Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Diagnosis and Management of Placenta Previa
Caricato da
mtorquato_1Descrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Diagnosis and Management of Placenta Previa
Caricato da
mtorquato_1Copyright:
Formati disponibili
SOGC CLINICAL PRACTICE GUIDELINE
SOGC CLINICAL PRACTICE GUIDELINE No. 189, March 2007
Diagnosis and Management of Placenta Previa
2. Sonographers are encouraged to report the actual distance from
This guideline has been reviewed by the Clinical Obstetrics the placental edge to the internal cervical os at TVS, using
Committee and approved by the Executive and Council of the standard terminology of millimetres away from the os or millimetres
Society of Obstetricians and Gynaecologists of Canada. of overlap. A placental edge exactly reaching the internal os is
described as 0 mm. When the placental edge reaches or overlaps
PRINCIPAL AUTHOR the internal os on TVS between 18 and 24 weeks’ gestation
Lawrence Oppenheimer, MD, FRCSC, Ottawa ON (incidence 2–4%), a follow-up examination for placental location in
the third trimester is recommended. Overlap of more than 15 mm is
MATERNAL FETAL MEDICINE COMMITTEE associated with an increased likelihood of placenta previa at term. (ll-2A)
Dr Anthony Armson, MD, Halifax NS 3. When the placental edge lies between 20 mm away from the
Dr Dan Farine (Chair), MD, Toronto ON internal os and 20 mm of overlap after 26 weeks’ gestation,
ultrasound should be repeated at regular intervals depending on
Ms Lisa Keenan-Lindsay, RN, Oakville ON the gestational age, distance from the internal os, and clinical
Dr Valerie Morin, MD, Cap-Rouge QC features such as bleeding, because continued change in placental
location is likely. Overlap of 20 mm or more at any time in the third
Dr Tracy Pressey, MD, Vancouver BC
trimester is highly predictive of the need for Caesarean section
Dr Marie-France Delisle, MD, Vancouver BC (CS). (llI-B)
Dr Robert Gagnon, MD, London ON 4. The os–placental edge distance on TVS after 35 weeks’ gestation
Dr William Robert Mundle, MD, Windsor ON is valuable in planning route of delivery. When the placental edge
lies > 20 mm away from the internal cervical os, women can be
Dr John Van Aerde, MD, Edmonton AB offered a trial of labour with a high expectation of success. A
distance of 20 to 0 mm away from the os is associated with a
higher CS rate, although vaginal delivery is still possible depending
Abstract on the clinical circumstances. (ll-2A)
Objective: To review the use of transvaginal ultrasound for the 5. In general, any degree of overlap (> 0 mm) after 35 weeks is an
diagnosis of placenta previa and recommend management based indication for Caesarean section as the route of delivery. (ll-2A)
on accurate placental localization. 6. Outpatient management of placenta previa may be appropriate
Options: Transvaginal sonography (TVS) versus transabdominal for stable women with home support, close proximity to a
sonography for the diagnosis of placenta previa; route of delivery, hospital, and readily available transportation and telephone
based on placenta edge to internal cervical os distance; in-patient communication. (ll-2C)
versus out-patient antenatal care; cerclage to prevent bleeding; 7. There is insufficient evidence to recommend the practice of cervical
regional versus general anaesthesia; prenatal diagnosis of cerclage to reduce bleeding in placenta previa. (llI-D)
placenta accreta.
8. Regional anaesthesia may be employed for CS in the presence of
Outcome: Proven clinical benefit in the use of TVS for diagnosing placenta previa. (II-2B)
and planning management of placenta previa.
9. Women with a placenta previa and a prior CS are at high risk for
Evidence: MEDLINE search for “placenta previa” and bibliographic placenta accreta. If there is imaging evidence of pathological
review. adherence of the placenta, delivery should be planned in an
Benefits, Harms, and Costs: Accurate diagnosis of placenta previa appropriate setting with adequate resources. (II-2B)
may reduce hospital stays and unnecessary interventions. Validation: Comparison with Placenta previa and placenta previa
Recommendations: accreta: diagnosis and management. Royal College of
Obstetricians and Gynaecologists, Guideline No. 27,
1. Transvaginal sonography, if available, may be used to investigate October 2005.
placental location at any time in pregnancy when the placenta is
thought to be low-lying. It is significantly more accurate than The level of evidence and quality of recommendations are described
transabdominal sonography, and its safety is well using the criteria and classifications of the Canadian Task Force on
established. (11–2A) Preventive Health Care (Table).
J Obstet Gynaecol Can 2007;29(3):261–266
Key Words: Placenta previa, Caesarean section, transvaginal
ultrasonography, low-lying placenta
This guideline reflects emerging clinical and scientific advances as of the date issued and is subject to change. The information
should not be construed as dictating an exclusive course of treatment or procedure to be followed. Local institutions can dictate
amendments to these opinions. They should be well documented if modified at the local level. None of these contents may be
reproduced in any form without prior written permission of the SOGC.
MARCH JOGC MARS 2007 l 261
SOGC CLINICAL PRACTICE GUIDELINE
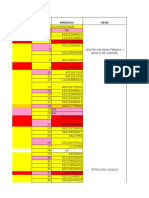
Key to evidence statements and grading of recommendations, using the ranking of the Canadian Task Force
on Preventive Health Care
Quality of Evidence Assessment* Classification of Recommendations†
I: Evidence obtained from at least one properly randomized A. There is good evidence to recommend the clinical preventive
controlled trial action
II-1: Evidence from well-designed controlled trials without B. There is fair evidence to recommend the clinical preventive
randomization action
II-2: Evidence from well-designed cohort (prospective or C. The existing evidence is conflicting and does not allow to
retrospective) or case-control studies, preferably from more make a recommendation for or against use of the clinical
than one centre or research group preventive action; however, other factors may influence
decision-making
II-3: Evidence obtained from comparisons between times or
places with or without the intervention. Dramatic results in D. There is fair evidence to recommend against the clinical
uncontrolled experiments (such as the results of treatment preventive action
with penicillin in the 1940s) could also be included in this E. There is good evidence to recommend against the clinical
category preventive action
III: Opinions of respected authorities, based on clinical I. There is insufficient evidence (in quantity or quality) to make
experience, descriptive studies, or reports of expert a recommendation; however, other factors may influence
committees decision-making
*The quality of evidence reported in these guidelines has been adapted from the Evaluation of Evidence criteria described in the Canadian Task Force
on the Periodic Preventive Health Exam Care.59
†Recommendations included in these guidelines have been adapted from the Classification of Recommendations criteria described in the Canadian
Task Force on the Periodic Preventive Health Exam Care.59
INTRODUCTION DIAGNOSIS OF PLACENTA PREVIA
Transvaginal sonography is now well established as the pre-
lacenta previa is defined as a placenta implanted in the
P lower segment of the uterus, presenting ahead of the
ferred method for the accurate localization of a low-lying
placenta. Sixty percent of women who undergo
leading pole of the fetus. It occurs in 2.8/1000 singleton transabdominal sonography (TAS) may have a reclassifica-
pregnancies and 3.9/1000 twin pregnancies1 and represents tion of placental position when they undergo TVS.7–10 With
a significant clinical problem, because the patient may need TAS, there is poor visualization of the posterior placenta,11
to be admitted to hospital for observation, she may need the fetal head can interfere with the visualization of the
blood transfusion, and she is at risk for premature delivery. lower segment,12 and obesity13 and underfilling or overfill-
The incidence of hysterectomy after Caesarean section (CS) ing of the bladder14,15 also interfere with accuracy. For these
for placenta previa is 5.3% (relative risk compared with reasons, TAS is associated with a false positive rate for the
those undergoing CS without placenta previa is 33).2 diagnosis of placenta previa of up to 25%.16 Accuracy rates
Perinatal mortality rates are three to four times higher than for TVS are high (sensitivity 87.5%, specificity 98.8%, posi-
in normal pregnancies.3,4 tive predictive value 93.3%, negative predictive value
97.6%), establishing TVS as the gold standard for the diag-
nosis of placenta previa.17 The only randomized trial to date
The traditional classification of placenta previa describes comparing TVS and TAS confirmed that TVS is more ben-
the degree to which the placenta encroaches upon the cer- eficial.18 TVS has also been shown to be safe in the presence
vix in labour and is divided into low-lying, marginal, partial, of placenta previa,17,19 even when there is established vagi-
or complete placenta previa.5 In recent years, publications nal bleeding. Magnetic resonance imaging (MRI) will also
have described the diagnosis and outcome of placenta accurately image the placenta and is superior to TAS.20 It is
previa on the basis of localization, using transvaginal unlikely that it confers any benefit over TVS for placental
sonography (TVS) when the exact relationship of the pla- localization, but this has not been properly evaluated.
cental edge to the internal cervical os can be accurately mea- Furthermore, MRI is not readily available in most units.
sured. The increased prognostic value of TVS diagnosis has
Recommendation
rendered the imprecise terminology of the traditional classi-
fication obsolete.6 This guideline describes the current diag- 1. Transvaginal sonography, if available, may be used to
nosis and management of placenta previa and is based investigate placental location at any time in pregnancy
largely on studies using TVS. when the placenta is thought to be low-lying. It is
262 l MARCH JOGC MARS 2007
Diagnosis and Management of Placenta Previa
significantly more accurate than transabdominal Transperineal or translabial ultrasound (using a
sonography, and its safety is well established. (ll-2A) transabdominal probe) can also improve upon the diagnos-
tic accuracy of TAS and may be a useful alternative when
PREDICTION OF PLACENTA PREVIA AT DELIVERY TVS is not available.29
The occurrence of placenta previa is common in the first Recommendations
half of pregnancy, and its persistence to term will depend on
2. Sonographers are encouraged to report the actual dis-
the gestational age and the definition employed for the
tance from the placental edge to the internal cervical os at
exact relationship of the internal cervical os to the placental
TVS, using standard terminology of millimetres away
edge on TVS.21–26 In this guideline, the following terminol-
from the os or millimetres of overlap. A placental edge
ogy is recommended to describe this relationship: when the
exactly reaching the internal os is described as 0 mm.
placenta edge does not reach the internal os, the distance is
When the placental edge reaches or overlaps the internal
reported in millimetres away from the internal os; when the
cervical os on TVS between 18 and 24 weeks’ gestation
placental edge overlaps the internal os by any amount, the
(incidence 2–4%), a follow-up examination for placental
distance is described as millimetres of overlap. A placental
location in the third trimester is recommended. Overlap
edge that exactly reaches the internal os is described by a
of more than 15 mm is associated with an increased
measurement of 0 mm.
likelihood of plaenta previa at term. (ll-2A)
For a placental edge reaching or overlapping the internal os,
3. When the placental edge lies between 20 mm away from
Mustafa et al.21 found in a longitudinal study an incidence of
the internal os and 20 mm overlap after 26 weeks’ gesta-
42% between 11 and 14 weeks, 3.9% between 20 and 24
tion, ultrasound should be repeated at regular intervals
weeks, and 1.9% at term. With overlap of 23 mm between
depending on the gestational age, distance from the
11 and 14 weeks, they estimated that the probability of pla-
internal os, and clinical features such as bleeding,
centa previa at term was 8%. Similarly, Hill et al.22 reported
because continued change in placental location is likely.
an incidence of 6.2% for a placenta extending over the
Overlap of 20 mm or more at any time in the third tri-
internal os between 9 and 13 weeks. In their series of 1252
mester is highly predictive of the need for CS. (lll-B)
patients, 20 (1.6%) had overlap of the placental edge of
16 mm or more, and only 4 of these had placenta previa
ROUTE OF DELIVERY AT TERM
persisting to term (0.3%). Two additional studies that have
examined various distances of overlap between 9 and The need for CS at term is predicated upon the os to placen-
16 weeks23,24 agreed that persistence of placenta previa is tal edge distance and clinical features (e.g., presence of
extremely unlikely if the degree of placental overlap is no unstable lie and/or bleeding). Five studies have examined
more than 10 mm. Two studies examined cut-off values at the likelihood of CS for placenta previa on the basis of dis-
18 to 23 weeks’ gestation.25,26 These found a similar inci- tance to the placental edge on the last ultrasound prior to
dence of the placenta reaching or overlapping the internal delivery.6,27–31 The last scan was performed at a mean of 35
os of up to 2%, and overall less than 20% of these persisted to 36 weeks’ gestational age, and a distance of > 20 mm
as placenta previa. The likelihood of persistent placenta away from the os was associated with a high likelihood of
previa was effectively zero when the placental edge reached vaginal delivery (range 63–100%). It has been suggested
but did not overlap the os (0 mm) and increased significantly that this cut-off distance of > 20 mm away from the os
beyond 15 mm overlap such that a distance of > 25 mm should be defined as a low-lying placenta, rather than a pla-
overlap had a likelihood of placenta previa at delivery of centa previa, in order to avoid the bias of physicians per-
between 40% and 100%. forming elective section based on the report of a placenta
previa.30 These cases can be managed in the high
The process of placental “migration” or relative upward
expectation of a vaginal delivery.
shift of the placenta due to differential growth of the lower
segment is continuous into the late third trimester.15,18,27 Of Between 20 mm and 0 mm away from the os on the last
26 patients scanned at an average of 29 weeks’ gestational scan, CS for placenta previa varies from approximately 40%
age when the placenta lay between 20 mm away from the to 90% and may be driven by the exact distance from the os
internal os and 20 mm of overlap, only 3 (11.5%) required and physicians’ prior knowledge of the ultrasound find-
CS for placenta previa at delivery. An average migration rate ing.28,30,31 In this latter group, trial of labour may be appro-
of > 1 mm per week was highly predictive of a normal out- priate in the absence of an unstable lie or bleeding,30
come. An overlap of > 20 mm after 26 weeks was predic- although more data in the form of prospective studies are
tive of the need for CS.27 Predanic et al.28 have subsequently required on the likelihood of antepartum and intrapartum
published similar results. bleeding.
MARCH JOGC MARS 2007 l 263
SOGC CLINICAL PRACTICE GUIDELINE
When the placenta overlaps the os by any amount on the of the baby weighing less than 2000 g. However, random-
last scan prior to delivery, CS is required in all cases27–31; this ization in this trial was by birth date, and analysis was by
was previously defined as “complete placenta previa.” treatment received not intention to treat.
Recommendations Recommendation
4. The os–placental edge distance on TVS after 35 weeks’ 7. There is insufficient evidence to recommend the practice
gestation is valuable in planning route of delivery. When of cervical cerclage to reduce bleeding in placenta
the placental edge lies > 20 mm away from the internal previa. (lll-D)
cervical os, women can be offered a trial of labour with a
high expectation of success. A distance of 20 to 0 mm METHOD OF ANAESTHESIA FOR CAESAREAN SECTION
away from the os is associated with a higher CS rate,
Anaesthesiologists are divided in their opinions regarding
although vaginal delivery is still possible depending on
the safest method of anaesthesia for CS with placenta
the clinical circumstances. (ll-2A)
previa.40 Two retrospective studies conclude that regional
5. In general, any degree of overlap (> 0 mm) after 35 weeks anaesthesia is safe,41,42 and one small randomized trial sug-
is an indication for Caesarean section as the route of gests that epidural anaesthesia is superior to general anaes-
delivery.(ll-2A) thesia with regard to maternal hemodynamics.43 When pro-
longed surgery is anticipated in women with prenatally diag-
INPATIENT VERSUS OUTPATIENT MANAGEMENT nosed placenta accreta, general anaesthesia may be prefera-
There has been one small published randomized trial32 that ble, and regional analgesia could be converted to general
explored home versus hospital management of women with anaesthesia if undiagnosed accreta is encountered.41
placenta previa. Twenty-seven women were randomized to Recommendation
bed rest with minimal ambulation in hospital, and 26
women were discharged home. Recurrent bleeding 8. Regional anaesthesia may be employed for CS in the
occurred in 62% of subjects. Overall, there was no differ- presence of placenta previa. (II-2B)
ence in any major outcome, and there was a significant sav-
PLACENTA PREVIA AND PLACENTA ACCRETA
ing of days in hospital in the outpatient group. A number of
retrospective reviews have also examined this question,33–35 The association between prior CS, placenta previa, and pla-
and the results of these trials also support the use of centa accreta (pathological adherence of the placenta) is
outpatient management for stable patients. However, it was well recognized. The incidence of placenta previa climbs
found that the clinical outcomes for placenta previa are with the number of prior CS,44,45 and there is a suggestion
highly variable and cannot be predicted confidently from that the incidence of placenta previa is rising because of the
antenatal events,32 although the degree of previa may be a increasing CS rate.46 The mechanism of causation of previa
guide to the likelihood of complications.36 Overall, the total by a previous scar is poorly understood, but it may be due to
number of women studied was small, and the statistical reduced differential growth of the lower segment resulting
power of these studies to address the issue of maternal and in less upward shift in placental position as pregnancy
neonatal safety was very limited. Further research is neces- advances.47, 48 Certainly the increasing CS rate is driving the
sary to make firm conclusions, and conservative in-hospital increasing rate of placenta accreta, which now stands at
management is the appropriate approach for women with 1:2500 deliveries.46 The relative risk of placenta accreta in
bleeding. the presence of placenta previa is 1:2065, which is consider-
Recommendation ably higher than the risk for women who have a normally
situated placenta.46 The risk of placenta accreta in the pres-
6. Outpatient management of placenta previa may be ence of placenta previa increases dramatically with the num-
appropriate for stable women with home support, close ber of previous CS, with a 25% risk for one prior CS, and
proximity to a hospital, and readily available transporta- more than 40% for two prior CS.45,49 Placenta accreta is a
tion and telephone communication. (ll-2C) significant condition with high potential for hysterectomy,
and a maternal death rate reported at 7%. Prenatal diagnosis
CERVICAL CERCLAGE
may be beneficial in preparing for delivery.50 A number of
The benefit of cervical cerclage in the antenatal manage- imaging techniques, including ultrasonography,51 colour
ment of placenta previa has been examined in a systematic Doppler,52,53 and MRI,54,55 are helpful in making a prenatal
review.37 Two trials were identified.38,39 A total of 64 diagnosis of placenta accreta. Conservative management of
women were randomized, and in one study38 there was a placenta accreta with preservation of the uterus is a thera-
reduction in the risk of delivery before 34 weeks or the birth peutic option. Case series56–58 report successes with leaving
264 l MARCH JOGC MARS 2007
Diagnosis and Management of Placenta Previa
the placenta in-situ and performing uterine artery 20. Powell MC, Buckley J, Price H, Worthington BS, Symonds EM. Magnetic
resonance imaging and placenta praevia. Am J Obstet Gynecol
embolization. 1986;154:656–9.
Recommendation 21. Mustafa SA, Brizot ML, Carvalho MHB, Watanabe L, Kahhale S, Zugaib Z.
Transvaginal ultrasonography in predicting placenta previa at delivery: a
9. Women with a placenta previa and a prior CS are at high longitudinal study. Ultrasound Obstet Gynecol 2002:20:356–9.
risk for placenta accreta. If there is imaging evidence of
22. Hill LM, Di Nofrio DM, Chenevey P. Transvaginal sonographic evaluation
pathological adherence of the placenta, delivery should of first-trimester placenta previa. Ultrasound Obstet Gynecol 1995;5:301–3.
be planned in an appropriate setting with adequate 23. Taipale P. Hiilesmaa V, Ylostalo P. Diagnosis of placenta previa by
resources. (II-2B) transvaginal sonographic screening at 12–16 weeks in a nonselected
population. Obstet Gynecol 1997;89:364–7.
REFERENCES 24. Rosati P, Guariglia L. Clinical significance of placenta previa detected at
1. Ananth CV, Demissie K, Smulian JC, Vintzileos AM. Placenta previa in early routine transvaginal scan. Ultrasound Med 2000;19:581–5.
singleton and twin births in the United States, 1989 through 1998: a 25. Taipale P. Hiilesmaa V, Ylostalo P. Transvaginal ultrasonography at 1823
comparison of risk factor profiles and associated conditions. Am J Obstet weeks in predicting placenta previa at delivery. Ultrasound Obstet Gynecol
Gynecol 2003;188: 275–81.
1998;12: 422–5.
2. Crane JM, Van den Hof MC, Dodds L, Armson BA, Liston R. Maternal
complications with placenta previa. Am J Perinatol. 2000;17:101–5. 26. Becker RH, Vonk R, Mende BC, Ragosch V, Entezami M. The relevance of
placental location at 20–23 gestational weeks for prediction of placenta
3. Crane JM, Van den Hof MC, Dods L, Armson BA, Liston R. Neonatal previa at delivery: evaluation of 8650 cases. Ultrasound Obstet Gynecol
outcomes with placenta previa. Obstet Gynecol 1997;177:210–4.
2001;17:496–501.
4. Ananth CV, Smulian JC, Vintzileos AM. The effect of placenta previa on
neonatal mortality: a population-based study in the United States, 1989 27. Oppenheimer L, Holmes P, Simpson N, Dabrowski A. Diagnosis of
through 1997. Am J Obstet Gynecol 2003;188:1299–304. low-lying placenta: can migration in the third trimester predict outcome?
Ultrasound Obstet Gynecol 2001;8:100–2.
5. Obstetrical Hemorrhage. In: Cunningham FG, MacDonald PC, Grant NF,
Leveno KJ, Gilstrap LC, Hankins GDV, et al., eds. Williams Obstetrics. 28. Predanic M, Perni SC, Baergen RN, Jean-Pierre C, Chasen ST, Chervenak
20th ed. Norwalk, Conn: Appleton & Lang 1997:745–82. FA. A sonographic assessment of different patterns of placenta previa
6. Oppenheimer L, Farine D, Ritchie K, Lovinsky RM, Telford J, Fairbanks “migration” in the third trimester of pregnancy. J Ultrasound Med 2005;
LA. What is a low-lying placenta? Am J Obstet Gynecol 1991;165:1036–8. 24:773–80.
7. Farine D, Fox HE, Timor-Tritsch I. Vaginal ultrasound for ruling out 29. Dawson WB, Dumas MD, Romano WM, Gagnon R, Gratton RJ, Mowbray
placenta previa. Br J Obstet Gynecol 1989;96:117–9. D. Translabial ultrasonography and placenta previa: does measurement of
8. Smith RS, Lauria MR, Comstock CH, Treadwell MC, Kirk JS, Lee W, et al. the os-placental distance predict outcome? J Ultrasound Med
Transvaginal ultrasonography for all placentas that appear to be low-lying 1996;15:441–6.
or over the internal cervical os. Ultrasound Obstet Gynecol 1997;9:22–4. 30. Sallout B, Oppenheimer, LW. The classification of placenta previa based on
9. Farine D, Fox HE, Jakobson S, Timor-Tritsch IE. Vaginal ultrasound for os-placental edge distance at transvaginal sonography. Am J Obstet
diagnosis of placenta previa. Am J Obstet Gynecol 1988;159:566–9. Gynecol 2002;187(6):S94.
10. Oyelese KO, Holden D, Awadh A, Coates S, Campbell S. Placenta previa: 31. Bhide A, Prefumo F, Moore J, Hollis B, Thilaganathan B. Placental edge to
the case for transvaginal sonography. Cont Rev Obstet Gynaecol internal os distance in the late third trimester and mode of delivery in
1999:257–61. placenta previa. Br J Obstet Gynaecol 2003;110:860–4.
11. Edlestone DI. Placental localization by ultrasound. Clin Obstet Gynecol 32. Wing DA, Paul RH, Millar LK. Management of the symptomatic placenta
1977;20:285–7. previa: a randomized, controlled trial of inpatient versus outpatient
expectant management. Am J Obstet Gynecol 1996;175:806–11.
12. King DL. Placental ultrasonography. JCU 1973;1:21–6.
33. Love CDB, Wallace EM. Pregnancies complicated by placenta praevia: what
13. Timor-Tritsch IE, Rottem S. Transvaginal sonography. New York: Elsevier
is appropriate management? Br J Obstet Gynaecol 1996;103:864–7.
1987:1–13.
34. Droste S, Keil K. Expectant management of placenta praevia: cost benefit
14. Townsend RR, Laing FC, Nyberg DA, Jeffrey RB, Wing VW. Technical
analysis of outpatient treatment. Am J Obstet Gynecol 1994;170:1254–7.
factors responsible for placental migration: sonographic assessment.
Radiology 1986;160:105–8. 35. Mouer JR. Placenta praevia: antepartum conservative management, inpatient
versus outpatient. Am J Obstet Gynecol 1994;170:1683–6.
15. Lauria MR, Smith RS, Treadwell MC, Comstock CH, Kirk JS, Lee W,
Bottoms SF. The use of second-trimester transvaginal sonography to 36. Dola CP, Garite TJ, Dowling DD, Friend D, Ahdoot D, Asrat T. Placenta
predict placenta previa. Ultrasound Obstet Gynecol 1996;8:337–40. previa: does its type affect pregnancy outcome? Am J Perinatol
2003:353–60.
16. McClure N, Dorman JC. Early identification of placenta praevia. Br J Obstet
Gynaecol 1990;97:959–61. 37. Nelson JP. Interventions for suspected placenta praevia (Cochrane review).
In The Cochrane Library, Oxford: Update software. 2004; Issue 2.
17. Leerentveld RA, Gilberts ECAM, Arnold KJCW, Wladimiroff JW. Accuracy
and safety of transvaginal sonographic placental localization. Obstet 38. Arias F. Cervical cerclage for the temporary treatment of patients with
Gynecol 1990;76:759–62. placenta previa. Obstet Gynecol 1988;71:545–8.
18. Sherman SJ, Carlson DE, Platt LD, Mediaris AL. Transvaginal ultrasound: 39. Cobo E, Conde-Agudelo A, Delgado J, Canaval H, Congote A. Cervical
does it help in the diagnosis of placenta praevia? Ultrasound Obstet cerclage: an alternative for the management of placenta previa. Am J Obstet
Gynecol 1992;256–60. Gynecol 1998;179:122–5.
19. Timor-Tritsch IE, Yunis RA. Confirming the safety of transvaginal 40. Bonner SM, Haynes SR, Ryall D. The anaesthetic management of caesarean
sonography in patients suspected of placenta previa. Obstet Gynecol section for placenta praevia: a questionnaire survey. Anaesthesia
1993;81:742–4. 1995;50:992–4.
MARCH JOGC MARS 2007 l 265
SOGC CLINICAL PRACTICE GUIDELINE
41. Parekh N, Husaini SW, Russel IF. Caesarean section for placenta praevia: a 52. Chou MM, Ho ESC. Prenatal diagnosis of placenta praevia accreta with
retrospective study of anaesthetic management. Br J Anaesth power amplitude ultrasonic angiography. Am J Obstet Gynecol
2000;84:725–30. 1997;177:1523–5.
42. Frederiksen MC, Glasenberg R, Stika CS. Placenta previa: a 22-year analysis.
53. Yang JI, Lim YK, Kim HS, Chang KH, Lee JP, Ryu HS. Sonographic
Am J Obstet Gynecol 1999;180:1432–7.
findings of placental lacunae and the prediction of adherent placenta in
43. Hong JY, Jee YS, Yoon HJ, Kim SM. Comparison of epidural and general women with placenta previa totalis and prior Cesarean section. Ultrasound
anaesthesia in cesarean section for placenta previa. Intl J Obstet Anaesthesia Obstet Gynecol. 2006;28:178–82.
2003;12:12–6.
54. Tanaka YO, Sohda S, Shigemitsu S, Niitsu M, Itai Y. High temporal
44. Gilliam M, Rosenberg D, Davis F. The likelihood of placenta previa with
resolution contrast MRI in high risk group for placenta accreta. Magn
greater number of cesarean deliveries and higher parity. Obstet Gynecol
Reson Imaging 2001;19:635–42.
2002;99:976–80.
45. Clark SL, Koonings PP, Phelan JP. Placenta praevia / accreta and prior 55. Warshak CR, Eskander R, Hull AD, Scioscia AL, Mattrey RF, Benirschke K,
caesarean section. Obstet Gynecol 1985;66:89–92. et al. Accuracy of ultrasonography and magnetic resonance imaging in the
46. Miller DA, Chollet JA, Goodwin TM. Clinical risk factors for placenta diagnosis of placenta accreta. Obstet Gynecol. 2006;108:573–81.
praevia -placenta accreta. Am J Obstet Gynecol 1997;177:210–4.
56. Ouellet A, Sallout B, Oppenheimer LW. Conservative v surgical
47. Dashe JS, McIntire DD, Ramus RM, Santos-Ramos R, Twickler DM. management of placenta accreta; a systematic review of the literature and
Persistence of placenta previa according to gestational age at ultrasound case series. Am J Obstet Gynecol 2003:189:S130.
detection. Obstet Gynecol 2002;99:692–7.
57. Courbiere B, Bretelle F, Porcu G, Gamere M, Blanc B. Conservative
48. Laughon SK, Wolfe HM, Visco AG. Prior cesarean and the risk for placenta
treatment of placenta accreta. J Gynecol Obstet Biol Reprod
previa on second-trimester ultrasonography. Obstet Gynecol
2003;32:549–54.
2005;105:962–5.
49. Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, et al. 58. Clement D, Kayem G, Cabrol D. Conservative treatment of placenta
Maternal morbidity associated with multiple repeat cesarean deliveries. percreta: a safe alternative. Eur J Obstet Gynaecol Reprod Biol
Obstet Gynecol 2006;107:1226–32. 2004;114:108–9.
50. O’Brien JM, Barton JR, Donaldson ES. The management of placenta
59. Woolf SH, Battista RN, Angerson GM, Logan AG, Eel W.
percreta: conservative and operative strategies. Am J Obstet Gynecol
Canadian Task Force on Preventive Health Care. New grades for
1996;75:1632–8.
recommendations from the Canadian Task Force on Preventive Health
51. Finberg H, Williams J. Placenta accreta: prospective sonographic diagnosis Care. Can Med Assoc J 2003;169(3):207-8.
in patients with placenta previa and prior cesarean section. J Ultrasound
Med 1992;11:333–43.
266 l MARCH JOGC MARS 2007
Potrebbero piacerti anche
- Absolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationDa EverandAbsolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationNessuna valutazione finora
- 102E CPG May2001Documento4 pagine102E CPG May2001Sidonia CatalinaNessuna valutazione finora
- Lower Genital Tract Precancer: Colposcopy, Pathology and TreatmentDa EverandLower Genital Tract Precancer: Colposcopy, Pathology and TreatmentNessuna valutazione finora
- Canadian Guidelines For Prenatal Diagnosis: Echniques of Renatal IagnosisDocumento9 pagineCanadian Guidelines For Prenatal Diagnosis: Echniques of Renatal IagnosisRuxandra CretuNessuna valutazione finora
- Pregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsDa EverandPregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsNessuna valutazione finora
- Green Top Guidelines 8Documento13 pagineGreen Top Guidelines 8Arafath AkramNessuna valutazione finora
- Atypical Breast Proliferative Lesions and Benign Breast DiseaseDa EverandAtypical Breast Proliferative Lesions and Benign Breast DiseaseFarin AmersiNessuna valutazione finora
- Vasa Praevia Peer Review DraftDocumento11 pagineVasa Praevia Peer Review DraftFelix CamposNessuna valutazione finora
- Trial of Labor Compared With Elective Cesarean.12Documento10 pagineTrial of Labor Compared With Elective Cesarean.12Herman FiraNessuna valutazione finora
- CVX Length SOGCDocumento14 pagineCVX Length SOGCBrendaNessuna valutazione finora
- RANZCOG Management of Breech PresentationDocumento9 pagineRANZCOG Management of Breech PresentationKe XuNessuna valutazione finora
- Placenta Previa PDFDocumento15 paginePlacenta Previa PDFDamaris GonzálezNessuna valutazione finora
- Ultrasoundinearly Pregnancy: Viability, Unknown Locations, and Ectopic PregnanciesDocumento13 pagineUltrasoundinearly Pregnancy: Viability, Unknown Locations, and Ectopic PregnanciesAdriana MartínezNessuna valutazione finora
- Jurnal Obgyn 2018 2Documento15 pagineJurnal Obgyn 2018 2aulNessuna valutazione finora
- Hemorragia y EmbrazoDocumento6 pagineHemorragia y Embrazoana catalinaNessuna valutazione finora
- How To Perform Standardized Sonographic Examination of Cesarean Scar Pregnancy in The First TrimesterDocumento22 pagineHow To Perform Standardized Sonographic Examination of Cesarean Scar Pregnancy in The First TrimesterWillans Eduardo Rosha HumerezNessuna valutazione finora
- New Options for Managing Adherent PlacentaDocumento6 pagineNew Options for Managing Adherent PlacentaAngelique Ramos PascuaNessuna valutazione finora
- Risk Factors for Severe PPH After C-Section for Placenta PraeviaDocumento7 pagineRisk Factors for Severe PPH After C-Section for Placenta PraeviaCorina PavalacheNessuna valutazione finora
- Placenta Praevia, Placenta Accreta and Vasa Praevia Managment and Diagnosis Royal College of ObgDocumento26 paginePlacenta Praevia, Placenta Accreta and Vasa Praevia Managment and Diagnosis Royal College of ObgDiana PanaitNessuna valutazione finora
- s12884 019 2244 4 PDFDocumento7 pagines12884 019 2244 4 PDFAnitaNessuna valutazione finora
- 10 The Role of Routine Cervical Length Screening in Selected High - and Low-Risk Women For Preterm Birth PreventionDocumento6 pagine10 The Role of Routine Cervical Length Screening in Selected High - and Low-Risk Women For Preterm Birth PreventionWailea Faye SalvaNessuna valutazione finora
- Cervical Cerclage, Pessary, or Vaginal Progesterone 2019 PDFDocumento10 pagineCervical Cerclage, Pessary, or Vaginal Progesterone 2019 PDFBodhi PadmaNessuna valutazione finora
- Clinical Green Top Guidelines: 3.1 Using PostureDocumento6 pagineClinical Green Top Guidelines: 3.1 Using PostureResti RusydiNessuna valutazione finora
- IJHS Robson PublicationDocumento9 pagineIJHS Robson PublicationVinod BharatiNessuna valutazione finora
- Amniosentesis Dan CvsDocumento13 pagineAmniosentesis Dan CvsFitri Amelia RizkiNessuna valutazione finora
- A Short Cervical Length in PregnancyDocumento10 pagineA Short Cervical Length in Pregnancydinda_zaidiNessuna valutazione finora
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Documento2 pagineP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)shelly_shellyNessuna valutazione finora
- Committee Opinion: Placenta AccretaDocumento5 pagineCommittee Opinion: Placenta AccretaagungNessuna valutazione finora
- Jurnal Plasenta Akreta PDFDocumento5 pagineJurnal Plasenta Akreta PDFfatqur28Nessuna valutazione finora
- Aust NZ J Obst Gynaeco - 2022 - Silveira - Placenta Accreta Spectrum We Can Do BetterDocumento7 pagineAust NZ J Obst Gynaeco - 2022 - Silveira - Placenta Accreta Spectrum We Can Do BetterDrFeelgood WolfslandNessuna valutazione finora
- Cesarean Scar Pregnancy Diagnosis and TreatmentDocumento13 pagineCesarean Scar Pregnancy Diagnosis and TreatmentTandyo TriasmoroNessuna valutazione finora
- Desi Rahayu (153112540120468Documento53 pagineDesi Rahayu (153112540120468Bella FebriyantiNessuna valutazione finora
- Vaginal Delivery After Cesarean Section.: Rubina Bashir and Khurshid KhattakDocumento2 pagineVaginal Delivery After Cesarean Section.: Rubina Bashir and Khurshid KhattakMaria KatherineNessuna valutazione finora
- 1 s2.0 S0002937819312062 MainDocumento9 pagine1 s2.0 S0002937819312062 MainprofbarrosordemNessuna valutazione finora
- Cervical pessary reduces preterm birth in twin pregnancies with short cervixDocumento8 pagineCervical pessary reduces preterm birth in twin pregnancies with short cervixjj_cani91Nessuna valutazione finora
- C-Obs 38 Planned Vaginal Birth After C-Section New Jul 10Documento7 pagineC-Obs 38 Planned Vaginal Birth After C-Section New Jul 10Aris SugiatnoNessuna valutazione finora
- Cervical Conization and The Risk of Preterm DeliveryDocumento11 pagineCervical Conization and The Risk of Preterm DeliveryGelo ConcepcionNessuna valutazione finora
- Rcog - Management of Tubal PDFDocumento10 pagineRcog - Management of Tubal PDFBoyNessuna valutazione finora
- ACOG Guides and Opinion On Placenta Accreta ManagementDocumento5 pagineACOG Guides and Opinion On Placenta Accreta ManagementCharlene FernándezNessuna valutazione finora
- Screen-and-Treat Approaches For Cervical Cancer Prevention in Low-Resource SettingsDocumento9 pagineScreen-and-Treat Approaches For Cervical Cancer Prevention in Low-Resource SettingsSaddam FuadNessuna valutazione finora
- CHSJ 48 02 04 2022Documento7 pagineCHSJ 48 02 04 2022mihail.boldeanuNessuna valutazione finora
- Guidelines for diagnosis and treatment of laparoscopy during pregnancyDocumento13 pagineGuidelines for diagnosis and treatment of laparoscopy during pregnancyCecilia Quispe JaureguiNessuna valutazione finora
- gtg60 Cervicalcerclage PDFDocumento21 paginegtg60 Cervicalcerclage PDFLijoeliyas100% (1)
- Cervicval Shortening / Cervical Insufficiency: EtiologyDocumento3 pagineCervicval Shortening / Cervical Insufficiency: EtiologyMiska RaihanaNessuna valutazione finora
- Guide to Breech Presentation DeliveryDocumento13 pagineGuide to Breech Presentation DeliveryRahmawati Dianing PangestuNessuna valutazione finora
- Surgical Treatment of Cesarean Scar Ectopic PregnancyDocumento7 pagineSurgical Treatment of Cesarean Scar Ectopic PregnancyIndRa KaBhuomNessuna valutazione finora
- Simcox 2009Documento6 pagineSimcox 2009Aulya ArchuletaNessuna valutazione finora
- SOGC CLINICAL PRACTICE GUIDELINE Vaginal Delivery of Breech PresentationDocumento8 pagineSOGC CLINICAL PRACTICE GUIDELINE Vaginal Delivery of Breech PresentationsobgyniaNessuna valutazione finora
- Management of Breech PresentationDocumento13 pagineManagement of Breech Presentationdr.Hansen.SH100% (1)
- Vaginal Birth After Caeserean Section: BY Seun ODocumento24 pagineVaginal Birth After Caeserean Section: BY Seun OOlaiya OluwaseunNessuna valutazione finora
- Screening For Cervical Cancer: U.S. Preventive Services Task ForceDocumento9 pagineScreening For Cervical Cancer: U.S. Preventive Services Task Forcemutya yulindaNessuna valutazione finora
- Committee Opinion: Placenta AccretaDocumento5 pagineCommittee Opinion: Placenta AccretabebetteryesyoucanNessuna valutazione finora
- Committee Opinion: Scheduled Cesarean Delivery and The Prevention of Vertical Transmission of HIV InfectionDocumento4 pagineCommittee Opinion: Scheduled Cesarean Delivery and The Prevention of Vertical Transmission of HIV InfectionHerry SasukeNessuna valutazione finora
- Cerclage For Women With Twin Pregnancies: A Systematic Review and MetaanalysisDocumento16 pagineCerclage For Women With Twin Pregnancies: A Systematic Review and MetaanalysisSaira MendozaNessuna valutazione finora
- Knight Et Al-2014-BJOG An International Journal of Obstetrics & GynaecologyDocumento10 pagineKnight Et Al-2014-BJOG An International Journal of Obstetrics & GynaecologyAndrian drsNessuna valutazione finora
- Role of Ultrasonography in Diagnosis of Ectopic Pregnancy With Clinical Analysis and Management in Tertiary Care HospitalDocumento4 pagineRole of Ultrasonography in Diagnosis of Ectopic Pregnancy With Clinical Analysis and Management in Tertiary Care HospitalRizka AdiNessuna valutazione finora
- Managing Placenta Accreta: Medical vs Surgical OptionsDocumento9 pagineManaging Placenta Accreta: Medical vs Surgical OptionsAslesa Wangpathi PagehgiriNessuna valutazione finora
- Mustafa 2016Documento7 pagineMustafa 2016ejigsonNessuna valutazione finora
- Caesarean Scar Pregnancy. Diagnosis, Natural History and Treatment (Curr Opin Obstet Gynecol - Oct 2022)Documento8 pagineCaesarean Scar Pregnancy. Diagnosis, Natural History and Treatment (Curr Opin Obstet Gynecol - Oct 2022)garomeros5366Nessuna valutazione finora
- Prev Lscs RcogDocumento17 paginePrev Lscs Rcogkutra3000Nessuna valutazione finora
- JurnalDocumento8 pagineJurnaldhea handyaraNessuna valutazione finora
- Case Studies 4Documento19 pagineCase Studies 4FA KhanNessuna valutazione finora
- Invent A RioDocumento56 pagineInvent A RioJhoel Eusebio Parraga IsidroNessuna valutazione finora
- Chapter 32 - Anesthesia For Genitourinary SurgeryDocumento20 pagineChapter 32 - Anesthesia For Genitourinary SurgeryfewNessuna valutazione finora
- Nursing Course Syllabus ns4143 Winter 2013Documento11 pagineNursing Course Syllabus ns4143 Winter 2013api-232466940Nessuna valutazione finora
- Essential Newborn CareDocumento104 pagineEssential Newborn CareNacel Celeste100% (11)
- Prostho Lecture 8, Teeth Selection & SettingDocumento11 pagineProstho Lecture 8, Teeth Selection & SettingJustDen09Nessuna valutazione finora
- Uterine CancerDocumento20 pagineUterine CancerAjurs UrsabiaNessuna valutazione finora
- The Holistic Midwifery Care of Post Partum Mother With PostDocumento11 pagineThe Holistic Midwifery Care of Post Partum Mother With PostrezayantiquNessuna valutazione finora
- Auricular Acupuncture at The Shenmen'' and Point Zero'' Points Induced Parasympathetic ActivationDocumento5 pagineAuricular Acupuncture at The Shenmen'' and Point Zero'' Points Induced Parasympathetic Activationraspino1959Nessuna valutazione finora
- Independent nurse midwifery practitioner issuesDocumento8 pagineIndependent nurse midwifery practitioner issuesKrishnaveni Murugesh100% (3)
- Breast Feeding GuidelinesDocumento18 pagineBreast Feeding GuidelinesAdelle SmithNessuna valutazione finora
- Maternity Magazine 2012 - 2013 PDFDocumento212 pagineMaternity Magazine 2012 - 2013 PDFMaria Carolina LowenNessuna valutazione finora
- Ectopic Pregnancy GuideDocumento27 pagineEctopic Pregnancy GuideuunuunuunNessuna valutazione finora
- Inggris IndonesiaDocumento26 pagineInggris IndonesialaudyaFebNessuna valutazione finora
- Obstetrics MCQsDocumento28 pagineObstetrics MCQsMenna KamalNessuna valutazione finora
- Dental BooklistDocumento14 pagineDental Booklistالمكتبة المليونيةNessuna valutazione finora
- Hare Krishna: The Possible HealDocumento3 pagineHare Krishna: The Possible HealReshinth AdithyanNessuna valutazione finora
- Dentest 5th Edition Clinicals ErrataDocumento18 pagineDentest 5th Edition Clinicals ErrataSrinivasan Balaji0% (2)
- Historia de La AnatomíaDocumento1 paginaHistoria de La AnatomíaPaolo MafaldoNessuna valutazione finora
- Rodriguez2005-Cognitive Dysfunction After Total Knee Arthroplasty - Effects of Intraoperative Cerebral Embolization and Postoperative ComplicationsDocumento9 pagineRodriguez2005-Cognitive Dysfunction After Total Knee Arthroplasty - Effects of Intraoperative Cerebral Embolization and Postoperative ComplicationsSyahpikal SahanaNessuna valutazione finora
- Clinical Practice Guidelines 11-18Documento20 pagineClinical Practice Guidelines 11-18Feroz RaZa SoomrOoNessuna valutazione finora
- Organisasi Perawat Indonesia Dan Dunia PDFDocumento35 pagineOrganisasi Perawat Indonesia Dan Dunia PDFRosalina LubisNessuna valutazione finora
- Benign Diseases of Vulva and VaginaDocumento6 pagineBenign Diseases of Vulva and VaginaTj Kevin P-DoctorNessuna valutazione finora
- University of Health Sciences, Lahore: Admission Form ForDocumento2 pagineUniversity of Health Sciences, Lahore: Admission Form ForMuhammad AbubakarNessuna valutazione finora
- ASEAN Mutual Recognition Arrangement For Indonesian Nurses: Is It A Promise?Documento4 pagineASEAN Mutual Recognition Arrangement For Indonesian Nurses: Is It A Promise?Krisha JacobNessuna valutazione finora
- Trauma and Spine Sessions at Medical ConferenceDocumento5 pagineTrauma and Spine Sessions at Medical ConferencesrisaravananNessuna valutazione finora
- Med Record ClerkDocumento3 pagineMed Record ClerkrengikrishnaNessuna valutazione finora
- Asian Hospital and Medical CenterDocumento2 pagineAsian Hospital and Medical CenterErnest Brian Fernandez100% (1)
- Prof - Rajesh Malhotra PDFDocumento7 pagineProf - Rajesh Malhotra PDFashish gargNessuna valutazione finora
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (13)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDa EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsValutazione: 5 su 5 stelle5/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDa EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityValutazione: 3.5 su 5 stelle3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDa EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsValutazione: 3.5 su 5 stelle3.5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDa EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionValutazione: 4 su 5 stelle4/5 (402)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDa EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNessuna valutazione finora
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 5 su 5 stelle5/5 (78)
- Techniques Exercises And Tricks For Memory ImprovementDa EverandTechniques Exercises And Tricks For Memory ImprovementValutazione: 4.5 su 5 stelle4.5/5 (40)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDa EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisValutazione: 4 su 5 stelle4/5 (1)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDa EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsValutazione: 4.5 su 5 stelle4.5/5 (169)
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 5 su 5 stelle5/5 (4)
- The Ultimate Guide To Memory Improvement TechniquesDa EverandThe Ultimate Guide To Memory Improvement TechniquesValutazione: 5 su 5 stelle5/5 (34)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDa EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessValutazione: 4.5 su 5 stelle4.5/5 (327)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsDa EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNessuna valutazione finora
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingDa EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingValutazione: 5 su 5 stelle5/5 (4)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDa EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeValutazione: 4.5 su 5 stelle4.5/5 (253)
- The Happiness Trap: How to Stop Struggling and Start LivingDa EverandThe Happiness Trap: How to Stop Struggling and Start LivingValutazione: 4 su 5 stelle4/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDa EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisValutazione: 4.5 su 5 stelle4.5/5 (41)
- Seeing What Others Don't: The Remarkable Ways We Gain InsightsDa EverandSeeing What Others Don't: The Remarkable Ways We Gain InsightsValutazione: 4 su 5 stelle4/5 (288)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingDa EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingValutazione: 3.5 su 5 stelle3.5/5 (33)
- The Tennis Partner: A Doctor's Story of Friendship and LossDa EverandThe Tennis Partner: A Doctor's Story of Friendship and LossValutazione: 4.5 su 5 stelle4.5/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDa EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDa EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisValutazione: 5 su 5 stelle5/5 (8)