Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Terminología y Clasificación de Las Displasias (2004) PDF
Caricato da
lucasher35Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Terminología y Clasificación de Las Displasias (2004) PDF
Caricato da
lucasher35Copyright:
Formati disponibili
Articles
Terminology and classification of the
cortical dysplasias
A. Palmini, MD, PhD; I. Najm, MD; G. Avanzini, MD; T. Babb, PhD; R. Guerrini, MD;
N. Foldvary-Schaefer, DO; G. Jackson, MD; H.O. Lüders, MD, PhD; R. Prayson, MD, PhD;
R. Spreafico, MD, PhD; and H.V. Vinters, MD
Abstract—Background: There have been difficulties in achieving a uniform terminology in the literature regarding issues
of classification with respect to focal cortical dysplasias (FCDs) associated with epilepsy. Objectives: To review and refine
the current terminology and classification issues of potential clinical relevance to epileptologists, neuroradiologists, and
neuropathologists dealing with FCD. Methods: A panel discussion of epileptologists, neuropathologists, and neuroradiolo-
gists with special expertise in FCD was held. Results: The panel proposed 1) a specific terminology for the different types
of abnormal cells encountered in the cerebral cortex of patients with FCD; 2) a reappraisal of the different histopathologic
abnormalities usually subsumed under the term “microdysgenesis,” and suggested that this terminology be abandoned;
and 3) a more detailed yet straightforward classification of the various histopathologic features that usually are included
under the heterogeneous term of “focal cortical dysplasia.” Conclusion: The panel hopes that these proposals will stimulate
the debate toward more specific clinical, imaging, histopathologic, and prognostic correlations in patients with FCD
associated with epilepsy.
NEUROLOGY 2004;62(Suppl 3):S2–S8
Malformations caused by abnormalities of cortical Previous studies indicated that the pathogenesis
development (MCD),1 also known as disorders of cor- of the various histopathologic patterns is multifacto-
tical development,2 cortical dysplasias,3-5 cortical dys- rial: genetic mutations,13,14,30,31 in utero injuries at
genesis,6,7 or neuronal migration disorders (NMDs),8,9 different stages of brain development,6,32-35 and even
have been recognized increasingly in patients with perinatal or postnatal insults may contribute to their
drug-resistant epilepsy. Advances in basic and clini- etiology.36,37 The type, timing, and severity of envi-
cal neurosciences have opened exciting avenues for ronmental insults or the nature of genetic mutation
research on the mechanisms of epileptogenicity and and the impact of an abnormal gene product at dif-
cerebral dysfunction in patients with MCD. ferent stages of brain development will likely influ-
The advent of various MRI techniques has facili- ence the expression of the histopathologic and
tated the in vivo identification of a large group of corti- anatomic types of MCD.
cal malformations in patients with epilepsy.5,10-12 There Previous attempts to classifying MCDs provided
has been progress in the understanding of various either simplistic or complex classification schemes
pathogenetic mechanisms,13-18 engineering and testing that addressed specific aspects of these disor-
of various animal models of MCD;19-21 description of ders.5,26,38 Thus far, the most comprehensive classifi-
direct clinical-electrographic correlations,22-25 and the cation is that proposed by Barkovich et al.,1 who
delineation of surgical strategies26-29 for management of have included embryologic, histopathologic, imaging,
the various types of MCD associated with epilepsy. De- and genetic aspects within their scheme. The major
spite these advances, it has become obvious that there merit of this classification is its organization of the
was a lack of uniform, well-defined clinically sound various types of MCD within an embryologic-
histopathologic nomenclature for and classification of pathophysiologic framework, recognizing that MCD
these disorders. Such classification may allow for fur- could be caused by abnormalities during specific
ther progress in understanding these entities through stages of cortical development (neuroglial prolifera-
improved communication at the clinical/electrographic, tion and differentiation, neuronal migration, and
histopathologic, and basic scientific levels of research. postmigratory cortical organization). This classifica-
From the Pontificia Universidade Católica do Rio Grande do Sul (PUCRS) (Dr. Palmini), Porto Alegre, Brazil; The Cleveland Clinic Foundation (Drs. Najm,
Foldvary-Schaefer, Lüders, and Prayson), Cleveland, OH; Istituto Nazionale Neurologico “C. Besta” (Drs. Avanzini and Spreafico), Milan, Italy; Wayne State
University (Dr. Babb), Detroit, MI; Istituto de Neuropsichiatria Infantile (R. Guerrini), University of Pisa, Italy; Austin Hospital (Dr. Jackson), Melbourne,
Australia; and University of California Los Angeles Medical Center (Dr. Vinters), Los Angeles, CA.
I.N. was supported by grants K08-NS02046 and R21-NS42354 from the NIH.
Address correspondence and reprint requests to André Palmini, Serviço de Neurologia, Hospital São Lucas da PUCRS, Avenida Ipiranga 6690, Porto Alegre,
RS, Brazil, CEP 90610-000; e-mail: apalmini@uol.com.br
S2 Copyright © 2004 by AAN Enterprises, Inc.
tion1 did not emphasize a key issue in current epilep-
tology, the existence of focal cortical dysplasias
(FCDs), which are localized malformations increas-
ingly associated with refractory seizures and cur-
rently operated on at most epilepsy centers.39-42 A
good clinical correlation to the different aspects of
the histopathologic findings within FCDs has not
been described.
Thus, we suggest that it may be time for a reap-
praisal of nomenclature and classification issues in
patients with MCD, particularly for those harboring
FCD and other subtle microscopic abnormalities,
usually encompassed under the term microdysgen-
esis. This panel of epileptologists working in the area
of epilepsy surgery, neuropathologists, neuroradiolo-
gists, and basic scientists attempted to organize a
scheme that could be of practical and broad applica-
tion. We hope that the use of the proposed classifica-
tion scheme in everyday practice and for research
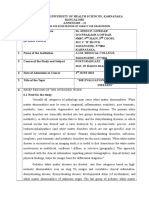
purposes will refine and validate its usefulness. Figure 1. Cresylecht violet staining shows the dysmorphic
Our proposal is divided into three parts: 1) defini- neurons. Note the high Nissl stain density and the various
tion of terminology for the histopathologic descrip- directions of the neurons; scale bar, 50 m.
tion of FCDs; 2) description of selected aspects of
FCDs; and 3) a classification proper, in which differ- malities of intracortical architecture in patients with
ent histopathologic subtypes are described and corre- generalized epilepsies undergoing autopsy studies.
lated with their current status of identification by Furthermore, the panel thought that the following
MRI, as well as with some clinical features and prog- terms should be either more clearly defined or
nostic aspects. replaced.
Definition of terms: toward a uniform nomen- Microdysgenesis. This term has been the focus of
clature. The first issue debated was the preferred significant confusion since it was proposed original-
denomination for this entire group of entities. There ly.43 Some authors have used the term to describe
are “developmental” factors that may be independent subtle derangements of focal cortical architecture
of the mechanism of injury (genetic, intrauterine, or such as 1) cortical laminar disorganization; 2) single
even perinatal) and that substantially affect cortical (or small aggregates of) heterotopic white matter
mantle formation.36,37 Because one or more of the neurons and neurons in the molecular layer; 3) per-
mechanisms important in corticogenesis can be af- sistent subpial granular layer; and 4) marginal glio-
fected and because even the malpositioning of nodu- neuronal heterotopia.41 In contrast, others have used
lar or laminar aggregates of neuroblasts and glial the term microdysgenesis to describe any type of
cells in heterotopic positions actually represent in- MRI-negative MCD.44 Because many instances of
terferences with cortical formation (these cells were MRI-negative MCDs can be associated with severe
destined originally for the cerebral cortex), the panel histopathologic abnormalities, including dysplastic
agreed with the denomination “malformations due to neurons and balloon cells, there is a clear histologic
abnormal cortical development.” Accordingly, the lack of congruence between the two uses of the term
panel suggested that the denomination “cortical dys- microdysgenesis.22,26,45-47 The panel recommended
plasias” should be applied only to the subtype of that the use of the term microdysgenesis should be
MCD in which the developmental abnormality is abandoned. Because most of the mild abnormalities
strictly or mostly intracortical. Thus, FCD would be reviewed by Mischel et al.41 involve cortical layer I, a
a good term within this framework only. Additional proposal was made to subdivide the mildest forms of
subdivision of FCD based on histologic/cellular char- MCD into those characterized by ectopically placed
acteristics will be presented. Likewise, the term neurons in or adjacent to layer I, and those in which
“neuronal migration disorder,” historically applied to abnormalities are outside layer I (see below).
all forms of MCD in the early 1990s,8,9 would suggest
that all MCDs were caused by predominant interfer- Cellular abnormalities. Dysmorphic neurons.
ences with migratory mechanisms affecting cortical These are misshapen cells with abnormal orienta-
neuronal precursors. It is clear that other pathoge- tion, size, cytoskeletal structure, and atypical den-
netic mechanisms apply as well; therefore, NMDs dritic processes. Nissl substance can be seen in
are more correctly considered a subtype of MCD. clumps, and the cells are rich in cytoplasmic neuro-
Moreover, MCD would be descriptive of the micro- filaments (SMI 31; figure 1).48,49
dysgeneses that were proposed originally by Balloon cells. These are abnormal cellular ele-
Meencke et al.43 to describe minimal, subtle abnor- ments with a thin membrane; pale, glassy, and eo-
March 2004 NEUROLOGY 62(Suppl 3) S3
morphic or giant but sometimes are seen in association
with giant or dysmorphic neurons. They are occasion-
ally the most common cell types in macroscopically vis-
ible heterotopic nodules.7,49
(Microscopic) neuronal heterotopias. These
microscopic abnormalities are mainly caused by ar-
chitectural disorganization. They are clusters of mis-
placed neurons. Conversely, the macroscopic
heterotopia (periventricular, subcortical nodular,
and band heterotopia) are grossly apparent well-
defined abnormalities of neuroblast migration (see
below).
Histopathology of FCDs. As discussed previ-
Figure 2. H-E staining shows a large balloon cell in the ously, there are several cellular elements, which may
subcortical white matter. Note the large opalescent cyto- occur in variable combinations, leading to specific
plasm and the eccentric nucleus; scale bar, 100 m. histopathologic features in cortical dysplastic lesions.
There is increasing information on correlations be-
sinophilic cytoplasm; and eccentric nucleus (or tween the histopathologic and electroclinical and
nuclei, because some are multinucleated). Balloon MRI abnormalities of FCD.2,46,51-55 Thus, the panel
cells usually are of increased size compared with decided to re-evaluate the several histopathologic
gemistocytic astrocytes. Previous immunocytochemi- scenarios that have been subsumed under the gen-
cal studies have shown that these cells have neuro- eral term “focal cortical dysplasias,” with a view to a
nal or glial characteristics.49,50 Most balloon cells are more clinically meaningful classification.
vimentin positive, but others are glial (e.g., glial Over the years, there has been some degree of het-
fibrillary acidic protein) or neuron-specific enolase/ erogeneity in the clinical, surgical, and histopathologic
MAP/NeuN-immunoreactive (Najm et al., personal literature, and terms like “focal cortical dysplasia,”
communication).49 These data suggest some degree of “mild cortical dysplasia,” “Taylor-type focal cortical
heterogeneity among the cells with partial commit- dysplasia,” “balloon cell dysplasia,” “non– balloon cell
ment toward glial or neuronal differentiation (figure 2). dysplasia,” and “microdysgenesis” all have been ap-
Giant neurons. These are neurons of increased plied to describe architectural and cellular abnormali-
size (compared with layer V pyramidal neurons) with ties of the cortical mantle.5,16,44,46,48,55,56 For example,
central nuclei. However, they preserve a pyramidal some authors use the descriptor Taylor-type FCD only
morphology (i.e., are not dysmorphic) and do not when balloon cells are present,16,57 whereas others, in-
overexpress cytoplasmic neurofilaments (figure 3). cluding Taylor et al.3 in their original report, include
Immature neurons. These are round (or oval) some patients whose lesions had dysmorphic neurons
cells, all homogeneous, with a large (immature) nu- but lacked balloon cells. Although the panel accepted
cleus and a thin rim of cytoplasm. They are not dys- that a definitive understanding of the relevance of each
cell type or architectural abnormality among the vari-
ous possible combinations relies on further develop-
ments on the mechanisms of corticogenesis and their
relation to clinical and imaging findings, a tentative
practical approach was attempted.
As a first step, it was consensually accepted that
one or more of the following might be present in
these lesions: dyslamination and other mild abnor-
malities (architectural abnormalities), “immature”
neurons, giant neurons, dysmorphic neurons, and
balloon cells. The most frequent histopathologic pic-
tures combining these elements then were agreed on
and considered to be the following.
Isolated architectural abnormalities (dyslamina-
tion). These are intracortical lesions that are charac-
terized by dyslamination and columnar disorganiza-
tion. These lesions represent the mildest end of the
histopathologic spectrum of FCD and may most closely
approximate the original description of microdysgen-
Figure 3. H-E staining shows a giant neuron with central esis. In the medial temporal lobe, particularly in the
nucleus. Note the presence of smaller dysmorphic neurons; hippocampus, abnormalities of the infolding of the den-
scale bar, 100 m. tate gyrus and focal dyslamination may occur.58
S4 NEUROLOGY 62(Suppl 3) March 2004
Architectural abnormalities associated with giant
neurons. In these lesions, the defining abnormality
is the presence of giant neurons. These lesions do not
contain dysmorphic or balloon cells. Whether the
presence of these cells has any clinical meaning and
thus differentiates the lesions from those harboring
only dyslamination is unclear.
Architectural abnormalities associated with dys-
morphic neurons. Irrespective of the occasional co-
occurrence of giant or immature neurons, the Figure 4. Cresylecht violet staining of sections represent-
hallmark of these lesions is the presence of clearly ing normal neocortex and type I, type IIA, and type IIB
dysmorphic neurons as defined previously.48,49 Accu- malformations of cortical development; scale bar, 100 m.
mulation of neurofilaments within neuronal cyto-
plasm of these cells leads to distorted morphology of
the perikarya, proximal axons, and dendrites. It is
debate on the role of these mild changes in the cau-
theoretically conceivable that these reflect more se-
sation of epilepsy in general but especially when the
vere abnormalities from a histopathologic stand-
histologic abnormalities are found in mesial tempo-
point.41 In the original publication of Taylor et al.,3 4
ral structures, leading to microscopic heterotopia in
of 10 patients had this histopathologic picture.
the dentate or parahippocampal gyri.60,61 Likewise,
Architectural abnormalities associated with dys-
the association of mesial limbic malformations with
morphic neurons and balloon cells. These lesions
schizophrenia and autism has attracted the atten-
are characterized mainly by the presence of balloon
tion of nonepileptologists to the putative clinical con-
cells that are intermixed typically with dysmorphic
sequences of mild MCD.62-64
neurons in patients with severe architectural disor-
ganization. Six of the 10 original patients reported FCDs (figure 4)
by Taylor et al.3 had a similar histopathologic pat- Type I: no dysmorphic neurons or balloon cells
tern. These lesions are considered to represent the
most severe end of the spectrum of histopathologic Type IA: isolated architectural abnormalities
abnormalities of FCD.41 (dyslamination, accompanied or not by other
There is preliminary evidence that the presence of abnormalities of mild MCD)
dysmorphic neurons, with or without balloon cells, is Type IB: architectural abnormalities, plus giant
associated with higher degrees of epileptogenicity.2 or immature, but not dysmorphic neurons
Moreover, recent studies suggest that the main his- Structural imaging: it is unclear at the time of this
topathologic subtypes that show MRI abnormalities report whether type I FCD as defined here can
are those that contain dysmorphic neurons with or be identified in vivo by current MRI techniques.
without balloon cells.4,46,47,54 These results suggest Should a common nomenclature be used by vari-
the separation of the histologic subtypes as delin- ous centers, it is likely that imaging-histo-
eated will allow much better electroclinical, imaging, pathologic correlations soon will clarify this issue.
and histopathologic correlations. Histopathology: as described previously
A classification scheme: imaging, histopathol- Potential clinical relevance. It is likely that some
ogy, and potential clinical relevance. Consider- of these patients will have epilepsy, whereas others
ing the definition of terms and the re-evaluation of will not; those without epilepsy may be either
the histopathologic scenarios mentioned here, the asymptomatic or instead seek treatment for learning
following classification is proposed. disorders or other types of cognitive impairment.
There are no specific data delineating a clinical or
Mild MCD
neurophysiologic profile of patients with epilepsy
Type I: with ectopically placed neurons in or adja- and type IA/B FCDs. Because hitherto most of these
cent to layer I mild abnormalities defy in vivo imaging recognition,
Type II: with microscopic neuronal heterotopia the only available evidence is from patients undergo-
outside layer I ing epilepsy surgery in whom such mild abnormali-
Structural imaging: both types probably are not ties were the only histopathologic finding.5,55 This
detectable by current MRI techniques suggests that at least some patients with type IA/B
FCD can have medically refractory epilepsy. How-
Histopathology: as described previously
ever, whether this is a common occurrence or repre-
Potential clinical relevance. It has been shown sents only the most severe end of a spectrum is
that these mild MCDs may be related to epilepsy and unclear. Interestingly, surgical patients in whom
other behavioral and cognitive abnormalities.44,59-61 these mild MCDs were found retrospectively tend to
Because diagnosis usually is retrospective, clear clin- have much better results compared with the surgical
ical and epileptic profiles of patients with these mild results obtained from patients with other types of
malformations are not available. Thus, there is some FCDs.
March 2004 NEUROLOGY 62(Suppl 3) S5
Type II: Taylor-type FCD (dysmorphic neurons Structural imaging and histopathology. Both le-
without or with balloon cells) sions usually are restricted to the cortex and may
Type IIA: architectural abnormalities with dys- present a combination of cystic and calcified areas.
morphic neurons but without balloon cells Perhaps the most striking imaging aspect is that the
MRI signal often is irregular and poorly delineated,
Type IIB: architectural abnormalities with dys-
attesting to the presence of different histopathologic
morphic neurons and balloon cells
elements and the association of perilesional dysplas-
Structural imaging: these are the focal lesions tic and immediately subcortical heterotopic cells.
most commonly identified on MRI. However, one There is no perilesional edema or mass effect.40,72
should be aware that several different imaging Clinical relevance. DNETs and gangliogliomas
possibilities might be observed in patients with are (with rare exception) benign lesions from an on-
Taylor-type FCD. MRI can be either normal,45,47 cologic point of view. However, they often are associ-
despite the use of high-resolution techniques, or ated with medically refractory partial seizures,
may demonstrate one or more of the following which usually manifest clinically before 20 years of
characteristics: 1) focal areas of increased corti- age. Patients with DNETs and epilepsy may be
cal thickness;46,47 2) blurring of the cortex (gray)/ cured with surgery, providing complete resection is
white matter junction;51,54 3) increased signal on feasible. Remaining tumoral or dysplastic tissue may
T2-weighted, proton density, or fluid-attenuated be associated with persistent seizures, despite major
inversion recovery sequences (more likely to oc- lesion resection.40,72
cur in balloon cell-containing lesions);51,54 and 4)
extension of cortical tissue with increased signal Challenges for the future. This report repre-
from the surface to the ventricle (transmantle sents an attempt toward a simple yet practical classi-
dysplasia).65-67 fication for FCDs that may be beneficial for clinicians
Histopathology: as detailed previously and researchers who are interested in the management
of FCDs and an understanding of mechanisms by
Potential clinical relevance. Type IIA/B FCDs which they cause epilepsy. Some imaging and his-
are characterized by truly abnormal, grossly dysmor- topathologic correlations were suggested, but there has
phic cellular elements, which are accompanied by un- been no attempt to include an embryologic perspective
questionable abnormalities in inhibitory and excitatory in the classification. It is likely that advances in the
neurotransmission. Data collected through immunocy- molecular neurobiology of these disorders will signifi-
tochemical studies support an increase in excitatory cantly change our views in terms of pathogenesis. To
amino acid neurotransmission and an overall decrease further understand these disorders and to validate the
in intralesional and perilesional inhibition.16,48,49 The usefulness of this proposed classification, there is need
net result is a high degree of intrinsic epileptogenicity, for the following: 1) clinical-electrical-pathologic corre-
which has been demonstrated by experimental and lations in patients with epilepsy who are undergoing
clinical studies.22,23,26,42,68,69 Most patients diagnosed by electrocorticographic and depth electrode recording
imaging studies (see above) as having lesions identi- evaluations;73 2) imaging-pathologic-functional correla-
fied as type IIA/B FCD have medically intractable tions based on careful studies of surgically resected
partial epilepsy, with frequently disabling motor and cortical samples; and 3) cellular-molecular studies of
secondary generalized seizures. Many patients have the mechanisms of epileptogenicity through direct cor-
a history of status epilepticus, including epilepsia relation with electrocorticographic data obtained
partialis continua, and scalp EEG and acute electro- through invasive recordings.18
corticography often show continuous spiking or other
highly epileptogenic patterns, attesting to some type Note added in proof. Recent utilization of this classification
framework has generated initial data suggesting that the different
of re-entrant excitatory circuitry unopposed by faulty types of FCD indeed tend to be associated with some specific
inhibition.26,52,55 These patients often are correctly di- anatomical, clinical, electrographic, and imaging characteris-
agnosed before surgery, but surgical results still are tics.74,75 Thus, Type I focal cortical dysplastic lesions have been
not fully satisfactory in many of them. Issues related shown to be most often localized to the temporal lobes, to lack
highly specific electrographic patterns, and to present on MRI as
to a preferential localization around the perirolandic hypoplasia of the temporal pole and/or increased signal in the
cortex and to a microscopic extension of abnormal white matter core, with poorly defined limits. On the other hand,
tissue beyond the MRI lesional margins often are Type II (Taylor type) FCD has been increasingly shown to repre-
sent an extratemporal entity, with lesions localized to one of four
mentioned to explain unsatisfactory results. major anatomical subcompartments: frontal lobe only, fronto-
Dysplastic tumors. There are at least two types central, peri-rolandic, or in the posterior quadrant. In addition, it
of tumor that may represent a more extreme end of has been confirmed that these lesions are frequently associated
the histopathologic spectrum of FCDs. Dysembryo- with ictal-like patterns or direct cortical recordings.22,76,77 Finally, a
recent report advances one step further, suggesting that the sub-
plastic neuroepithelial tumors (DNETs) and ganglio- divisions of Type II FCD may be differently related to ictal gener-
gliomas may be associated with surrounding cortical ation and preservation of function.78 In patients with peri-rolandic
regions displaying abnormal cytoarchitecture (dys- FCD, those portions of the lesions classified as Type IIA were
lamination) and large, at times dysmorphic, neurons shown to harbor the ictal onset zone and to retain motor function,
in contrast to those portions of the lesions containing balloon cells
and glial cells.70,71 Subcortical heterotopic neurons (Type IIB), which were functionally silent and not associated with
also can be seen.40,72 seizure onset. If confirmed, these findings may have a significant
S6 NEUROLOGY 62(Suppl 3) March 2004
impact in surgical planning, and will emphasize even more the 28. Hirabayashi S, Binnie C, Janota I, Polkey C. Surgical treatment of
need for in vivo MRI identification of subtypes of FCD. epilepsy due to cortical dysplasia: clinical and EEG findings. J Neurol
Neurosurg Psychiatry 1993;56:765–770.
29. Najm I, Bingaman W, Luders H. The use of subdural grids in the
management of focal malformations due to abnormal cortical develop-
References ment. Neurosurg Clin N Am 2002;13:87–92.
30. Granata T, Farina L, Faiella A, et al. Familial schizencephaly associ-
1. Barkovich A, Kuzniecky R, Dobyns W, Jackson G, Becker L, Evrard P.
ated with EMX2 mutation. Neurology 1997;48:1403–1406.
A classification scheme for malformations of cortical development. Neu-
31. Kato M, Kimura T, Lin C, et al. A novel mutation of the doublecortin
ropediatrics 1996;27:59 – 63.
gene in Japanese patients with X-linked lissencephaly and subcortical
2. Palmini A. Disorders of cortical development. Curr Opin Neurol 2000;
13:183–192. band heterotopia. Hum Genet 1999;104:341–344.
3. Taylor DFM, Bruton C, Corsellis J. Focal dysplasia of the cerebral 32. Roper S, Gilmore R, Houser C. Experimentally induced disorders of
cortex in epilepsy. J Neurol Neurosurg Psychiatry 1971;34:369 –387. neuronal migration produce an increased propensity for electrographic
4. Adamsbaum CRO, Cohen PA, Delalande O, Fohlen M, Kalifa G. Focal seizures in rats. Epilepsy Res 1995;21:205–219.
cortical dysplasia and hemimegalencephaly: histological and neuroim- 33. Roper S, King M, Abraham L, Boillot M. Disinhibited in vitro neocorti-
aging correlations. Pediatr Radiol 1998;28:583–590. cal slices containing experimentally induced cortical dysplasia demon-
5. Kuzniecky R, Garcia J, Faught E, Morawetz R. Cortical dysplasia in strate hyperexcitability. Epilepsy Res 1997;26:443– 449.
temporal lobe epilepsy: magnetic resonance imaging correlations. Ann 34. Kondo S, Najm I, Kunieda T, Perryman S, Yacubova K, Luders H.
Neurol 1991;29:293–298. Electroencephalographic characterization of an adult rat model of
6. Roper S. In utero irradiation of rats as a model of human cerebrocorti- radiation-induced cortical dysplasia. Epilepsia 2001;42:1221–1227.
cal dysgenesis: a review. Epilepsy Res 1998;32:63–74. 35. Palmini A, Andermann E, Andermann F. Prenatal events and genetic
7. Van BP, David P, Gillain C, et al. Perisylvian dysgenesis. Clinical, factors in epileptic patients with neuronal migration disorders. Epilep-
EEG, MRI and glucose metabolism features in 10 patients. Brain 1998; sia 1994;35:965–973.
121:2229 –2238. 36. Lombroso C. Can early postnatal closed head injury induce cortical
8. Palmini A, Andermann F, de Grissac H, et al. Stages and patterns of dysplasia? Epilepsia 2000;41:245–253.
centrifugal arrest of diffuse neuronal migration disorders. Dev Med 37. Sarnat H. Disturbances of late neuronal migrations in the perinatal
Child Neurol 1993;35:331–339. period. Am J Dis Child 1987;141:969 –980.
9. Simone I, Federico F, Tortorella C, et al. Metabolic changes in neuronal 38. Palmini A, Andermann F, Olivier A, et al. Neuronal migration disor-
migration disorders: evaluation by combined MRI and proton MR spec- ders: a contribution of modern neuroimaging to the etiologic diagnosis
troscopy. Epilepsia 1999;40:872– 879. of epilepsy. Can J Neurol Sci 1991;18:580 –587.
10. Palmini A, Andermann F, Aicardi J, et al. Diffuse cortical dysplasia, or 39. Palmini A, Gambardella A, Andermann F, et al. Intrinsic epileptogenic-
the “double cortex” syndrome: the clinical and epileptic spectrum in 10 ity of human dysplastic cortex as suggested by corticography and surgi-
patients. Neurology 1991;41:1656 –1662. cal results. Ann Neurol 1995;37:476 – 487.
11. Palmini A, Andermann F, Olivier A, Tampieri D, Robitaille Y. Focal 40. Raymond A, Fish D, Sisodiya S, Alsanjari N, Stevens J, Shorvon S.
neuronal migration disorders and intractable partial epilepsy: results of Abnormalities of gyration, heterotopias, tuberous sclerosis, focal corti-
surgical treatment. Ann Neurol 1991;30:750 –757. cal dysplasia, microdysgenesis, dysembryoplastic neuroepithelial tu-
12. Barkovich A, Chuang S, Norman D. MR of neuronal migration anoma- mour and dysgenesis of the archicortex in epilepsy. Clinical, EEG and
lies. AJR Am J Roentgenol 1988;150:179 –187. neuroimaging features in 100 adult patients. Brain 1995;118:629 – 660.
13. Gleeson J, Minnerath S, Fox J, et al. Characterization of mutations in 41. Mischel P, Nguyen L, Vinters H. Cerebral cortical dysplasia associated
the gene doublecortin in patients with double cortex syndrome. Ann with pediatric epilepsy. Review of neuropathologic features and pro-
Neurol 1999;45:146 –153. posal for a grading system. J Neuropathol Exp Neurol 1995;54:137–153.
14. Fox J, Lamperti E, Eksioglu Y, et al. Mutations in filamin 1 prevent 42. Morioka T, Nishio S, Ishibashi H, et al. Intrinsic epileptogenicity of
migration of cerebral cortical neurons in human periventricular hetero- focal cortical dysplasia as revealed by magnetoencephalography and
topia. Neuron 1998;21:1315–1325. electrocorticography. Epilepsy Res 1999;33:177–187.
15. Yamanouchi H, Jay V, Otsubo H, Kaga M, Becker L, Takashima S. 43. Meencke H, Janz D. The significance of microdysgenesia in primary
Early forms of microtubule-associated protein are strongly expressed in generalized epilepsy: an answer to the considerations of Lyon and
cortical dysplasia. Acta Neuropathol (Berl) 1998;95:466 – 470. Gastaut. Epilepsia 1985;26:368 –371.
16. Ferrer I, Pineda M, Tallda M, et al. Abnormal local circuit neurons in 44. Keene D, Jimenez C, Ventureyra E. Cortical microdysplasia and surgi-
epilepsia partialis continua associated with focal cortical dysplasia. cal outcome in refractory epilepsy of childhood. Pediatr Neurosurg
Acta Neuropathol 1992;83:647– 652. 1998;29:69 –72.
17. Ying Z, Babb T, Comair Y, Bingaman W, Bushey M, Touhalisky K. 45. Desbiens R, Berkovic S, Dubeau F, et al. Life-threatening focal status
Induced expression of NMDAR2 proteins and differential expression of epilepticus due to occult cortical dysplasia. Arch Neurol 1993;50:695–
NMDAR1 splice variants in dysplastic neurons of human epileptic neo- 700.
cortex. J Neuropathol Exp Neurol 1998;57:47– 62. 46. Chan S, Chin S, Nordli D, Goodman R, DeLaPaz R, Pedley T. Prospec-
18. Najm I, Ying Z, Babb T, et al. NMDA receptor 2A/B subtype differential tive magnetic resonance imaging identification of focal cortical dyspla-
expression in human cortical dysplasia: correlation with in situ epilep- sia, including the non-balloon cell subtype. Ann Neurol 1998;44:749 –
togenicity. Epilepsia 2000;41:971–976.
757.
19. Chevassus-Au-Louis N, Congar P, Represa A, Ben-Ari Y, Gaiarsa
47. Bastos A, Comeau R, Andermann F, et al. Diagnosis of subtle focal
J. Neuronal migration disorders: heterotopic neocortical neurons in
dysplastic lesions: curvilinear reformatting from three-dimensional
CA1 provide a bridge between the hippocampus and the neocortex. Proc
magnetic resonance imaging. Ann Neurol 1999;46:88 –94.
Natl Acad Sci USA 1998;95:10263–10268.
48. Spreafico R, Battaglia G, Arcelli P, et al. Cortical dysplasia: an immu-
20. Holmes G, Sarkisian M, Ben-Ari Y, Liu Z, Chevassus-Au-Louis N. Con-
nocytochemical study of three patients. Neurology 1998;50:27–36.
sequences of cortical dysplasia during development in rats. Epilepsia
49. Spreafico R, Pasquier B, Minotti L, et al. Immunocytochemical investi-
1999;40:537–544.
21. Chevassus-au-Louis N, Baraban S, Gaiarsa J, Ben-Ari Y. Cortical mal- gation on dysplastic human tissue from epileptic patients. Epilepsy Res
formations and epilepsy: new insights from animal models. Epilepsia 1998;32:34 – 48.
1999;40:811– 821. 50. Barbosa-Coutinho L, Hilbig A, Calcagnotto M, et al. Neuropathology of
22. Palmini A, Gambardella A, Andermann F, et al. Intrinsic epileptogenic- hard to control epilepsy. Study of 300 consecutive cases [Portuguese].
ity of human dysplastic cortex as suggested by corticography and surgi- Arq Neuropsiquiatr 1999;57:405–14.
cal results. Ann Neurol 1995;37:476 – 487. 51. Bronen R, Vives K, Kim J, Fulbright R, Spencer S, Spencer D. Focal
23. Gambardella A, Palmini A, Andermann F, et al. Usefulness of focal cortical dysplasia of Taylor, balloon cell subtype: MR differentiation
rhythmic discharges on scalp EEG of patients with focal cortical dyspla- from low-grade tumors. AJNR Am J Neuroradiol 1997;18:1141–1151.
sia and intractable epilepsy. Electroencephalogr Clin Neurophysiol 52. Palmini A, da Costa J, Calcagnotto M, Pagliolo-Neto E, Paglioli E,
1996;98:243–249. Coutinho L. Patients with specific histopathological types of cortical
24. Dubeau F, Palmini A, Fish D, et al. The significance of electrocortico- dysplasia have specific degrees of severity of the epileptic condition.
graphic findings in focal cortical dysplasia: a review of their clinical, Epilepsia 1997;38:5.
electrophysiological and neurochemical characteristics. Electroencepha- 53. Guerrini R, Genton P, Bureau M, et al. Multilobar polymicrogyria,
logr Clin Neurophysiol Suppl 1998;48:77–96. intractable drop attack seizures, and sleep-related electrical status epi-
25. Guerrini R, Dravet C, Raybaud C, et al. Epilepsy and focal gyral anom- lepticus. Neurology 1998;51:504 –512.
alies detected by MRI: electroclinico-morphological correlations and fol- 54. Lee B, Schmidt R, Hatfield G, Bourgeois B, Park T. MRI of focal cortical
low up. Dev Med Child Neurol 1992;34:706 –718. dysplasia. Neuroradiology 1998;40:675– 683.
26. Palmini A, Gambardella A, Andermann F, et al. Operative strategies 55. Rosenow F, Lüders H, Dinner D, et al. Histopathological correlates of
for patients with cortical dysplastic lesions and intractable epilepsy. epileptogenicity as expressed by electrocorticographic spiking and sei-
Epilepsia 1994;35:S57–S71. zure frequency. Epilepsia 1998;39:850 – 856.
27. Palmini A, Andermann F, Olivier A, et al. Focal neuronal migration 56. Palmini A, Andermann F, Olivier A, et al. Focal neuronal migration
disorders and intractable partial epilepsy: a study of 30 patients. Ann disorders and intractable partial epilepsy: a study of 30 patients. Ann
Neurol 1991;30:741–749. Neurol 1991;30:741–749.
March 2004 NEUROLOGY 62(Suppl 3) S7
57. Garbelli R, Munari C, De Biasi S, et al. Taylor’s cortical dysplasia: a 69. Avoli M, Bernasconi A, Mattia D, Olivier A, Hwa G. Epileptiform dis-
confocal and ultrastructural immunohistochemical study. Brain Pathol charges in the human dysplastic neocortex: in vitro physiology and
1999;9:445– 461. pharmacology. Ann Neurol 1999;46:816 – 826.
58. Lehericy S, Dormont D, Semah F. Developmental abnormalities of the 70. Wolf HK, Müller MB, Spanle M, et al. Ganglioglioma: a detailed his-
medial temporal lobe in patients with temporal lobe epilepsy. AJNR topathological and immunocytochemical analysis of 61 cases. Acta Neu-
Am J Neuroradiol 1995;16:617– 626. ropathol 1994;88:166 –173.
59. Raymond G, Bauman M, Kemper T. Hippocampus in autism: a Golgi 71. Prayson RA, Khajavi K, Comair YG. Cortical architectural abnormali-
analysis. Acta Neuropathol (Berl) 1996;91:117–119. ties and MIB1 immunoreactivity in gangliogliomas: a study of 60 pa-
60. Akil M, Lewis D. Cytoarchitecture of the entorhinal cortex in schizo- tients with intracranial tumors. J Neuropathol Exp Neurol 1995;54:
phrenia. Am J Psychiatry 1997;154:1010 –1012. 513–520.
61. Galaburda A, Sherman G, Rosen G, Aboitiz F, Geschwind N. Develop- 72. Daumas-Duport CSB, Scheithauer BW, Chodkiewicz JP, et al. Dysem-
mental dyslexia: four consecutive patients with cortical anomalies. Ann bryoplastic neuroepithelial tumor: a surgically curable tumor of young
Neurol 1985;18:222–233. patients with intractable partial seizures. Report of thirty-nine cases.
62. Akbarian S, Bunney W, Potkin S, et al. Altered distribution of Neurosurgery 1988;23:545–556.
nicotinamide-adenine dinucleotide phosphate-diaphorase cells in fron- 73. Munari C, Francione S, Kahane P, et al. Usefulness of stereo EEG
tal lobe of schizophrenics implies disturbances of cortical development.
investigations in partial epilepsy associated with cortical dysplastic
Arch Gen Psychiatry 1993;50:169 –177.
lesions and gray matter heterotopia. In: Guerrini R, Andermann F,
63. Bunney B, Potkin S, Bunney W. New morphological and neuropatholog-
Canapicchi R, Roger J, Zifkin B, Pfanner P, eds. Dysplasias of Cerebral
ical findings in schizophrenia: a neurodevelopmental perspective. Clin
Cortex and Epilepsy. Philadelphia: Lippincott-Raven, 1995:383–394.
Neurosci 1995;3:81– 88.
64. Courchesne E. Brainstem, cerebellar and limbic neuroanatomical ab- 74. Tassi L, Colombo N, Garbelli R, et al. Focal cortical dysplasia: neuro-
normalities in autism. Curr Opin Neurobiol 1997;7:269 –278. pathological subtypes, EEG, neuroimaging and surgical outcome. Brain
65. Barkovich A, Kuzniecky R, Bollen A, Grant P. Focal transmantle dys- 2002;125:1719 –1732.
plasia: a specific malformation of cortical development. Neurology 1997; 75. Colombo N, Tassi L, Galli C, et al. Focal cortical dysplasias: MR imag-
49:1148 –1152. ing, histopathologic, and clinical correlations in surgically treated pa-
66. Barkovich A, Kuzniecky R, Bollen A, Grant P. Focal transmantle dys- tients with epilepsy. AJNR Am J Neuroradiol 2003;24:724 –733.
plasia: a specific malformation of cortical development. Neurology 1997; 76. Chassoux F, Devaux B, Landré E, et al. Stereoelectroencephalography
49:1148 –1152. in focal cortical dysplasia: a 3D approach to delineating the dysplastic
67. Bronen R, Spencer D, Fulbright R. Cerebrospinal fluid cleft with corti- cortex. Brain Dev 2000;123:1733–1755.
cal dimple: MR imaging marker for focal cortical dysgenesis. Radiology 77. Ferrier CH, Alarcon G, Engelsman J, et al. Relevance of residual histo-
2000;214:657– 663. logic and electrocorticographic abnormalities for surgical outcome in
68. Dubeau F, Palmini A, Fish D, et al. The significance of electrocortico- frontal lobe epilepsy. Epilepsia 2001;42:363–371.
graphic findings in focal cortical dysplasia: a review of their clinical, 78. Boonyapisit K, Najm I, Klem G, et al. Epileptogenicity of focal malforma-
electrophysiological and neurochemical characteristics. Electroencepha- tions due to abnormal cortical development: direct electrocorticographic-
logr Clin Neurophysiol Suppl 1998;48:77–96. histopathologic correlations. Epilepsia 2003;44:69 –76.
S8 NEUROLOGY 62(Suppl 3) March 2004
Potrebbero piacerti anche
- Terminology and Classification of The Cortical Dysplasias PalminiDocumento9 pagineTerminology and Classification of The Cortical Dysplasias PalminiAyhan BölükNessuna valutazione finora
- Malformaciones Cortical. 2pdfDocumento37 pagineMalformaciones Cortical. 2pdfEsthibaliz RdzNessuna valutazione finora
- Definitions and Classification of Malformations of Cortical Development Practical GuidelinesDocumento21 pagineDefinitions and Classification of Malformations of Cortical Development Practical GuidelinesAhmedHiddNessuna valutazione finora
- Developmental Anomalies of The Brain in Mental RetardationDocumento10 pagineDevelopmental Anomalies of The Brain in Mental RetardationKaterina ChatzNessuna valutazione finora
- Proforma For Registration of Subject For Dissertation: TH RDDocumento10 pagineProforma For Registration of Subject For Dissertation: TH RDHariNessuna valutazione finora
- Inflammatory Cortical Demyelination in Early Multiple SclerosisDocumento10 pagineInflammatory Cortical Demyelination in Early Multiple SclerosisWulan AzmiNessuna valutazione finora
- MRI in Motor DelayDocumento9 pagineMRI in Motor DelayKriti ShuklaNessuna valutazione finora
- E200032 FullDocumento13 pagineE200032 FullAlice MaulisovaNessuna valutazione finora
- 人工智能在神经病理学中的应用:基于深度学习的tau蛋白病变评估Documento23 pagine人工智能在神经病理学中的应用:基于深度学习的tau蛋白病变评估meiwanlanjunNessuna valutazione finora
- A Magnetic Resonance Approach To Metabolic Disorders in ChildhoodDocumento12 pagineA Magnetic Resonance Approach To Metabolic Disorders in ChildhoodAna TelloNessuna valutazione finora
- Autosomal Recessive Primary Microcephaly (MCPH) : A Review of Clinical, Molecular, and Evolutionary FindingsDocumento12 pagineAutosomal Recessive Primary Microcephaly (MCPH) : A Review of Clinical, Molecular, and Evolutionary FindingsAli HaiderNessuna valutazione finora
- Displasia Cortical de TaylorDocumento11 pagineDisplasia Cortical de TaylorOscar F. Ochoa RuizNessuna valutazione finora
- Hypomyelinating Leukodystrophies Translational Research Progress and ProspectsDocumento15 pagineHypomyelinating Leukodystrophies Translational Research Progress and ProspectsgomaNessuna valutazione finora
- OrganoidesDocumento10 pagineOrganoidesg.colleenNessuna valutazione finora
- Krabbe DiseaseDocumento6 pagineKrabbe DiseaseUrko GoroquietaNessuna valutazione finora
- Zhang 2019Documento10 pagineZhang 2019NATALIA MARTINEZ CORDOBANessuna valutazione finora
- Neurology. Classification System For Malformations of Cortical Development (Barkovich Et Al.) PDFDocumento13 pagineNeurology. Classification System For Malformations of Cortical Development (Barkovich Et Al.) PDFJuan Pablo Anabalón SaavedraNessuna valutazione finora
- Abstract BookDocumento90 pagineAbstract BookPopescu RoxanaNessuna valutazione finora
- MB, Clinical Implication, Taylor, NatRevNeuro, 2012Documento12 pagineMB, Clinical Implication, Taylor, NatRevNeuro, 2012AbsjeyNessuna valutazione finora
- Detection of Cognitive Impairment in Multiple Sclerosis Based On P300 Event-Related PotentialDocumento8 pagineDetection of Cognitive Impairment in Multiple Sclerosis Based On P300 Event-Related Potentialzwecker4458Nessuna valutazione finora
- Clinicopathological Correlations in BehaviouralDocumento17 pagineClinicopathological Correlations in BehaviouralAlexandra CastellanosNessuna valutazione finora
- Brain 2009 Barkovich 3199 230 Neuroembyology1Documento32 pagineBrain 2009 Barkovich 3199 230 Neuroembyology1Azalia BahatNessuna valutazione finora
- 7 PDFDocumento22 pagine7 PDFAndrés MesaNessuna valutazione finora
- Winawer Et Al-2018-Annals of NeurologyDocumento14 pagineWinawer Et Al-2018-Annals of NeurologyAndoingNessuna valutazione finora
- MicrosDocumento11 pagineMicrosEka JuliantaraNessuna valutazione finora
- A Practical Approach To Diagnosis of Spinal DysraphismDocumento17 pagineA Practical Approach To Diagnosis of Spinal DysraphismSecret AccordNessuna valutazione finora
- Journal AlzheimerDocumento10 pagineJournal AlzheimerFaza KeumalasariNessuna valutazione finora
- Personal View: Graham Teasdale, Andrew Maas, Fiona Lecky, Geoff Rey Manley, Nino Stocchetti, Gordon MurrayDocumento11 paginePersonal View: Graham Teasdale, Andrew Maas, Fiona Lecky, Geoff Rey Manley, Nino Stocchetti, Gordon MurrayMariana PeredaNessuna valutazione finora
- Optic Nerve Glioma: Case Series With Review of Clinical, Radiologic, Molecular, and Histopathologic CharacteristicsDocumento5 pagineOptic Nerve Glioma: Case Series With Review of Clinical, Radiologic, Molecular, and Histopathologic CharacteristicsUtama Hadiputra SurbaktiNessuna valutazione finora
- Cirurgia EpilepsiaDocumento30 pagineCirurgia EpilepsiaSARANessuna valutazione finora
- Cerebellar Mutism SyndromeDocumento12 pagineCerebellar Mutism SyndromeshokoNessuna valutazione finora
- 2010 MayDocumento16 pagine2010 MayAli HaiderNessuna valutazione finora
- Neuromodulation For The Treatment of Prader-Willi Syndrome - A Systematic ReviewDocumento9 pagineNeuromodulation For The Treatment of Prader-Willi Syndrome - A Systematic ReviewCristina Sánchez MoralesNessuna valutazione finora
- Retinal Abnormatilites As A Diagnostic or Prognostic Marker of SchizophreniaDocumento6 pagineRetinal Abnormatilites As A Diagnostic or Prognostic Marker of SchizophreniatratrNessuna valutazione finora
- Ams Postmortem - GDocumento6 pagineAms Postmortem - GJUAN ANDRES GUARDIAS GARZONNessuna valutazione finora
- Corpus Callosotomy in Children and The Disconnection Syndromes: A ReviewDocumento9 pagineCorpus Callosotomy in Children and The Disconnection Syndromes: A ReviewCraig JohnsonNessuna valutazione finora
- Differential Diagnosis of Suspected Multiple Sclerosis - An Updated Consensus ApproachDocumento15 pagineDifferential Diagnosis of Suspected Multiple Sclerosis - An Updated Consensus ApproachInthe MOON youNessuna valutazione finora
- Limperopoulos Bolduc09 Neurodevelopmental Outcomes After CB Injury REVIEWDocumento12 pagineLimperopoulos Bolduc09 Neurodevelopmental Outcomes After CB Injury REVIEWEccoNessuna valutazione finora
- Bedeschi 2006Documento8 pagineBedeschi 2006Modou NianeNessuna valutazione finora
- The Molecular Pathology of Schizophrenia: An Overview of Existing Knowledge and New Directions For Future ResearchDocumento22 pagineThe Molecular Pathology of Schizophrenia: An Overview of Existing Knowledge and New Directions For Future ResearchJorge SalazarNessuna valutazione finora
- Miller DiekerDocumento8 pagineMiller DiekerJucsy JuxyNessuna valutazione finora
- What Have Organoids and Assembloids Taught Us About The Pat - 2023 - BiologicalDocumento10 pagineWhat Have Organoids and Assembloids Taught Us About The Pat - 2023 - Biologicalg.colleenNessuna valutazione finora
- Schizencefalia A Bibliographic Review of Clinical Aspects 379Documento3 pagineSchizencefalia A Bibliographic Review of Clinical Aspects 379Leidy FuentesNessuna valutazione finora
- 668 FullDocumento10 pagine668 FullfranciscoNessuna valutazione finora
- NEUROLOGY2014621771Documento13 pagineNEUROLOGY2014621771Alexandra SerbanNessuna valutazione finora
- Sca IiDocumento8 pagineSca IiAlfredo Enrique Marin AliagaNessuna valutazione finora
- Frisoni-11 Criterios ADDocumento4 pagineFrisoni-11 Criterios ADMARIA MONTSERRAT SOMOZA MONCADANessuna valutazione finora
- 1 s2.0 S0022510X23008559 MainDocumento2 pagine1 s2.0 S0022510X23008559 MainAmin AminiNessuna valutazione finora
- Ryan's Retina 7th Ed. Vol.3Documento1.064 pagineRyan's Retina 7th Ed. Vol.3karpathakimargaritaNessuna valutazione finora
- Neuropharmacology: Tjitske Kleefstra, Annette Schenck, Jamie M. Kramer, Hans Van BokhovenDocumento12 pagineNeuropharmacology: Tjitske Kleefstra, Annette Schenck, Jamie M. Kramer, Hans Van Bokhovenastir1234Nessuna valutazione finora
- tmp4D8B TMPDocumento2 paginetmp4D8B TMPFrontiersNessuna valutazione finora
- Ahmed-13 Taupatías Globulares GlialesDocumento8 pagineAhmed-13 Taupatías Globulares GlialesMARIA MONTSERRAT SOMOZA MONCADANessuna valutazione finora
- Pediatric Movement Disorders: Five New ThingsDocumento8 paginePediatric Movement Disorders: Five New ThingsAndrea PederziniNessuna valutazione finora
- Surgical Management of Spinal Dysraphism: Five - Year Experience in A Central HospitalDocumento5 pagineSurgical Management of Spinal Dysraphism: Five - Year Experience in A Central HospitalBhayu RizallinoorNessuna valutazione finora
- Deciphering Neurodegenerative Diseases Using Long-Read SequencingDocumento12 pagineDeciphering Neurodegenerative Diseases Using Long-Read SequencingShavana RajkumarNessuna valutazione finora
- Choroid Plexus Volume in Multiple Sclerosis Vs Neuromyelitis Optica Spectrum DisorderDocumento14 pagineChoroid Plexus Volume in Multiple Sclerosis Vs Neuromyelitis Optica Spectrum DisorderYaquelin del valle torres DomínguezNessuna valutazione finora
- Benedict 2020Documento12 pagineBenedict 2020HannaNessuna valutazione finora
- Epilepsia - 2022 - NajmDocumento21 pagineEpilepsia - 2022 - NajmFrancis CastellonNessuna valutazione finora
- Highlights in Neuro OphthalmologyDocumento2 pagineHighlights in Neuro OphthalmologyShruthi VMNessuna valutazione finora
- RMN 3TDocumento6 pagineRMN 3Tlucasher35Nessuna valutazione finora
- Dysembryoplastic Neuroepithelial Tumors in Childhood: Long-Term Outcome and Prognostic FeaturesDocumento7 pagineDysembryoplastic Neuroepithelial Tumors in Childhood: Long-Term Outcome and Prognostic Featureslucasher35Nessuna valutazione finora
- Cesare Lombroso y EpilepsiaDocumento5 pagineCesare Lombroso y Epilepsialucasher35Nessuna valutazione finora
- Barkovich Clasificación de DisplasiasDocumento15 pagineBarkovich Clasificación de Displasiaslucasher35Nessuna valutazione finora
- Epileptogenésis de Las DisplasiasDocumento5 pagineEpileptogenésis de Las Displasiaslucasher35Nessuna valutazione finora
- Manejo Neuroquirurgico de La Epilepsia PediátricaDocumento16 pagineManejo Neuroquirurgico de La Epilepsia Pediátricalucasher35Nessuna valutazione finora
- Displasia Tipo TaylorDocumento7 pagineDisplasia Tipo Taylorlucasher35Nessuna valutazione finora
- Displasia FrontalDocumento17 pagineDisplasia Frontallucasher35Nessuna valutazione finora
- Displasia Tipo TaylorDocumento7 pagineDisplasia Tipo Taylorlucasher35Nessuna valutazione finora
- Manejo Neuroquirurgico de La Epilepsia PediátricaDocumento16 pagineManejo Neuroquirurgico de La Epilepsia Pediátricalucasher35Nessuna valutazione finora
- Neuroimágenes de Displasias CorticalesDocumento3 pagineNeuroimágenes de Displasias Corticaleslucasher35Nessuna valutazione finora
- Cesare Lombroso y EpilepsiaDocumento5 pagineCesare Lombroso y Epilepsialucasher35Nessuna valutazione finora
- Barkovich Clasificación de DisplasiasDocumento15 pagineBarkovich Clasificación de Displasiaslucasher35Nessuna valutazione finora
- 3 Delinquent Mta Molinaetal07Documento13 pagine3 Delinquent Mta Molinaetal07lucasher35Nessuna valutazione finora
- 3-Year Follow-Up of The NIMH MTA StudyDocumento14 pagine3-Year Follow-Up of The NIMH MTA StudyFariNessuna valutazione finora
- Felbamato Pediatric - Neurology - 2010 - 42 - (6) 396Documento8 pagineFelbamato Pediatric - Neurology - 2010 - 42 - (6) 396lucasher35Nessuna valutazione finora
- 2 Growth Rates Mta36month Swansonetal07bDocumento13 pagine2 Growth Rates Mta36month Swansonetal07blucasher35Nessuna valutazione finora
- NeuromarketingDocumento10 pagineNeuromarketingmortruuu100% (1)
- Bipolar DisorderDocumento13 pagineBipolar Disorderapi-34875287550% (2)
- 3.visual Sign and Symptomps of Multiple System AtrophyDocumento9 pagine3.visual Sign and Symptomps of Multiple System AtrophyNia AnestyaNessuna valutazione finora
- Musculoskeletal Clinical Translation FrameworkDocumento1 paginaMusculoskeletal Clinical Translation FrameworkRafaelNessuna valutazione finora
- Multiple SclerosisDocumento2 pagineMultiple Sclerosisplethoraldork100% (5)
- Compediu TesteDocumento6 pagineCompediu TesteAlexandra TasmocNessuna valutazione finora
- Lambert-Eaton Myasthenic SyndromeDocumento5 pagineLambert-Eaton Myasthenic SyndromenoraNessuna valutazione finora
- Essay 2 False MemoriesDocumento1 paginaEssay 2 False Memoriesapi-545177972Nessuna valutazione finora
- Training To Optimize Performance Driving Reorganization?: Exercise and Functional in Stroke: NeuralDocumento10 pagineTraining To Optimize Performance Driving Reorganization?: Exercise and Functional in Stroke: NeuralPhooi Yee LauNessuna valutazione finora
- Artificial Neural NetworksDocumento8 pagineArtificial Neural NetworksPavan SaiNessuna valutazione finora
- Opioid Analgesics and AntagonistsDocumento18 pagineOpioid Analgesics and AntagonistsLaura KristyNessuna valutazione finora
- The Posterior Fossa VeinsDocumento24 pagineThe Posterior Fossa Veinsbodeadumitru9261100% (2)
- Neuroscience of Substance Abuse and DependenceDocumento62 pagineNeuroscience of Substance Abuse and Dependencedrkadiyala2100% (1)
- Second Periodical Test Science 6Documento12 pagineSecond Periodical Test Science 6Hardy Misagal100% (1)
- Visual Acuity and Retina-3Documento14 pagineVisual Acuity and Retina-3Vedehi BansalNessuna valutazione finora
- Presented by DR/ Nadia Mohamed: Lecturer of Psychiatric Nursing & Mental HealthDocumento46 paginePresented by DR/ Nadia Mohamed: Lecturer of Psychiatric Nursing & Mental HealthMariem BasmaNessuna valutazione finora
- CRANIOTOMYDocumento59 pagineCRANIOTOMYJhay LawrenceNessuna valutazione finora
- Q3 Science Reviewer - PopoDocumento10 pagineQ3 Science Reviewer - PopoXY PLAYZNessuna valutazione finora
- Idiopathic Intracranial Hypertension in University Hospital in Saudi Arabia, Retrospective StudyDocumento6 pagineIdiopathic Intracranial Hypertension in University Hospital in Saudi Arabia, Retrospective StudyIJAR JOURNALNessuna valutazione finora
- Module 9Documento28 pagineModule 9charlene rodicolNessuna valutazione finora
- Brain HemispheresDocumento7 pagineBrain Hemispheresyannie091Nessuna valutazione finora
- Pathophysiology of HydrocephalusDocumento3 paginePathophysiology of HydrocephalusJan Rae Barnatia AtienzaNessuna valutazione finora
- (CITATION Sar11 /L 1033) : 1. James - Lange TheoryDocumento5 pagine(CITATION Sar11 /L 1033) : 1. James - Lange TheorySHINGYNessuna valutazione finora
- Brainstem Gliomas: BackgroundDocumento10 pagineBrainstem Gliomas: Backgroundanak99Nessuna valutazione finora
- Do We Embody Second Language Evidence Fo PDFDocumento9 pagineDo We Embody Second Language Evidence Fo PDFChrist TorresNessuna valutazione finora
- ANA 6.01 General Somatic Afferents Dr. EsguerraDocumento22 pagineANA 6.01 General Somatic Afferents Dr. EsguerraNinna Ricci San JuanNessuna valutazione finora
- Brain Stem Evoked Response AudiometryDocumento2 pagineBrain Stem Evoked Response AudiometryPulkitNessuna valutazione finora
- Pearson Science New South Wales 9 Chapter 6 TestDocumento13 paginePearson Science New South Wales 9 Chapter 6 TestAbigail ScottNessuna valutazione finora
- Fix 2nd Announcement JogjaclanDocumento8 pagineFix 2nd Announcement JogjaclanHafida AuliaristaNessuna valutazione finora
- Syllabus DU FYUP PDFDocumento30 pagineSyllabus DU FYUP PDFSHRUTKIRTI SINGH 1951072Nessuna valutazione finora