Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Co-Infections and COVID-19 in Children An Observational Study
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Co-Infections and COVID-19 in Children An Observational Study
Copyright:
Formati disponibili
Volume 5, Issue 8, August – 2020 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
Co-infections and COVID-19 in Children:
An Observational Study
1.
Uzzal Kumar Ghosh
Registrar, Dept. of Paediatrics,
Dr. M R Khan Shishu Hospital& ICH, Mirpur-2, Dhaka.
2. 3.
MadhabiBaidya Azmeri Sultana
Assistant Professor,Dept. of Paediatric Gastroenterology Associate Professor, Dept. of Paediatrics, Dr. M R Khan
Hepatology and Nutrition, Dhaka Shishu (Children) Shishu Hospital & ICH,
Hospital. Mirpur-2, Dhaka.
4. 5.
Nobo Krishna Ghosh M. F. Abiduzzaman
Professor, Dept. of Paediatrics, Dr. M R Khan Shishu Registrar, Dept. of Paediatrics, Dr. M R Khan Shishu
Hospital & ICH, Mirpur-2, Dhaka. Hospital & ICH, Mirpur-2, Dhaka.
6. 7.
Joairya Yasmeen Bushra Md. ManiruzzamanNayan
Assistant Registrar, Dept. of Paediatrics, Dr. M R Khan Trainee, IbnSina Medical College & Hospital,
Shishu Hospital & ICH, Mirpur-2, Dhaka. Kallaynpur, Dhaka.
Abstract:- withCOVID-191 (3.3%), bacterial pneumonia
withCOVID-191 (3.3%) were found. RT-PCR was
Background: positive forCOVID-1930(100%), blood culture was
Acute illnessis causedby bacteria, viruses, and positive for Salmonella Typhi 4(13.3%), Widal test was
parasites.Co-infection is the simultaneous infectionof a reactive (high rising titer) 8(26.7%), Latex agglutination
host by multiple pathogens resulting in a delay in test was positive for bacterial meningitis 6(20%), urine
diagnosis and bad prognosis.Currently,coronavirus culture was positive for E.coli 3(10%), blood culture was
infection is a pandemic and global health concern. positive for Salmonella Para typhi A 2(6.7%), Weil-Felix
Coronavirus infection in children withconcomitant other reaction was found (high rising titer) 2(6.7%), Anti HAV
infections is rarely reported in our country. This study IgM was positive 2(6.7%), Anti HEV IgM was positive
was performed to find out the coronavirus 1(3.3%), Blood culturewas positive (staph.aureus) for
infectionassociated with recent illnesses to minimize septic arthritis 1(3.3%), blood culture was positive
morbidity and mortality. (strep. pneumoniae) for bacterialPneumonia 1(3.3%).
Methodology: Conclusion:
The study was done at Dr. M R Khan Shishu This study showed that COVID-19 in Bangladeshi
Hospital & ICH from April 2020 to June 2020. Patients children was found associated with co-infections. So, co-
with fever, rash, vomiting, diarrhea, cough, respiratory infection with COVID-19 patients should be closely
distress, dysuria, convulsion, jaundice, and other monitored and managed accordingly.
symptoms; admitted in the hospital were taken for this
study. The diagnosis was made by clinical symptoms Keywords: -Co-infections, COVID-19.
plus investigations accordingly and appropriate
treatment was given for recent illnesses. During follow I. INTRODUCTION
up these cases; there was the persistence of symptoms
and some other new features appeared. These arouse our Coronaviruses (CoVs) are enveloped, single-stranded,
suspicion that there might be associated with zoonotic, RNA viruses ofa large family. The novel CoVs
coronavirus infection in this pandemic. severe acute respiratory syndrome coronavirus (SARS-CoV)
emerged in 2002. The 2019 novel coronavirus (SARS-CoV-
Results: 2) is currently causing a severe outbreak of disease (called
Thirty cases were taken co-infection with COVID- COVID-19) in China and multiple other countries including
19.Age was found 4 months to 8 years.The male-female Bangladesh. Now it is a pandemic and global health
ratio was 1.5:1.Typhoid fever with COVID-1912(40%), concern. In humans, CoVs mostly cause respiratory and
Bacterial meningitis with COVID-196(20%), UTI with gastrointestinal symptoms. Clinical manifestations range
COVID-19 3(10%), Paratyphoid fever with COVID- from a common cold to severe diseases such as
192(6.7%), Typhus/ Rickettsial fever withCOVID-19 bronchiolitis, pneumonia, ARDS, inflammatory syndrome,
2(6.7%),HAV infection withCOVID-192(6.7%),HEV multi-organ failure, and even death. SARS-CoV and SARS-
infection withCOVID-19 1 (3.3%), Septic arthritis CoV-2 less commonly affect children and less severe
IJISRT20AUG156 www.ijisrt.com 343
Volume 5, Issue 8, August – 2020 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
disease compared with adults and are associated with lower prognosis. This study was performed to find out the
fatality. Evidence suggests children are as likely as adults to coronavirus infection associated with recent illnesses.
become infected with SARS-CoV-2 but are less likely to be
symptomatic. The majority of children infected by novel II. METHODOLOGY
CoVs have documented household contact. In contrast,
adults more often have nosocomial exposure. 1 An observational study was done at Dr. M R Khan
Shishu Hospital & ICH, Mirpur-2, Dhaka from April 2020
According toNational Guidelines on Clinical to June 2020. Patients with fever, rash, cough, respiratory
Management of Coronavirus Disease 2019 (COVID-19) in distress, vomiting, diarrhea, dysuria, convulsion, jaundice,
Bangladesh shows corona symptoms are Mild illness and other symptoms; admitted in the hospital were taken for
(Influenza-like illness-ILI), Pneumonia, Severe pneumonia, this study. The diagnosis was made by clinical symptoms
Acute respiratory distress syndrome, Sepsis, Septic shock. 2 criteria plus investigations accordingly and appropriate
treatment was given. During follow up these cases; we
Common symptoms of COVID-19 in children are observed that those patients had persistence of high-grade
cough and fever. It is important to note that these symptoms non-remitting fever, rash, vomiting,burking/dry cough,
may not always be present; thus, a high index of suspicion deepening of jaundice, uncontrolled convulsion& some
for SARS-CoV-2 infection is required in children.3 other new features appeared. These features could not be
correlated with the specific disease symptomsdespite getting
China and the United States reported only about 2.4% appropriate treatment. These arouse our suspicion that there
coronavirus infection among children where age was under might be some associated with coronavirus infection in this
19 years.4, 5. Most cases in children are mild, and treatment pandemic. Then nasopharyngeal and oropharyngeal swab
consists of supportive care. No drugs or biologics have been was taken and sent for RT-PCR for COVID-19. Typhoid
approved by the US Food and Drug Administration (FDA) and paratyphoid feverwere diagnosed by either blood culture
for the prevention or treatment of COVID-19, and no or very high titer of Widal test where T: O/A: Omore than
vaccine is currently available. 6 1:320 and rising titer subsequently. Typhus fever was
identified by Weil-Felix reaction OX titer of 1:320 or an
UK study says the majority of patients under 18 years increasein OX titer in the follow-up. Bacterial meningitis
old experienced a mild disease and less than 1% of them was diagnosed by CSF studywitha bacterial Antigen test
died.7 (Latex agglutination test). Hepatitis A virus infection was
diagnosed by a rapid very high rise ofSGPT, prolonged PT,
A study of European children with COVID-19 rising of serum bilirubin, and Anti HAV IgM positive.
suggests deaths are extremely rare. Four of the 582 children Hepatitis E virus infection was identified by abnormal liver
studied died, two of whom had known underlying health function tests with Anti-HEV IgM positive. Pneumonia
conditions. Children's symptoms were generally mild. Some causing organisms isolated by blood culture. Septic arthritis
who tested positive had no symptoms, but about one in 10 in was diagnosed by blood culture and X-ray of the affected
the study needed intensive care.8 joint. Urinary tract infection by urine routine microscopic
examination& urine culture positive for an organism with
Nearly one-half of the infected children had co- significant colony count.Co-infection with COVID-19 was
infection with other common respiratory pathogens. 9Fourty our case experience (N).
patients (83%) had significant preexisting comorbidities. 10
III. RESULTS
Acute illness is caused by bacteria, viruses, and
parasites. Co-infection is the simultaneous infection of a Thirty cases were taken co-infection withCOVID-
host by multiple pathogens. COVID-19 in children with 19.Here sample size N=30
other infections is rarely reported in our country. In this
pandemic situation, children with recent illnesses may be Age was found 4 months to 8 years.
associated with coronavirus infection. Recent illness is non-
responding to conventional & appropriate treatment or Among the patients of co-infection withCOVID-19;
deteriorating or atypically present; when they are might be the male was 18 (60%) and the female was 12 (40%). The
associated with coronavirus infection. COVID-19 symptoms male-female ratio was 1.5: 1 (Table I)
may mimic with various other diseases. The febrile phase of
dengue fever, typhoid fever, paratyphoid fever, typhusor Gender Number (n) Percentage (%)
rickettsial fever, malaria, and many other diseases may Male 18 60
overlap with the coronavirus infection that leads to
Female 12 40
substantial misdiagnosis.
Table I showing the gender distribution of the study sample
In this view, a high index of suspicion, careful (N= 30)
attention to the clinical course, and RT-PCR are necessary
to identify the coronavirus infection with recent illnesses. Among the patients of different infections with
Delay in diagnosis of associated COVID-19 results bad COVID-19; Typhoid fever with COVID-19was12(40%),
Bacterial meningitis with COVID-19 was 6(20%), UTI with
IJISRT20AUG156 www.ijisrt.com 344
Volume 5, Issue 8, August – 2020 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
COVID-19 was3(10%), Paratyphoid fever with COVID-19 infection) with COVID-19 was1 (3.3%), Septic arthritis with
was2(6.7%), Typhus/Rickettsial fever with COVID-19 COVID-19 was1 (3.3%), Bacterial pneumonia withCOVID-
was2(6.7%), Acute viral hepatitis (HAV infection) with 19 was1 (3.3%). (Table II)
COVID-19 was2(6.7%), Acute viral hepatitis (HEV
Diagnosis Number (n) Percentage (%)
Typhoid fever with COVID-19 12 40
Bacterial meningitis with COVID-19 6 20
UTI with COVID-19 3 10
Paratyphoid fever with COVID-19 2 6.7
Typhus/Rickettsial fever with COVID-19 2 6.7
Acute viral hepatitis (HAV infection) with COVID-19 2 6.7
Acute viral hepatitis (HEV infection) with COVID-19 1 3.3
Septic arthritis with COVID-19 1 3.3
Bacterial pneumonia with COVID-19 1 3.3
Table II: - showing different disease pattern with COVID-19 (N= 30)
RT-PCR was positive for COVID-1930(100%), blood Anti HAV IgMwas positive (hepatitis A virus
culture was positive for Salmonella Typhi 4(13.3%),Widal infection)2(6.7%), Anti HEV IgMwas positive (hepatitis E
test was reactive (high rising titer) 8(26.7%), Latex virus infection) 1(3.3%), Blood culture was positive
agglutination test was positive for Bacterial meningitis (staphylococcusaureus) for Septic arthritis 1(3.3%), blood
6(20%), urine culture was positive for E.coli 3(10%), blood culture was positive (StreptococcusPneumoniae) for
culture was positive for Salmonella Paratyphi A bacterial pneumonia 1(3.3%) (Table III)
2(6.7%),Weil-Felixreaction (high rising titer)was2(6.7%),
Attributes Number (n) Percentage (%)
COVID-19
RT-PCR positive 30 100
Enteric fever
Blood C/S positive for S. typhi 4 13.3
Widal test reactive 8 26.7
Bacterial Meningitis
Latex agglutination test positive 6 20
Urinary tract infection
Urine C/S positive for E. coli (more than 105) 3 10
Blood C/S positive for S. paratyphi A 2 6.7
Typhus fever
Weil-Felix reaction 2 6.7
Acute viral hepatitis
Anti HAV IgM positive 2 6.7
Anti HEV IgM positive 1 3.3
Septic Arthritis
Blood C/S positive for Staphylococcusaureus 1 3.3
Bacterial pneumonia
Blood C/S positive for streptococcusPneumoniae 1 3.3
Table III showing the pattern of investigation findings for the diagnosis of different disease with COVID-19 (N=30)
IV. DISCUSSION was 2 cases, Typhus/Rickettsial fever with COVID-19 was 2
cases, Acute viral hepatitis (HAV infection) with COVID-
In this study, 30 cases of co-infection with COVID-19 19 was 2 cases, Acute viral hepatitis (HEV infection) with
were taken. Age was found 4 months to 8 years. Among the COVID-19 was one case, Septic arthritis with COVID-19
patients of co-infection with COVID-19; the male was 18 was one case, bacterial pneumonia with COVID-19 was one
and the female was 12. case.
Among the 30 patients of different infections with All cases were RT-PCR positive for COVID-19. Blood
COVID-19; Typhoid fever with COVID-19 was 12 cases, culture was positive for Salmonella Typhi 4 cases, Widal
Bacterial meningitis with COVID-19 was 6 cases, UTI with test was reactive (high rising titer) 8 cases, Latex
COVID-19 was 3 cases, Paratyphoid fever with COVID-19 agglutination test was positive for Bacterial meningitis 6
IJISRT20AUG156 www.ijisrt.com 345
Volume 5, Issue 8, August – 2020 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
cases, urine culture was positive for E.coli 3 cases, blood inthe following day, the COVID-19 PCR was also
culture was positive for Salmonella Paratyphi A 2 cases, positive.17
Weil-Felix reaction (high rising titer) was 2 cases, Anti
HAV IgM was positive (hepatitis A virus infection 2 cases, Bangladesh is a small developing country.The
Anti HEV IgM was positive (hepatitis E virus infection) one population is gradually increasing and theylive in
cases, blood culture was positive for Septic arthritis one overcrowded places. Sanitation system, water supply
case, blood culture was positive for system, disinfection system is still developing. So
streptococcusPneumoniae one case. communicable diseases, infectious diseases, waterborne
diseases, mosquito-borne diseases are common.But
In this study, Bangladeshi children were found typhoid successful EPI vaccination program in Bangladesh reduces
fever with COVID-19 as a co-infection communicable and infectious diseasesassociated with
predominantly.COVID-19 and Salmonella Typhi co- morbidity and mortality.
epidemics in Pakistan. Those articles have pointed out the
impact of co-epidemics/co-infections of COVID-19 and V. LIMITATION
other infectious diseases on an all ready overburdened.
Pakistan is entirely occupied with the COVID-19 Severity and outcome of co-infections with COVID-19
catastrophe; simultaneously around 20000 typhoid cases could not have mentioned in our study. Virus isolation could
within 10 days of June 2020 have also been reported along not be possible in our settings. So, co-infection by other
with COVID-19.11 viruses along with coronavirus missed identifying.
Dengue and COVID-19 co-infection is a deadly VI. CONCLUSION
combination. Still in Bangladesh dengue is a major public
health problem. Every year many people including children This study showed thatCOVID-19 inBangladeshi
die due to dengue fever with its complication.Althoughit children were found associated with co-infections. So, co-
was an important concern in our study no case was infection with COVID-19patients should be closely
identified of dengue fever with COVID-19. A case has been monitored and managed accordingly. Here, we have to
reported, co-infection of dengue and COVID-19; share mention that childhood disease pattern depends on different
common clinical and laboratory features.12 epidemiological and geographical location. So, the co-
infection pattern with COVID-19 can vary. But our study
Our study showed bacterial meningitis with COVID- concluded that co-infection is not very uncommon with
19 as a co-infection.A case report of nosocomial infection COVID-19.
with SARS CoV-2 in a one-year-old Meningoencephalitis
patient in a tertiary hospital of Bangladesh.13 RECOMMENDATION
We found acute hepatitis with COVID-19 as a co- Co-morbidities are a great concern with COVID-19.
infection with the hepatitis A or hepatitis E virus.A study So, co-infection with COVID-19 might be a concern also.
was found where COVID-19 presenting as Acute Epidemiological and geographical basis study is
Hepatitis.14 recommended.
Pediatric patients with COVID-19 presented with Conflict of interest
distinct epidemiological, clinical, and radiologic No conflict of interest.
characteristics from adult patients. Nearly one-half of the
infected children had co-infection with other common ACKNOWLEDGEMENT
respiratory pathogens. 15
Grateful to all the Authors of Dr. M R Khan Shishu hospital
One case reported in our study was & Institute of Child Health, and Dhaka Shishu
streptococcuspneumoniae with coronavirus infection as a (Children) Hospital.
co-infection. In children, the co-infection rate was seen for
adenovirus C and influenza B virus at 68.4%, 10.7% REFERENCES
respectively. Significantly lower co-infection rates were
seen for influenza viruses and human metapneumovirus [1]. Zimmermann, Petra, Curtis, Nigel. Coronavirus
compared with other viral strains. Rhinovirus was identified Infections in Children Including COVID-19. The
associated with the most co-infections overall and co- Pediatric Infectious Disease Journal, May 2020; 39(5):
infection rate in children at 33.3%, where adults were only 355-368. DOI:10.1097/INF.0000000000002660.
5%.16 [2]. National Guidelines on Clinical Management of
Coronavirus Disease 2019 (COVID-19); Version 4.0
A case reported a 4-month-old boy with a muscular 30 March 2020: Disease Control Division, Directorate
ventricular septal defect and atopic dermatitis presentedwith General of Health Services, Ministry of Health &
gastroenteritis and respiratory tract infection with a Family Welfare, Government of the People's Republic
documented history of home exposure to COVID-19. The of Bangladesh. Page 9-10.
initial respiratory pathogen was positive for adenovirus. But
IJISRT20AUG156 www.ijisrt.com 346
Volume 5, Issue 8, August – 2020 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
[3]. Issa B, Cennimo DJ. Coronavirus Disease 2019 diseases/symptoms Case report 2020; 13(6):
(COVID-19) in Children. Medscape. Drugs & http://orcid.org/0000-0003-0726-6349.
Diseases>Pediatrics: General Medicine; updated Jul
23, 2020.
[4]. WHO. Report of the WHO-China Joint Mission on
Coronavirus Disease 2019 (COVID-19). World Health
Organization. 2020 Feb 28; Accessed: April 9, 2020.
[5]. CDC COVID-19 Response Team. Coronavirus
Disease in Children- United States, February 12-April
2, 2020; 69 (14):422-6.
[6]. NIH Clinical Trial Shows Remdesivir Accelerates
Recovery from advanced COVID-19. National
Institute of Allergy and Infectious Diseases
(NIAID).2020 Apr 29.
[7]. Dr. Ayodola Adigun. COVID-19 disease in children is
usually mild, fatalities rare, Abc News Coronavirus
Health & Science 26 June 2020.
[8]. Coronavirus: Most children ‘experience only mild
disease’. Health: BBC News 26 June 2020.
[9]. Wu Q, Xing Y, Shi L, Li W. Co-infection, and Other
Clinical Characteristics of COVID-19 in Children.
Pediatrics May 2020; 146(1):e20200961. DOI:
10.1542/peds.2020-0961.
[10]. Shekerdemian LS, Mahmood NR, Wolfe KK, Riggs
BJ, Ross CE, Christine AC et al. Characteristics and
Outcomes of Children with Coronavirus Disease 2019
(COVID-19) Infection Admitted to US and Canadian
Pediatric Intensive Care Units. JAMA Pediatr. May
11, 2020.doi:10.1001/jamapediatrics.2020.1948.
[11]. Haqqi A, Khurram M, Salah Ud Din M, Aftab MN,
Ali M, Ahmed H, Afzal MS. COVID-19, and
Salmonella Typhi co-epidemics in Pakistan: A real
problem 10 Jul 2020. DOI: 10.1002/jmv.26293.
[12]. Verduyn M, Allou N, Gazaille V, Andre M, Desroche
T, Jaffar M-C, et al. (2020) Co-infection of dengue and
COVID-19: A case report. PLoSNegl Trop Dis 14(8):
e0008476.
https://doi.org/10.1371/journal.pntd.0008476.
[13]. Akram A, Jewel MSH, Chowdhury R, Chowdhury
MRU. A case report of nosocomial infection with
SARS CoV-2 in a one-year-old Meningoencephalitis
patient in a tertiary hospital of Bangladesh. Microbes
and Infectious Diseases, 2020.
[14]. Wander P, Epstein M, Bernstein D. COVID-19
Presenting as Acute Hepatitis. The American Journal
of Gastroenterology 1 April 2020; 115(6): DOI:
10.14309/ajg.0000000000000660.
[15]. Wu Q, Xing Y, Shi L, Li W, Gao Y, Pan S, Wang Y,
Wang W, Xing Q. Co-infection and Other Clinical
Characteristics of COVID-19 in Children. Pediatrics
July 2020, 146 (1) e20200961; DOI:
https://doi.org/10.1542/peds.2020-0961.
[16]. Mandelia Y, Procop GW, Richter SS, Worley S, Liu
W, Esper F. Dynamics and predisposition of
respiratory viral co-infections in children and adults
[published online June 12, 2020].
ClinMicrobiolInfect.doi: 10.1016/j.cmi.2020.05.042.
[17]. Danley K, Kent P. 4-month-old boy coinfected with
COVID-19 and adenovirus.Unusual association of
IJISRT20AUG156 www.ijisrt.com 347
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (894)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- THE DOSE, Issue 1 (Tokyo)Documento142 pagineTHE DOSE, Issue 1 (Tokyo)Damage85% (20)
- Real Estate Broker ReviewerREBLEXDocumento124 pagineReal Estate Broker ReviewerREBLEXMar100% (4)
- Gapped SentencesDocumento8 pagineGapped SentencesKianujillaNessuna valutazione finora
- Formulation and Evaluation of Poly Herbal Body ScrubDocumento6 pagineFormulation and Evaluation of Poly Herbal Body ScrubInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Comparatively Design and Analyze Elevated Rectangular Water Reservoir with and without Bracing for Different Stagging HeightDocumento4 pagineComparatively Design and Analyze Elevated Rectangular Water Reservoir with and without Bracing for Different Stagging HeightInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Explorning the Role of Machine Learning in Enhancing Cloud SecurityDocumento5 pagineExplorning the Role of Machine Learning in Enhancing Cloud SecurityInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- A Review: Pink Eye Outbreak in IndiaDocumento3 pagineA Review: Pink Eye Outbreak in IndiaInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Design, Development and Evaluation of Methi-Shikakai Herbal ShampooDocumento8 pagineDesign, Development and Evaluation of Methi-Shikakai Herbal ShampooInternational Journal of Innovative Science and Research Technology100% (3)
- Studying the Situation and Proposing Some Basic Solutions to Improve Psychological Harmony Between Managerial Staff and Students of Medical Universities in Hanoi AreaDocumento5 pagineStudying the Situation and Proposing Some Basic Solutions to Improve Psychological Harmony Between Managerial Staff and Students of Medical Universities in Hanoi AreaInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- A Survey of the Plastic Waste used in Paving BlocksDocumento4 pagineA Survey of the Plastic Waste used in Paving BlocksInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Electro-Optics Properties of Intact Cocoa Beans based on Near Infrared TechnologyDocumento7 pagineElectro-Optics Properties of Intact Cocoa Beans based on Near Infrared TechnologyInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Auto Encoder Driven Hybrid Pipelines for Image Deblurring using NAFNETDocumento6 pagineAuto Encoder Driven Hybrid Pipelines for Image Deblurring using NAFNETInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Cyberbullying: Legal and Ethical Implications, Challenges and Opportunities for Policy DevelopmentDocumento7 pagineCyberbullying: Legal and Ethical Implications, Challenges and Opportunities for Policy DevelopmentInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Navigating Digitalization: AHP Insights for SMEs' Strategic TransformationDocumento11 pagineNavigating Digitalization: AHP Insights for SMEs' Strategic TransformationInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Hepatic Portovenous Gas in a Young MaleDocumento2 pagineHepatic Portovenous Gas in a Young MaleInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Review of Biomechanics in Footwear Design and Development: An Exploration of Key Concepts and InnovationsDocumento5 pagineReview of Biomechanics in Footwear Design and Development: An Exploration of Key Concepts and InnovationsInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Automatic Power Factor ControllerDocumento4 pagineAutomatic Power Factor ControllerInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Formation of New Technology in Automated Highway System in Peripheral HighwayDocumento6 pagineFormation of New Technology in Automated Highway System in Peripheral HighwayInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Drug Dosage Control System Using Reinforcement LearningDocumento8 pagineDrug Dosage Control System Using Reinforcement LearningInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- The Effect of Time Variables as Predictors of Senior Secondary School Students' Mathematical Performance Department of Mathematics Education Freetown PolytechnicDocumento7 pagineThe Effect of Time Variables as Predictors of Senior Secondary School Students' Mathematical Performance Department of Mathematics Education Freetown PolytechnicInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Mobile Distractions among Adolescents: Impact on Learning in the Aftermath of COVID-19 in IndiaDocumento2 pagineMobile Distractions among Adolescents: Impact on Learning in the Aftermath of COVID-19 in IndiaInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Securing Document Exchange with Blockchain Technology: A New Paradigm for Information SharingDocumento4 pagineSecuring Document Exchange with Blockchain Technology: A New Paradigm for Information SharingInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Perceived Impact of Active Pedagogy in Medical Students' Learning at the Faculty of Medicine and Pharmacy of CasablancaDocumento5 paginePerceived Impact of Active Pedagogy in Medical Students' Learning at the Faculty of Medicine and Pharmacy of CasablancaInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Intelligent Engines: Revolutionizing Manufacturing and Supply Chains with AIDocumento14 pagineIntelligent Engines: Revolutionizing Manufacturing and Supply Chains with AIInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Enhancing the Strength of Concrete by Using Human Hairs as a FiberDocumento3 pagineEnhancing the Strength of Concrete by Using Human Hairs as a FiberInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Exploring the Clinical Characteristics, Chromosomal Analysis, and Emotional and Social Considerations in Parents of Children with Down SyndromeDocumento8 pagineExploring the Clinical Characteristics, Chromosomal Analysis, and Emotional and Social Considerations in Parents of Children with Down SyndromeInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Supply Chain 5.0: A Comprehensive Literature Review on Implications, Applications and ChallengesDocumento11 pagineSupply Chain 5.0: A Comprehensive Literature Review on Implications, Applications and ChallengesInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Teachers' Perceptions about Distributed Leadership Practices in South Asia: A Case Study on Academic Activities in Government Colleges of BangladeshDocumento7 pagineTeachers' Perceptions about Distributed Leadership Practices in South Asia: A Case Study on Academic Activities in Government Colleges of BangladeshInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Advancing Opthalmic Diagnostics: U-Net for Retinal Blood Vessel SegmentationDocumento8 pagineAdvancing Opthalmic Diagnostics: U-Net for Retinal Blood Vessel SegmentationInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- The Making of Self-Disposing Contactless Motion-Activated Trash Bin Using Ultrasonic SensorsDocumento7 pagineThe Making of Self-Disposing Contactless Motion-Activated Trash Bin Using Ultrasonic SensorsInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Natural Peel-Off Mask Formulation and EvaluationDocumento6 pagineNatural Peel-Off Mask Formulation and EvaluationInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Beyond Shelters: A Gendered Approach to Disaster Preparedness and Resilience in Urban CentersDocumento6 pagineBeyond Shelters: A Gendered Approach to Disaster Preparedness and Resilience in Urban CentersInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Handling Disruptive Behaviors of Students in San Jose National High SchoolDocumento5 pagineHandling Disruptive Behaviors of Students in San Jose National High SchoolInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Beauty ProductDocumento12 pagineBeauty ProductSrishti SoniNessuna valutazione finora
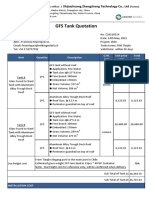
- GFS Tank Quotation C20210514Documento4 pagineGFS Tank Quotation C20210514Francisco ManriquezNessuna valutazione finora
- SOP-for RecallDocumento3 pagineSOP-for RecallNilove PervezNessuna valutazione finora
- Product Data Sheet For CP 680-P and CP 680-M Cast-In Firestop Devices Technical Information ASSET DOC LOC 1540966Documento1 paginaProduct Data Sheet For CP 680-P and CP 680-M Cast-In Firestop Devices Technical Information ASSET DOC LOC 1540966shama093Nessuna valutazione finora
- A Princess of Mars Part 3Documento4 pagineA Princess of Mars Part 3Sheila Inca100% (1)
- Typical T Intersection On Rural Local Road With Left Turn LanesDocumento1 paginaTypical T Intersection On Rural Local Road With Left Turn Lanesahmed.almakawyNessuna valutazione finora
- EA Linear RegressionDocumento3 pagineEA Linear RegressionJosh RamosNessuna valutazione finora
- Mrs. Universe PH - Empowering Women, Inspiring ChildrenDocumento2 pagineMrs. Universe PH - Empowering Women, Inspiring ChildrenKate PestanasNessuna valutazione finora
- Simba s7d Long Hole Drill RigDocumento2 pagineSimba s7d Long Hole Drill RigJaime Asis LopezNessuna valutazione finora
- Alternate Tuning Guide: Bill SetharesDocumento96 pagineAlternate Tuning Guide: Bill SetharesPedro de CarvalhoNessuna valutazione finora
- Emergency Management of AnaphylaxisDocumento1 paginaEmergency Management of AnaphylaxisEugene SandhuNessuna valutazione finora
- Steps To Christ AW November 2016 Page Spreaad PDFDocumento2 pagineSteps To Christ AW November 2016 Page Spreaad PDFHampson MalekanoNessuna valutazione finora
- OS LabDocumento130 pagineOS LabSourav BadhanNessuna valutazione finora
- Guia de Usuario GPS Spectra SP80 PDFDocumento118 pagineGuia de Usuario GPS Spectra SP80 PDFAlbrichs BennettNessuna valutazione finora
- Tutorial 1 Discussion Document - Batch 03Documento4 pagineTutorial 1 Discussion Document - Batch 03Anindya CostaNessuna valutazione finora
- SEC QPP Coop TrainingDocumento62 pagineSEC QPP Coop TrainingAbdalelah BagajateNessuna valutazione finora
- Busbar sizing recommendations for Masterpact circuit breakersDocumento1 paginaBusbar sizing recommendations for Masterpact circuit breakersVikram SinghNessuna valutazione finora
- Qad Quick StartDocumento534 pagineQad Quick StartMahadev Subramani100% (1)
- Bad DayDocumento3 pagineBad DayLink YouNessuna valutazione finora
- Dance Appreciation and CompositionDocumento1 paginaDance Appreciation and CompositionFretz Ael100% (1)
- October 2009 Centeral Aucland, Royal Forest and Bird Protecton Society NewsletterDocumento8 pagineOctober 2009 Centeral Aucland, Royal Forest and Bird Protecton Society NewsletterRoyal Forest and Bird Protecton SocietyNessuna valutazione finora
- Differential Pulse Code ModulationDocumento12 pagineDifferential Pulse Code ModulationNarasimhareddy MmkNessuna valutazione finora
- LSMW With Rfbibl00Documento14 pagineLSMW With Rfbibl00abbasx0% (1)
- Empanelment of Architect-Consultant - Work Costing More Than 200 Lacs. (Category-B)Documento6 pagineEmpanelment of Architect-Consultant - Work Costing More Than 200 Lacs. (Category-B)HARSHITRAJ KOTIYANessuna valutazione finora
- Ecc Part 2Documento25 pagineEcc Part 2Shivansh PundirNessuna valutazione finora
- !!!Логос - конференц10.12.21 копіяDocumento141 pagine!!!Логос - конференц10.12.21 копіяНаталія БондарNessuna valutazione finora
- Excess AirDocumento10 pagineExcess AirjkaunoNessuna valutazione finora