Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Blood Sir Cristino
Caricato da
Andrei Borata0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
7 visualizzazioni12 pagineTitolo originale
Blood-Sir-Cristino
Copyright
© © All Rights Reserved
Formati disponibili
DOCX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
7 visualizzazioni12 pagineBlood Sir Cristino
Caricato da
Andrei BorataCopyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 12
Fluids and Transport 3.
Restriction of fluid losses at injury
sites
Blood
4. Defense against toxins and
What are the components of the
pathogens
cardiovascular system, and their major
functions? 5. Stabilization of body temperature
The Cardiovascular System Whole Blood
A circulating transport system: Plasma:
– Is similar to, and exchanges
– a pump (the heart)
fluids with, interstitial fluid
– a conducting system (blood – Is matrix of formed elements
vessels) Formed elements:
– 3 Types of Formed
– a fluid medium (blood)
Elements:
Functions of the Cardiovascular System: a. Red blood cells
(RBCs) or
To transport materials to and from erythrocytes
cells: - transport
– oxygen and carbon dioxide oxygen
b. White blood cells
– nutrients (WBCs) or
– hormones leukocytes
- part of the
– immune system components immune
– waste products system
c. Platelets
- cell fragments
What are the important components and involved in
major functions of blood? clotting
Water
Blood Dissolved plasma proteins
– Is specialized fluid of connective Other solutes
tissue Hemopoiesis
– Contains cells suspended in a fluid
matrix – Process of producing formed
elements
5 Functions of Blood: – By myeloid and lymphoid stem cells
1. Transport of dissolved substances Fractionation
2. Regulation of pH and ions – Process of separating whole blood
for clinical analysis:
– into plasma and formed elements Globulins (35%)
Fibrinogen (4%)
3 General Characteristics of Blood
Albumins
38°C (100.4°F) is normal
temperature Transport substances:
High viscosity
– fatty acids
Slightly alkaline pH (7.35–7.45)
– thyroid hormones
Blood Volume
– steroid hormones
Blood volume (liters) = 7% of body
weight (kilograms): Globulins
– adult male: 5 to 6 liters 1. Antibodies, also called
immunoglobulins
– adult female: 4 to 5 liters
2. Transport globulins (small
molecules):
What is the composition and function of
– hormone-binding proteins
plasma?
– metalloproteins
Plasma
– Makes up 50–60% of blood – apolipoproteins (lipoproteins)
volume
– steroid-binding proteins
– More than 90% of plasma is
water Fibrinogen
Extracellular Fluids
– Molecules form clots
– Interstitial fluid (IF) and
– Produce long, insoluble strands of
plasma
fibrin
– Materials plasma and IF
exchange across capillary Serum
walls:
Liquid part of a blood sample:
Water
Ions – in which dissolved fibrinogen
Small solutes has converted to solid fibrin
Differences between Plasma and IF: Other Plasma Proteins
1. Levels of O2 and CO2 1% of plasma:
2. Dissolved proteins: – changing quantities of
specialized plasma proteins
plasma proteins do not pass
through capillary walls – enzymes, hormones, and
prohormones
3 Classes of Plasma Proteins:
Origins of Plasma Proteins
Albumins (60%)
– 90% made in liver – female: 3 – 47
– Antibodies made by plasma cells
RBC Structure
– Peptide hormones made by
endocrine organs Small and highly specialized disc
Fun Fact: Thin in middle and thicker at edge
Total blood volume (liters) = 7% of Importance of RBC Shape and Size
body weight (kilograms)
About 1/2 the volume of whole 1. High surface-to-volume ratio:
blood is cells and cell products quickly absorbs and releases
Plasma resembles interstitial fluid, oxygen
but contains a unique mixture of 2. Discs form stacks:
proteins not found in other
extracellular fluids – smoothes flow through
narrow blood vessels
3. Discs bend and flex entering small
What are the characteristics and capillaries:
functions of red blood cells?
– 7.8 µm RBC passes through 4
Red Blood Cells µm capillary
Red blood cells (RBCs) make up Lifespan of RBCs
99.9% of blood’s formed elements
Lack nuclei, mitochondria, and
Measuring RBCs ribosomes
Red blood cell count: Live about 120 days
– reports the number of RBCs
in 1 microliter whole blood What is the structure and function of
hemoglobin?
Hematocrit (packed cell volume,
PCV): Hemoglobin (Hb)
– percentage of RBCs in Protein molecule, transports
centrifuged whole blood respiratory gases
Normal Blood Counts: Normal hemoglobin (adult male):
14 – 18 g/dl whole blood
RBC:
Hemoglobin Structure
male: 4.5 – 6.3 million
Complex quaternary structure
– female: 4.0 – 5.5 million 4 globular protein subunits:
Hematocrit: each with 1 molecule of heme
– male: 4 – 52 each heme contains 1 iron ion
Iron ions easily: Diagnosing Disorders
associate with oxygen
Hemoglobinuria:
(oxyhemoglobin)
– hemoglobin breakdown
dissociate from oxygen
products in urine due to
(deoxyhemoglobin)
excess hemolysis in blood
Fetal Hemoglobin stream
Hematuria:
Strong form of hemoglobin found in – whole red blood cells in urine
embryos. due to kidney or tissue
Takes oxygen from mother’s damage
hemoglobin.
Hemoglobin Recycling
Carbaminohemoglobin
Phagocytes break hemoglobin into
With low oxygen (peripheral components:
capillaries): globular proteins to amino
hemoglobin releases oxygen acids
binds carbon dioxide and heme to biliverdin
carries it to lungs iron
Anemia Iron Recycling
Hematocrit or hemoglobin levels are To transport proteins (transferrin)
below normal
To storage proteins (feritin and
Is caused by several conditions hemosiderin)
Breakdown of Biliverdin
How are the components of old or Biliverdin (green) is converted to
damaged red blood cells recycled?
bilirubin (yellow)
Recycling RBCs Bilirubin is:
excreted by liver (bile)
1% of circulating RBCs wear out per
jaundice is caused by
day:
bilirubin buildup
about 3 million RBCs per
converted by intestinal
second
bacteria to urobilins and
Macrophages of liver, spleen, and
stercobilins which account
bone marrow: for the yellow brown to
monitor RBCs brown color of stool.
engulf RBCs before
membranes rupture
(hemolyze)
Mature RBC
What is erythropoiesis? What are the Components
stages of red blood cell maturation,
Building red blood cells requires:
and how is red blood cell production
regulated? amino acids
iron
Erythropoiesis vitamins B12, B6, and folic
Red blood cell formation acid
Occurs only in red bone marrow Pernicious Anemia
(myeloid tissue)
Stem cells mature to become RBCs Low RBC production
Due to unavailability of vitamin B12
Hemocytoblasts (remember the intrinsic factor
produced by the parietal cells in the
Stem cells in bone marrow divide to
gastric glands of the stomach, which
produce:
is needed to absorb vitamin B12)
myeloid stem cells:
become RBCs, some Stimulating Hormones
WBCs
lymphoid stem cells: Erythropoietin (EPO)
become lymphocytes Also called erythropoiesis-
stimulating hormone:
Stages of RBC Maturation secreted when oxygen in
Myeloid stem cell peripheral tissues is low
(hypoxia)
due to disease or high altitude
Fun Facts:
Proerythroblast Red blood cells (RBCs) are the most
numerous cells in the body
RBCs circulate for approximately 4
months before recycling
Several million are produced each
Erythroblasts second
Hemoglobin in RBCs transports:
– oxygen from lungs to
peripheral tissues
Reticulocyte – carbon dioxide from tissues
to lungs
What is blood typing, and why is it
important? What is the basis for ABO
The Rh Factor
and Rh incompatibilities?
– Also called D antigen
Surface Antigens
– Either Rh positive (Rh+) or Rh
Are cell surface proteins that identify negative (Rh—)
cells to immune system. – Only sensitized Rh— blood has anti-
Normal cells are ignored and foreign Rh antibodies
cells attacked.
Cross-Reaction
Blood Types
– Also called transfusion reaction
Are genetically determined – Plasma antibody meets its specific
By presence or absence of RBC surface antigen
surface antigens A, B, Rh – Blood will agglutinate and hemolyze
– If donor and recipient blood types
4 Basic Blood Types: not compatible
A (surface antigen A) Blood Type Test
B (surface antigen B)
– Determines blood type and
AB (antigens A and B)
compatibility
(neither A nor B)
Cross-Match Test
Agglutinogens
– Performed on donor and recipient
Antigens on surface of RBCs
blood for compatibility
Screened by immune system – Without cross-match, type O— is
Plasma antibodies attack universal donor
(agglutinate) foreign antigens
Blood Plasma Antibodies
Based on structures and functions, what
Type A: are the types of white blood cells, and
type B antibodies what factors regulate the production of
Type B: each type?
– type A antibodies White Blood Cells (WBCs)
Type AB: – Also called leukocytes
neither A nor B – Do not have hemoglobin
Type O: – Have nuclei and other organelles
– both A and B antibodies WBC Functions:
Defend against pathogens
Remove toxins and wastes
Attack abnormal cells
WBC Movement – Pale cytoplasm granules with:
lysosomal enzymes
– Most WBCs in:
bactericides (hydrogen
connective tissue proper peroxide and superoxide)
lymphatic system organs
Neutrophil Action
– Small numbers in blood:
– Very active, first to attack bacteria
6000 to 9000 per microliter – Engulf pathogens
– Digest pathogens
Circulating WBCs – Release prostaglandins and
1. Migrate out of bloodstream leukotrienes
2. Have amoeboid movement – Form pus
3. Attracted to chemical stimuli Degranulation
(positive chemotaxis)
4. Some are phagocytic: – Removing granules from cytoplasm
– neutrophils, eosinophils, and – Defensins:
monocytes peptides from lysosomes
attack pathogen membranes
Types of WBCs:
Eosinophils
– Also called acidophils
– 2–4% of circulating WBCs
– Attack large parasites
– Excrete toxic compounds:
nitric oxide
cytotoxic enzymes
Eosinophil Actions
Types of WBCs: – Are sensitive to allergens
– Control inflammation with enzymes
Neutrophils that counteract inflammatory effects
Eosinophils of neutrophils and mast cells
Basophils
Basophils
Monocytes
Lymphocytes – Are less than 1% of circulating
WBCs
– Are small
Neutrophils – Accumulate in damaged tissue
– Also called polymorphonuclear
leukocytes
– 50–70% of circulating WBCs
Basophil Actions Natural Killer Cells (NK)
Detect and destroy abnormal
– Release histamine:
tissue cells (cancers)
dilates blood vessels
– Release heparin: The Differential Count of Circulating
prevents blood clotting WBCs
Monocytes – Detects changes in WBC populations
– Infections, inflammation, and
– 2–8% of circulating WBCs
allergic reactions
– Are large and spherical
– Enter peripheral tissues and become WBC Disorders
macrophages
Leukopenia
Macrophage Actions abnormally low WBC count
– Engulf large particles and pathogens Leukocytosis
– Secrete substances that attract abnormally high WBC count
immune system cells and fibroblasts Leukemia
to injured area extremely high WBC count
Lymphocytes Fun Fact:
– 20–30% of circulating WBCs RBCs outnumber WBCs 1000:1
– Are larger than RBCs WBCs defend against infection,
– Migrate in and out of blood foreign cells, or toxins
– Mostly in connective tissues and WBCs clean up and repair damaged
lymphatic organs tissues
The most numerous WBCs:
Lymphocyte Actions
o neutrophils
– Are part of the body’s specific – engulf bacteria
defense system o lymphocytes
3 Classes of Lymphocytes: – are responsible for
specific defenses of
T cells immune response
Cell-mediated immunity
WBC Production
Attack foreign cells directly
B cells – All blood cells originate from
Humoral immunity hemocytoblasts:
Differentiate into plasma which produce myeloid stem
cells (activated B cells that cells and lymphoid stem cells
secrete antibodies).
Synthesize antibodies
Myeloid Stem Cells
4. Multi-CSF:
– Differentiate into progenitor cells: – accelerates production
which produce all WBCs of granulocytes,
except lymphocytes monocytes, platelets,
and RBCs
Lymphocytes
– Are produced by lymphoid stem cells What is the structure and function of
– Lymphopoiesis: platelets, and how are they produced?
the production of
lymphocytes Platelets
WBC Development – Cell fragments involved in human
clotting system
WBCs, except monocytes: – Nonmammalian vertebrates have
– develop fully in bone marrow thrombocytes (nucleated cells)
Monocytes:
– develop into macrophages in Platelet Circulation
peripheral tissues – Circulates for 9–12 days
Other Lymphopoiesis – Are removed by spleen
– 2/3 are reserved for emergencies
– Some lymphoid stem cells migrate to
peripheral lymphoid tissues (thymus, Platelet Counts
spleen, lymph nodes) – 150,000 to 500,000 per microliter
– Also produce lymphocytes Thrombocytopenia:
4 Colony-Stimulating Factors (CSFs) – abnormally low platelet count
Thrombocytosis:
– Hormones that regulate blood cell – abnormally high platelet
populations: count
1. M-CSF:
– stimulates monocyte Functions of Platelets:
production Release important clotting chemicals
2. G-CSF:
Temporarily patch damaged vessel
– stimulates granulocyte
walls
production
Actively contract tissue after clot
– neutrophils,
formation
eosinophils, and
basophils Platelet Production
3. GM-CSF:
– stimulates granulocyte – Also called thrombocytopoiesis:
and monocyte occurs in bone marrow
production
Megakaryocytes The Platelet Phase
– Giant cells – Begins within 15 seconds after injury
– Manufacture platelets from
2 Steps of the Platelet Phase
cytoplasm
1. Platelet adhesion (attachment):
Hormonal Controls
– to sticky endothelial surfaces
Thrombopoietin (TPO) – to basal laminae
Inteleukin-6 (IL-6) – to exposed collagen fibers
Multi-CSF 2. Platelet aggregation (stick
together):
– forms platelet plug
What mechanisms control blood loss after – closes small breaks
injury, and what is the reaction sequence Activated Platelets Release Clotting
in blood clotting? Compounds
Hemostasis Adenosine diphosphate (ADP)
– The cessation of bleeding: Thromboxane A2 and serotonin
vascular phase Clotting factors
platelet phase Platelet-derived growth factor
coagulation phase (PDGF)
Calcium ions
The Vascular Phase
Platelet Plug: Size Restriction (1 of 2)
– A cut triggers vascular spasm
– 30-minute contraction Prostacyclin:
– released by endothelial cells
3 Steps of the Vascular Phase – inhibits platelet aggregation
1. Endothelial cells contract: Inhibitory compounds:
– expose basal lamina to – released by other white blood
bloodstream cells
2. Endothelial cells release:
The Coagulation Phase
– chemical factors:
ADP, tissue factor, – Begins 30 seconds or more after the
and prostacyclin injury
– local hormones: – Blood clotting (coagulation):
endothelins Involves a series of steps
– stimulate smooth muscle converts circulating
contraction and cell division fibrinogen into insoluble
3. Endothelial cell membranes become fibrin
“sticky”:
– seal off blood flow
Blood Clot The Extrinsic Pathway
– Fibrin network – Damaged cells release tissue factor
– Covers platelet plug (TF)
– Traps blood cells – TF + other compounds = enzyme
– Seals off area complex
– Activates Factor X
Clotting Factors
The Intrinsic Pathway
– Also called procoagulants
– Proteins or ions in plasma – Activation of enzymes by collagen
– Required for normal clotting – Platelets release factors (e.g., PF–3)
– Series of reactions activate Factor X
Plasma Clotting Factors
The Common Pathway
– Enzymes activate Factor X
– Forms enzyme prothrombinase
– Converts prothrombin to thrombin
– Thrombin converts fibrinogen to
fibrin
Functions of Thrombin
– Stimulates formation of tissue factor
Cascade Reactions
stimulates release of PF-3
– During coagulation phase (platelet factor)
– Chain reactions of enzymes and forms positive feedback loop
proenzymes (intrinsic and extrinsic):
– Form 3 pathways accelerates clotting
3 Coagulation Pathways Bleeding Time
Extrinsic pathway: – Normally, a small puncture wound
– begins in the vessel wall stops bleeding in 1–4 minutes
– outside blood stream
Clotting: Area Restriction
Intrinsic pathway:
– begins with circulating 1. Anticoagulants (plasma proteins):
proenzymes – antithrombin-III
– within bloodstream – alpha-2-macroglobulin
Common pathway: 2. Heparin
– where intrinsic and extrinsic 3. Protein C
pathways converge – stimulates plasmin formation
an enzyme that breaks down
fibrin strands (Protein C is
activated by
thrombomodulin)
4. Prostacyclin also inhibits platelet
aggregation.
Other Factors
– Calcium ions (Ca2+) and vitamin K
are both essential to the clotting
process
Clot Retraction
– After clot has formed:
Platelets contract and pull
torn area together
– Takes 30–60 minutes
Fibrinolysis
– Slow process of dissolving clot:
thrombin and tissue
plasminogen activator (t-PA):
activate plasminogen
– Plasminogen produces plasmin:
digests fibrin strands
Fun Fact:
Platelets are involved in coordination
of hemostasis (blood clotting)
Platelets, activated by abnormal
changes in local environment, release
clotting factors and other chemicals
Hemostasis is a complex cascade that
builds a fibrous patch that can be
remodeled and removed as the
damaged area is repaired
Potrebbero piacerti anche
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Learner Enrollment and Survey Form: Grade Level and School InformationDocumento2 pagineLearner Enrollment and Survey Form: Grade Level and School InformationThe Great Papyrus90% (73)
- Reporting in Earth Science I (Energy Resources) : 11 STEM-PasteurDocumento9 pagineReporting in Earth Science I (Energy Resources) : 11 STEM-PasteurAndrei BorataNessuna valutazione finora
- Catalase Enzyme - Qualitative AnalysisDocumento5 pagineCatalase Enzyme - Qualitative AnalysisAndrei BorataNessuna valutazione finora
- Grade 11-Pasteur: Name Address Attendance StatusDocumento1 paginaGrade 11-Pasteur: Name Address Attendance StatusAndrei BorataNessuna valutazione finora
- NCM 107 Worksheet Week 16.v2Documento2 pagineNCM 107 Worksheet Week 16.v2Andrei BorataNessuna valutazione finora
- Borata - FNCP (Parenthood)Documento2 pagineBorata - FNCP (Parenthood)Andrei BorataNessuna valutazione finora
- NCM 104 Worksheet Week 16Documento1 paginaNCM 104 Worksheet Week 16Andrei BorataNessuna valutazione finora
- Science Resource Book 3Documento42 pagineScience Resource Book 3Andrei BorataNessuna valutazione finora
- VALUES AND ETHICS IN COMMUNITY HEALTH NURSING SekitoDocumento8 pagineVALUES AND ETHICS IN COMMUNITY HEALTH NURSING SekitoAndrei BorataNessuna valutazione finora
- Laws Affecting Community Health Nursing Practice in The PhilippinesDocumento2 pagineLaws Affecting Community Health Nursing Practice in The PhilippinesAndrei Borata100% (1)
- Protein Lab Report 3Documento6 pagineProtein Lab Report 3Andrei BorataNessuna valutazione finora
- Nursing Care of The Family Having Difficulty Conceiving A ChildDocumento10 pagineNursing Care of The Family Having Difficulty Conceiving A ChildAndrei Borata100% (2)
- Relating Whole-Genome Expression Data With Protein-Protein InteractionsDocumento30 pagineRelating Whole-Genome Expression Data With Protein-Protein InteractionsKaye Pales CalamboNessuna valutazione finora
- CHN Sekito FinalsDocumento6 pagineCHN Sekito FinalsAndrei BorataNessuna valutazione finora
- Untitled Document PDFDocumento4 pagineUntitled Document PDFAndrei BorataNessuna valutazione finora
- VALUES AND ETHICS IN COMMUNITY HEALTH NURSING SekitoDocumento8 pagineVALUES AND ETHICS IN COMMUNITY HEALTH NURSING SekitoAndrei BorataNessuna valutazione finora
- BORATA, F - LAB Activity 1 PDFDocumento23 pagineBORATA, F - LAB Activity 1 PDFAndrei BorataNessuna valutazione finora
- Untitled Document PDFDocumento4 pagineUntitled Document PDFAndrei BorataNessuna valutazione finora
- Schistosomiasis Japonicum Infection As A Health DeficitDocumento4 pagineSchistosomiasis Japonicum Infection As A Health DeficitAndrei BorataNessuna valutazione finora
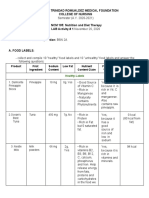
- Remedios Trinidad Romualdez Medical Foundation College of NursingDocumento23 pagineRemedios Trinidad Romualdez Medical Foundation College of NursingAndrei BorataNessuna valutazione finora
- ReportingMCN PDFX PDFDocumento136 pagineReportingMCN PDFX PDFAndrei BorataNessuna valutazione finora
- Group B CHNDocumento11 pagineGroup B CHNAndrei BorataNessuna valutazione finora
- Remedios Trinidad Romualdez Medical Foundation College of NursingDocumento23 pagineRemedios Trinidad Romualdez Medical Foundation College of NursingAndrei BorataNessuna valutazione finora
- Group B CHNDocumento11 pagineGroup B CHNAndrei BorataNessuna valutazione finora
- Protein Lab Report 3Documento6 pagineProtein Lab Report 3Andrei BorataNessuna valutazione finora
- Anaphy Special SensesDocumento180 pagineAnaphy Special SensesAndrei Borata100% (1)
- Protein Lab Report 3Documento6 pagineProtein Lab Report 3Andrei BorataNessuna valutazione finora
- Priority Setting Possible Complicated Pregnancy Schistosomiasis InfectionDocumento3 paginePriority Setting Possible Complicated Pregnancy Schistosomiasis InfectionAndrei BorataNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Presentation On Dysuria 1Documento25 paginePresentation On Dysuria 1ankur acharyaNessuna valutazione finora
- Carcinoma of Prostate: Dr. Saadat Hashmi Consultant UrologistDocumento48 pagineCarcinoma of Prostate: Dr. Saadat Hashmi Consultant UrologistMuhammad ArsalNessuna valutazione finora
- Nurs 512 Andersen Behavioral TheoryDocumento7 pagineNurs 512 Andersen Behavioral Theoryapi-251235373Nessuna valutazione finora
- Digital Meter: KIT No: 0349 307 620Documento6 pagineDigital Meter: KIT No: 0349 307 620Garlin MunarNessuna valutazione finora
- Pizza Hut and Dominos - A Comparative AnalysisDocumento19 paginePizza Hut and Dominos - A Comparative AnalysisSarvesh Kumar GautamNessuna valutazione finora
- SECTION 02892 Traffic Signals Rev 0Documento65 pagineSECTION 02892 Traffic Signals Rev 0Abdul HannanNessuna valutazione finora
- HC Letter Templates 26jun13Documento2 pagineHC Letter Templates 26jun13Jasdeep0% (1)
- By Josephine G. Ignacio, MD and Jennifer T. Co, MD, FPOGSDocumento9 pagineBy Josephine G. Ignacio, MD and Jennifer T. Co, MD, FPOGSAngela SaldajenoNessuna valutazione finora
- Cleaning Disinfecting School ClassroomsDocumento2 pagineCleaning Disinfecting School ClassroomsFitz JaminitNessuna valutazione finora
- Developments in Injection Moulding 3Documento331 pagineDevelopments in Injection Moulding 3Salah HammamiNessuna valutazione finora
- Passive In-Line Chlorination For Drinking Water DiDocumento18 paginePassive In-Line Chlorination For Drinking Water DitefovNessuna valutazione finora
- July 15, 2011 Strathmore TimesDocumento24 pagineJuly 15, 2011 Strathmore TimesStrathmore TimesNessuna valutazione finora
- LMA An. I-Sem 1-Engleza LEC-The Category of Aspect & Aspect 3-Reedited OnDocumento4 pagineLMA An. I-Sem 1-Engleza LEC-The Category of Aspect & Aspect 3-Reedited OnIlie IonelNessuna valutazione finora
- EP-HQ-GDL-008-00 Safety - Critical - Elements - Integrity - Management - GuidelineDocumento57 pagineEP-HQ-GDL-008-00 Safety - Critical - Elements - Integrity - Management - GuidelineAHMED AMIRA100% (5)
- TC Colorcode PDFDocumento7 pagineTC Colorcode PDFPatrick MonteroNessuna valutazione finora
- Epoxy Plus Pipeline Repai Grout TG - MSDSDocumento5 pagineEpoxy Plus Pipeline Repai Grout TG - MSDSgrimaguilNessuna valutazione finora
- Manoshe Street Takeaway MenuDocumento9 pagineManoshe Street Takeaway MenuimaddakrNessuna valutazione finora
- Potential Use of Probiotics: Ekachai ChukeatiroteDocumento8 paginePotential Use of Probiotics: Ekachai ChukeatiroteDanu EffendiNessuna valutazione finora
- Pulse Production in India: Major Constraints and Way ForwardDocumento33 paginePulse Production in India: Major Constraints and Way ForwardDeus EXNessuna valutazione finora
- Pneumatic Oscillator Valve - Pneumatic Controls - Impulse Automation LTDDocumento3 paginePneumatic Oscillator Valve - Pneumatic Controls - Impulse Automation LTDDindin NajmudinNessuna valutazione finora
- Mapeh 10 1 Grading Examination: E. Modern NationalismDocumento3 pagineMapeh 10 1 Grading Examination: E. Modern NationalismMildred Abad SarmientoNessuna valutazione finora
- VálvulasDocumento44 pagineVálvulasCarlos LópezNessuna valutazione finora
- Northern NVProvider DirectoryDocumento82 pagineNorthern NVProvider DirectoryGuru NandeshwarNessuna valutazione finora
- Model CV QLDocumento6 pagineModel CV QLMircea GiugleaNessuna valutazione finora
- Full Download Test Bank For Nursing A Concept Based Approach To Learning Volume II 3rd Edition 3rd Edition PDF Full ChapterDocumento36 pagineFull Download Test Bank For Nursing A Concept Based Approach To Learning Volume II 3rd Edition 3rd Edition PDF Full Chaptersignor.truss.j26uk100% (17)
- 17.8 Inheritance IGCSE CIE Biology Ext Theory MS - LDocumento9 pagine17.8 Inheritance IGCSE CIE Biology Ext Theory MS - LBlessing TshumaNessuna valutazione finora
- Dr. Shekhar Challa Joins Bioscience Americas Board of AdvisorsDocumento2 pagineDr. Shekhar Challa Joins Bioscience Americas Board of AdvisorsPR.comNessuna valutazione finora
- Cessna 206 Chapter 24 Illustrated Parts CatalogueDocumento33 pagineCessna 206 Chapter 24 Illustrated Parts Cataloguekanwar100% (1)
- Denon DHT-T100 Ver 3 PDFDocumento34 pagineDenon DHT-T100 Ver 3 PDFboroda241083% (6)
- 1st English Lesson 6-7 - CompressedDocumento21 pagine1st English Lesson 6-7 - Compressedharonac588Nessuna valutazione finora