Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Brain Tumors in Children!!
Caricato da
melaniefarahdillaDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Brain Tumors in Children!!
Caricato da
melaniefarahdillaCopyright:
Formati disponibili
Brain Tumors in Children: Evaluation and Management
Adam S. Levy, MD
ccording to the National Cancer Institute’s effects on the family of a child with a CNS tumor will be
A Surveillance, Epidemiology, and End Results
(SEER) data, the incidence of central nervous
addressed. Finally, palliative care strategies for children
with CNS tumors will be discussed.
system (CNS) tumors is 27 per 1 million children less
than 19 years old. After leukemias, CNS tumors are
the second most common neoplasm in children. Brain Common Presentations of CNS
tumors are the most common solid tumors of children Tumors
and account for the greatest mortality from cancer in
children.1,2 Approximately 11,000 children in the The presentation of a child with a CNS tumor may
United States will be diagnosed with cancer each year, be subtle or dramatic and is dependent on a combina-
and of these just over 2000 will be CNS tumors. tion of the patient’s age, the tumor location, and the
Over the last 30 years, there appears to be a slow tumor histology.
increase in the overall incidence of childhood cancers In infancy, brain tumors may present insidiously.
in the US, including CNS tumors in children. The Indeed, the only sign of a CNS lesion may be an
overall 5-year survival for patients younger than 19 increased head circumference secondary to hydro-
years with CNS tumors is around 65%.3 The outcome cephalus. When the head circumference is dispropor-
for children with CNS tumors has shown improvement tionately large compared with the length or weight, the
over the last several decades, but remains guarded for pediatrician must consider an intracranial process as
a large subset of children with certain brain tumors. In the cause. While it may be more common that the
comparison to the outcome for children with leuke- relatively increased head circumference is familial,
mias, the outcome for children with brain tumors has this conclusion must be reached with great caution,
not had as dramatic improvement over the past three and a trend of increasing head circumference out of
decades. proportion to the length and weight must be further
CNS tumors represent a diverse group of neoplasms evaluated. Unusual fullness or bulging of the fonta-
of the brain and spine with varying histology. The nelle may also be a sign of hydrocephalus or increas-
clinical presentation is often dictated by the location of ing intracranial pressure. Also, from increased intra-
the tumor in terms of the neurological deficit or cranial pressure, infants or toddlers may present with
obstructive hydrocephalus. The onset may be indolent irritability or Parinaud’s syndrome (paralysis of con-
or rapid depending on the histology and aggressive- jugate upward movement of the eyes and poorly
ness of the tumor. reactive pupils). Developmental delay may be the
The goal of this article is to discuss the common main symptom at diagnosis, but more typical would be
presentations of pediatric CNS tumors, to detail the a loss of previously attained milestones. Thus, a young
appropriate initial evaluation and management, to review toddler who is not yet walking may not be particularly
the more common CNS tumors, and to discuss treatment worrisome, but a toddler who had been walking well
modalities. Long-term follow-up for survivors and the and then becomes ataxic warrants further evaluation.
Likewise, a child who has a primary speech delay
should be approached differently than a child whose
From the The Children’s Hospital at Montefiore, Bronx, New York. speech regresses.
Curr Probl Pediatr Adolesc Health Care 2005;35:230 –245 Toddlers and school-age children may present in a
1538-5442/$ - see front matter
© 2005 Elsevier Inc. All rights reserved. variety of ways. New onset seizure (unrelated to fever)
doi:10.1016/j.cppeds.2005.04.001 is more likely to be secondary to a seizure disorder,
230 Curr Probl Pediatr Adolesc Health Care, July 2005
but an intracranial mass must be considered. The level able resources at the health center. For example, a
of evaluation and timing of studies for patients pre- patient presenting with signs and symptoms of in-
senting with new onset seizure is debated, though creased ICP requires specific management including
many would agree that a magnetic resonance imaging high-dose corticosteroids, relative fluid restriction,
(MRI) of the brain is warranted for new onset seizure head elevation, and possibly neurosurgical interven-
that is not associated with fever. tion. Urgent brain imaging is also indicated.
Many of the symptoms of a brain tumor result from Obtaining an urgent computerized tomography (CT)
increased intracranial pressure (ICP) from either hydro- scan may be more realistic than obtaining an MRI scan
cephalus or the mass effect of the tumor itself. The as MRIs are less commonly available and are likely to
classic presentation of increased ICP is morning head- require prolonged sedation for pediatric patients. Thus,
ache with vomiting. Frequently, there is no nausea while an MRI may be the ideal scan to evaluate a
associated with the emesis. On lying down overnight, patient for a brain tumor, an initial evaluation with a
obstructive hydrocephalus may be worsened as the sleep CT scan is more common and still likely to be useful.
position does not allow gravity to promote cerebrospinal CT scans allow accurate evaluation of ventricle size
fluid (CSF) flow. The increased ICP causes headache and and detection of hemorrhage or stroke. CT scans will
may trigger emesis, and the headache is often relieved also frequently detect brain tumors, especially those
following the emesis. It is not unusual for patients with a associated with calcification.
brain tumor to present with emesis that had been diag- In general, the diagnostic test of choice is an MRI
nosed as acute gastroenteritis. Isolated emesis without with and without contrast (Gadolinium). FLAIR se-
accompanying diarrhea or dyspepsia should alert the quences are often useful in determining tumor infiltra-
pediatrician to the possibility of increased ICP. tion or surrounding edema.4 Diffusion-weighted im-
In older children and adolescents, brain tumors may aging can help differentiate cysts from solid tumors
present secondary to endocrine dysfunction. Some tu- and identify areas of necrosis.5,6 However, while
mors, such as prolactinomas, are the primary cause of standard MRI provides excellent images of anatomical
endocrine dysfunction. Other times, tumor compression structure of the brain and spinal cord, standard MRI
on the pituitary may cause pituitary dysfunction. does not provide information regarding tissue func-
Depending on the tumor location, children may present tion, metabolic state, blood supply, and malignant
with a focal neurological deficit. Diplopia secondary to potential.7 Such information would be clinically useful
cranial nerve deficits is not an uncommon presenting sign in determining surgical approach, response to therapy,
of a brain tumor. For tumors located near the motor and monitoring for relapse.
cortex, specific losses of physical function may be the Newer imaging techniques, broadly referred to as
presenting symptom. Tumors affecting the brainstem functional imaging, are under development and being
commonly present with ataxia. Spinal cord tumors may used more frequently in clinical practice. Magnetic
present with incontinence to urine or stool as well as resonance spectroscopy (MRS) allows for the mea-
other focal deficits. surement of biologically important molecules such as
With ICP increasing to a critical level, a patient’s choline, creatine, N-acetyl aspartate, glutamate, lac-
mental status may be affected and the patient’s vital tate, and lipid. The profile of the concentration of these
signs may be altered. Specifically, the triad of hyper- molecules may differ among tumor, normal brain, or
tension, bradycardia, and tachypnea (Cushing’s Triad) fibrosis and scarring.8 Some studies suggest that tumor
should alert the clinician to the possibility of increased histology can be determined by the signal pattern of
ICP. This is usually a late sign of increased ICP. the molecules.9 Enhanced tumor localization with
Hypertension compensates for the raised ICP in an MRS may also help determine the ideal location for
effort to normalize intracranial blood flow. tissue biopsy10 and may predict outcome and response
to therapy.11
Positron emission tomography (PET) scan is a sen-
Initial Evaluation and Management of sitive and specific imaging tool to evaluate the tissue
Suspected CNS Tumor metabolism. 18Fluorodeoxyglucose, a glucose analog,
is taken up by tissues with high-glucose metabolism,
The initial evaluation of a suspected CNS tumor and this uptake can be measured by PET. Again,
depends on the presenting signs, symptoms, and avail- glucose metabolism may be markedly distinct in tumor
Curr Probl Pediatr Adolesc Health Care, July 2005 231
compared with normal brain or fibrosis and may in the determine adjuvant therapy (either chemotherapy or
future become a more standard tool to help direct radiation therapy). Following adjuvant therapy, a com-
clinical decisions.7 plete resection may then be more safely accom-
In some circumstances, the radiographic presenta- plished.14
tion may be diagnostic obviating the need for tissue Recent advances in neurosurgical techniques have
diagnosis. The most common examples of this are enhanced the ability to biopsy and resect tumors more
diffuse intrinsic brain stem tumors and optic pathway safely. State-of-the-art neurosurgical techniques in-
tumors that are usually low-grade gliomas (to be clude intraoperative navigation systems (neuronaviga-
discussed in detail later). In most other settings, tissue tion), intraoperative MRI, and frameless strereotaxy
is needed to confirm the tumor histology. As such, the that allow intraoperative guidance with the ability to
majority of pediatric patients presenting with a CNS visualize the tumor in multiple planes.15 Cortical
tumor will require a neurosurgical procedure. mapping is frequently needed for tumors in close
proximity to the motor and speech cortex.16
Unfortunately, complications from either the tumor
Neurosurgical Approach to CNS or the surgery are not uncommon. Postoperative swell-
Tumors ing or edema commonly results in worsening of
symptoms in the immediate postoperative period.17
The neurosurgical approach to a CNS tumor depends Focal neurological deficits following surgery are com-
on the clinical status of the patient, the location of the mon but generally have some or complete resolution
lesion, and the suspected histology of the lesion based over time. Hydrocephalus may occur before surgery
on the imaging studies. Urgent surgical intervention but may also develop even after a complete tumor
may be indicated to manage hydrocephalus, hemor- resection either from edema, a hematoma, or an
rhage, or the acute mass effect of a tumor. In these alteration of CSF dynamics that is not clearly de-
settings, the primary goal is to manage the acute fined.15
life-threatening problem. In such circumstances it may Following the resection of a posterior fossa tumor,
be necessary to perform a second neurosurgical pro- approximately 10% of patients may develop “Posterior
cedure to deal more definitively with the tumor. Fossa Syndrome,” also known as cerebellar mutism.
Fortunately, most of the time the presentation of a This syndrome is characterized by postoperative mut-
CNS tumor is not this acute, thereby allowing for ism, ataxia, 6th and 7th nerve palsies, and hemipare-
thoughtful planning. At a minimum, the primary goal sis,18 and this syndrome is more commonly associated
of nonurgent neurosurgical intervention is to obtain with malignant tumors as compared with benign le-
tissue for a histological diagnosis. Depending on the sions. The onset is typically within days of surgery and
location of the mass, this may be accomplished by a recovery may take weeks to months with up to 20% of
biopsy, partial resection, or complete resection (also patients having permanent features.15
referred to as a gross total resection). Other postoperative complications include wound
In general, the outcome for children with brain infection, pseudomeningocele, aseptic meningitis,
tumors is associated with the extent of surgical resec- bacterial meningitis, stroke, and seizures. Given the
tion.12,13 Thus, there is a tendency for experienced technical and clinical considerations involved in the
pediatric neurosurgeons to favor a relatively aggres- neurosurgical management of pediatric CNS tumors,
sive approach. However, the desire to accomplish a the importance of referral to an experienced pediatric
maximal resection or tumor debulking must be tem- neurosurgeon with state-of-the-art operative tools at a
pered by the possible neurological insult from aggres- center with experience treating such patients cannot be
sive surgery. For this reason, it is preferable for overemphasized.
neurosurgical interventions to be made by surgeons
with experience with pediatric CNS tumors in the
setting of a tertiary care hospital where the case can be Radiation Therapy Approach to
discussed with a pediatric oncologist and a radiation Pediatric CNS Tumors
oncologist with pediatric CNS tumor experience.
In a situation where the tumor location precludes For those pediatric brain tumor patients that cannot
complete resection, a biopsy alone will likely help be cured by surgery alone, radiation therapy is fre-
232 Curr Probl Pediatr Adolesc Health Care, July 2005
quently the definitive adjunctive treatment of choice. microscopic disease.19 For tumors with high malig-
The majority of brain tumor patients with high-grade nant potential to spread throughout the CNS, cranio-
or malignant tumors will receive radiation to either the spinal radiation with a boost to the tumor may be
tumor, the resection bed, the whole brain, or the entire indicated. The radiation dose is based on the type of
craniospinal axis. tumor and its location in the body.
Radiation therapy takes advantage of the inherent There have been recent advances in the ability to
differences in radiosensitivity between tumor cells and deliver radiation therapy in the full doses needed to
normal tissues. In general, normal tissue is better able provide tumor response while limiting the exposure of
to tolerate the insult of ionizing radiation than tumor normal surrounding tissue.21 If one considers deliver-
cells. Ionizing radiation causes DNA damage either ing a single high-energy beam to a tumor within the
directly or indirectly by the formation of free radicals brain surrounded by normal tissue, it is clear the
that chemically interact with DNA.19,20 Since the normal tissue between the energy source and the tumor
damaging effects are thought to be the result of will receive the highest dose of energy. The normal
free-radical formation, many clinicians transfuse pa- tissue on the other side of the tumor will receive a high
tients as needed to maintain relatively normal hemo- radiation dose as the beam exits the body. Three-
globin concentrations in the blood in an effort to dimensional conformal radiation therapy allows the
ensure adequate oxygen delivery to the tumor during radiation therapy team to select beam shapes and
radiation therapy. angles that divide the total dose into multiple inter-
Just as some tumors are more radiosensitive than secting energy beams. Thus, the treatment high-energy
others, normal tissues vary in degree of radiosensitiv- dose can more precisely conform to the target volume
ity. As compared with hematopoietic stem cells, neu- while limiting the dose to normal tissue.21
rons are significantly less radiosensitive. This is clin- Intensity-Modulated Radiation Therapy (IMRT) is a
ically evident in patients receiving craniospinal relatively new approach that allows even greater
radiation for whom myelosuppression is more likely to precision of radiation delivery by modulating the
cause an interruption in radiation therapy than acute intensity of each beam with individual radio-opaque
radiation effects on the CNS. leaves. The individual leaves are moved in and out of
An acceptable therapeutic ratio can also be achieved the radiation field during treatment such that the
by targeted delivery of radiation.20 A main focus of energy beam can be sculpted to conform to irregular-
radiation therapy advances has been to more precisely shaped tumors within the body.19,21
deliver radiation to the tumor target. To repeatedly Radiosurgery utilizes multiple radiation beams all
deliver radiation to a limited target volume, methods converging on the same tumor target thereby deliver-
have been developed to place a patient in a reproduc- ing a single high-dose fraction of radiation to the
ible position over the days to weeks of therapy.19 For tumor. Radiosurgery is usually limited to use for small
younger pediatric patients, the positioning needed for treatment volumes.19,21
radiation administration can be so challenging that Proton Beam Therapy is particularly helpful in
anesthesia is frequently necessary. Essentially an im- limiting exposure of normal tissue. Unlike the photons
mobilization device such as a plastic facemask is or more standard RT, protons enter the body with a
customized for the patient. The mask is placed on the relatively low radiation dose and that energy is depos-
child and then attached to the treatment table in an ited in the tumor target with very little energy passing
effort to limit movement as much as possible. With through the target into surrounding tissue. Normal
technology that is designed to deliver radiation with tissues distal to the target are not irradiated.21,22
precision on the order of millimeters, patient move- Toxicity of radiation therapy is of particular concern
ment cannot be allowed. in pediatrics and can be characterized as acute and late
Radiation oncologists utilize MRIs, CT scans, and effects. Common acute effects include local skin
sophisticated computer systems in conjunction with reactions, anorexia, nausea, somnolence, focal alope-
medical physicists to define the target volume of the cia, mucositis (depending on radiation beam path),
radiation dose and determine the treatment plan to otitis, and myelosuppression (with spinal radiation).
deliver a given amount of radiation to the target Long-term effects are of even greater concern and
volume. The target volume includes the gross tumor include radionecrosis of normal tissue, vascular injury,
volume and surrounding tissue at risk for spread of bone growth stunting, endocrine abnormalities, hear-
Curr Probl Pediatr Adolesc Health Care, July 2005 233
ing loss, secondary malignancies, cognitive deficits, The range of intensity of chemotherapy regimens for
and neuropsychological effects.17,22,23 pediatric brain tumors is great. Some treatment plans
call for single-agent oral chemotherapy that is gener-
ally very well tolerated24; in other settings high-dose
Chemotherapeutic Approach to chemotherapy with stem cell rescue (autologous stem
Pediatric CNS Tumors cell transplant) is indicated.25 Despite the oncologist’s
Over the past several decades, chemotherapy has usual comfort in chemotherapy administration, the
gained increasing acceptance as an important thera- therapeutic index for chemotherapeutic agents is gen-
peutic approach for a variety of brain tumors. For erally small. Thus, while families are often willing to
patients with low-grade tumors, complete resection is “try anything” in desperate situations, physicians must
likely to be curative. However, when a complete be reminded to only provide rational therapy.
resection cannot be accomplished for low-grade tu- A variety of chemotherapy drugs are commonly used
mors, additional therapy must be considered. Like- in the treatment of pediatric brain tumors. In general,
wise, for high-grade lesions regardless of the extent of single-agent Phase I trials are utilized to show feasi-
resection adjuvant therapy must be considered as bility and perhaps some benefit in a specific tumor.
dissemination and recurrence after surgery alone are Over time agents with known benefit have been tried
likely. In general, the younger the patient, the more in combination. The most common chemotherapy
likely the late effects of RT will be devastating. agents for pediatric brain tumors will be detailed
The mainstay of brain tumor management in adults below. For a detailed review of chemotherapy agents
has been surgery and radiation with chemotherapy in used in pediatrics, see Balis and coworkers26 and
some cases. However, because of the effects of radi- Banerjee and Mathay27 from which the discussion
ation therapy (RT) on the developing brain, there has below is derived (see also Table 1). Combination
been a movement to try and avoid RT in children or at treatment plans will be reviewed later as they relate to
least delay RT administration until the patient is older. specific tumor types.
With advances in supportive care, chemotherapy can Vincristine is a commonly used drug in the manage-
be delivered more safely and with greater predictabil- ment of low-grade gliomas as well as high-grade and
ity of side effects thereby justifying attempts to incor- malignant brain tumors despite its limited documented
porate chemotherapy into a broader range of pediatric CNS penetration.28 Usually given as an intravenous
CNS tumor treatment plans. The goal is to improve push in combination with other agents, vincristine is
survival and decrease the morbidity of RT. Of course relatively well tolerated with the most common side
there is the added morbidity of the chemotherapy effects being constipation, jaw pain with administra-
itself. tion, and peripheral neuropathy which is usually re-
Though chemotherapy regimens may appear haphaz- versible and related to cumulative doses. Vincristine is
ard, they are generally designed to provide comple- a plant alkaloid that induces metaphase arrest through
mentary insults to the tumor while avoiding overlap- the binding of tubulin.26
ping dose-limiting toxicities. For example, the ideal Etoposide also binds tubulin and interacts with
multi-agent chemotherapy regimen would include topoisomerase II resulting in cell cycle arrest.26 Eto-
drugs that have different mechanisms of action in an poside is used intravenously in combination with
effort to avoid intrinsic or acquired tumor resistance. multiple agents to aggressively treat brain tumor
On the other hand, the toxicity profile must in some patients, but can also be prescribed orally in a more
ways be dissimilar so that the chemotherapy agents palliative setting with potential effect and acceptable
can be given contemporaneously. In other pediatric side effects. Common toxicities include nausea, my-
cancers such as acute lymphoblastic leukemia, multi- elosuppresion, and alopecia. Frequently the greatest
agent chemotherapy regimens have successfully re- concern with etoposide administration is the increased
sulted in impressive improvement in survival with risk of secondary malignancies.
acceptable morbidity. For a subset of brain tumors Cisplatin and carboplatin are alkylating agents used
multi-agent chemotherapy has proven successful, but for a variety of CNS tumors given as intravenous
for other brain tumors results have been equivocal or infusions. Cisplatin generally requires close manage-
proven to be unsuccessful (to be discussed below for ment of fluid and electrolyte balance and is more likely
the common pediatric brain tumors). to cause significant renal toxicity and hearing loss.
234 Curr Probl Pediatr Adolesc Health Care, July 2005
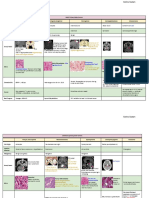
TABLE 1. Commonly used chemotherapeutic agents for the treatment of brain tumors
Chemotherapeutic agent Mechanism of action Tumors treated Side effects
Vincristine Induces metaphase arrest Low-grade gliomas as well as Constipation, jaw pain with
through the binding of high-grade and malignant administration, and
tubulin brain tumors peripheral neuropathy, which
is usually reversible and
related to cumulative doses
Etoposide Binds tubulin and interacts Malignant brain tumors Nausea, myelosuppression,
with topoisomerase II and alopecia; increased risk
resulting in cell-cycle arrest of secondary malignancies
Cisplatin, Carboplatin Alkylating agents Variety of CNS tumors Renal toxicity and hearing loss;
highly emetogenic
Cyclophosphamide Alkylating agent that inhibits High-grade or malignant brain Myelosuppression, nausea,
DNA synthesis tumors alopecia, hemorrhagic
cystitis, and impaired fertility
Nitrosureas: Alkylating agents Variety of CNS tumors Nausea and delayed
Lomustine (CCNU, given myelosuppression
orally), Carmustine (BCNU,
given IV)
Methotrexate Anti-metabolite; interferes with High grade or malignant brain Renal toxicity (high doses)
folate metabolism tumors Myelosuppression, neurological
sequelae, stomatitis, and
photosensitivity
Temozolomide Alkylating agent Low-grade as well as high-grade Nausea, constipation, and
pediatric brain tumors myelosuppression
Cisplatin is also one of the most emetogenic chemo- well tolerated but is known to cause nausea, constipa-
therapeutic agents used. The toxicity profile of carbo- tion, and myelosuppression.
platin is similar but usually less severe with respect to Tumor cells may have intrinsic resistance to a given
nausea, ototoxicity, and renal toxicity.27 Both plati- chemotherapy. That is, the tumor resists chemotherapy
num compounds are myelosuppressive. cell kill based on some inherent tumor biology. On the
Cyclophosphamide is an alkylating agent that inhib- other hand, a tumor may be relatively sensitive to a
its DNA synthesis. Cyclophosphamide is usually chemotherapeutic agent initially but resistance may be
given as an intravenous infusion for high-grade or acquired as tumor cells that are relatively less sensitive
malignant brain tumors.27 Common side effects in- survive. The concept of tumor resistance in brain
clude myelosuppression, nausea, and alopecia. Other tumors is similar to other pediatric neoplasms. Adju-
concerning side effects include hemorrhagic cystitis vant therapies are under development to obviate mech-
and impaired fertility. anisms of resistance. In other pediatric tumors, che-
The nitrosureas Lomustine (CCNU) and Carmustine motherapy dose intensification and multi-agent
(BCNU) are alkylating agents that are given orally and chemotherapy regimens have often improved overall
intravenously, respectfully.27 These agents have good survival, though the intensification of chemotherapy is
CNS penetration. The most common toxicities are at the expense of added iatrogenic toxicity.
nausea and delayed myelosuppression. The use of chemotherapy in CNS tumors has the
Methotrexate is an antifolate drug that causes de- added obstacle of the blood brain barrier (BBB),
creased DNA synthesis. It can be given by mouth, which under normal circumstances limits many large
intravenously, or intrathecally. Methotrexate has been molecules from leaving the peripheral bloodstream to
used recently to intensify therapy for pediatric patients penetrate the CNS. The BBB is conceptualized as tight
with high-grade or malignant brain tumors.29 Con- endothelial cell junctions that allow small lipophilic
cerning side effects are renal toxicity when given in molecules to permeate into the CNS while excluding
high doses. Myelosuppression is also possible as are large hydrophilic molecules.27 Thus, there is concern
neurological sequelae, stomatitis, and photosensitivity. that systemically administered chemotherapy may not
Temozolomide is a relatively new oral alkylating achieve optimal concentrations within the tumor.
agent that has been used for low-grade as well as Thus, CNS penetration of chemotherapy agents must
high-grade pediatric brain tumors.27 It is generally be considered when choosing among them. Despite
Curr Probl Pediatr Adolesc Health Care, July 2005 235
these theoretical concerns, it is thought that the pres- to improve the treatment of primary brain tumors in
ence of a CNS tumor partially disrupts the BBB children. The PBTC comprises 10 institutions with
allowing for even large water-soluble molecules to be extensive clinical experience and research focus on
effective chemotherapy agents. This is clinically evi- pediatric brain tumors. The PBTC’s main focus is on
dent in the uptake of gadolinium on MRI as well.27 novel therapeutic approaches. Other goals are devel-
Disruption of the BBB in an effort to enhance chemo- oping more accurate prognostic markers and neuroim-
therapy penetration into the CNS remains an area of aging techniques.
active research interest.
Family and Physician Resources
Clinical Trials There are many local resources and foundations for
children with cancer and specifically for children with
Great advances in the management of pediatric brain tumors. Family education is vital so that they
tumors have been realized largely from the participa- understand the rationale behind their child’s treatment
tion of patients and their care providers in clinical plan and the resources available to families of children
trials. The culture within pediatric oncology is one that with cancer. Centers with experience caring for chil-
expects enrollment of most patients on a treatment trial dren with cancer should facilitate contact for families
and a study of tumor biology. The majority of patients under their care. CureSearch (www.curesearch.org) is
eligible for an available clinical trial in the United the parent organization of the Children’s Oncology
States are enrolled in one. This is in sharp contrast to Group and the National Childhood Cancer Foundation
adult cancer patients who are not likely to be enrolled and can provide outstanding information for families
in a clinical trial. The relative rarity of pediatric and physicians alike. The Children’s Brain Tumor
tumors makes clinical trial participation through con- Foundation (www.cbtf.org) is another suggested re-
sortiums necessary as most single institutions will not source for families of children with brain tumors.
have enough pediatric tumor patients within a reason-
able time period to perform a clinical trial for a
specific disease. The Children’s Oncology Group
Etiology of Pediatric Brain Tumors
(COG) is an international consortium devoted to For the vast majority of CNS tumors in children, the
clinical and laboratory research for patients with etiology cannot be defined. Known risk factors include
pediatric tumors. Most tertiary care centers throughout high-dose therapeutic radiation (uncommonly a factor
the US that treat pediatric cancer patients are COG in pediatric patients) and genetic syndromes including
institutions and many nontertiary centers are affiliated neurofibromatosis type 1 and type 2, Li-Fraumeni
as well. syndrome, Turcot syndrome, Gorlin syndrome, tuber-
COG is divided by disease discipline and there are a ous sclerosis, and von Hippel-Lindau syndrome.30-32
number of clinical and biology trials available for Several environmental factors have been extensively
children with brain tumors. The goal of each COG studied but remain inconclusive. A common concern
subcommittee is to have an available clinical trial for of patients and their families is the risk of exposure to
each specific disease. As such there is presently cellular phone use, but at least two large studies failed
available a distinct clinical trial for medulloblastoma, to show an association between brain tumor develop-
high-grade gliomas, recurrent high-grade gliomas, ment and cellular phone use.33,34 Another common
ependymomas, low-grade gliomas, brain stem glio- concern is the effect of nonionizing electromagnetic
mas, and others. Enrollment in a given study is at the fields that can be emitted from power lines. This has
discretion of the treating oncologist and must be made been extensively studied and the data do not support a
with the full informed consent of a parent and the correlation between electromagnetic fields and brain
assent of older children. Patients may only be enrolled tumors.32,35,36
at COG institutions that have institutional IRB ap-
proval for the clinical trial to be offered.
According to their website (www.pbtc.org), The
Common Pediatric CNS Tumors
Pediatric Brain Tumor Consortium (PBTC) was The World Health Organization (WHO) classifica-
formed by the National Cancer Institute (NCI) in 1999 tion is the most widely accepted classification system
236 Curr Probl Pediatr Adolesc Health Care, July 2005
and is categorized by histological appearance37 (Table TABLE 2. Classification strategies for common pediatric brain tumors
by histology/tissue type: WHO classification
2). The WHO system classifies CNS tumors as tumors
Neuroepithelial tumors
of neuroepithelial tissue, tumors of peripheral nerves, Astrocytic
tumors of the meninges, lymphomas, and hematopoi- Low-grade astrocytoma
etic neoplasms, germ cell tumors, tumors of the sellar Anaplastic astrocytoma
Glioblastoma multiforme
region, and metastatic tumors. In the pediatric popu- Embryonal
lation tumors of neuroepithelial origin are by far the Medulloblastomas
most common and include astrocytic tumors, embry- Supratentorial primitive neuroectodermal tumors (PNETs)
Atypical teratoid/rhabdoid tumor
onal tumors, and ependymal tumors. The WHO clas- Ependymal
sification also includes tumor Grades I, II, III, and IV, Various subtypes of ependymomas
which indicate varying malignant potential with Grade
IV tumors having the greatest malignant potential.
Despite the WHO system, many tumors remain diffi- TABLE 3. Classification strategies for brain tumors by location: with
associated symptoms signs
cult to classify and neuropathology remains one of the Location Associated symptoms/signs
more challenging subspecialties within pathology with
Supratentorial Signs of increased intracranial pressure
regard to definitive diagnosis. Optic chiasm Visual field defects, visual loss, hormonal
While cumbersome, classification is important in Hypothalamic abnormalities, behavior changes
dictating treatment strategy and prognosis. Thus, fur- Pineal Abnormal eye movements
Hemispheric Focal neurologic signs, seizures
ther delineation of the more common pediatric tumors Infratentorial
is warranted. Astrocytic tumors include low-grade Cerebellar Gait abnormalities, ataxia
astrocytomas, anaplastic astrocytomas, and glioblas- Brain stem tumors Signs of increased intracranial pressure/
Medulloblastoma 4th ventricle obstruction/Cranial nerve
toma multiforme. Ependymal tumors include ependy- dysfunction
momas of various subtypes. Embryonal tumors in-
clude medulloblastomas and supratentorial primitive
neuroectodermal tumors (PNETs).
Many clinicians find it useful to classify CNS lesion approximately 20% of pediatric brain tumors, and
by location as well as tumor type38 (Table 3). Supra- ependymomas account for approximately 10%.30-32
tentorial tumors may present with symptoms or signs
that reflect their location. Tumors in proximity to the
optic chiasm or hypothalamus often present with
Low-Grade Gliomas
visual loss or visual field deficits, hormonal abnormal- Low-grade gliomas are the most common brain
ities, and behavioral changes. Tumors in the region of tumors in children accounting for just over half of all
the pineal gland can present with abnormalities of eye pediatric brain tumors. Within “low-grade gliomas”
movements. Hemispheric lesions can present with there are variations in histology, but in general treat-
focal neurologic signs or induce seizures. Supratento- ment decisions are made based on the general diagno-
rial tumors can also present with signs of increased sis of low-grade glioma rather than the subtype. For
ICP secondary to obstruction of flow of cerebrospinal example, children eligible for the most recent Chil-
fluid. Infratentorial tumors (cerebellar tumors, pilo- dren’s Oncology Group Protocol for low-grade glio-
cytic astrocytomas, medulloblastomas) can present mas included those with fibrillary, protoplasmic, and
with gait abnormalities, ataxia, and signs of increased mixed variants. Other types include pilocytic astrocy-
ICP as a result of obstruction of the fourth ventricle.39 tomas, pleomorphic xanthroastrocytomas, and sub-
The frequency of certain CNS tumor types in chil- ependymal giant cell astrocytomas.
dren is markedly distinct from that observed in adults Gross total resection is likely to cure a low-grade
in whom metastatic lesions and high-grade gliomas are glioma. Frequently complete resection is not possible.
much more common. Approximately half of all pedi- Following incomplete resection, the options are obser-
atric brain tumors are low-grade cerebellar astrocyto- vation alone with regularly scheduled MRIs or adju-
mas (gliomas). PNETs (of which medulloblastomas vant treatment. Some data suggest that low-grade
are a subset) are the most common malignant CNS gliomas may be stable or even regress following
tumors in pediatric patients and account for over 20% partial resection.40 As such, intervention is only nec-
of all pediatric brain tumors. Other gliomas represent essary if the patient is symptomatic or if the tumor is
Curr Probl Pediatr Adolesc Health Care, July 2005 237
located where even minimal increase in size could Diagnosis of medulloblastoma can be predicted by
have profound detrimental effect. Treatment is clearly radiographic appearance and location, but requires
indicated if there is tumor progression following histological confirmation. Given the tendency to
incomplete resection or recurrence. spread throughout the CNS, an MRI of the spine is
Children with neurofibromatosis Type 1 have an indicated to rule out “drop-metastases.” It is important
increased risk of developing CNS tumors, especially that the spine MRI be performed either before surgery
low-grade optic pathway gliomas. The natural pro- or 10 to 14 days after surgery as postoperative blood
gression of these tumors is not predictable and treat- products in the CNS may be confused with metastatic
ment can be deferred until there is clear progression or disease.42 Cytological evaluation of CSF is also part of
impending neurological compromise. Given the poten- the standard metastatic evaluation. Of note, CSF
tial added toxicity and increased risk of secondary obtained from a lumbar puncture more accurately
malignancies in patients with neurofibromatosis, RT is reflects the presence of CSF seeding than CSF ob-
avoided when possible for these patients. tained from ventricular sampling.43 Since medullo-
RT has been the standard therapy for progressive or blastomas only rarely metastasize outside the CNS,
recurrent low-grade gliomas. However, given the ef- extent of disease evaluation of bone and bone marrow
fects of RT on young children, chemotherapy is is not standard but must be considered if clinically
generally the first-line therapy for children under 10 indicated.
years of age. A recent Children’s Oncology Group Surgical resection is a cornerstone in management of
study (No. 9952) randomly compared two chemo- medulloblastoma; however, a gross total resection has
therapy plans. Regimen A utilized vincristine and not been shown to improve outcome compared with
carboplatin, while Regimen B included thioguanine, near total resection. Patients with residual tumor less
procarbazine, CCNU, and vincristine given for ap- than 1.5 cm2 have had the same outcome as those with
proximately 1 year or until progression. The results are no radiographically detected residual disease.44 Post-
not yet published regarding efficacy and safety. An- operative MRIs obtained more than 48 to 72 hours
other approach has been oral temozolomide, which after surgery may be difficult to interpret based on
provides ease of administration with promising poten- edema, gliosis, and residual blood product degrada-
tial tumor control.24 A new Phase I trial through the tion; as such, postoperative MRI should be obtained
COG incorporates vincristine, carboplatin, and temo- within 1 or 2 days after surgery to accurately assess the
zolomide (ACNS0126). amount of residual tumor.42
Patients with medulloblastoma can be stratified ac-
Medulloblastomas cording to age, stage, and risk group. Average risk
patients are those 3 years or older with less than 1.5
Medulloblastomas are the most common malignant cm2 of residual tumor and no evidence of dissemina-
CNS tumor in pediatrics. The peak incidence occurs in tion. High-risk patients are less than 3 years old or
children between 5 and 9 years old.30 Given the those with greater than 1.5 cm2 of residual tumor or
location of medulloblastomas in the posterior fossa, evidence of dissemination either by radiograph or by
the typical presenting signs are consistent with hydro- cytological analysis of CSF.
cephalus resulting from compression or invasion of the Treatment with surgery alone is not sufficient to
fourth ventricle. Other typical symptoms include irri- ensure durable remission. Standard approaches for
tability, decline in school performance, headache, children over 3 years old include surgery followed by
emesis, truncal ataxia, nystagmus, and cranial nerve radiation therapy to the posterior fossa and complete
palsies.30,41 The time course of symptoms is usually 2 neuraxis as well as combination chemotherapy. The
to 6 months before diagnosis.42 Medulloblastomas present Children’s Oncology Group clinical trial
present with distant spread of disease in approximately (ACNS0331) for standard risk medulloblastoma in
20% of patients and rarely can spread outside the children 3 to 7 years old seeks to determine if the total
CNS.41 A small percentage of patients with medullo- dose of craniospinal RT and the target volume to the
blastoma have a germline mutation such as one found primary tumor site can be reduced. Following surgery,
in Gorlin’s syndrome, Turcot’s syndrome, Li-Frau- patients are randomized to either standard-dose cra-
menmi syndrome, or ataxia telangiectasia, but for most niospinal RT (23.4 Gy) or reduced-dose craniospinal
patients the etiology is unknown.30,41,42 RT (18 Gy). Patients are then randomized to receive a
238 Curr Probl Pediatr Adolesc Health Care, July 2005
radiation boost to either the entire posterior fossa or a mens may allow RT to be deferred until the patient is
local boost to the tumor bed. During RT, patients older. So, while not curative, many believe the expo-
receive weekly vincristine. Following RT, patients sure to intensive chemotherapy is warranted.
receive chemotherapy including vincristine, CCNU,
Ependymomas
cisplatin, and cyclophosphamide. Children 8 years of
age and older receive standard craniospinal RT dosing, Ependymomas constitute approximately 9% of pe-
as the concern for RT toxicity is outweighed by the diatric CNS tumors and can arise throughout the CNS.
concern of distant recurrence in this older age group. Ependymal epithelium that lines the ventricles is
There is no standard approach for high-risk patients, thought to be the cell of origin for these tumors. The
but a common approach in young children with most common sites for ependymomas to occur are the
medulloblastoma is to utilize more intensive chemo- fourth, third, and lateral ventricles as well as the
therapy with myeloablative chemotherapy and autolo- lumbosacral spinal cord.48 The peak incidence occur-
gous stem cell rescue. This approach has been shown rence is children less than 6 years old and the great
to be feasible with an overall 3-year survival of 60%. majority are intracranial.49 Approximately 10% of
While this survival rate is not acceptable, it is encour- ependymomas occur in the spine, but there is an
aging that this survival rate was achieved with avoid- increased frequency of ependymomas of the spinal
ing or delaying RT in many patients.29 cord in patients with neurofibromatosis type II.30
The overall survival for all children with ependy-
High-Grade Gliomas
moma is between 50 and 60%.48 However, ependy-
Like “low-grade glioma,” “high-grade glioma” is a momas include a range of histologic variants ranging
general pathological description that encompasses from benign to anaplastic (WHO III) and prognosis is
anaplastic astrocytomas (WHO III), glioblastoma mul- dependent on histology as well as extent of resection.
tiforme (WHO IV), and the less common gliosarcoma. While ependymomas are responsive to chemotherapy,
High-grade gliomas account for approximately 15% of no study has shown that chemotherapy affects overall
pediatric CNS tumors and may arise throughout the survival. However, chemotherapy has been shown to
CNS.30 As a class of tumors, high-grade gliomas are allow for delayed RT in young patients with ependy-
relatively refractory to adjuvant therapy. The chance moma.50,51
of cure depends on the extent of resection. Patients For older children, standard therapy includes resec-
who undergo a resection of less than 90% of the tumor tion followed by focal RT.49,52 The current clinical
volume have significantly worse outcome than those trial available through the Children’s Oncology Group
who undergo a greater resection.45 Even following a (ACNS0121) takes into account extent of resection
gross total resection, recurrence is the rule. With the and ependymoma histology. Patients with differenti-
exception of the youngest patients, children with ated histology (that is, low malignant potential) who
high-grade gliomas receive RT even following a gross experience a gross total resection will not receive
total resection. Even those who undergo a gross total adjuvant therapy and will be followed with observa-
resection and receive adjuvant RT with or without tion alone. Patients with a gross total resection of an
chemotherapy have less than 50% 5-year survival rate. ependymoma with anaplastic (malignant) histology
The histology within high-grade gliomas is predictive will receive conformal RT as will patients with micro-
of outcome as described by WHO grade. That is, the scopic disease regardless of histology. Patients follow-
outcome for glioblastoma multiforme (WHO IV) is ing a subtotal resection regardless of histology will
worse than for anaplastic astrocytomas (WHO III).37 receive a trial of chemotherapy with vincristine, car-
The current standard therapeutic approach includes boplatin, cyclophosphamide, and etoposide with the
maximal surgical resection followed by conformal RT hope that response will make second surgery with a
to the area of the tumor with concurrent and mainte- complete resection possible. Patients then receive
nance oral temozolomide (Children’s Oncology Group conformal RT.
Trial ACNS0126). For children younger than 3 years
Craniopharyngiomas
old, multi-agent chemotherapy with or without my-
eloablative chemotherapy and autologous stem cell Craniopharyngiomas account for approximately 5%
rescue has been used with limited success unless a of all pediatric brain tumors with a peak incidence in
gross total resection was obtained.46,47 These regi- children between 5 and 14 years old. While benign in
Curr Probl Pediatr Adolesc Health Care, July 2005 239
that they do not disseminate, their local effect on the End of Therapy
optic pathway and pituitary can result in significant
visual and endocrine effects at presentation or follow- Even when treatment has been successful and well-
ing therapy.53 Diagnosis is based on MRI findings, but tolerated, the end of therapy is frequently anxiety-
CT scan is particularly helpful to distinguish cranio- provoking for the patient and family. Many have
pharyngiomas in children as 80% will have tumor- difficulty transferring from the active role of “doing
associated calcifications best seen on CT.53,54 something” to treat the tumor to the more passive role
Given the endocrine abnormalities associated with of observation. Patients must also adjust to the less
craniopharygiomas, it is helpful to involve a pediatric frequent reinforcement and support that they received
endocrinologist in the patient’s care soon after presen- during the more intense treatment period.
tation. Delayed endocrine defects may require pro- Just as anticipatory guidance is an important role for
longed management. the general pediatrician, anticipatory guidance from
Treatment of craniopharyngiomas remains contro- pediatric oncologists can help allay many fears and
versial, with limited evidence-based data from clinical ensure better follow-up. An open discussion about the
trials to support surgical resection versus radiation family’s feelings about the end of therapy is an
therapy. This is a polarizing issue without clear con- essential part of comprehensive and compassionate
sensus.53,55,56 Many believe that for older patients RT care.
In general, the tumor follow-up and surveillance
is the preferred modality and therefore reserve surgery
after completion of therapy is straightforward. Most of
for younger patients in an effort to avoid toxicity from
the time patients require follow-up MRIs at 3-month
RT. Chemotherapy has not been used with consistent
intervals for the first years with a gradual decrease in
success and in general is reserved for patients that
imaging frequency over the next few years until a
have multiple recurrences and that are not candidates
yearly follow-up MRI is adequate. It is important to
for further surgery or RT.
have the scans performed in a consistent manner so
that slight alterations in technique do not confound
Brain Stem Tumors interpretation. Many neuroradiologists prefer the scans
to be performed at their center under specific guide-
“Brain stem tumors” include diffuse intrinsic brain lines. For patients with residual MRI abnormalities or
stem gliomas, exophytic brain stem gliomas, and tectal enhancement, it is important to compare each new
gliomas. Intrinsic brain stem gliomas have a classic scan to a true baseline scan such as the first scan
radiographic appearance obviating the need for bi- performed at the end of therapy. Subtle changes
opsy. Brain stem gliomas can present with cranial between two subsequent scans may be more difficult
nerve abnormalities or upper motor neuron signs, such to appreciate than differences between each new scan
as contralateral hemiparesis, speech changes, stridor, and the true baseline scan.
and hyperreflexia.39 When a patient can be considered “cured” depends
Surgical excision is not possible because of the on the type of tumor. In general, the longer off therapy
tumor location. As such, RT and chemotherapy have without recurrence, the less likely recurrence will
been utilized with minimal success. The 2-year pro- happen. Nonetheless, a small chance of recurrence
gression-free survival remains less than 10% despite persists for several years after completion of therapy
RT intensification, chemotherapy intensification, and for most patients. Other important medical surveil-
combination therapy. The median time to progression lance includes serial endocrine surveillance, audio-
is generally 6 months and the median time to death is grams, and neuropsychological evaluation.
less than 1 year.25,57,58 For the patient, the return to routine activities can be
Patients that achieve a good initial response to very challenging. Most patients have prolonged school
steroids and RT may enjoy a window of neurological absences. The return to school can be very difficult
normalization, but almost all progress. New strategies especially when the patient has suffered physical,
are needed. The Children’s Oncology Group presently esthetic, cognitive, or emotional effects from the
has a trial incorporating oral Temozolomide with RT tumor or therapy. Some centers have child-life spe-
(ACNS0126) and a Phase I trial utilizing Motexafin- cialists that visit the school to meet with teachers or
Gadolinium as a radiosensitizer for involved field RT. even the patient’s classmates to help answer questions
240 Curr Probl Pediatr Adolesc Health Care, July 2005
about the student’s absence and return. Other physi- apy dose, and treatment volume, and presence of
cians prefer to contact the school principal, teacher, or hydrocephalus.60
nurse to discuss particular concerns regarding the There is a consensus that radiation to young children
patient. Of course such contact must be made with the is more likely to result in significant cognitive delay.
parent’s permission and preferably with the patient’s As discussed, studies have been directed at avoiding
knowledge. RT in young patients or at least delaying RT by up
Another transition is regarding medical care. For front chemotherapy in an effort to preserve intellectual
family convenience as well as medical concerns, outcome.61
pediatric oncologists sometimes serve as the general A recent study illustrated that survivors of medullo-
pediatrician for patients receiving therapy. After inten- blastoma demonstrated significantly less development
sive therapy, many patients’ families are unsure what of normal-appearing white matter (NAWM) volume
medical issues should be referred to their general than healthy controls. As NAWM volume is known to
pediatrician and what issues require involvement of be associated with neurocognitive test performance,
the oncologist. the authors suggest volumetric monitoring of brain
Following up with immunizations is another con- development to be used to guide the care of survivors
cern. During chemotherapy, few oncologists give rou- and assess clinical trial toxicity.62 Pediatric medullo-
tine vaccinations. The recommendation is to provide blastoma survivors also demonstrate abnormal hip-
seasonal influenza vaccination. Immediately after che- pocampal development following treatment.63
motherapy, the efficacy of vaccination is variable. Given the known neurocognitive effects of brain
Three to 6 months after immune-suppressive chemo- tumors and their management, comprehensive neuro-
therapy, patients should receive routine vaccinations psychological testing is indicated for years after treat-
again and vaccinations to catch up for those missed. ment. Many clinical trials provide clear guidelines
regarding the precise testing required. Multiple testing
tools are often needed to provide a comprehensive
Long-Term Follow-up analysis from specialized psychologists.64
Endocrine complications are another major concern
With the increasing success for pediatric oncology for pediatric brain tumor survivors. Tumor invasion
patients in general, there has been an enhanced aware- and surgical causes of endocrine dysfunction can
ness regarding issues of long-term follow-up. Some occur but studies suggest the risk of endocrine dys-
centers have clinic sessions devoted strictly to these function is increased by RT.65 The most frequent
patients. Most centers do not have dedicated clinics for endocrine abnormality secondary to lesions of the
long-term follow-up and rely on the oncologist to hypothalamic-pituitary area is growth hormone defi-
coordinate and oversee this aspect of care. While ciency.66 Growth hormone replacement in growth
recurrence is the most common cause of late death, hormone deficient brain tumor survivors has been
neurological, neurocognitive, and endocrine distur- shown to result in an overall greater final height in at
bances are prevalent disabilities among pediatric brain least one study.67
tumor long-term survivors.59 Pediatric brain tumor patients who receive RT for
Deficits may result from the tumor itself or as a posterior fossa tumors have been shown to have
consequence of surgery, RT, or chemotherapy. In diminished total body and lumbar spine bone mineral
general most consider RT the most detrimental factor density compared with the general population despite
in later cognitive development. Cognitive deficits are management of growth hormone deficiency and hypo-
most completely described among children surviving thyroidism.68 Hearing loss is not uncommon either
posterior fossa tumors (specifically medulloblastomas from cochlear exposure to RT or from cisplatin.42
and ependymomas). These patients tend to suffer As with other pediatric cancer patients, second
significant losses in IQ scores likely from an inability malignancies remain a concern for brain tumor survi-
to keep learning at a normal pace rather than from a vors. A recent study showed that the 15-year cumula-
loss of knowledge. Risk factors for a greater degree of tive incidence rate for malignant second neoplasms
IQ loss include younger age at time of treatment, (ie, not primary tumor recurrence) was 4%. While the
longer time since treatment, female sex, and clinical total number of patients with second malignancies was
variables such as exposure to radiotherapy, radiother- small, there was no clear difference in estimated
Curr Probl Pediatr Adolesc Health Care, July 2005 241
incidence of second malignancy among patients that child, it is important that patients feel they can trust
received different types of therapy.69 their doctor. It is likely that patients will conclude
what is going on or overhear conversations and then
learn that others are being deceptive.
Palliative Care Physicians have different approaches to these issues.
Some feel very strongly that patients of a certain age
For many brain tumor patients, palliation becomes must be told their prognosis. Other physicians will
the main goal of therapy. Often this transition from actively withhold or misrepresent information out of
cure-oriented care to palliative care is clear, but it may respect for the parents’ wishes. Other physicians
be quite subtle. respect parents’ wishes by agreeing not to proactively
The pediatric oncologist must consider the effect of provide details to the patient but allow the patient the
this transition on the wide range of people involved. opportunity to ask questions alone and with the par-
Usually the decision to pursue palliative care is made ents. Questions are answered truthfully in a way that is
with the patient’s parents. Parents may be resistant to appropriate for the child’s understanding and develop-
acknowledge that there is little or no hope for cure, but ment. This compromise acknowledges the parent’s
parents are usually thankful that they and their child authority and respects the patient’s autonomy. While
had the opportunity to make decisions based on the many in health care feel compelled to disclose every
reality of the disease. Parents who pursue very aggres- detail to a dying patient, others feel that patients will
sive therapy despite a very poor prognosis often regret ask what they want to know when they are ready to
subjecting their child to the difficulties of therapy. hear the likely answer.
However, many consider a worse regret would be to In addition to the patient and the patient’s parents,
think they had not “done everything.” the oncologist must consider the needs of the rest of
Physicians need to balance the hope of new drug the patient’s family. Grandparents must cope with the
trials and chemotherapy protocols with realistic expec- loss of their grandchild and the suffering of their
tations. Even for physicians and families that seek children. After experiencing major changes in family
novel or aggressive therapy, a conscious decision to dynamics, siblings must deal with their loss and
switch the goal of therapy is likely and appropriate at frequently experience survivor guilt.
some point. In most cases, there is time to have thoughtful
The goal of palliative care to most oncologists is to discussions with parents and patients about where they
provide the patient the best quality of life possible. want the patient to die. Some prefer the concept of
This concept is not mutually exclusive with providing having their child at home with coordinated home-
chemotherapy depending on the chemotherapy regi- hospice care. It is not uncommon even for these
men and expected toxicity. Some chemotherapy regi- families to request hospitalization as death becomes
mens are well-tolerated, easy to take, and may prolong clearly more imminent. There are limited inpatient
the period of time that the patient has good function. hospice facilities for children. Many parents prefer to
The intent, however, of palliative chemotherapy is not have their child die in the hospital at which s/he was
to cause tumor eradication, but to enhance the pa- treated where the staff is familiar and the parents have
tient’s quality of life. confidence that the patient will be well cared for.
Eventually, palliative chemotherapy becomes less Whether the patient is at home or in the hospital, it
appropriate in the view of most oncologists as the is important to discuss the parent’s and patient’s desire
patient’s physical and cognitive condition worsens. At regarding resuscitation. While a formal “Do Not Re-
this point, the goal of care is to provide comfort care suscitate” consent is not strictly required when resus-
and support to the patient and family. citation would be medically futile, most clinicians and
Except for the youngest patients, parents usually hospital staff prefer an open discussion with the
need guidance regarding how to discuss the changes in parents and patient when appropriate to clarify their
treatment with the patient. Most oncologists learn that wishes. This is particularly important for patients in
incorporating the patient in the discussion of treatment teaching hospitals so that house staff and nurses have
goals is appropriate. Of course this needs to be done in clear guidelines, and it is crucial for patients receiving
a developmentally sensitive manner. While parents hospice at home so that when the patient dies ambu-
frequently request withholding information from their lance staff has clear direction.
242 Curr Probl Pediatr Adolesc Health Care, July 2005
In general, malignancy is considered a contraindica- gram 1975-1995. Bethesda, MD: National Cancer Institute,
tion for organ donation.70 In some circumstances, eye SEER Program; NIH Publication No. 99-4649, 1999.
2. Reddy AT. Advances in biology and treatment of childhood
donation may be possible. While most clinicians have
brain tumors. Curr Neurol Neurosci Rep 2001;1(2):137-43.
difficulty raising this prospect with families, many 3. Gurney, JG, Kadan-Lottick, N. Brain and other central ner-
parents will be thankful for the opportunity. It is vous system tumors: rates, trends, and epidemiology. Curr
appropriate to check with the organ procurement Opin Oncol 2001;13(3):160-6.
center so that parents are given accurate information 4. Husstedt HW, Sickert M, Kostler H, et al. Diagnostic value of
and the topic is raised only when donation is possible. the fast-FLAIR sequence in MR imaging of intracranial
tumors. Eur Radiol 2000;10(5):745-52.
After a child’s death, health care providers must
5. Bryant SO, Cha S, Barkovich AJ. Modern Neuroimaging of
balance the need to continue to provide support to the Pediatric CNS Tumors. In: Gupta N, Banerjee A, Haas-Kogan
family with the family’s need for privacy. The correct D, editors. Pediatric CNS Tumors. Berlin Heidelberg:
balance can only be defined for each family. Many Springer-Verlag, 2004.
families are grateful when members of the health care 6. Chang YW, Yoon HK, Shin HJ, et al. MR imaging of
team attend funerals or make contact after the child’s glioblastoma in children: usefulness of diffusion/perfusion-
death. Other families prefer more distance. At a weighted MRI and MR spectroscopy. Pediatr Radiol 2003
Dec;33(12):836-42. Epub 2003 Oct 17.
minimum it is important that families know they are 7. Peet AC, Leach MO, Pinkerton CR, et al. The development of
welcome to call for help and support. The relationship functional imaging in the diagnosis, management and under-
does not end with the death of their child. standing of childhood brain tumours. Pediatr Blood Cancer
Finally, it is important to note the effect of a 2005;44(2):103-13.
patient’s death on colleagues and staff. While sea- 8. Hunter JV, Wang ZJ. MR spectroscopy in pediatric neurora-
soned oncologists may have developed a successful diology. Magn Reson Imaging Clin North Am 2001;9:165-89.
9. Preul MC, Leblanc R, Caramanos Z, et al. Magnetic
coping mechanism regarding patient death, the refer-
resonance spectroscopy guided brain tumor resection: dif-
ring pediatrician, junior colleagues, and staff may need ferentiation between recurrent glioma and radiation change
guidance and support. Many centers have regular in two diagnostically difficult cases. Can J Neurol Sci 1998
memorial services for their patients. Some centers Feb;25(1):13-22.
have structured discussions to provide an outlet for 10. Burtscher IM, Skagerberg G, Geijer B, et al. Proton MR
physicians, nurses, and other staff. Just as the health spectroscopy and preoperative diagnostic accuracy: an evalu-
ation of intracranial mass lesions characterized by stereotactic
care team looked to the lead physician for treatment
biopsy findings. AJNR Am J Neuroradiol 2000;21(1):84-93.
decisions, members of the team may look to the 11. Girard N, Wang ZJ, Erbetta A, et al. Prognostic value of
attending physician at the time of a patient’s death. protom MR spectroscopy of cerebral hemisphere tumors in
children. Neuroradiology 1998;40:121-5.
12. Pollack IF. The role of surgery in pediatric gliomas. J Neu-
Summary rooncol 1999;42(3):271-88.
13. Shaw EG, Wisoff JH. Prospective clinical trials of intracranial
Brain and spinal cord tumors represent the most low-grade glioma in adults and children. Neurooncology
common solid tumors in children. Recent advances in 2003;5(3):153-60.
imaging techniques, neurosurgical techniques, chemo- 14. Khan RB, Sanford RA, Kun LE, et al. Morbidity of second-
therapy approaches, and radiation oncology have re- look surgery in pediatric central nervous system tumors.
sulted in some improvement in overall survival and Pediatr Neurosurg 2001;35(5):225-9.
15. Gupta N, Perry V, Berger MS. Current surgical management.
morbidity. However, the prognosis for many children In: Gupta N, Banerjee A, Haas-Kogan D, editors. Pediatric
with high-grade and malignant brain tumors remains CNS Tumors. Berlin Heidelberg: Springer-Verlag; 2004.
guarded in terms of mortality and long-term sequelae. 16. Keles GE, Berger MS. Advances in neurosurgical technique in
Given the rarity of tumors in children, patients are the current management of brain tumors. Semin Oncol
likely best served at tertiary centers that can offer a 2004;31(5):659-65.
comprehensive multidiscipline approach. 17. Shiminski-Maher T, Cullen P, Sansalone M. Childhood Brain
and Spinal Cord Tumors: A Guide for Families, Friends and
Caregivers. Sebastopol, CA: O’Reilly & Associates, Inc.;
References 2002.
1. Gurney JG, Smith MA, Bunin GR. CNS and miscellaneous 18. Doxey D, Bruce D, Sklar F, et al. Posterior fossa syndrome:
intracranial and intraspinal neoplasms. In: Reis LAG, Sith identifiable risk factors and irreversible complications. Pediatr
MA, Gurney JG, et al, editors. Cancer Incidence and Survival Neurosurg 1999;31(3):131-6.
among Children and Adolescents: United States SEER Pro- 19. Haas-Kogan D, Frisch BM. Advances in radiation therapy. In:
Curr Probl Pediatr Adolesc Health Care, July 2005 243
Gupta N, Banerjee A, Haas-Kogan D, eds. Pediatric CNS 37. Gupta N, Haas-Kogan D, Banergee A. Introduction. In: Gupta
Tumors. Berlin Heidelberg: Springer-Verlag; 2004. N, Banerjee A, Haas-Kogan D, editors. Pediatric CNS Tu-
20. Kun LE. General principles of radiation therapy. In: Pizzo PA, mors. Berlin Heidelberg: Springer-Verlag; 2004.
Poplack DG, eds. Principles and Practice of Pediatric Oncol- 38. Pollack IF. Brain tumors in children. N Engl J Med
ogy. Philadelphia: Lippincott-Raven Publishers; 1997. 1994;331(22):1500-7.
21. Kirsch DG, Tarbell NJ. Conformal radiation therapy for 39. Ullrich NJ, Pomeroy SL: Pediatric brain tumors. Neurol Clin
childhood CNS tumors. Oncologist 2004;9(4):442-50. 2003 Nov;21(4)897-913. Review.
22. Duffner PK. Long-term effects of radiation therapy on cogni- 40. Wisoff J, Kernan JC, Horgan, MA, et al. Spontaneous invo-
tive and endocrine function in children with leukemia and lution of a diencephalic astrocytoma. Pediatr Neurosurg 1998;
brain tumors. Neurologist 2004;10(6):293-310. 29:149-53.
23. Donahue B. Short- and long-term complications of radiation 41. Packer RJ, Cogen P, Vezina G, et al. Medulloblastoma:
therapy for pediatric brain tumors. Pediatr Neurosurg clinical and biologic aspects. Neurooncology 1999;1:232-50.
1992;18:207-17. 42. Fisher PG. Embryonal tumors. In: Gupta N, Banerjee A,
24. Kuo JK, Weiner HL, Wisoff J, et al. Temozolomide is active Haas-Kogan D, editors. Pediatric CNS Tumors. Berlin
in childhood, progressive, unresectable, low-grade gliomas. Heidelberg: Springer-Verlag; 2004.
J Pediatr Hematol Oncol May 2003;25(5):372-8. 43. Gajjar AJ, Fouladi M, Walter A, et al. Comparison of lumbar
25. Wolff JE, Finlay JL. High-dose chemotherapy in childhood and shunt cerebrospinal fluid specimens for cytologic detec-
brain tumors. Onkologie 2004;27(3):239-45. tion of leptomeningeal disease in pediatric patients with brain
26. Balis FM, Holcenberg JS, Blaney S. General principles of tumors. J Clin Oncol 1999;17:1825-8.
chemotherapy. In: Pizzo PA, Poplack DG, eds. Principles and 44. Zeltzer PM, Boyett JM, Finlay JL, et al. Metastasis stage,
Practice of Pediatric Oncology. Philadelphia: Lippincott, Wil- adjuvant treatment, and residual tumor are prognostic factors
liams and Wilkins; 2000. for medulloblastoma in children: conclusions from the Chil-
27. Banerjee A, Mathay KK. Chemotherapy. In: Gupta N, Ban- dren’s Cancer Group 921 randomized phase II study. J Clin
erjee A, Haas-Kogan D, eds. Pediatric CNS Tumors. Berlin Oncol 1999;17:832-45.
Heidelberg: Springer-Verlag; 2004. 45. Wisoff JH, Boyett JM, Berger MS, et al. Current neurosurgical
28. Kellie SJ, Barbaric D, Koopmans P, et al. Cerebrospinal management and the impact of the extent of resection in the
fluid concentrations of vincristine after bolus intravenous treatment of malignant gliomas of childhood: a report of the
dosing: a surrogate marker of brain penetration. Cancer Children’s Oncology Group trial no. CCG-945. J Neurosurg
2002;94:1815-20. 1998;89:52-9.
29. Chi SN, Gardner SL, Levy AS, et al. Feasibility and response 46. Finlay JL, Goldman S, Wong MD, et al. Pilot study of high
to induction chemotherapy intensified with high-dose metho- dose thiotepa and etoposide with autologous bone marrow
trexate for young children with newly diagnosed high-risk rescue in children and young adults with recurrent CNS
disseminated medulloblastoma. J Clin Oncol 2004;22 tumors. The Children’s Oncology Group. J Clin Oncol
(24):4881-7. 1996;14:2495-503.
30. Gururangan S, Friedman HS. Recent advances in the treatment 47. Grovas AC, Boyett JM, Lindsley K, et al. Regimen-related
of pediatric brain tumors. Oncology Nov 2004;18(13): toxicity of myeloablative chemotherapy with BCNU, thiotepa,
1649-61. and etoposide followed by autologous stem cell rescue for
31. Strother DR, Pollack IF, Fisher PG, et al. Tumors of the children with newly diagnosed glioblastoma multiforme: re-
central nervous system: sequelae of treatment. In: Pizzo PA, port from the Children’s Cancer Group. Med Pediatr Oncol
Polack DG, eds. Principles and Practice of Pediatric Oncol- 1999;33:83-7.
ogy, 4th ed. Philadelphia: Lippincott, Williams and Wilkins; 48. Horn BN, Smyth M. Ependyma, in Gupta N, Banerjee A,
2002. p. 805-8. Haas-Kogan D, editors. Pediatric CNS Tumors. Berlin
32. Schuz J, Kaletsch U, Kaatsch P, et al. Risk factors for pediatric Heidelberg: Springer-Verlag; 2004.
tumors of the central nervous system: results from a German 49. Allen JC, Siffert J, Hukin J. Clinical manifestations of
population-based case-control study. Med Pediatr Oncol childhood ependymoma: a multitude of syndromes. Pediatr
2001;36(2):274-82. Neurosurg 1998;28:49-55.
33. Morgan RW, Kelsh MA, Zhao K, et al. Radiofrequency 50. Levy AS, Gardner S, Brady K, et al. Outcome for young
exposure and mortality from cancer of the brain and lymphat- children with ependymoma treated with intensive induction
ic/hematopoietic systems. Epidemiology 2000;11:118-27. chemotherapy followed by myeloablative consolidative che-
34. Inskip PD, Tarone RE, Hatch EE, et al. Cellular telephone use motherapy with autologous stem cell rescue: the Head Start
and brain tumors. N Engl J Med 2001;344:79-86. regimens (abstract 3232). Proc Am Soc Clin Oncol
35. Gurney JG, van Wijngaarden E. Extremely low frequency 2003;22:804.
electromagnetic fields (EMF) and brain cancer in adults and 51. Needle MN, Goldwein JW, Grass J, et al. Adjuvant chemo-
children: review and comment. Neurooncology 1999 therapy for the treatment of intracranial ependymoma of
Jul;1(3):212-20. childhood. Cancer 1997;80(2):341-7.
36. Portier CJ, Wolfe MS. Assessment of health effects from 52. Robertson PL, Zeltzer PM, Boyett JM, et al. Survival and
exposure to power-line frequency electric and magnetic fields: prognostic factors following radiation therapy and chemother-
NIEHS Working Group report. National Institute of Environ- apy for ependymomas in children: a report of the Children’s
mental Health Sciences; 1998; NIH Publication no. 98-3981. Cancer Group. J Neurosurg 88:695-703, 1998
244 Curr Probl Pediatr Adolesc Health Care, July 2005
53. Du R, Lustig RH, Fisch B, et al. Craniopharyngioma. In: matter volume development in children following craniospinal
Gupta N, Banerjee A, Haas-Kogan D, editors. Pediatric CNS irradiation. Neurooncology 2005;7(1):12-9.
Tumors. Berlin Heidelberg: Springer-Verlag; 2004. 63. Nagel BJ, Palmer SL, Reddick WE, et al. Abnormal hip-
54. Moore K, Couldwell WT. Craniopharyngioma. In: Bernstein pocampal development in children with medulloblastoma
M, Berger MS, editors. Neuro-Oncology: The Essentials. New treated with risk-adapted irradiation. AJNR Am J Neuroradiol
York: Thieme; 2000. 2004;25(9):1575-82.
55. Wisoff J. Surgical management of recurrent craniopharyngi- 64. Grill J, Kieffer V, Kalifa C. Measuring the neuro-cognitive
omas. Pediatr Neurosurg 1994;21(Suppl 1):108-13. side-effects of irradiation in children with brain tumors.
56. Tarbell NJ, Barnes P, Scott RM, et al. Advances in radiation Pediatr Blood Cancer 2004;42(5):452-6.
therapy for craniopharyngiomas. Pediatr Neurosurg 1994; 65. Anderson NE. Late complications in childhood central ner-
21(Suppl 1):101-7. vous system tumour survivors. Curr Opin Neurol 2003;
57. Packer RJ, Allen JC, Goldwein JL, et al. Hyperfractionated 16(6):677-83.
66. Brauner R, Adan L, Souberbielle JC. Hypothalamic-pituitary
radiotherapy for children with brainstem gliomas: a pilot study
function and growth in children with intracranial lesions.
using 7,200 cGy. Ann Neurol 1990;27:167-73.
Childs Nerv Syst 1999;15(11-12):662-9.
58. Mandell LR, Kadota R, Freeman C, et al. There is no role for
67. Gleeson HK, Stoeter R, Ogilvy-Stuart AL, et al. Improve-
hyperfractionated radiotherapy in the management of children
ments in final height over 25 years in growth hormone
with newly diagnosed diffuse intrinsic brainstem tumors:
(GH)-deficient childhood survivors of brain tumors receiving
results of a Pediatric Oncology Group phase III trial compar- GH replacement. J Clin Endocrinol Metab 2003;88(8):3682-9.
ing conventional vs. hyperfractionated radiotherapy. Int J 68. Krishnamoorthy P, Freeman C, Bernstein ML, et al. Osteope-
Radiat Oncol Biol Phys 1999;43:959-64. nia in children who have undergone posterior fossa or cranio-
59. Sklar CA. Childhood brain tumors. J Pediatr Endocrinol spinal irradiation for brain tumors. Arch Pediatr Adolesc Med
Metab 2002 May;15(Suppl 2):669-73. 2004;158(5):491-6.
60. Mulhern RK, Merchant TE, Gajjar A, et al. Late neurocogni- 69. Broniscer A, Ke W, Fuller CE, et al. Second neoplasms in
tive sequelae in survivors of brain tumours in childhood. pediatric patients with primary central nervous system tumors:
Lancet Oncol 2004;5(7):399-408. the St. Jude Children’s Research Hospital experience. Cancer
61. Lacaze E, Kieffer V, Streri A, et al. Neuropsychological 2004;100(10):2246-52.
outcome in children with optic pathway tumours when first- 70. Punnett AS, McMarthy LJ, Dirks PB, et al. Patients with
line treatment is chemotherapy. Br J Cancer 2003;89(11): primary brain tumors as organ donors: a case report and
2038-44. review of the literature. Pediatr Blood Cancer 2004;
62. Reddick WE, Glass JO, Palmer SL, et al. Atypical white 43(1):73-7.
Curr Probl Pediatr Adolesc Health Care, July 2005 245
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- SIOP22 - EPoster ViewingDocumento1.855 pagineSIOP22 - EPoster ViewingmgNessuna valutazione finora
- S974 Abstract Book ESTRO 2022: Variable N (%)Documento1 paginaS974 Abstract Book ESTRO 2022: Variable N (%)andresNessuna valutazione finora
- MedulloblastomaDocumento67 pagineMedulloblastomaAmira YasmineNessuna valutazione finora
- J Neurol Neurosurg Psychiatry 1999 Catsman Berrevoets 755 7Documento4 pagineJ Neurol Neurosurg Psychiatry 1999 Catsman Berrevoets 755 7Mihaela LitovcencoNessuna valutazione finora
- Cancer CellDocumento146 pagineCancer CellmanbastiNessuna valutazione finora
- Childhood Solid Tumors: For C-1 StudentsDocumento72 pagineChildhood Solid Tumors: For C-1 StudentsYemata HailuNessuna valutazione finora
- Brain Tumors - Current and Emerging Theraputic Strategies - A. Abujamra (Intech, 2011) WWDocumento432 pagineBrain Tumors - Current and Emerging Theraputic Strategies - A. Abujamra (Intech, 2011) WWKevinNessuna valutazione finora
- Pineal Guidelines PDFDocumento61 paginePineal Guidelines PDFWilliam LeeNessuna valutazione finora
- @ebookmedicinee2021 Hayat Tumors of The Central Nervous SystemDocumento132 pagine@ebookmedicinee2021 Hayat Tumors of The Central Nervous Systemvito100% (1)
- Central Nervous System Tumors: GeneralDocumento35 pagineCentral Nervous System Tumors: GeneralleartaNessuna valutazione finora
- Pediatric Brain TumorsDocumento19 paginePediatric Brain TumorsAngeline Pankaj TirkeyNessuna valutazione finora
- 39 MCQ's in NeurosurgeryDocumento26 pagine39 MCQ's in NeurosurgeryAhmed Hamid Ibrahim100% (4)
- MedulloblastomaDocumento35 pagineMedulloblastomatameemNessuna valutazione finora
- Cran Iectomy: Delayed Intracranial Hemorrhage in Children After SuboccipitalDocumento4 pagineCran Iectomy: Delayed Intracranial Hemorrhage in Children After SuboccipitalKhalvia KhairinNessuna valutazione finora
- Brain TumorsDocumento3 pagineBrain TumorsDrashty DesaiNessuna valutazione finora
- MedulloblastomaDocumento2 pagineMedulloblastomaMohammadAwitNessuna valutazione finora
- Brain Tumors - Classifications, Symptoms, Diagnosis and TreatmentsDocumento10 pagineBrain Tumors - Classifications, Symptoms, Diagnosis and TreatmentsshamimNessuna valutazione finora
- PertussisDocumento17 paginePertussischuckydoll1989Nessuna valutazione finora
- WHO Central Nervous System Tumor Classification PDFDocumento18 pagineWHO Central Nervous System Tumor Classification PDFAdli Wafi JabbarNessuna valutazione finora
- Brain and Spinal Tumors of ChildhoodDocumento560 pagineBrain and Spinal Tumors of ChildhoodmabidsaleemNessuna valutazione finora
- Pediatric Cancer v2 Teratoid Rhabdoid (UnitedVRG)Documento358 paginePediatric Cancer v2 Teratoid Rhabdoid (UnitedVRG)Andreea100% (1)
- Intracranial Tumors DeangelisDocumento419 pagineIntracranial Tumors DeangelisMuhammad Taufiq Regia ArnazNessuna valutazione finora
- Case PresentationDocumento31 pagineCase PresentationYogaPratayogaMNessuna valutazione finora
- AAP January 2022 Complete Issue Pediatrics in ReviewDocumento71 pagineAAP January 2022 Complete Issue Pediatrics in ReviewsureshNessuna valutazione finora
- FMGE LRR Pathology Part 1Documento62 pagineFMGE LRR Pathology Part 1Vishal KumarNessuna valutazione finora
- Brain Tumor in ChildrenDocumento42 pagineBrain Tumor in ChildrenKryztalGhail Llanora75% (4)
- Article OralDocumento36 pagineArticle Oralamina-fakirproNessuna valutazione finora
- Tumours of The Central Nervous System: FM Brett MD., FrcpathDocumento57 pagineTumours of The Central Nervous System: FM Brett MD., FrcpathDrGasnasNessuna valutazione finora
- Brain Tumors Children Cohen 2022Documento10 pagineBrain Tumors Children Cohen 2022Juan C. Salazar PajaresNessuna valutazione finora
- LRR NEET PG Pathology Part 1Documento82 pagineLRR NEET PG Pathology Part 1pdivyashreerajNessuna valutazione finora