Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
D Vitamin D Insufficiency - No Recommended Dietary Allowance Exists For This Nutrient COMMENTARY-VIETH, FRASER 11JUN02
Caricato da
ytreffalDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
D Vitamin D Insufficiency - No Recommended Dietary Allowance Exists For This Nutrient COMMENTARY-VIETH, FRASER 11JUN02
Caricato da
ytreffalCopyright:
Formati disponibili
Commentary
Commentaire
Vitamin D insufficiency: no recommended dietary
allowance exists for this nutrient
Reinhold Vieth, Donald Fraser
ß See related article page 1517
R
ickets, a defect in bone growth during infancy and designed to ensure anything. They are simply based on the
childhood, was first characterized in 1650. Al- old, default strategy for setting a nutritional guideline,
though cod-liver oil was used as a folk remedy in which is to recommend an amount of nutrient similar to
northern Europe starting in the late 1700s, it was not until what healthy people are eating. This approach underlies
1922 that the medical community realized that something the circular logic behind a familiar refrain about nutrition:
in it prevented and cured rickets.1,2 As recently as 4 decades “If you eat a good diet, you won’t need supplements.” By
ago, physicians assumed that vitamin D nutrition was ade- this logic, the answer to the question, “How much nutrient
quate if people exhibited no clinical or radiographic signs do you need?” is, “Whatever healthy people happen to be
of rickets.3,4 Osteomalacia, the adult counterpart of rickets, eating.” The essential point, lost in the confusing terminol-
was rarely seen, and it was assumed that adults require no ogy of modern nutrient recommendations, is that a recom-
more, and usually less, vitamin D than infants do.4 It was mended daily allowance (RDA) does not yet exist for vita-
also assumed that the vitamin D generated in the skin, vita- min D. Instead, the recommendations for it are referred to
min D3, was functionally equivalent to a different molecule, as “adequate intake” (AI).12,13 The AI for young adults (5 µg
vitamin D2, generated from lipids in yeast.3,4 or 200 IU) was chosen to approximate twice the average vi-
Physicians have been able to quantify vitamin D nutri- tamin D intake reported by 52 young women in a question-
tional status in their patients since the 1970s, by measuring naire-based study reported from Omaha, Neb., in 1997.13,14
the serum concentration of 25(OH)D. A low concentration Because the available evidence was acknowledged as weak,
of 25(OH)D causes a form of secondary hyperparathy- the Food and Nutrition Board of the US Institute of Medi-
roidism, which is thought to accelerate bone loss.5 Unfortu- cine called its recommendation an AI.13
nately, the practical advice about how to deal with vitamin The distinction between an RDA and an AI is impor-
D nutrition in adults has always been vague and, we think, tant. To qualify as an RDA, a dietary recommendation
misleading. must meet the known needs for the nutrient of practically
As part of the latest chapter in the history of vitamin D, all healthy people.15 This is an objective criterion which re-
Rucker and colleagues6 now report (page 1517) that a third of quires evidence that almost all adults taking the RDA
healthy Calgary men and women participating in the Canadian achieve a tangible health benefit or, alternatively, a target
Multicentre Osteoporosis Study (CaMos) had vitamin D insuf- blood level that would imply a health benefit. Thus, in con-
ficiency, defined as levels of 25-hydroxy vitamin D [25(OH)D] trast to the situation for an RDA, we are not safe in assum-
less than 40 nmol/L, during at least part of the year. From this ing that taking the AI for vitamin D will do anything at all.
and other reports,7–11 it is obvious that a lack of vitamin D is For vitamin D in particular, the traditional approach to
still common at northern latitudes. The mean age was about 64 nutrient recommendations is prone to gross error because
years. During the study, participants were asked to limit their in- most of us acquire far more of this “nutrient” through ex-
take of supplementary vitamin D to no more than 5 µg (200 posure to sunshine than we do from the diet.16 Before we
IU)/day.6 Recently, Atkinson and Ward12 reviewed the latest offi- can make any definitive statement about an RDA, we need
cial vitamin D intake recommendations in the CMAJ series on more precise knowledge of the total vitamin D supply in
clinical nutrition: 10 µg (400 IU)/day for those 51–70 years of age the body, its effects on serum concentrations of 25(OH)D
and 15 µg (600 IU)/day for those over 70 years of age. From and the associated effects on health.
these recommendations, one might conclude that if the CaMos Because of what was probably a misconception in recent
participants had taken the amount of supplement recommended years — that younger adults need less vitamin D than el-
for them (i.e., double or triple the 5 µg [200 IU]/day permitted derly people to bring about a given 25(OH)D concentration
by the study protocol), then vitamin D insufficiency would not — the Food and Nutrition Board in 1997 increased the AI
have occurred. However, this logic fails, because it assumes that only for elderly people. But even for this age group the
recommendations for supplemental vitamin D were designed to board went just part of the way, increasing the AI to only 15
ensure something specific, i.e. vitamin D adequacy. µg (600 IU) daily,13 which is less than the 20 µg (800 IU)
In fact, current recommendations for vitamin D are not needed in clinical trials (along with calcium) to prevent os-
CMAJ • JUNE 11, 2002; 166 (12) 1541
© 2002 Canadian Medical Association or its licensors
Commentaire
teoporotic fractures.17,18 Historically, 10 µg (400 IU) of vita- Toronto, Ont. Dr. Fraser is Professor Emeritus, Departments of Paediatrics and
Physiology, University of Toronto, and Honourary Physician, the Hospital for
min D was chosen for prophylaxis because it approximated Sick Children, Toronto, Ont. He was a member of the Committee on Nutrition,
the amount of vitamin D in a teaspoonful of cod-liver oil.3 American Academy of Pediatrics, the reports of which formed the basis of earlier
vitamin D recommendations for infants and adults.
All relevant studies in recent years have shown that the lat-
est adult AIs for vitamin D have been set much too low. For Competing interests: None declared.
example, an intervention study of Finnish adolescents19 and Contributors: Reinhold Vieth was the primary author of this commentary. Donald
Fraser was co-writer of the manuscript and provided additional perspectives.
2 cross-sectional studies8,10 showed that 10 µg (400 IU)/day
did not prevent wintertime insufficiency. Why should we
still expect this dose, originally used to prevent rickets in in- References
fants, to be appropriate for adults?
1. Harris LJ. Vitamin D and bone. In: Bourne GH, editor. The biochemistry and
Eventually, an RDA based on objective evidence will re- physiology of bone. New York: Academic Press; 1956. p. 581-622.
place the current guesstimated AI for vitamin D. One of us re- 2. Unraveling the enigma of vitamin D. In: Beyond discovery: the path from research
to human benefit series online. Washington: National Academy of Sciences;
cently showed that to ensure a serum 25(OH)D concentration 2000. Available: www.beyonddiscovery.org/content/view.article.asp?a=414 (ac-
of at least 40 nmol/L, Canadian adults require 25 µg (1000 IU) cessed 2002 Apr 23).
3. Park EA. The therapy of rickets. JAMA 1940;115(5):370-9.
of vitamin D3 per day.20 When the RDA for vitamin D is even- 4. Blumberg RW, Forbes GB, Fraser D, Hansen AE, Lowe CU, Smith NJ, et al.
tually established, it should be at that level — or greater. The prophylactic requirement and the toxicity of vitamin D. Pediatrics 1963;
We know that many consider vitamin D a toxic pariah 31:512-25.
5. Meunier P. Vitamin D insufficiency: reappraisal of its definition threshold and
among nutrients. However, toxicity has never been ob- bone consequences. In: Burckhardt P, Dawson-Hughes B, Heaney R, editors.
served in the physiologic amounts that can be derived from Nutritional aspects of osteoporosis. San Diego: Academic Press; 2001. p. 152-72.
6. Rucker D, Allan JA, Fick GH, Hanley DA. Vitamin D insufficiency in a pop-
sunshine — amounts associated with serum 25(OH)D con- ulation of healthy western Canadians. CMAJ 2002;166(12):1517-24. Avail-
centrations up to 235 nmol/L.16 To offer some perspective able: www.cmaj.ca/vol-166/issue-12/1517.html
7. Liu BA, Gordon M, Labranche JM, Murray TM, Vieth R, Shear NH. Sea-
here, an adult with white skin, exposed to summer sunshine sonal prevalence of vitamin D deficiency in institutionalized older adults. J
while wearing a bathing suit, generates about 250 µg Am Geriatr Soc 1997;45(5):598-603.
8. Vieth R, Cole DE, Hawker GA, Trang HM, Rubin LA. Wintertime vitamin
(10 000 IU) of vitamin D3 in 15 to 20 minutes; longer expo- D insufficiency is common in young Canadian women, and their vitamin D
sure generates no more vitamin D.16 That amount is equiva- intake does not prevent it. Eur J Clin Nutr 2001;55(12):1091-7.
9. Thomas MK, Lloyd-Jones DM, Thadhani RI, Shaw AC, Deraska DJ, Kitch
lent to the vitamin D3 in 25 conventional multivitamin pills BT, et al. Hypovitaminosis D in medical inpatients. N Engl J Med 1998;338
or 100 glasses of fortified milk. Long-term use of the official (12):777-83.
toxic dose, the “lowest observed adverse effect level,” 100 µg 10. Glerup H, Mikkelsen K, Poulsen L, Hass E, Overbeck S, Thomsen J, et al.
Commonly recommended daily intake of vitamin D is not sufficient if sun-
(4000 IU) of vitamin D3 per day, is in reality a physiologic light exposure is limited. J Intern Med 2000;247(2):260-8.
dose that has no effect on calcium levels in serum or urine.20 11. Gloth FM 3rd, Gundberg CM, Hollis BW, Haddad JG Jr, Tobin JD. Vita-
min D deficiency in homebound elderly persons. JAMA 1995;274(21):1683-6.
The vitamin D in the high doses available by prescrip- 12. Atkinson SA, Ward WE. Clinical nutrition: 2. The role of nutrition in the
tion (Ostoforte®, 50 000 IU/capsule) is not the same mole- prevention and treatment of adult osteoporosis. CMAJ 2001;165(11):1511-4.
Available: http://www.cmaj.ca/cgi/content/full/165/11/1511
cule that patients obtain “over the counter.” The physio- 13. Standing Committee on the Scientific Evaluation of Dietary Reference In-
logic, sun-derived product is vitamin D3 (cholecalciferol). takes. Dietary reference intakes: calcium, phosphorus, magnesium, vitamin D, and
fluoride. Washington: National Academy Press; 1997.
In Canada, multivitamins and milk almost always contain 14. Kinyamu HK, Gallagher JC, Balhorn KE, Petranick KM, Rafferty KA. Serum
vitamin D3. However, when a physician prescribes vitamin vitamin D metabolites and calcium absorption in normal young and elderly
D (the nutrient, not the hormone or its analogues) in free-living women and in women living in nursing homes [published erratum
appears in Am J Clin Nutr 1997;66[2]:454]. Am J Clin Nutr 1997;65(3):790-7.
North America, all the products available contain vitamin 15. Yates AA. Process and development of dietary reference intakes: basis, need, and
D2 (ergocalciferol), which is less effective than vitamin D3 at application of recommended dietary allowances. Nutr Rev 1998;56(4 Pt 2):S5-9.
16. Vieth R. Vitamin D supplementation, 25-hydroxyvitamin D concentrations,
increasing the serum 25(OH)D concentration.16 All iatro- and safety. Am J Clin Nutr 1999;69(5):842-56.
genic cases of vitamin D toxicity in the literature seen by us 17. Chapuy MC, Arlot ME, Duboeuf F, Brun J, Crouzet B, Arnaud S, et al. Vita-
min D3 and calcium to prevent hip fractures in the elderly women. N Engl J
have involved vitamin D2, a product not normally present Med 1992;327(23):1637-42.
in humans.16 Yes, poisonings have occurred with the physi- 18. Dawson-Hughes B, Harris SS, Krall EA, Dallal GE. Effect of calcium and vi-
tamin D supplementation on bone density in men and women 65 years of age
ologic molecule, vitamin D3, but all of those cases involved or older. N Engl J Med 1997;337(10):670-6.
intake on an “industrial scale,” with unintended, prolonged 19. Lehtonen-Veromaa M, Mottonen T, Irjala K, Karkkainen M, Lamberg-
Allardt C, Hakola P, et al. Vitamin D intake is low and hypovitaminosis D
daily consumption far beyond 1000 µg (> 40 000 IU).21 common in healthy 9- to 15-year old Finnish girls. Eur J Clin Nutr 1999;53
Until vitamin D is consumed by all adults in amounts (9):746-51.
much greater than is the case today, in accord with an 20. Vieth R, Chan PC, MacFarlane GD. Efficacy and safety of vitamin D(3) in-
take exceeding the lowest observed adverse effect level. Am J Clin Nutr 2001;
RDA that has not yet been established, many adults at 73(2):288-94.
northern latitudes will continue to exhibit undesirably low 21. Vieth R, Pinto T, Reen BS, Wong MM. Vitamin D poisoning by table sugar.
Lancet 2002;359:672.
concentrations of 25(OH)D.6–11 In the interim, we believe
that a daily supplement of 25 µg (1000 IU) of vitamin D3 is
advisable for all adults.
Correspondence to: Dr. Reinhold Vieth, Department of Pathology
Dr. Vieth is Associate Professor, Department of Laboratory Medicine and Patho-
and Laboratory Medicine, Mount Sinai Hospital, 600 University
biology, University of Toronto, and Director of the Bone and Mineral Laboratory, Ave., Toronto ON M5G 1X5; fax 416 586-8628;
Department of Pathology and Laboratory Medicine, Mount Sinai Hospital, rvieth@mtsinai.on.ca
1542 JAMC • 11 JUIN 2002; 166 (12)
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Fact Sheet On Vitamin DDocumento11 pagineFact Sheet On Vitamin DKerri Knox100% (4)
- D Symposium - Vitamin D Insufficiency - CALVO, WHITINGDocumento3 pagineD Symposium - Vitamin D Insufficiency - CALVO, WHITINGytreffalNessuna valutazione finora
- High-Dose Vitamin Therapy Stimulates Variant Enzymes With Decreased Coenzyme Binding AffinityDocumento43 pagineHigh-Dose Vitamin Therapy Stimulates Variant Enzymes With Decreased Coenzyme Binding AffinityytreffalNessuna valutazione finora
- Gamma-Tocopherol or Combinations of Vitamin E Forms Induce Cell Death in Human Prostate Cancer Cells. Jiang, Et Al., 2004.Documento6 pagineGamma-Tocopherol or Combinations of Vitamin E Forms Induce Cell Death in Human Prostate Cancer Cells. Jiang, Et Al., 2004.ytreffalNessuna valutazione finora
- Vitamin d10 2Documento18 pagineVitamin d10 2willianmeNessuna valutazione finora
- 6 - Vitamin D Requirements - Current and Future. WEAVER, FLEET AJCN DEC04Documento5 pagine6 - Vitamin D Requirements - Current and Future. WEAVER, FLEET AJCN DEC04ytreffalNessuna valutazione finora
- Engleza Vitamina D Beneficii Avantaje Si DezavantajeDocumento2 pagineEngleza Vitamina D Beneficii Avantaje Si DezavantajeLoredana LoreNessuna valutazione finora
- TELUGU - Life Skill ManualDocumento44 pagineTELUGU - Life Skill ManualChenna VijayNessuna valutazione finora
- Obat ObatDocumento8 pagineObat ObatMuhammad Aulia KurniawanNessuna valutazione finora
- Daftar Obat Untuk Formularium KlinikDocumento42 pagineDaftar Obat Untuk Formularium KlinikRianda LeeNessuna valutazione finora
- Jadwal Imsak Ramadan 1442-2021-Lamongan Maryam ArrowiDocumento5 pagineJadwal Imsak Ramadan 1442-2021-Lamongan Maryam Arrowisaiful ulumNessuna valutazione finora
- Harga Obat ApotikDocumento2 pagineHarga Obat ApotikRiska AmaliaNessuna valutazione finora
- hw499 - Unit 4 AssignmentDocumento10 paginehw499 - Unit 4 Assignmentapi-546774909Nessuna valutazione finora
- Vitamin Analysis by HPLC: Technical NoteDocumento4 pagineVitamin Analysis by HPLC: Technical NoteJuan PerezNessuna valutazione finora
- Vitamins For BSC Nursing Students (PHARMACOLOGY) - By: BINI P SAMUEL, ASSISTANT PROFESSORDocumento17 pagineVitamins For BSC Nursing Students (PHARMACOLOGY) - By: BINI P SAMUEL, ASSISTANT PROFESSORbinipsamuel25Nessuna valutazione finora
- Clasificator Medicamente 30.11.2016Documento1.038 pagineClasificator Medicamente 30.11.2016Cătălina GîlcaNessuna valutazione finora
- Every VitaminDocumento9 pagineEvery VitaminNur AlahiNessuna valutazione finora
- 07 Vitamins (Part 1)Documento48 pagine07 Vitamins (Part 1)NUR ANISAH MOHD ADNANNessuna valutazione finora
- Trade Name: Glucosamine/Chondroitin Softgels Concentration: Glucosamine Sulfate 500mg, Chondroitin Sulfate 400mgDocumento1 paginaTrade Name: Glucosamine/Chondroitin Softgels Concentration: Glucosamine Sulfate 500mg, Chondroitin Sulfate 400mgVitanut sasNessuna valutazione finora
- MS Protokol Nenad RosoDocumento2 pagineMS Protokol Nenad RosoМилош ЈовановићNessuna valutazione finora
- Fenanzamix Mineral Premix (Fish) : Analysis Per 1 KG of Product Content Actual Result UnitDocumento3 pagineFenanzamix Mineral Premix (Fish) : Analysis Per 1 KG of Product Content Actual Result UnitAnggaVaiNessuna valutazione finora
- Cannabinoid Boiling Points THC CBD - 0 PDFDocumento1 paginaCannabinoid Boiling Points THC CBD - 0 PDFmagiqoNessuna valutazione finora
- NovellDocumento6 pagineNovellEdwin JonatanNessuna valutazione finora
- Risks of Too Much Vitamin D3Documento6 pagineRisks of Too Much Vitamin D3Lorina BoligNessuna valutazione finora
- Chlorella Vulgaris Dan Spirulina PlatensisDocumento16 pagineChlorella Vulgaris Dan Spirulina PlatensisIrma RahmaNessuna valutazione finora
- Vitamin NotesDocumento3 pagineVitamin NotesKamran ZaheerNessuna valutazione finora
- Table 1 VeganDocumento2 pagineTable 1 Veganapi-524025751Nessuna valutazione finora
- Vitamin ClassificationDocumento6 pagineVitamin ClassificationAdrhien Ciane ManzanoNessuna valutazione finora
- The Suppliments GuideDocumento2 pagineThe Suppliments GuideIlyass AtNessuna valutazione finora
- SupplementsDocumento30 pagineSupplementsAwseome Vaibhav SahrawatNessuna valutazione finora
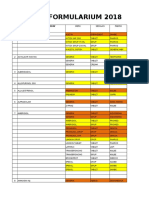
- Formularium Pengajuan 2018Documento44 pagineFormularium Pengajuan 2018Nuri IriyaniNessuna valutazione finora
- Green White Illustration Vegetables Healthy Balanced Diet PresentationDocumento11 pagineGreen White Illustration Vegetables Healthy Balanced Diet PresentationHubert Efrem-DonkorNessuna valutazione finora
- Template Nilai Gizi SusuDocumento8 pagineTemplate Nilai Gizi SusuRiena CemonkNessuna valutazione finora
- MultivitaminguideDocumento18 pagineMultivitaminguidestudboy100% (3)
- Vitamin and Nutritional RequirementDocumento158 pagineVitamin and Nutritional RequirementDerese BishawNessuna valutazione finora
- Blackmores - Apotek My PharmaDocumento12 pagineBlackmores - Apotek My PharmaApotek MyPharmaNessuna valutazione finora