local Injection Treatment For Lateral Epicondylitis: T. Altay, MD I. Günal, MD and H. Öztürk, MDDocumento4 pagineLocal Injection Treatment For Lateral Epicondylitis: T. Altay, MD I. Günal, MD and H. Öztürk, MDPankaj VatsaNessuna valutazione finora
- Stephen Holt MD-Live Cell Therapy A4MDocumento39 pagineStephen Holt MD-Live Cell Therapy A4MStephen Holt MDNessuna valutazione finora
- 553 - Acupuncture Final - 2Documento35 pagine553 - Acupuncture Final - 2José Manuel Ortiz RodriguezNessuna valutazione finora
- Case Scenario.... : Caesarian SectionDocumento5 pagineCase Scenario.... : Caesarian SectionLyka Joy DavilaNessuna valutazione finora
- 113_PerkinsDocumento1 pagina113_PerkinssimonyanNessuna valutazione finora
- Case Report: MRI Detection of Uterine Necrosis After Uterine Artery Embolization For FibroidsDocumento4 pagineCase Report: MRI Detection of Uterine Necrosis After Uterine Artery Embolization For FibroidsAnwar Ul HaqueNessuna valutazione finora
- Course Task 4 - Thrombophlebitis (De Jesus, LG E.)Documento2 pagineCourse Task 4 - Thrombophlebitis (De Jesus, LG E.)LOVELLE GRACE DE JESUSNessuna valutazione finora
- Nanda Nursing Diagnosis List 2018-2020Documento7 pagineNanda Nursing Diagnosis List 2018-2020jeenath justin doss100% (1)
- Vanzundert 2002Documento10 pagineVanzundert 2002adamNessuna valutazione finora
- Cupping Therapy An Alternative Method ofDocumento5 pagineCupping Therapy An Alternative Method ofKhadiga AhmadNessuna valutazione finora
- Mitsukawa 2012Documento3 pagineMitsukawa 2012adeNessuna valutazione finora
- Burn Management: Frederick W. Endorf and David AhrenholzDocumento5 pagineBurn Management: Frederick W. Endorf and David AhrenholzwilzmaxNessuna valutazione finora
- 7-3-9 - Chest PhysiotherapyDocumento10 pagine7-3-9 - Chest PhysiotherapyPrabu G SatiyaNessuna valutazione finora
- Coronary AtherosclerosisDocumento3 pagineCoronary AtherosclerosisGwyn Oona Florence ForroNessuna valutazione finora
- 0145561318823373Documento4 pagine0145561318823373jtbattaNessuna valutazione finora
- Lichtenstein or Darn Procedure in Inguinal Hernia Repair: A Prospective Randomized Comparative StudyDocumento5 pagineLichtenstein or Darn Procedure in Inguinal Hernia Repair: A Prospective Randomized Comparative StudyFikri AlfarisyiNessuna valutazione finora
- HEINKING CounterstrainInAcuteInjuries ACOFPDocumento60 pagineHEINKING CounterstrainInAcuteInjuries ACOFPRukaphuongNessuna valutazione finora
- Incisional Biopsy: Modul Stase Bedah OnkologiDocumento20 pagineIncisional Biopsy: Modul Stase Bedah OnkologiWara Samsarga GedeNessuna valutazione finora
- Vsim Case Sara Lin Virtual ClinicalDocumento12 pagineVsim Case Sara Lin Virtual ClinicalLivan Martell100% (4)
- Regional Nerve Blocks And Infiltration Therapy: Textbook and Color AtlasDa EverandRegional Nerve Blocks And Infiltration Therapy: Textbook and Color AtlasDanilo JankovicNessuna valutazione finora
- Interventional Radiology of the Spine: Image-Guided Pain TherapyDa EverandInterventional Radiology of the Spine: Image-Guided Pain TherapyJ. Kevin McGrawNessuna valutazione finora
- ACS Guidelines - CPM Guidelines That Will Be in EPICDocumento19 pagineACS Guidelines - CPM Guidelines That Will Be in EPICHimanshu PatelNessuna valutazione finora
- ACLS 2012 Pre-TesteDocumento14 pagineACLS 2012 Pre-TesteVitor Hugo G Correia100% (9)
- ACLS Cheat SheetDocumento8 pagineACLS Cheat SheetLenTheRN85% (27)
- Applebee's Nutrition InfoDocumento9 pagineApplebee's Nutrition InfoJody Ike LinerNessuna valutazione finora
- Metabolic AlkalosisDocumento4 pagineMetabolic AlkalosisCay Sevilla100% (1)
- APA 6 FormatDocumento4 pagineAPA 6 FormatHimanshu PatelNessuna valutazione finora
- Deficit)Documento2 pagineDeficit)goldenboyjNessuna valutazione finora
- Atropine 2011Documento3 pagineAtropine 2011Himanshu PatelNessuna valutazione finora
- A Client With Rheumatoid Arthritis: Nursing Care PlanDocumento1 paginaA Client With Rheumatoid Arthritis: Nursing Care PlanHimanshu Patel100% (1)
- DVT PreventionDocumento8 pagineDVT PreventionRonald ThakorNessuna valutazione finora