Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Entamoeba Histolytica
Caricato da
Julia IshakTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Entamoeba Histolytica
Caricato da
Julia IshakCopyright:
Formati disponibili
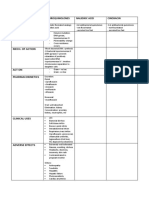
Aspect/ Entamoeba histolytica
Organism/
species
Causes disease .Amoebic desentery .Amebiasis
.Extraintestinal tissue invasion .Amebic hepatitis
Species
involved
Geo distribution .Cosmopolitan
Host Human
Habitat .Wall and lumen of colon
.Cecal and sigmoidorectal Regions
Human Contaminated food with cyst
Infection by / Portal of entry: Mouth
Mode of
infection
Morphology Trophozoite Precyst (trans)
Cyst --
Trophozoite .Wide, ectoplasm
.Thin fingerlike ectoplasmic pseupodia for movement and nutrition
.Endoplasm
..has RBCs in invasive stage
..single eccentric nucleus w central karyosome & fine peripheral chromatin granules
Precystic stage .Intermediate stage, no food inclusion
.Smaller than trophozoite, larger than cyst
Cyst .Rounded or oval, 10 – 20 µ in diameter
.Young cyst contains vacuoles w glycogen & Chromatoid bodies (RNA, DNA, represent stored food)
.Growing, dividing
.Immature cyst: single big nucleus
.Mature cyst: 4 nuclei
Reproduction / Excystation simple binary fission Encystation
Life cycle
Excystation .begins in cyst forms
.nucleus divides first
Encystation .in lumen of gut (lumen form only)
.essential for transmission
.only mature cyst is infective
Strains E.hartmanni
-small strain
-morphologically identical to E.histolytica
-Non-pathogenic
-Commensal in lumen of intestine
E. histolytica
-Has a commensal phase
Most of healthy carriers harbours minuta variety which changes into pathogenic form due to:
--lowered resistance
--bacterial & viral infections
--change of diet, etc..
Epidemiology .directly correlated w sanitary conditions (poor in tropical & subtropical areas)
.prevalent in ppl living under crowded conditions
.inadequate toilet & sanitary facilities (mental hospitals & migrant labour camps)
.generally poor socioeconomic circumstances
.male homosexuals (oral & anal intercourse)
Amoebic liver abscess, high in Mexico, India, Indonesia, some African countries
.Source of infection is cyst passing chronic patients or asymptomatic carriers
.transmission:
-water & vegetable contaminated w infective feces
-food contaminated by flies
-hands of infected food handlers
Pathology The lesion
-primarily intestinal
-secondarily extra-intestinal
Sites of 1º lesions
-wall of lumen of colon esp in cecal and sigmoidorectal regions (where colonic flow is slow)
Less frequently: ilio-cecal valve, ascending colon, rectim, sigmoid & hepatic flexures of transverse colon or appendix
.As infect progresses, additional sites of invasn develop
.Extraintestinal invasn (eg liver, etc) may occur in Px w clinical dysentery or in those w mild or latent infect
Pathologenic -resistance of host
xtvt depends -innate immunity
upon -state of nutritn
-freedom from infectious & debilitation d/s
-pathogenic & non-pathogenic strains + No of cysts
-condition in intestinal tract
mucosal injury
stasis
bacterial flora
carbohydrate diet
Complicatn Of intestinal amoebiasis (local)
.Appendicitis
.Intestinal perforation
.Amoeboma
.2º infect
Extra-intestinal
.Hepatic ameobiasis
-tissue forms reach the liver
-as emboli in portal circulatn
-direct extensn from amoebic ulcer in hepatic flexure of transverse colon
-Abscess may be single or multiple
-Abscess may become chronic
-Commonest site is dome of Rt lobe
.Pulmonary amoebiasis
.Amoebic brain abscess
Clinical Acute amoebic dysentery
manifestatn .onset is usually gradual w gripping abdominal pain, w or w/t tetesmus, may be preceded by an afibril diarrhea
.no of motion averages 4-8/day
.toxemic manifestatn – fever, anorexia, tachycardia
.dehydratn
.on palpation, abdominal tenderness
.differential dx = bacillary dysentery
Diagnosis A: Intestinal Amoebasiasis
1. Clinical picture
2. Stool examintn
-trophozoite in loose bloody stool
-cyst of 1 or 4 nuclei in normal stool
3. Sigmoidscopy
4. Barium enema
5. Stool culture
6. Serological dx
Treatment .Metronidazole (Flagyl)
.Emetine hydrochloride (alternative to [1])
Prevention .Tx of cases & carriers, examinant of contact
.sanitary sewage disposal & safe guarded water supply
.water may be boiled & ice should be made from boiling (if potable water is not available)
--trophozoites survive 5 hours at 37ºC
--killed by gastric acid juice
--cyst survive for 2 days at 37ºC
.Effect of chemicals
-Chlorice in concentratn used for water purification is not effective
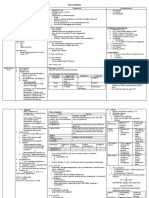
Genus and Species Entamoeba histolytica
Amoebiasis; Amoebic dysentery; Extraintestinal Amoebiasis, usually
Etiologic Agent of: Amoebic Liver Abscess = “anchovy sauce”); Amoeba Cutis; Amoebic
Lung Abscess (“liver-colored sputum”)
Infective stage Quadrinucleated cyst (having 4 nuclei)
Definitive Host Human
Portal of Entry Mouth
Mode of Transmission Ingestion of mature cyst through contaminated food or water
Habitat Colon and Cecum
Pathogenic Stage Trophozoite
Locomotive apparatus Pseudopodia (“False Foot”)
Motility Active, Progressive and Directional
'Ring and dot' appearance: peripheral chromatin and central
Nucleus
karyosome
Mode of Reproduction Binary Fission
Pathogenesis Lytic necrosis (it looks like “flask-shaped” holes in Gastrointestinal
tract sections (GIT)
Type of Encystment Protective and Reproductive
Most common is Direct Fecal Smear (DFS) and staining (but does not
allow identification to species level); Enzyme immunoassay (EIA);
Indirect Hemagglutination (IHA); Antigen detection – monoclonal
Lab Diagnosis
antibody; PCR for species identification. Sometimes only the use of a
fixative (formalin) is effective in detecting cysts. Culture: From faecal
samples - Robinson's medium, Jones' medium
Metronidazole for the invasive trophozoites PLUS a lumenal
amoebicide for those still in the intestine. Paromomycin (Humatin) is
the luminal drug of choice, since Diloxanide furoate (Furamide) is not
commercially available in the USA or Canada (only being available
from the Centers for Disease Control and Prevention). A direct
comparison of efficacy showed that Paromomycin had a higher cure
rate.[8] Paromomycin (Humatin) should be used with caution in
Treatment
patients with colitis as it is both nephrotoxic and ototoxic. Absorption
through the damaged wall of the intestinal tract can result in
permanent hearing loss and kidney damage. Recommended dosage:
Metronidazole 750 mg tid orally, for 5 to 10 days FOLLOWED BY
Paromomycin 30 mg/kg/day orally in 3 equal doses for 5 to 10 days or
Diloxanide furoate 500 mg tid orally for 10 days, to eradicate lumenal
amoebae and prevent relapse.[9]
Trophozoite Stage
Pathognomonic/Diagnostic
Ingested RBC; distinctive nucleus
Feature
Cyst Stage
Chromatoidal Body 'Cigar' shaped bodies (made up of crystalline ribosomes)
Number of Nuclei 1 in early stages, 4 when mature
Pathognomonic/Diagnostic
'Ring and dot' nucleus and chromatoid bodies
Feature
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- HistamineDocumento2 pagineHistamineJulia IshakNessuna valutazione finora
- Venum OrgDocumento3 pagineVenum OrgJulia IshakNessuna valutazione finora
- Aminoglycosides LadscapeDocumento2 pagineAminoglycosides LadscapeJulia IshakNessuna valutazione finora
- Antifolate DrugsDocumento2 pagineAntifolate DrugsJulia IshakNessuna valutazione finora
- Dna Gyrase InhibitorDocumento2 pagineDna Gyrase InhibitorJulia IshakNessuna valutazione finora
- ArthropodsDocumento2 pagineArthropodsJulia IshakNessuna valutazione finora
- AminoglycosidesDocumento2 pagineAminoglycosidesJulia IshakNessuna valutazione finora
- MB Gp2 PassDocumento1 paginaMB Gp2 PassJulia IshakNessuna valutazione finora
- Except in Viruses - May Be RNADocumento6 pagineExcept in Viruses - May Be RNAJulia IshakNessuna valutazione finora
- MB Rickettsiaceae PassDocumento2 pagineMB Rickettsiaceae PassJulia IshakNessuna valutazione finora
- MB GP 4 B& C PassDocumento3 pagineMB GP 4 B& C PassJulia IshakNessuna valutazione finora
- MB Spirochaete PassDocumento2 pagineMB Spirochaete PassJulia IshakNessuna valutazione finora
- Aureus C. Diphteriae (Man) : Classification Based On HaemolysisDocumento4 pagineAureus C. Diphteriae (Man) : Classification Based On HaemolysisJulia IshakNessuna valutazione finora
- ClostridiumDocumento1 paginaClostridiumJulia IshakNessuna valutazione finora
- MB Yeasts PassDocumento1 paginaMB Yeasts PassJulia IshakNessuna valutazione finora
- Bacterial MorphologyDocumento2 pagineBacterial MorphologyJulia IshakNessuna valutazione finora
- Subcutaneous MycosesDocumento1 paginaSubcutaneous MycosesJulia IshakNessuna valutazione finora
- Bacterial Virulence FactorsDocumento2 pagineBacterial Virulence FactorsJulia IshakNessuna valutazione finora
- Normal Body FloraDocumento1 paginaNormal Body FloraJulia IshakNessuna valutazione finora
- Intromycology& DermatophytesDocumento3 pagineIntromycology& DermatophytesJulia IshakNessuna valutazione finora
- Jirovecii: Kingdom: Phylum: Class: Order: Family: Genus: Species: PDocumento4 pagineJirovecii: Kingdom: Phylum: Class: Order: Family: Genus: Species: PJulia IshakNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Classification of Psychiatric DisordersDocumento64 pagineClassification of Psychiatric Disordersdrkadiyala2100% (1)
- Vestibular SchwannomaDocumento12 pagineVestibular SchwannomaEustakia Rini Kartika DewiNessuna valutazione finora
- 2020 11 07 XII Economics 1Documento17 pagine2020 11 07 XII Economics 1Sjft6hd FfNessuna valutazione finora
- Lecture 5 - Facial Pain and TMJ DiseaseDocumento6 pagineLecture 5 - Facial Pain and TMJ DiseaseJeff ChadwickNessuna valutazione finora
- Examinatin in Intensive CareDocumento731 pagineExaminatin in Intensive Careyankee1111100% (1)
- Cultivo Harknessia de EucaliptoDocumento18 pagineCultivo Harknessia de EucaliptoRosales Rosales JesúsNessuna valutazione finora
- Treatment of Sacroiliac Joint DysfunctionDocumento46 pagineTreatment of Sacroiliac Joint DysfunctionMichel Bakker100% (5)
- How The Brain Experiences ArchitectureDocumento16 pagineHow The Brain Experiences ArchitectureAbdu Thora100% (1)
- Jpog August 2013 IdDocumento51 pagineJpog August 2013 IdHasyim PurwadiNessuna valutazione finora
- Phlegmon: by - Dharmendra Singh Group No. - 317Documento15 paginePhlegmon: by - Dharmendra Singh Group No. - 317Mouna Jomaa DhifaouiNessuna valutazione finora
- Alkaloids - Biosynthesis Biological Roles and HealthDocumento285 pagineAlkaloids - Biosynthesis Biological Roles and HealthPrakash PatelNessuna valutazione finora
- Galvano-Spa-Bath and HealthDocumento2 pagineGalvano-Spa-Bath and HealthDeu na telha com Janaína BensdorpNessuna valutazione finora
- Other Products of ChesaDocumento4 pagineOther Products of ChesamikeeNessuna valutazione finora
- Cell DivisionDocumento28 pagineCell DivisionPalagiri MadhuNessuna valutazione finora
- SCHOOL NAME: - Proposed Date and Venue Materials Needed Budget Source Persons/ Offices Involved Expected OutcomesDocumento4 pagineSCHOOL NAME: - Proposed Date and Venue Materials Needed Budget Source Persons/ Offices Involved Expected OutcomesJOLLYBEL GAJWAYENNessuna valutazione finora
- Stroke:: What Should Nurses Need To Know About Stroke?Documento68 pagineStroke:: What Should Nurses Need To Know About Stroke?Suci Aning TNessuna valutazione finora
- Research Presentation Script I. Background of The Study & Introduction of Research TitleDocumento3 pagineResearch Presentation Script I. Background of The Study & Introduction of Research TitleSophia Adel RodriguezNessuna valutazione finora
- SaveBooklet BookletDocumento120 pagineSaveBooklet BookletRoscelie KhoNessuna valutazione finora
- National Medical National Medical Interns' Survey Interns' SurveyDocumento20 pagineNational Medical National Medical Interns' Survey Interns' SurveyKaren Jodes CapananNessuna valutazione finora
- Chapter 1 - A Context For CalculusDocumento7 pagineChapter 1 - A Context For Calculus0169514311Nessuna valutazione finora
- Atlas de AcupunturaDocumento258 pagineAtlas de AcupunturaPatricia Barrera100% (2)
- 2020 Article 773Documento10 pagine2020 Article 773bagas umam alwiNessuna valutazione finora
- Literature Review On Vegetable OilDocumento8 pagineLiterature Review On Vegetable Oilbteubwbnd100% (1)
- Trauma ToraksDocumento30 pagineTrauma ToraksMichael KwanNessuna valutazione finora
- 24.18.00 - Chikungunya2 DR RAGADocumento48 pagine24.18.00 - Chikungunya2 DR RAGAjcvh24Nessuna valutazione finora
- TRS601 Vocabulary ListDocumento5 pagineTRS601 Vocabulary ListNgo Van Hung (K17 HCM)Nessuna valutazione finora
- 3b Oral Exam Practice - Mock Exam THREE - ANSWER Guide PDFDocumento7 pagine3b Oral Exam Practice - Mock Exam THREE - ANSWER Guide PDFJyothsna SridharNessuna valutazione finora
- Giles B1Documento37 pagineGiles B1imgayNessuna valutazione finora
- Fix Daftar PustakaDocumento6 pagineFix Daftar Pustakaeka saptaning windu fitriNessuna valutazione finora
- EO 70 S. 2021 - Movement of Pigs and Pork Products ASF-DSDocumento8 pagineEO 70 S. 2021 - Movement of Pigs and Pork Products ASF-DSJamela SerutNessuna valutazione finora