Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Iras GT
Caricato da
ijudoptoDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Iras GT
Caricato da
ijudoptoCopyright:
Formati disponibili
Accuracy of IRAS GT interferometer
and potential acuity meter
prediction of visual acuity
after phacoemulsification
Prospective comparative study
Cécile Le Sage, MD, Christian Bazalgette, DBO, Bernard Arnaud, MD,
Clair-Florent Schmitt-Bernard, MD, PhD
ABSTRACT
Purpose: To assess and compare the accuracy of 2 methods of predicting visual acuity
after phacoemulsification.
Setting: Department of Ophthalmology, Montpellier, France.
Methods: This prospective study evaluated 47 eyes of 47 patients having uneventful
phacoemulsification over a 1-month period. All the patients had mild to moderate
cataract. Visual acuity recovery was predicted using the white-light IRAS GT姞 inter-
ferometer on the 3- and 8-degree wide test area and the Guyton-Minkowski potential
acuity meter (PAM). Best corrected visual acuity was evaluated 1 day before and
1 month after surgery.
Results: Both the interferometer and PAM underestimated the retinal visual capacity.
Three-degree white-light interferometry gave significantly better mean predicted results
than 8-degree interferometry and the PAM. There was no statistically significant dispar-
ity between predicted and postoperative results with 3-degree interferometry (1.04 ⫾
0.57 logMAR; – 0.09 ⫾ 0.27 decimal) (P ⫽ .0647) and a statistically significant disparity
with 8-degree interferometry (0.89 ⫾ 0.59 logMAR; – 0.13 ⫾ 0.27 decimal) and the PAM
(0.66 ⫾ 0.62 logMAR; – 0.22 ⫾ 0.24 decimal) (P ⫽ .0001). The predicted values were
widely dispersed; the correlation indices were 0.38 with the PAM (P ⫽ .091), 0.39 with
3-degree interferometry (P ⫽ .001), and 0.49 with 8-degree interferometry (P ⫽ .0005).
Conclusions: Three-degree white-light interferometry gave more accurate results than
8-degree interferometry and the PAM. The wide dispersion of results and unsatisfactory
correlation indices show the tests are poor predictors of individual acuity. They should
be used semiquantitatively and the results interpreted in relation to the clinical data.
Qualitative methods may be useful in confirming or refuting visual recovery capacity
ascertained by quantitative systems. J Cataract Refract Surg 2002; 28:131–138
© 2002 ASCRS and ESCRS
© 2002 ASCRS and ESCRS 0886-3350/02/$–see front matter
Published by Elsevier Science Inc. PII S0886-3350(01)01118-X
VISUAL ACUITY RECOVERY AFTER PHACOEMULSIFICATION
T he considerable contribution of cataract surgery to
the patient’s quality of life began with its early de-
velopment. Phacoemulsification further improved the
Patients and Methods
This study comprised 47 eyes of 47 patients
popularity of this surgery as its duration is short and (30 men, 17 women) having cataract surgery over a
visual rehabilitation is fast. Thus, patients expect early 1-month period, the single criterion for their inclusion.
and reliable visual recovery, and a poor visual outcome is No patient had previous ocular surgery. All patients
disappointing to patients and surgeons, especially after had phacoemulsification with in-the-bag intra-
uneventful phacoemulsification. ocular lens implantation by the same surgeon (B.A.)
Poor visual recovery after phacoemulsification is fre- with no postoperative complications over a 2-month
quently linked to undiagnosed retinal disease, which can follow-up.
be related to fundoscopy difficulty in cases of severe The patients’ demographics are shown in Table 1.
cataract, or to retinal or corneal pathology, which makes The mean age of the patients was 70.38 years ⫾ 15.84
prediction of visual recovery unreliable. (SD) (range 19 to 92 years); 70% were older than
Various methods to predict retinal acuity and the 70 years, fitting the general population requesting
risk/benefit ratio after extracapsular cataract extraction cataract surgery. All patients had mild to moderate cat-
(ECCE) have been developed. Several are based on ret- aract. Five patients (#2, 5, 10, 19, 33) had high myopia
inal qualitative indices. These include electroretinogra- (range –9.0 to –15.0 diopters [D]); 4 (#3, 23, 31, 45)
phy,1–3 visual evoked potentials,1,2,4,5 color vision had posterior subcapsular cataract; 4 (#9, 15, 28, 42)
tests,6 blue-field entoptic tests,7–9 and B-scan ultra- had atrophic age-related macular degeneration
sonography.2 Others are based on quantitative criteria (ARMD) and 1 (#16) exudative ARMD; 2 (#13, 35)
using pinhole techniques (J. Lowry, “Pinhole Tech- had retinitis pigmentosa; 1 (#43) was amblyopic;
niques Are Called Reliable, Easy, and Inexpensive,” 1 (#40) had a complex syndrome comprising corneal
Ophthalmology Times, September 1, 1986, pages 1, 31, dystrophy, aniridia, and nystagmus; and 1 (#47) had
35), laser or white-light interferometry,10 –13 and poten- open-angle glaucoma.
tial acuity meter (PAM) assessment.14,15 Preoperatively, a single evaluator performed a
In this prospective study, we analyzed the predicted clinical examination. This included slitlamp and fundo-
results of visual recovery after phacoemulsification using scopic evaluations and intraocular pressure measure-
2 technologically different quantitative methods: white- ment. The best corrected visual acuity (BCVA) was
light interferometry and the PAM assessment. We sta- evaluated using the decimal scale 1 day before and
tistically estimated the results of both systems. To our 1 month after surgery.
knowledge, no similar comparison of these methods has Prediction of visual acuity recovery was per-
been published. formed by a single trained examiner by the 2 meth-
ods available in the Department of Ophthalmology:
the white-light IRAS GT威 interferometer (Randwall
Instruments) on the 3- and 8-degree wide test area or
the Guyton-Minkowski PAM (Mentor O&O Inc.).
Accepted for publication July 30, 2001.
One drop of tropicamide was instilled 30 minutes before
From Service d’Ophtalmologie, CMC Gui de Chauliac, Montpellier, to obtain adequate pupil dilation in photopic condi-
France.
tions. To ensure their cooperation, all patients received
Gaston Le Sage, Institut National des Statistiques et des Etudes a thorough description of the instrument and its
Economiques, Montpellier, France, provided statistical analysis and Mi-
technique.
kaël Tritz, Ecole d’Ingénierie, Bourges, France, helped translate from
German. The IRAS GT is a white-light interferometer. The
light emitted from an incandescent source is focused on
None of the authors has a financial or proprietary interest in any material
or method mentioned. a holographic grating that splits the single coherent
source into 2 equally strong coherent lights. A relay lens
Reprint requests to Dr. Clair-Florent Schmitt-Bernard, Antigone Oph-
talmologie, Le Jardin Du Centre, Rue De L’Epire, 34000 Montpellier, system projects the 2 slit sources near the nodal point of
France. E-mail: cfsb@mnet.fr/cfsb@igh.cnrs.fr. the eye, where coherent light waves emanating from
132 J CATARACT REFRACT SURG—VOL 28, JANUARY 2002
VISUAL ACUITY RECOVERY AFTER PHACOEMULSIFICATION
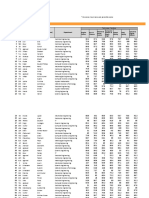
Table 1. Patient characteristics and visual acuities.
Decimal VA (LogMAR VA)
Age
Patient (Years) Sex Preop IF-3 IF-8 PAM Postop
1 75 M 0.40 (0.40) 0.80 (0.10) 0.67 (0.17) 0.80 (0.10) 0.90 (0.05)
2 64 F 0.40 (0.40) NA 1.00 (0.00) 0.50 (0.30) 0.80 (0.10)
3 64 F 0.20 (0.70) 0.33 (0.48) 0.33 (0.48) 0.40 (0.40) 0.90 (0.05)
4 80 F 0.40 (0.40) 1.00 (0.00) 0.67 (0.17) 0.50 (0.30) 0.90 (0.05)
5 70 F 0.40 (0.40) 0.67 (0.17) 0.67 (0.17) 0.50 (0.30) 0.60 (0.22)
6 70 F 0.40 (0.40) 0.50 (0.30) 0.67 (0.17) 0.80 (0.10) 0.60 (0.22)
7 80 F 0.30 (0.52) 0.80 (0.10) 0.67 (0.17) 0.33 (0.48) 0.90 (0.05)
8 63 F 0.40 (0.40) 1.00 (0.00) 1.00 (0.00) 0.40 (0.40) 0.80 (0.10)
9 92 F 0.10 (1.00) NA 0.05 (1.30) 0.50 (0.30) 0.10 (1.00)
10 61 F 0.20 (0.70) 0.80 (0.10) 0.33 (0.48) 0.25 (0.60) 0.30 (0.52)
11 69 F 0.40 (0.40) 0.80 (0.10) 0.67 (0.17) 0.80 (0.10) 0.80 (0.10)
12 28 M 0.40 (0.40) 1.00 (0.00) 1.00 (0.00) 0.80 (0.10) 1.00 (0.00)
13 68 M 0.10 (1.00) 0.02 (1.60) 0.02 (1.60) 0.10 (1.00) 0.10 (1.00)
14 88 M 0.40 (0.40) 1.00 (0.00) 0.80 (0.10) 0.50 (0.30) 0.80 (0.10)
15 82 F 0.20 (0.70) NA 0.05 (1.30) 0.10 (1.00) 0.30 (0.52)
16 78 F 0.40 (0.40) 1.00 (0.00) 1.00 (0.00) 0.40 (0.40) 0.50 (0.30)
17 64 F 0.30 (0.52) 0.67 (0.17) 0.40 (0.40) 0.50 (0.30) 0.70 (0.15)
18 77 F 0.20 (0.70) 0.50 (0.30) 0.50 (0.30) 0.28 (0.55) 0.50 (0.30)
19 78 F 0.40 (0.40) 0.80 (0.10) 0.40 (0.40) 0.50 (0.30) 0.70 (0.15)
20 79 F 0.30 (0.52) 0.67 (0.17) 0.67 (0.17) 0.33 (0.48) 0.90 (0.05)
21 74 F 0.40 (0.40) 0.80 (0.10) 1.00 (0.00) 0.66 (0.18) 0.90 (0.05)
22 77 M 0.50 (0.30) 0.80 (0.10) 0.67 (0.17) 0.80 (0.10) 0.90 (0.05)
23 30 M 0.05 (1.30) 0.02 (1.60) 0.02 (1.60) 0.50 (0.30) 0.80 (0.10)
24 57 M 0.40 (0.40) 0.50 (0.30) 0.50 (0.30) 0.33 (0.48) 1.00 (0.00)
25 74 M 0.40 (0.40) 0.80 (0.10) 0.80 (0.10) 0.50 (0.30) 1.00 (0.00)
26 85 M 0.40 (0.40) 0.80 (0.10) 0.80 (0.10) 0.66 (0.18) 0.80 (0.10)
27 76 F 0.20 (0.70) 0.50 (0.30) 0.50 (0.30) 0.40 (0.40) 1.00 (0.00)
28 78 F 0.30 (0.52) 0.02 (1.60) 0.33 (0.40) 0.50 (0.30) 0.50 (0.30)
29 79 F 0.40 (0.40) 0.33 (0.40) 0.20 (0.70) 0.50 (0.30) 0.80 (0.10)
30 85 M 0.40 (0.40) 1.00 (0.00) 0.80 (0.10) 0.80 (0.10) 1.00 (0.00)
31 62 F 0.16 (0.80) 0.25 (0.60) 0.30 (0.52) 1.00 (0.00) 0.70 (0.15)
32 73 F 0.40 (0.40) 1.00 (0.00) 0.80 (0.10) 0.66 (0.18) 1.00 (0.00)
33 75 M 0.10 (1.00) 0.33 (0.40) 0.25 (0.60) 0.28 (0.55) 0.60 (0.22)
34 76 M 0.40 (0.40) 0.67 (0.17) 0.67 (0.17) 0.50 (0.30) 0.70 (0.15)
35 80 F LP NA NA NA LP
36 80 F 0.16 (0.80) 0.67 (0.17) 0.67 (0.17) 0.50 (0.30) 1.00 (0.00)
37 62 M 0.40 (0.40) 0.80 (0.10) 0.67 (0.17) 0.66 (0.18) 0.60 (0.22)
38 73 F 0.40 (0.40) 1.00 (0.00) 0.80 (0.10) 0.80 (0.10) 0.80 (0.10)
39 78 F 0.10 (1.00) 0.67 (0.17) 0.40 (0.40) 0.20 (0.70) 1.00 (0.00)
40 23 F 0.05 (1.30) 0.40 (0.40) 0.80 (0.10) NA 0.10 (1.00)
J CATARACT REFRACT SURG—VOL 28, JANUARY 2002 133
VISUAL ACUITY RECOVERY AFTER PHACOEMULSIFICATION
Table 1. (cont.)
Decimal VA (LogMAR VA)
Age
Patient (Years) Sex Preop IF-3 IF-8 PAM Postop
41 74 F 0.30 (0.52) 0.67 (0.17) 0.50 (0.30) 1.00 (0.00) 0.90 (0.05)
42 76 F 0.40 (0.40) 1.00 (0.00) 1.00 (0.00) 1.00 (0.00) 0.80 (0.10)
43 19 M 0.05 (1.30) 0.50 (0.30) 0.40 (0.40) 0.28 (0.55) 0.50 (0.30)
44 81 M 0.30 (0.52) 0.67 (0.17) 0.67 (0.17) 0.50 (0.30) 0.60 (0.22)
45 78 F 0.40 (0.40) 0.20 (0.70) 0.40 (0.40) 0.66 (0.18) 0.50 (0.30)
46 80 F 0.40 (0.40) 0.80 (0.10) 0.67 (0.17) 1.00 (0.00) 0.90 (0.05)
47 73 M 0.40 (0.40) 1.00 (0.00) 1.00 (0.00) 0.80 (0.10) 0.90 (0.05)
VA ⫽ visual acuity; IF-3 ⫽ 3-degree interferometry; IF-8 ⫽ 8-degree interferometry; PAM ⫽ potential acuity meter; LP ⫽ light perception; NA ⫽
not applicable
each source interfere and form a series of black-and- Results
white lines on the retina. Orientation of the lines can be
set vertically, horizontally, or diagonally by rotating the The mean preoperative BCVA was 0.57 ⫾ 0.27
holographic grating. The equivalent acuity depends on logMAR (range light perception [LP] to 0.30) and
the interaction angle between the interfering wave 0.27 ⫾ 0.54 decimal (range LP to 0.50). The mean
fronts. The distance between these lines defines Snellen postoperative BCVA was (0.19 ⫾ 0.25) logMAR (range
visual acuity from 20/800 to 20/20 independent of the LP to 0.00) and 0.64 ⫾ 0.56 decimal (range LP to 1.0).
patient’s refraction. The gratings and Snellen letters do The predicted visual acuity was significantly closer to the
not have direct correlation because of the higher fre- final visual acuity with 3-degree interferometry (0.27 ⫾
quency components of the Snellen letters. A 3- or 8-de- 0.40 logMAR; 0.54 ⫾ 0.40 decimal) than with 8-degree
gree area of central retina can be evaluated depending on interferometry (0.33 ⫾ 0.39 logMAR; 0.47 ⫾ 0.41 dec-
the diaphragm aperture. imal) or the PAM (0.31 ⫾ 0.23 logMAR; 0.49 ⫾ 0.59
The Guyton-Minkowski PAM projects a Snellen decimal) (Figure 1).
chart ranging from 20/400 to 20/20 in a small beam The 3 methods of prediction displayed a non-Gaus-
of light (0.15 mm diameter aperture). The light beam sian curve of distribution of results. There was no statis-
is aimed through the less opaque area of the lens. The tically significant disparity between predicted and
diopter control is set at the spherocylindrical equiva- postoperative results with 3-degree interferometry
lent of the patient’s refraction (–10.0 to ⫹13.0 D). (1.04 ⫾ 0.57 logMAR; – 0.09 ⫾ 0.27 decimal) (P ⫽
In patients with myopia greater than –10.0 D, the .0647) and a statistically significant disparity with 8-de-
measurement was done with the best spectacle gree interferometry (0.89 ⫾ 0.59 logMAR; – 0.13 ⫾
correction. 0.27 decimal) and the PAM (0.66 ⫾ 0.62 logMAR;
– 0.22 ⫾ 0.24 decimal) (P ⫽ .0001). Therefore, the
Statistical Analysis mean predictive results with 3-degree interferometry
Preoperative and postoperative visual acuities were significantly matched the final visual acuity, and all
compared with the results of the predictive tests, and 3 tests underestimated postoperative visual acuity. The
their statistical significance was analyzed using the Wil- mean underestimation was less than 1 line (decimal
coxon matched test as the distribution did not fit a scale) with 3-degree interferometry, making it the most
Gaussian pattern. The Altman and Bland test was used accurate method of predicting visual acuity recovery.
to determine the dispersion of results, and their correla- There was no significant difference in the level of
tion was calculated by the Spearman correlation test. dispersion of results between 3-degree interferometry
Decimal visual acuity was expressed as a logMAR equiv- (– 0.81 to 0.60 logMAR) and 8-degree interferometry
alent for data analysis.16 (– 0.79 to 0.51 logMAR) (P ⫽ .0001), 3-degree inter-
134 J CATARACT REFRACT SURG—VOL 28, JANUARY 2002
VISUAL ACUITY RECOVERY AFTER PHACOEMULSIFICATION
Figure 1. (Le Sage) Variation be-
tween predicted and actual postoper-
ative visual acuity (black bar ⫽
3-degree interferometry; white bar ⫽
8-degree interferometry; gray bar ⫽
PAM; y-axis ⫽ acuity, decimal scale).
ferometry and the PAM (– 0.58 to 0.30 logMAR) (P ⫽ sion test showed that individual prediction may be
.0216), or 8-degree interferometry and the PAM (P ⫽ overestimated or underestimated from ⫹0.25 to – 0.15
.003) (Figure 2). Therefore, even though 3-degree inter- lines on the decimal scale around the mean result. This
ferometry appeared to be the best predictor, the disper- was also true with 8-degree interferometry (⫹0.31 to
– 0.16 lines, decimal) and the PAM (⫹0.50 to – 0.26
lines, decimal). The PAM had a wider dispersion of
results than either interferometry method when individ-
ually results were considered; the difference was not sta-
tistically significant, however.
There was a significantly poor individual correla-
tion between predicted and postoperative visual acuities
with all 3 methods: 3-degree interferometry (r ⫽ 0.39,
P ⫽ .01); 8-degree interferometry (r ⫽ 0.49, P ⫽
.0005); PAM (r ⫽ 0.38, P ⫽ .0091).
Discussion
In this comparative study, 3-degree white-light in-
terferometry was more reliable in predicting postopera-
tive visual acuity than 8-degree interferometry or the
PAM; the mean prediction with 3-degree white-light
interferometry was approximately 1 line (decimal scale)
from the final visual acuity. However, all 3 methods
underestimated postoperative visual acuity, which may
have relatively little effect on patient satisfaction. It may
be of concern to surgeons evaluating the risk/benefit
ratio of cataract surgery. All 3 methods had a tendency
toward poor prediction of individual acuity as the dis-
persion of results was significantly wide and the correla-
tion indices unsatisfactory. Thus, none of the methods
can predict final visual acuity in a linear mode and a
prediction of poor visual recovery may not reflect an
individual’s visual capacity.
All the patients in our study had mild to moderate
Figure 2. (Le Sage) Dispersion of predicted versus final visual
acuity. Top: 3-degree interferometry (IF-3°). Middle: 8-degree inter- cataract. There were no cases of mature cataract, which
ferometry (IF-8°). Bottom: PAM (x- and y-axis ⫽ logMAR scale). is more likely to induce a false negative (underestimated)
J CATARACT REFRACT SURG—VOL 28, JANUARY 2002 135
VISUAL ACUITY RECOVERY AFTER PHACOEMULSIFICATION
predicted visual acuity. Other conditions reported to interferometry. This in agreement with the results of
induce inaccurate prediction of visual recovery are pos- Goldmann and coauthors,20 who suggest that small
terior subcapsular cataract, high myopia, ARMD, cys- fields are more accurately centered on the fovea and may
toid macular edema, retinal detachment, amblyopia, be more accurate in patients suspected of having macu-
nystagmus, glaucoma, and miosis.17–23 lar disease. This prevents test recognition from the
In our study, 4 of the 5 myopic patients displayed a parafoveal retina.
strong disparity in predicted visual acuity and final vi- In our study, a single trained examiner performed all
sual acuity between the 2 interferometry tests and be- visual acuity prediction tests after providing patients a
tween the interferometer and the PAM. The orientation detailed explanation. This increased the reliability of the
of the light rays reaching adjacent areas of the retina may results. Miller et al.29 propose that the poor correlation
be a cause of this disparity.19,20 Thus, the 3 methods indices in their series of 82 patients obtained with both
seemed inaccurate in predicting final acuity in eyes with interferometry (r ⫽ 0.03) and the PAM (r ⫽ 0.07) were
high myopia. This is in contrast to the results of Datiles the result of the technician’s lack of experience as well as
et al.,24 who report accurate predicted acuity in 3 cases the patients’ ages and associated diseases, which lead to
of high myopia. Datiles et al. stress that the low preop- poor cooperation. These biases result in a poor estima-
erative visual acuity in high myopia may be the result of tion of visual acuity recovery and thus contradictory
amplified distortion when the light passes through even outcomes among studies.25,28 –31
a moderate cataract. Few studies have compared the use of interferom-
The predicted acuity was underestimated by inter- etry and the PAM in ECCE. Most did not provide
ferometry in all 4 patients with posterior subcapsular a statistical analysis to determine whether interferom-
cataract and by the PAM in 3 of the patients. The results etry or the PAM is significantly accurate. Spurny and
support the findings of Lasa and coauthors21 and coauthors25 compared a white-light interferometer
Schraub and coauthors,23 who used a Rodenstock威 reti- (Lotmar visometer, Haag-Streit) with the PAM in
nometer and the PAM to predict acuity. Both groups 54 eyes having cataract surgery or neodymium:YAG
hypothesize that this underestimation is linked to the laser capsulotomy. Predictions were more accurate
increased central density of the opacity in a nuclear cat- with the visometer than the PAM, supporting our
aract; the opacity is more diffuse and regular, giving results. Strong30 compared the Rodenstock laser
more reliable values. interferometer, Lotmar visometer, and white-light
As previously described,17,18,21,25 interferometry IRAS interferometer in 14 eyes. The laser interferome-
accurately predicted visual acuity in patients with atro- ter was the most accurate, but no statistical analysis
phic ARMD and overestimated it in the patient with was reported. Graney et al.28 found laser interferometry
exudative ARMD. The PAM results were more accurate and the PAM less accurate than a clinical index based on
in the case of exudative ARMD. age, preoperative visual acuity, number of current pre-
The postoperative visual acuity matched the pre- scription medications, and the ability to read a newspa-
dicted outcome with all 3 methods in patients with pig- per. Nevertheless, these studies had several biases as
ment epithelium retinopathy, which agrees with the different ophthalmologists performed the prediction
findings in a previous study.26 The results in the patient tests and all patients were from middle- or upper-class
with amblyopia were also accurate, which is in contrast families. However, the PAM was statistically more accu-
to previous studies showing overestimation in such cas- rate in predicting acuity than laser interferometry. In a
es.9 In the patient with nystagmus, interferometry over- prospective study of 35 eyes, Datiles et al.24 found that
estimated and the PAM underestimated final visual the PAM and laser interferometer were equally good
acuity, as reported in a previous study.27 However, con- predictors in cases of mild to moderate cataract. Gold-
clusions cannot be made based on the evaluation of a stein et al.31 found better results with the Lotmar vi-
single individual. someter than with the IRAS interferometer. Therefore,
There was a significant disparity among the 3 meth- it appears that these studies had several strong examiner
ods in predicting visual acuity recovery after phacoemul- and patient biases, which may account for the contra-
sification. The best results were obtained with 3-degree dictory results.
136 J CATARACT REFRACT SURG—VOL 28, JANUARY 2002
VISUAL ACUITY RECOVERY AFTER PHACOEMULSIFICATION
Conclusion nomenon in cataract patients. Arch Ophthalmol 1979;
97:1092–1095
Our findings suggest that the interferometer and 10. Lotmar W. Apparatus for the measurement of retinal
the PAM are accurate predictors of postoperative vi- visual acuity by moiré fringes. Invest Ophthalmol Vis Sci
sual acuity in healthy eyes with moderate cataract. 1980; 19:393– 400
Conversely, both instruments lack reliability in eyes 11. Goldmann H, Lotmar W. Retinale Sehschärfenbestim-
with retinal disorders. These methods are suited to mung bei Katarakt. Ophthalmologica 1970; 161:175–
179
daily practice as they are fast and easy and give reliable
12. Green DG. Testing the vision of cataract patients by
prediction of visual recovery in most patients having means of laser-generated interference fringes. Science
phacoemulsification. 1970; 168:1240 –1242
However, we believe that the instruments should be 13. Rassow B, Rätzke P. Der prognostische Wert der Bestim-
used semiquantitatively and the results be interpreted in mung der retinalen Sehschärfe bei Patienten mit Kat-
relation to the clinical data. The results must also be arakt. Klin Monatsbl Augenheilkd 1977; 171:643– 650
assessed on an individual basis considering their wide 14. Minkowski JS, Guyton DL. New methods for predicting
visual acuity after cataract surgery. Ann Ophthalmol
dispersion, especially in patients with associated ocular
1984; 16:511–516
pathology. In this respect, qualitative methods may help 15. Cavonius CR, Hilz R. A technique for testing visual func-
confirm or refute the capacity for visual recovery ascer- tion in the presence of opacities. Invest Ophthalmol
tained by quantitative systems. 1973; 12:933–936
16. Holladay JT. Proper method for calculating average vi-
sual acuity. J Refract Surg 1997; 13:388 –391
References 17. Faulkner W. Laser interferometric prediction of postop-
erative visual acuity in patients with cataracts. Am J Oph-
1. Bertrand F, Delplace MP, Bertrand P. Interet de l’ERG et thalmol 1983; 95:626 – 636
des VEP en rouge dans le pronostic preoperatoire des 18. Bloom TD, Fishman GA, Traubert BS. Laser interfero-
cataractes seniles. Bull Soc Ophtalmol Fr 1984; metric visual acuity in senile macular degeneration. Arch
84:1321–1324 Ophthalmol 1983; 101:925–926
2. Sherman J, Davis E, Schnider C, et al. Presurgical predic- 19. Gstalder RJ, Green DG. Laser interferometric acuity in
tion of postsurgical visual acuity in patients with media amblyopia. J Pediatr Ophthalmol Strabismus 1971;
opacities. J Am Optom Assoc 1988; 59:481– 488 8:251–266
3. Wu D-Z, Wu L, XU X, et al. The significance of testing 20. Goldmann H, Chrenková A, Cornaro S. Retinal visual
preoperative visual function in cataract using laser inter- acuity in cataractous eyes; determination with interfer-
ferometric visual acuity and ERG. Yen Ko Hsueh Pao ence fringes. Arch Ophthalmol 1980; 98:1778 –1781
1991; 7:21–24 21. Lasa MSM, Datiles MB II, Freidlin V. Potential vision
4. Odom JV, Chao G-M, Weinstein GW. Preoperative pre- tests in patients with cataracts. Ophthalmology 1995;
diction of postoperative visual acuity in patients with 102:1007–1011
cataracts: a quantitative review. Doc Ophthalmol 1988; 22. Rassow B, Wolf D. Die Messung der “retinalen Sehs-
70:5–17 chärfe” mit dem Laserinterferenzgerät als klinische Rou-
5. Van Lith GHM, Hekkert-Wiebenga W. Cataract, pat- tinemethode. Adv Ophthalmol 1977; 34:116 –142
tern stimulation and visually evoked potentials. Doc 23. Schraub M, Flament J, Sahel J, Bronner A. Evaluation de
Ophthalmol 1983; 55:107–112 la capacité fonctionnelle maculaire interférométrie au la-
6. Kogure S, Iijima H, Tsukahara S. Assessment of potential ser hélium-néon. J Fr Ophtalmol 1985; 8:427– 432
macular function using a color saturation discrimination 24. Datiles MB, Edwards PA, Kaiser-Kupfer MI, et al. A
test in eyes with cataract. J Cataract Refract Surg 1999; comparative study between the PAM and the laser inter-
25:569 –574 ferometer in cataracts. Graefes Arch Clin Exp Ophthal-
7. Grignolo FM, Moscone F, Sobrero C, Leone M. Evalu- mol 1987; 225:457– 460
ation of macular function by Lotmar’s visometer test and 25. Spurny RC, Zaldivar R, Belcher CD III, Simmons
blue-field entoptic test in patients with cataract. Ann RJ. Instruments for predicting visual acuity; a clinical
Ophthalmol 1988; 20:247–250 comparison. Arch Ophthalmol 1986; 104:196 –200
8. Miris R, Missotten L. Evaluation of the macular function 26. Kogure S, Iijima H. Preoperative evaluation by laser in-
in cataractous eyes by means of the blue field entopto- terferometry in cataractous eyes with retinitis pigmen-
scope. Bull Soc Belge Ophtalmol 1982; 201:121–126 tosa. Jpn J Ophthalmol 1993; 37:282–286
9. Sinclair SH, Loebl M, Riva CE. Blue field entoptic phe- 27. Minkowski JS, Palese M, Guyton DL. Potential Acuity
J CATARACT REFRACT SURG—VOL 28, JANUARY 2002 137
VISUAL ACUITY RECOVERY AFTER PHACOEMULSIFICATION
Meter using a minute aerial pinhole aperture. Ophthal- 30. Strong N. Interferometer assessment of potential visual
mology 1983; 90:1360 –1368 acuity before YAG capsulotomy: relative performance of
28. Graney MJ, Applegate WB, Miller ST, et al. A clinical three instruments. Graefes Arch Clin Exp Ophthalmol
index for predicting visual acuity after cataract surgery. 1992; 230:42– 46
Am J Ophthalmol 1988; 105:460 – 465 31. Goldstein J, Jamara RJ, Hecht SD, et al. Clinical com-
29. Miller ST, Graney MJ, Elam JT, et al. Predictions of parison of the SITE IRAS hand held interferometer and
outcomes from cataract surgery in elderly persons. Oph- Haag-Streit Lotmar visometer. J Cataract Refract Surg
thalmology 1988; 95:1125–1129 1988; 14:208 –211
138 J CATARACT REFRACT SURG—VOL 28, JANUARY 2002
Potrebbero piacerti anche
- Corneal Asymmetry Analysis by Pentacam Scheimpflug Tomography For Keratoconus DiagnosisDocumento13 pagineCorneal Asymmetry Analysis by Pentacam Scheimpflug Tomography For Keratoconus DiagnosisJuanes MagnoNessuna valutazione finora
- OptometryDocumento8 pagineOptometryasad aliNessuna valutazione finora
- IndianJOphthalmol6310775-4654929 125549Documento4 pagineIndianJOphthalmol6310775-4654929 1255496jprsrbhkcNessuna valutazione finora
- Artículo 5Documento6 pagineArtículo 5María Oña MartosNessuna valutazione finora
- Single-Step Transepithelial PHDocumento9 pagineSingle-Step Transepithelial PHlenniNessuna valutazione finora
- Chalam 2010Documento6 pagineChalam 2010Sonya MabroukNessuna valutazione finora
- Thickness Obtained by Software Image Normative Data of Outer Photoreceptor LayerDocumento7 pagineThickness Obtained by Software Image Normative Data of Outer Photoreceptor LayerAzuleslindoNessuna valutazione finora
- Ijpt (2967-2979)Documento14 pagineIjpt (2967-2979)VenkatramanNessuna valutazione finora
- PAP Ophth 1999Documento6 paginePAP Ophth 1999KrueNessuna valutazione finora
- Comparison of Topical Versus Peribulbar Anesthesia For 23G Pars Plana VitrectomyDocumento4 pagineComparison of Topical Versus Peribulbar Anesthesia For 23G Pars Plana VitrectomyUsman ImtiazNessuna valutazione finora
- Phacoemulsification Versus Manual Small Incision Cataract Surgery in Hard NuclearDocumento6 paginePhacoemulsification Versus Manual Small Incision Cataract Surgery in Hard NuclearRagni MishraNessuna valutazione finora
- BiometryDocumento7 pagineBiometrysandip shelakeNessuna valutazione finora
- PterygiumDocumento6 paginePterygiumDewiakyuNessuna valutazione finora
- Adminku Journal Manager ErlaniDocumento7 pagineAdminku Journal Manager Erlanirm suryaubungNessuna valutazione finora
- 2015 Acta Endocrinologica - Optochiasmatic Syndrome Assessing Optic Nerve Changes by OCTDocumento8 pagine2015 Acta Endocrinologica - Optochiasmatic Syndrome Assessing Optic Nerve Changes by OCTHoratiuSilaghiNessuna valutazione finora
- Glaucoma Congenital CCDocumento6 pagineGlaucoma Congenital CCAllyciaNessuna valutazione finora
- Development of Topographic Scoring System For Identifying Glaucoma in Myopic EyesDocumento10 pagineDevelopment of Topographic Scoring System For Identifying Glaucoma in Myopic EyesValentina Gracia ReyNessuna valutazione finora
- Reti No MetriDocumento4 pagineReti No MetriEstmar ValentinoNessuna valutazione finora
- Central Corneal Thickness Changes Following Manual Small Incision Cataract Surgery Versus Phacoemulsification For White CataractDocumento7 pagineCentral Corneal Thickness Changes Following Manual Small Incision Cataract Surgery Versus Phacoemulsification For White CataractFadhila AnggariniNessuna valutazione finora
- FiltrationDocumento16 pagineFiltrationjojokawayNessuna valutazione finora
- 16 Nigwekar Etal.Documento4 pagine16 Nigwekar Etal.editorijmrhsNessuna valutazione finora
- Five-Year Results of ViscotrabeculotomyDocumento10 pagineFive-Year Results of ViscotrabeculotomyChintya Redina HapsariNessuna valutazione finora
- CE (Ra1) F (SH) PF1 (SC SS) PFA (SC KM) PN (KM)Documento4 pagineCE (Ra1) F (SH) PF1 (SC SS) PFA (SC KM) PN (KM)Ofkom UnhasNessuna valutazione finora
- Long Term Follow-Up Safety and E Myopia Refractive Surgery: Ffectiveness ofDocumento9 pagineLong Term Follow-Up Safety and E Myopia Refractive Surgery: Ffectiveness ofayurNessuna valutazione finora
- Z Score SISCOMDocumento9 pagineZ Score SISCOMAiswarya HariNessuna valutazione finora
- Novel Artificial Intelligence Index Based On.93Documento24 pagineNovel Artificial Intelligence Index Based On.93Alejandra VenegasNessuna valutazione finora
- Central Corneal Thickness: Ultrasound Pachymetry Verus Anterior Segment Optical Coherence TomographyDocumento5 pagineCentral Corneal Thickness: Ultrasound Pachymetry Verus Anterior Segment Optical Coherence TomographybasharatNessuna valutazione finora
- RiboflavinUltravioletAinduced Collagen Wollensak Et Al Keratoconus 2003Documento8 pagineRiboflavinUltravioletAinduced Collagen Wollensak Et Al Keratoconus 2003SergioNessuna valutazione finora
- Keywords:-Tonometers, Intraocular Pressure, CentralDocumento6 pagineKeywords:-Tonometers, Intraocular Pressure, CentralInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- TgkkkkjuipohgfhiDocumento6 pagineTgkkkkjuipohgfhisiscaNessuna valutazione finora
- JOVRDocumento5 pagineJOVRkrishan bansalNessuna valutazione finora
- Iris Morphology: Ophthalmology March 2008Documento3 pagineIris Morphology: Ophthalmology March 2008Hasnain AjmalNessuna valutazione finora
- 19 - Weleber2016 PDFDocumento15 pagine19 - Weleber2016 PDFHarsya LuthfiNessuna valutazione finora
- Efficacy and Toxicity of Intravitreous Chemotherapy For Retinoblastoma: Four-Year ExperienceDocumento8 pagineEfficacy and Toxicity of Intravitreous Chemotherapy For Retinoblastoma: Four-Year ExperienceSlr RandiNessuna valutazione finora
- J Jocn 2019 07 005Documento6 pagineJ Jocn 2019 07 005andrema123Nessuna valutazione finora
- Cotofana 2021Documento9 pagineCotofana 2021Emrys1987Nessuna valutazione finora
- Clinical Study: Comparison of The Optical Quality Between Small Incision Lenticule Extraction and Femtosecond Laser LASIKDocumento10 pagineClinical Study: Comparison of The Optical Quality Between Small Incision Lenticule Extraction and Femtosecond Laser LASIKnicoNessuna valutazione finora
- Transcaruncular Double Injection Technique For Peribulbar Anesthesia in Vitreoretinal SurgeryDocumento5 pagineTranscaruncular Double Injection Technique For Peribulbar Anesthesia in Vitreoretinal SurgeryanxNessuna valutazione finora
- Scheimpflug Corneal Densitometry Changes After TrabeculectomyDocumento7 pagineScheimpflug Corneal Densitometry Changes After TrabeculectomyFernando MartínezNessuna valutazione finora
- Artículo 1 TransprkDocumento6 pagineArtículo 1 TransprkGiancarlo Varillas MerinoNessuna valutazione finora
- Diagnostic Ability of Retinal Ganglion Cell Complex, RetinalDocumento7 pagineDiagnostic Ability of Retinal Ganglion Cell Complex, RetinalYoselin Herrera GuzmánNessuna valutazione finora
- Irregular Astigmatism After Corneal Transplantation-Efficacy and Safety of Topography-Guided TreatmentDocumento7 pagineIrregular Astigmatism After Corneal Transplantation-Efficacy and Safety of Topography-Guided TreatmentJoseph Chipana GutierrezNessuna valutazione finora
- Feng Et Al 2023 Epithelial Thickness Mapping in Keratoconic Corneas Repeatability and Agreement Between Cso Ms 39Documento14 pagineFeng Et Al 2023 Epithelial Thickness Mapping in Keratoconic Corneas Repeatability and Agreement Between Cso Ms 39vahidsmpNessuna valutazione finora
- Retinal Nerve Fiber Loss in High-And Normal-Tension Glaucoma by Optical Coherence TomographyDocumento4 pagineRetinal Nerve Fiber Loss in High-And Normal-Tension Glaucoma by Optical Coherence TomographyRaditya BagusNessuna valutazione finora
- J Wneu 2010 08 021Documento9 pagineJ Wneu 2010 08 021Boukhenoufa Mouhammed ElamineNessuna valutazione finora
- Randomized Clinical Trial of Topical Betaxolol For Persistent Macular Edema After Vitrectomy and Epiretinal Membrane RemovalDocumento8 pagineRandomized Clinical Trial of Topical Betaxolol For Persistent Macular Edema After Vitrectomy and Epiretinal Membrane RemovalsiscaNessuna valutazione finora
- Body Mass Index and Interocular Asymmetry of Retinal and Choroidal Thickness in Emmetropic and Ametropic SubjectsDocumento13 pagineBody Mass Index and Interocular Asymmetry of Retinal and Choroidal Thickness in Emmetropic and Ametropic SubjectsAthenaeum Scientific PublishersNessuna valutazione finora
- Assessment of Corneal Biomechanics, Tonometry and Pachymetry With The Corvis ST in MyopiaDocumento10 pagineAssessment of Corneal Biomechanics, Tonometry and Pachymetry With The Corvis ST in Myopiavergarajaviera548Nessuna valutazione finora
- Jurnal Mata 5Documento6 pagineJurnal Mata 5Dahru KinanggaNessuna valutazione finora
- Ni Hms 12505Documento10 pagineNi Hms 12505noorhadi.n10Nessuna valutazione finora
- Pentacam enDocumento18 paginePentacam endarkspawn69Nessuna valutazione finora
- Catarct SinilisDocumento5 pagineCatarct SinilisAsri Mukti NantaNessuna valutazione finora
- Comparison of Postoperative Refractive Outcome in Eyes UndergoingDocumento9 pagineComparison of Postoperative Refractive Outcome in Eyes UndergoingAndi Ayu LestariNessuna valutazione finora
- Corneal Parameters Measurement in Healthy Subjects Using Scheimpflug and Anterior Segment Optical Coherence TomographyDocumento6 pagineCorneal Parameters Measurement in Healthy Subjects Using Scheimpflug and Anterior Segment Optical Coherence TomographyvahidsmpNessuna valutazione finora
- Clinical Study: Two-Year Accelerated Corneal Cross-Linking Outcome in Patients With Progressive KeratoconusDocumento10 pagineClinical Study: Two-Year Accelerated Corneal Cross-Linking Outcome in Patients With Progressive KeratoconusPunam RazputriNessuna valutazione finora
- Deep Learning For Automatically Visual Evoked Potential Classification During Surgical Decompression of Sellar Region TumorDocumento7 pagineDeep Learning For Automatically Visual Evoked Potential Classification During Surgical Decompression of Sellar Region TumoradityaNessuna valutazione finora
- A Deep Learning System For Automatic Assessment of Anterior Chamber Angle in Ultrasound Biomicroscopy ImagesDocumento11 pagineA Deep Learning System For Automatic Assessment of Anterior Chamber Angle in Ultrasound Biomicroscopy Imageszj xiaoNessuna valutazione finora
- 1233 2373 1 SMDocumento6 pagine1233 2373 1 SMellaNessuna valutazione finora
- Comparative Axial Length Measurements Using Optical and Acoustic Biometry in Normal Persons and in Patients With Retinal LesionsDocumento5 pagineComparative Axial Length Measurements Using Optical and Acoustic Biometry in Normal Persons and in Patients With Retinal LesionsAyu Wedhani SpcNessuna valutazione finora
- LED-Based Photoacoustic Imaging: From Bench to BedsideDa EverandLED-Based Photoacoustic Imaging: From Bench to BedsideMithun Kuniyil Ajith SinghNessuna valutazione finora
- Stereogram CuesDocumento10 pagineStereogram CuesijudoptoNessuna valutazione finora
- Turnitin Effectiveness HEDocumento12 pagineTurnitin Effectiveness HEpraveen3530Nessuna valutazione finora
- Matlab Toolbox For PsychologyDocumento7 pagineMatlab Toolbox For PsychologyijudoptoNessuna valutazione finora
- Algorithm For Random Dot StereogramsDocumento22 pagineAlgorithm For Random Dot Stereogramsijudopto100% (1)
- Effects of Glare On VisionDocumento2 pagineEffects of Glare On VisionijudoptoNessuna valutazione finora
- Smith Test, Goniolens, Shadow TestDocumento3 pagineSmith Test, Goniolens, Shadow TestJLo100% (1)
- Retsimp 2013Documento9 pagineRetsimp 2013ijudoptoNessuna valutazione finora
- CancerEpi PDFDocumento441 pagineCancerEpi PDFMark EbrahimNessuna valutazione finora
- Bach Meigen 1999 PDFDocumento13 pagineBach Meigen 1999 PDFijudoptoNessuna valutazione finora
- Basic Human Visual Processing LectureDocumento6 pagineBasic Human Visual Processing LectureijudoptoNessuna valutazione finora
- ECVP 2012 Supplement AbstractsDocumento275 pagineECVP 2012 Supplement AbstractsijudoptoNessuna valutazione finora
- Avian Sensory Systems: Sensory World Similar To Ours, That of Other Primates, Primarily VisualDocumento30 pagineAvian Sensory Systems: Sensory World Similar To Ours, That of Other Primates, Primarily VisualijudoptoNessuna valutazione finora
- BenFiles An Introduction To EEGDocumento58 pagineBenFiles An Introduction To EEGJesus PeñaNessuna valutazione finora
- Pelli-Robson & ETDRS Score Sheet & InstructionsDocumento8 paginePelli-Robson & ETDRS Score Sheet & InstructionsPaul H Artes100% (3)
- The Age of ResearchDocumento4 pagineThe Age of ResearchijudoptoNessuna valutazione finora
- Progressive Lens Optics - Part 2Documento10 pagineProgressive Lens Optics - Part 2ijudopto100% (1)
- Notes On Progressive LensesDocumento9 pagineNotes On Progressive LensesijudoptoNessuna valutazione finora
- Pateras - Measurement of Prog Add Lenses With InterferometryDocumento12 paginePateras - Measurement of Prog Add Lenses With InterferometryijudoptoNessuna valutazione finora
- Spatial VisionDocumento13 pagineSpatial VisionijudoptoNessuna valutazione finora
- Effects of Refractive Error On Detection Acuity and Resolution Acuity in Peripheral VisionDocumento10 pagineEffects of Refractive Error On Detection Acuity and Resolution Acuity in Peripheral VisionijudoptoNessuna valutazione finora
- J Physiol 1968 Campbell 551 66Documento16 pagineJ Physiol 1968 Campbell 551 66ijudoptoNessuna valutazione finora
- Warping Constant of Open Sections With Arbitrary Profile Geometry Rev 1 2011Documento24 pagineWarping Constant of Open Sections With Arbitrary Profile Geometry Rev 1 2011hoojzteNessuna valutazione finora
- Ba101 Engineering Mathematics 1Documento21 pagineBa101 Engineering Mathematics 1nurhaiziinovasiNessuna valutazione finora
- Things To Remember When Writing Your Conference Proposal AbstractDocumento2 pagineThings To Remember When Writing Your Conference Proposal AbstractBalizkoa BadaezpadakoaNessuna valutazione finora
- Pasig Transparency OrdinanceDocumento9 paginePasig Transparency OrdinanceVico Sotto100% (3)
- Backup Archive and Recovery Archive Users and PermissionsDocumento5 pagineBackup Archive and Recovery Archive Users and PermissionsgabilovesadellaNessuna valutazione finora
- Stone ChapaisDocumento6 pagineStone ChapaisMaría GallardoNessuna valutazione finora
- Transcript Biu2032Documento5 pagineTranscript Biu2032Kuna KunavathiNessuna valutazione finora
- Chemistry Chemical EngineeringDocumento124 pagineChemistry Chemical Engineeringjrobs314Nessuna valutazione finora
- Windows Steady State HandbookDocumento81 pagineWindows Steady State HandbookcapellaNessuna valutazione finora
- Innoventure List of Short Listed CandidatesDocumento69 pagineInnoventure List of Short Listed CandidatesgovindmalhotraNessuna valutazione finora
- Exercise of English LanguageDocumento2 pagineExercise of English LanguageErspnNessuna valutazione finora
- HSG11 V3+AnswersDocumento10 pagineHSG11 V3+AnswershaNessuna valutazione finora
- Informal and Formal Letter Writing X E Sem II 2018 - 2019Documento15 pagineInformal and Formal Letter Writing X E Sem II 2018 - 2019Oana Nedelcu0% (1)
- Green ManagementDocumento58 pagineGreen ManagementRavish ChaudhryNessuna valutazione finora
- Pacific Plate Movement WorksheetDocumento3 paginePacific Plate Movement WorksheetJohn OsborneNessuna valutazione finora
- CLOCKSDocumento62 pagineCLOCKSdasarajubhavani05Nessuna valutazione finora
- Treasure HuntDocumento9 pagineTreasure HuntNutsdieyaa ErnieNessuna valutazione finora
- Carl Jung - CW 18 Symbolic Life AbstractsDocumento50 pagineCarl Jung - CW 18 Symbolic Life AbstractsReni DimitrovaNessuna valutazione finora
- Dürer's Rhinoceros Springer Esteban JMDocumento29 pagineDürer's Rhinoceros Springer Esteban JMmiguelestebanNessuna valutazione finora
- Quotient Tool An Holistic Assessment Tool For An Individual's Fit To A Specific Organizational RoleDocumento1 paginaQuotient Tool An Holistic Assessment Tool For An Individual's Fit To A Specific Organizational RoleCarina CovaNessuna valutazione finora
- 23 Encoding PDFDocumento5 pagine23 Encoding PDFBharghav RoyNessuna valutazione finora
- Lip Prints: IntroductionDocumento4 pagineLip Prints: Introductionkaran desaiNessuna valutazione finora
- DS - en 1991-1-7 DK Na - 2007 eDocumento6 pagineDS - en 1991-1-7 DK Na - 2007 ep_meulendijks108Nessuna valutazione finora
- 2011bibliography Part I (Preparation and Initial Assessment)Documento188 pagine2011bibliography Part I (Preparation and Initial Assessment)Espiritu MineralNessuna valutazione finora
- IO Chapter6 FinalDocumento10 pagineIO Chapter6 FinalJulia MoplaNessuna valutazione finora
- Topic 8 Class Notes1 PDFDocumento6 pagineTopic 8 Class Notes1 PDFMuhammad Adnan LaghariNessuna valutazione finora
- Sample MidtermDocumento7 pagineSample MidtermMuhammad WasifNessuna valutazione finora
- Ubd Food ChainDocumento5 pagineUbd Food Chainapi-313687749Nessuna valutazione finora
- فص یروئت Queuining TheoryDocumento47 pagineفص یروئت Queuining Theorycampal123Nessuna valutazione finora