Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
[03241750 - Acta Medica Bulgarica] Extraintestinal Manifestations and Intestinal Complications in Patients with Crohn's Disease_ Associations with Some Clinico-Laboratory Findings, Immunological Markers and Therapy.pdf
Caricato da
TeodorCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
[03241750 - Acta Medica Bulgarica] Extraintestinal Manifestations and Intestinal Complications in Patients with Crohn's Disease_ Associations with Some Clinico-Laboratory Findings, Immunological Markers and Therapy.pdf
Caricato da
TeodorCopyright:
Formati disponibili
10.
2478/AMB-2018-0003
EXTRAINTESTINAL MANIFESTATIONS AND INTESTINAL
COMPLICATIONS IN PATIENTS WITH CROHN'S DISEASE:
ASSOCIATIONS WITH SOME CLINICO-LABORATORY
FINDINGS, IMMUNOLOGICAL MARKERS AND THERAPY
Ts. Velikova1, R. Miladinova2, E. Ivanova-Todorova3, D. Kyurkchiev3, Z. Spasova4
1
Clinical Immunology, University Hospital “Lozenetz” – Sofia, Bulgaria
2
Clinic of Nephrology, University Hospital “Sv. Ivan Rilski”, Medical University – Sofia, Bulgaria
3
Laboratory of Clinical Immunology, University Hospital “Sv. Ivan Rilski”,
Department of Clinical Laboratory and Clinical Immunology, Medical University – Sofia, Bulgaria
4
Clinic of Gastroenterology, University Hospital “Sv. Ivan Rilski”, Medical University – Sofia, Bulgaria
Abstract. Crohn's disease (CD) may have some severe complications that pose an in-
creasing health burden and negatively impact the quality of life. There are two major
types – intestinal and extraintestinal complications, in which immune and non-immune
mechanisms take place. We aimed to search for some associations between specific ex-
traintestinal manifestation and intestinal complications in CD patients with some clinical-
laboratory findings, immunological markers, and the therapy administered. We examined
retrospectively medical files of 26 patients with CD at mean age 42 ± 13 years, including
the laboratory results. The immunological markers fecal calprotectin (FC) and fecal lacto-
ferrin (FL) were assessed in frozen fecal samples of the chosen patients. Seventy-three
percent of the investigated CD patients had some extraintestinal manifestation and/or
intestinal complications, at least 13/26 had intestinal complications. All three patients with
extraintestinal signs were positive for FC and 2/3 were positive for FL. We observed a
higher serum level of CRP (24.49 mg/l vs. 3.13 mg/l, p = 0.010), slightly lowered serum
level of hemoglobin (120 g/l vs. 145 g/l, p = 0.044) and about 2-fold lower iron level (7.23
μmol/l vs. 14.0 μmol/l, p = 0.019) in patients with intestinal complications compared to
patients without complications, respectively. Four out of thirteen patients with intestinal
complications were without immunosuppressive therapy at the time of our study, and nine
out of thirteen – on immunosuppressive drugs. Routine laboratory and immunology test-
ing could be beneficial for gastroenterologists in identifying patients at high risk for the
development of complications and in the decision making for more aggressive therapy
early after diagnosis.
Key words: Crohn`s disease, complications, fecal calprotectin, fecal lactoferrin, immunosup-
pressive drugs
Corresponding author: Tsvetelina Velikova, MD, PhD, e-mail: ts_velikova@abv.bg
16 Acta Medica Bulgarica, Vol. XLV, 2018, № 1 // Original article
INTRODUCTION Extraintestinal features in CD patients are presented
as eye complications, arthropathy, skin and oral le-
C
rohn’s disease (CD) is a chronic inflammatory sions, delayed growth in children, etc. Some of these
disorder which may involve every part of the complications may have an association with disease
gastrointestinal tract. The illness often passes activity, like episcleritis, but others, i.e., pyoderma
asymptomatically and may take up to several years to gangrenosum, may not correlate with disease activ-
be diagnosed [1]. CD may have some severe compli- ity [3]. However, in general, extraintestinal manifesta-
cations which negatively impact the quality of life and tions tend to follow the clinical course of CD and may
could lead to necessity of surgical treatment [2]. The have huge impact on the quality of life, morbidity and
complications in patients with CD are two major types even mortality [3, 5, 6]. The complications that are
– intestinal and extraintestinal [3]. The most common associated with the activity of CD could respond to
intestinal complications are an obstruction, formation treatment of the bowel disease, but there is no spe-
of a fistula, perforation, abscesses forming a collec- cific treatment available for them [5]. Some condi-
tion of pus, and intestinal bleeding [4]. Patients are tions are associated with the damaged function of the
obliged to the chronic inflammation that produces intestine, like gallstones and kidney stones, anemia,
scar tissue known as stricture and deep ulcers, which osteomalacia, sensory disturbances (zinc deficiency,
are very peculiar for CD [1]. It is thought that immune vitamin B deficiency) [1]. The delicate mechanism is
and genetic factors (as HLA genes) are involved in related to the impaired absorption and malnutrition or
the pathogenesis of extraintestinal manifestations. the side effects of therapy (Figure 1) [7].
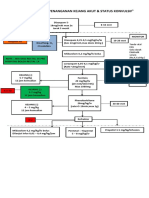
Fig. 1. The most frequent extraintestinal complications in Crohn's disease patients (Courtesy of Spekhorst, BMJ Open, 2017)
Both intestinal and extraintestinal complications crucial these complications and manifestations to be
contribute to increased morbidity and mortality of uncovered in time. The complications can occur, par-
patients with CD. Thus, they are of growing health ticularly during frequent or severe flare-ups [1]. Since
burden for these patients. This is the reason why it is there are some validated laboratory and immunologi-
Extraintestinal manifestations and intestinal complications... 17
cal findings (i.e., CRP, ESR, fecal calprotectin, etc.) sum (n = 1), and intestinal complications: fistulas (n =
that may be used to assess the disease activity, we 6), obstructions (n = 2), anal fissures (n = 4). We also
aimed to search for some associations between spe- used the laboratory findings of the medical files for C-
cific extraintestinal manifestation and intestinal com- reactive protein, iron, and hemoglobin in serum.
plications in CD patients with some clinico-laboratory
Immunological methods
findings and immunological markers. We also ques-
tioned whether the therapy administered influences The immunological markers fecal calprotectin (FC)
the occurrence of complications. and fecal lactoferrin (FL) were assessed in frozen
(-80°C) fecal samples of the patients by perform-
ing qualitative card-tests (One step card test, Cert-
MATERIALS AND METHODS
est, Spain) at the Laboratory of Clinical Immunology,
Patients University Hospital “Sv. Ivan Rilski”, Sofia, according
to manufacturer’s instructions. The methods were
We examined retrospectively medical files of 26 pa-
tients with CD, diagnosed and treated in the Clinic based on lateral immunochromatographic diffusion,
of Gastroenterology at University Hospital “Sv. Ivan and the cut-off for both tests was 50 mg/kg.
Rilski” from 2011 to 2012. The diagnosis was con- Statistical methods
firmed by colonoscopy plus biopsy and MRI.
We performed descriptive statistics, T-test, correla-
All patients have signed the informed agreement, tion and other analytical techniques to achieve the
and the study was approved by the Ethic Committee aim of the study by using SPSS v.19 (IBM). We ac-
of the Medical University of Sofia.
cept the results as significant if p < 0.05.
Eight men (30.8%) and 18 women (69.2%) at mean
age 42 ± 13 years (range 21-71 years) were exam-
RESULTS
ined. The activity of the disease was assessed by
CDAI (Crohn’s disease activity index). The over- Overall, 19 (73%) of the investigated CD patients had
whelming proportion of the patients was at a state some extraintestinal manifestation and/or intestinal
of activity (77.9%). We divided patients into groups
complications. We observed extraintestinal mani-
according to treatment regimens, Montreal classified
festations in 3/26 patients, 13/26 were with intestinal
localisation of the disease [8], and disease duration
complications, and 3/26 had both (Table 2).
(Table 1).
Table 1. Characteristics of the study subjects presented as number (%)
Characteristics of the patients Number (%)
Young patients (<44 years old) 16 (60%)
Age
Older patients (>44 years old) 10 (40%)
Male 8 (30.8%)
Sex
Female 18 (69.2%)
CDAI < 150 (remission) 6 (23.1%)
Disease activity
CDAI > 150 (activity) 20 (77.9%)
Illeal – L1 2 (8.7%)
Localisation
Colonic – L2 10 (43.5%)
(Montreal classification)
Illeo-colonic – L3 11 (47.8%)
None 7 (28%)
Therapy Immunosuppression 18 (69.2%)
Immunosuppression + Biologic 1 (4%)
< 1 year 7 (28%)
Duration of the disease 1-10 years 15 (60%)
> 10 years 2 (12%)
We collected clinical and laboratory data from medical Extraintestinal manifestations were documented
files of the patients retrospectively. We found the fol- more often in women with long-lasting and active
lowing registered extraintestinal manifestations in pa- disease (without reaching significance, p > 0.05).
tients: arthralgia/arthritis (n = 2), pyoderma gangreno- All three patients with extraintestinal manifestations
18 Ts. Velikova, R. Miladinova, E. Ivanova-Todorova et al.
Table 2. Associations between extraintestinal manifestations, intestinal complications, and some demographic, clinical, laboratory and immunological findings. were positive for FC and 2/3 were positive for
Pos. Neg.
5/13
FL (Table 2).
1/3
1/3
lactoferrin
Fecal Intestinal complications occurred more often
8/13
in patients with the active and long-lasting dis-
2/3
2/3
Neg. ease, however, non-significantly (p > 0.05), also
2/13
in women, in non-immunosuppressive treated
calprotectin
1/3
0 patients, in patients with positive FC and FL
Fecal
11/13
(p > 0.05) (Table 2). The intestinal complica-
Pos.
3/3
2/3
tions were more frequent in women than men
– 55.6% vs. 37.5% respectively, regardless the
IS + B
n=1
1/1
state of activity (66.7% of patients were at a
0
state of remission, and 45.0% of patients were
n = 18
at a state of activity when they had complica-
2/18
9/18
1/18
IS
tions). However, 37.5% of men had none com-
Therapy
plications during the disease.
n=7
*NIS – Non-immunosuppressive therapy; IS – Immunosuppressive therapy; IS + B – Immunosuppressive plus biologic therapy
1/7
4/7
1/7
NI
The overwhelming proportion of patients
(66.7%) with long-lasting disease (up to 10
Duration of the disease
n=2
> 10
2/2
years) had at least one extraintestinal manifes-
0
tation and/or intestinal complication, the most
n = 7 n = 15
Frequencies are shown as number
of these patients receiving non-immunosup-
1-10
3/15
8/15
pressive therapy, too.
(years)
The majority of the CD patients with positive FC
<1
5/7
1/7
0
and FL had intestinal complications. Positive
(Montreal classification)
n = 10 n = 11
markers were associated with the active state
1/11
5/11
2/11
L3
of the disease (according to CDAI).
We also found differences in some laboratory
2/10
7/10
1/10
Localisation
markers depending on the presence of compli-
L2
cations. We observed higher serum level of CRP
n=2
(24.49 mg/l vs. 3.13 mg/l, p = 0.010), slightly
1/2
L1
lowered serum level of hemoglobin (120 g/l vs.
145 g/l, p = 0.044) and about 2-fold lower iron
CDAI > 150
level (7.23 μmol/l vs. 14.0 μmol/l, p = 0.019) in
n = 20
3/20
9/20
2/20
patients with intestinal complications compared
L1 – Illeal form; L2 – Colonic form; L3 – Illeo-colonic form
Disease activity
to patients without complications, respectively
CDAI < 150
(Figure 2 A, B, C).
From the three patients with extraintestinal
n=6
4/6
1/6
manifestations of the disease, one was on non-
0
immunosuppressive therapy and two – on im-
Female
munosuppressive drugs. Four out of thirteen
n = 18
10/18
2/18
2/18
patients with intestinal complications were with-
out immunosuppressive treatment at the time of
n=8
Male
Sex
our study, and nine out of thirteen – on immu-
1/8
3/8
1/8
nosuppressive medications. Three patients with
Intestinal complica-
Intestinal complica-
tions + extraintesti-
nal manifestations
both intestinal and extraintestinal symptoms
simultaneously
manifestations
Extraintestinal
were divided in the three therapeutic groups,
one in every group (non-immunosuppressive,
n = 13
immunosuppressive and immunosuppressive +
n=3
n=3
tions
biologic therapy) (Table 2).
Extraintestinal manifestations and intestinal complications... 19
A. B.
Fig. 2. Some laboratory findings and the presence of complica-
tions in Crohn's disease patients: A Serum C-reactive protein,
C. mg/l; B – Hemoglobin, g/l; C – Serum iron, μmol/l
DISCUSSION and more extensive localization than the disease with
a later start. It was mentioned above that the extrain-
We found that patients with long-lasting (over ten testinal complications might be due to side effects
years) disease have at least one intestinal compli- of therapy or the damaged function of the intestines
cation/extraintestinal manifestation of CD (73% of [12]. We found that our patients on immunosuppres-
the study group). This is not surprising since CD is sive therapy had more intestinal complications than
a chronic progressive disease that begins as an in- extraintestinal ones. The reason for that may lie in
flammation in the mucosa and then progressively the fact that immunosuppressive drugs are neces-
develops over time to a more complex illness with sary when the disease is severe which includes the
stricture and fistula formation [9]. Furthermore, it is presence of complications. Moreover, it is shown that
found that half of the patients with a lasting disease early administration of immunosuppressants was as-
over 20 years suffered from intestinal complications sociated with a decreased risk of surgical interven-
and half of the hospitalized patients needed surgi- tion for structuring and penetrating disease among
cal treatment within ten years from diagnosis [9, 10]. CD patients [13-16]. The use of immunosuppressive
There are accumulated data that over 60% of CD medicaments has increased in the last 20 years, and
patients develop structuring and penetrating compli- it is not accidental. A multivariate Cox – regression
cations, where twenty-year actual rates of inflamma- analysis revealed that the time to initiation of Aza-
tory, structuring and penetrating disease were 12%, thioprine therapy was significantly associated with
18% and 70%, respectively [11]. In our study 13/26 the decade of CD diagnosis (p < 0.001, hazard ratio
(50%) CD patients had intestinal complications which (HR) 2.88-6.53), age at onset (p = 0.008, HR 1.76),
result is in line with the cited resources. disease behavior at diagnosis (p < 0.001, HR 1.76-
It is determined that disease phenotype is changed 2.07), need for systematic steroids (p < 0.001, HR
markedly over time, with nearly 80% of inflammatory 2.71) and the time to intestinal surgery (HR 0.43,
disease ultimately evolving into structuring or pene- [95% CI: 0.28-0.65]) [17]. According to extraintes-
trating pattern of behavior. [12]. Moreover, it is shown tinal manifestations/complications of CD, we ob-
that CD with early onset has more severe behavior served such in about 15% of our cohort of patients.
20 Ts. Velikova, R. Miladinova, E. Ivanova-Todorova et al.
It is thought that some extraintestinal complications REFERENCES
arise simultaneously during the flare of the bowel dis-
1. Friedman S et Blumberg S. Chapter 295 Inflammatory Bowel
ease, and consequently, they can be influenced by Disease. In: Harrison’s Principles of Internal Medicine, 18 edi-
the treatment of the flare. tion, Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson
JL, Loscalzo J, USA, 2012.
The next aspect of our study was to investigate the
2. Ha F et Khalil H. Crohn’s disease: a clinical update. Ther Adv
association between complications and the levels of Gastroenterol, 2015, 8(6), 352–359.
some common laboratory findings in CD patients. 3. Levine JS et Burakoff B. Extraintestinal Manifestations of In-
CRP is documented to be increased during the active flammatory Bowel Disease. Gastroenterology & Hepatology,
2011, 7(4), 235-241.
stage of the disease and may achieve up to and above 4. Bernstein CN, Fried M, Krabshuis JH et al. World Gastroen-
200 mg/l depending on the disease severity and the terology Organization Practice Guidelines for the Diagnosis
individual capacity of producing acute phase proteins. and Management of IBD in 2010. Inflammatory Bowel Dis-
Furthermore, 86% of CD patients with elevated CRP eases, 2010, 16(1), 112-114.
5. Rothfuss KS, Stange EF, Herrlinger KR. Extraintestinal mani-
exhibited inflammation at colonoscopy [18]. In our festations and complications in inflammatory bowel diseases.
study, patients with intestinal complications showed World J Gastroenterol, 2006, 12(30), 4819-31.
about an 8-fold increase in CRP compared to patients 6. Vavricka SR, Schoepfer A, Scharl M et al. Extraintestinal
without intestinal complications (p = 0.010). We also Manifestations of Inflammatory Bowel Disease. Inflamm Bow-
el Dis, 2015, 21, 1982-1992.
found alterations in hemoglobin (p = 0.044) and iron 7. Spekhorst LM, Imhann F, Festen EA on behalf of the Parels-
levels (p = 0.019) according to the presence of the noer Institute (PSI) and the Dutch Initiative on Crohn and Colitis
complications. These tests are laboratory routine for (ICC), et al. Cohort profile: design and first results of the Dutch
IBD Biobank: a prospective, nationwide biobank of patients with
CD patients, including pediatric patients. Other com-
inflammatory bowel disease. BMJ Open, 2017, 7, e016695.
mon laboratory abnormalities in CD patients also en- 8. Satsangi J, Silverberg MS, Vermeire S et al. The Montreal
list anemia, thrombocytosis (> 450 x 109 cells per L), classification of inflammatory bowel disease: controversies,
and elevated ESR (> 20 mm/per hour). At least one consensus, and implications. Gut, 2006, 55, 749-753.
9. Freeman HJ. Natural history and long-term clinical course of
abnormal result was found for 72% of patients with
Crohn’s disease. World J Gastroenterol, 2014, 20(1), 31-36.
IBD, and more than one in about 49% of them [19]. 10. Hellers G. Crohn’s disease in Stockholm county 1955-1974. A
study of epidemiology, results of surgical treatment and long-
We also found an association between high levels
term prognosis. Acta Chir Scand Suppl, 1979, 490, 1-84.
of fecal markers, FC and FL, and the frequency of 11. Cosnes J, Cattan S, Blain A et al. Long-term evolution of dis-
complications in our group of CD patients. These out- ease behavior of Crohn’s disease. Inflamm Bowel Dis, 2002,
comes are in confirmation of our previously published 8(4), 244-50.
12. Fedorak RN. Is it time to re-classify Crohn’s disease? Best
results [20]. Fecal markers are well accepted for diag-
Pract Res Clin Gastroenterol, 2004, 18 Suppl, 99-106.
nosis, prediction of activity and response to therapy. 13. Herfarth HH, Long MD, Kappelman MD. Immunosuppres-
The sensitivity and specificity in identifying the activ- sion for management of Crohn’s disease. The Lancet, 2016,
ity of IBD by colonoscopy are shown to be 70-100% 387(10020), 747-748.
14. Khanna, R, Bressler, B, Levesque, BG et al. Early combined
and 44-100%, respectively [18, 21]. In our study, we immunosuppression for the management of Crohn’s disease
pointed out another utility of FC and FL, namely in (REACT): a cluster randomised controlled trial. Lancet, 2015,
identifying these patients with positive tests that may 386, 1825-1834.
15. D’Haens, G, Baert, F, van Assche, G et al. Early combined
also have intestinal complications.
immunosuppression or conventional management in patients
with newly diagnosed Crohn’s disease: an open randomised
trial. Lancet, 2008, 371, 660–667.
CONCLUSION
16. Colombel, JF, Sandborn, WJ, Reinisch, W et al. Infliximab,
azathioprine, or combination therapy for Crohn’s disease. N
In our study, we obtained data in order to assess the Engl J Med, 2010, 362, 1383-1395.
associations between particular extraintestinal mani- 17. Lakatos PL, Lakatos L, Kiss LS et al. Treatment of extraintes-
tinal manifestations in inflammatory bowel disease. Digestion,
festation and intestinal complications in CD patients
2012, 86 (Suppl 1), 28-35.
with some clinical and laboratory findings (CRP, he- 18. Iskandar HN, Ciorba MA. Biomarkers in inflammatory bowel
moglobin, serum iron), immunological markers (fecal disease: current practices and recent advances. Transl Res,
2012, 159(4), 313-25.
markers – FC and FL), and the administered therapy.
19. Benor S, Russell GH, Silver M et al. Shortcomings of the
These results could be beneficial for gastroenterolo- inflammatory bowel disease Serology 7 panel. Pediatrics,
gists in identifying patients at high risk for the devel- 2010, 125(6), 1230-6.
20. Velikova TV. Investigations of immunological parameters for
opment of complications and in the decision making intestinal inflammation in order to establish new markers for
for more aggressive therapy early after diagnosis. diagnosis and follow-up of inflammatory bowel disease. Dis-
sertation 2014. Medical university of Sofia.
Conflict of interests: None declared 21. Lewis JD. The Utility of Biomarkers in the Diagnosis and Ther-
apy of Inflammatory Bowel Disease. Gastroenterology, 2011,
Acknowledgement: None 140(6), 1817-1826.
Extraintestinal manifestations and intestinal complications... 21
Potrebbero piacerti anche
- Inflammatory Bowel Disease: Translating Basic Science into Clinical PracticeDa EverandInflammatory Bowel Disease: Translating Basic Science into Clinical PracticeNessuna valutazione finora
- A Cross-Sectional Study of The Prevalence ofDocumento9 pagineA Cross-Sectional Study of The Prevalence ofKurnia pralisaNessuna valutazione finora
- Fast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeDa EverandFast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeNessuna valutazione finora
- Small Intestinal Contrast UltrasonographDocumento5 pagineSmall Intestinal Contrast UltrasonographСергей СадовниковNessuna valutazione finora
- Atlas of Inflammatory Bowel DiseasesDa EverandAtlas of Inflammatory Bowel DiseasesWon Ho KimNessuna valutazione finora
- Development of type I gastric carcinoid in chronic atrophic gastritis patientsDocumento9 pagineDevelopment of type I gastric carcinoid in chronic atrophic gastritis patientsAbristaSeptikasariNessuna valutazione finora
- proktitisDocumento13 pagineproktitisRENTI NOVITANessuna valutazione finora
- Gut Dysbiosis and Fecal Calprotectin Predict Response to Immune CheckpointDocumento10 pagineGut Dysbiosis and Fecal Calprotectin Predict Response to Immune CheckpointMartinaNessuna valutazione finora
- Editorial Commentary On The Indian Journal of Gastroenterology May-June 2020Documento3 pagineEditorial Commentary On The Indian Journal of Gastroenterology May-June 2020sivagiri.pNessuna valutazione finora
- Prevalence of Anemia and Iron Deficiency in Romanian Patients With Inflammatory Bowel Disease: A Prospective Multicenter StudyDocumento6 paginePrevalence of Anemia and Iron Deficiency in Romanian Patients With Inflammatory Bowel Disease: A Prospective Multicenter StudyOcha24 TupamahuNessuna valutazione finora
- Journal of Pediatric Surgery: Wendy K. Fujioka, Robert A. CowlesDocumento3 pagineJournal of Pediatric Surgery: Wendy K. Fujioka, Robert A. CowlesVmiguel LcastilloNessuna valutazione finora
- Fecal Calprotectin in IBDDocumento34 pagineFecal Calprotectin in IBDNathania Nadia Budiman100% (1)
- Fecal Calprotectin in IBDDocumento34 pagineFecal Calprotectin in IBDNathania Nadia BudimanNessuna valutazione finora
- Intestinal Tuberculosis: A Diagnostic Challenge: Open Access Case DOI: 10.7759/cureus.13058Documento4 pagineIntestinal Tuberculosis: A Diagnostic Challenge: Open Access Case DOI: 10.7759/cureus.13058ATIKA INDAH SARINessuna valutazione finora
- Jurnal DiagnosisDocumento9 pagineJurnal DiagnosisRenyNessuna valutazione finora
- Neutrophil To Lymphocyte Ratio in Diagnosis of Complicated and Non-Complicated AppendicitisDocumento7 pagineNeutrophil To Lymphocyte Ratio in Diagnosis of Complicated and Non-Complicated AppendicitisHamza AhmedNessuna valutazione finora
- Ajpgi 00190 2011 PDFDocumento8 pagineAjpgi 00190 2011 PDFAnonymous CQSNUSNessuna valutazione finora
- Etiology and Risk Factors of Acute Gastroenteritis in A Taipei Emergency Department: Clinical Features For Bacterial GastroenteritisDocumento8 pagineEtiology and Risk Factors of Acute Gastroenteritis in A Taipei Emergency Department: Clinical Features For Bacterial GastroenteritisakhmadNessuna valutazione finora
- Healthmed 15 1 Damir SecicDocumento6 pagineHealthmed 15 1 Damir SecicEdoHNessuna valutazione finora
- Phagocytic Activity Is Impaired in Type 2 Diabetes Mellitus and Increases After Metabolic ImprovementDocumento6 paginePhagocytic Activity Is Impaired in Type 2 Diabetes Mellitus and Increases After Metabolic ImprovementJenny JennyssimaNessuna valutazione finora
- Endo 1Documento7 pagineEndo 1Soulseller1983Nessuna valutazione finora
- Iihyuyu6756e54tw5w3553w5et6yfug5757 Jgut75Documento6 pagineIihyuyu6756e54tw5w3553w5et6yfug5757 Jgut75RIBNessuna valutazione finora
- Infections After Laparoscopic and Open Cholecystectomy: Ceftriaxone Versus Placebo A Double Blind Randomized Clinical TrialDocumento6 pagineInfections After Laparoscopic and Open Cholecystectomy: Ceftriaxone Versus Placebo A Double Blind Randomized Clinical TrialvivianmtNessuna valutazione finora
- Background: Ormdl3 and of GSDMB Were Significantly Increased in Hrv-Stimulated PBMCSDocumento6 pagineBackground: Ormdl3 and of GSDMB Were Significantly Increased in Hrv-Stimulated PBMCSSav GaNessuna valutazione finora
- FK concentration in celiac diseaseDocumento3 pagineFK concentration in celiac diseaseNejc KovačNessuna valutazione finora
- Heparin-Binding Protein: A Diagnostic Biomarker of Urinary Tract Infection in AdultsDocumento9 pagineHeparin-Binding Protein: A Diagnostic Biomarker of Urinary Tract Infection in AdultsFitria NurulfathNessuna valutazione finora
- 05 Lugovic Mihic PDFDocumento9 pagine05 Lugovic Mihic PDFmarkoperic2014Nessuna valutazione finora
- Hematochezia Case Report on Crohn's Disease in Young MaleDocumento3 pagineHematochezia Case Report on Crohn's Disease in Young Maleseptian_tjayaNessuna valutazione finora
- PCR Detection of AIEC Using CRISPR Genes in IBDDocumento2 paginePCR Detection of AIEC Using CRISPR Genes in IBDNilo BarretoNessuna valutazione finora
- Approach To The Management of Recently Diagnosed IDocumento19 pagineApproach To The Management of Recently Diagnosed IdudinkarulesNessuna valutazione finora
- 1 s2.0 S0140673623009662 MainDocumento14 pagine1 s2.0 S0140673623009662 MainKesia MaldonadoNessuna valutazione finora
- Crohn's diseaseDocumento15 pagineCrohn's diseaseManuel alexanderNessuna valutazione finora
- Van Nella 2010Documento9 pagineVan Nella 2010Anonymous tSdibBveNessuna valutazione finora
- Psychological FactorsDocumento7 paginePsychological FactorsMarcelo Santos SoledadeNessuna valutazione finora
- Acute Pyelonephritis in PregnancyDocumento7 pagineAcute Pyelonephritis in PregnancyKvmLlyNessuna valutazione finora
- Tuberculosis in Patients On DialysisDocumento5 pagineTuberculosis in Patients On Dialysisvasarhely imolaNessuna valutazione finora
- Gastritis and Gastropathy Perspectives From The EndoscopistDocumento4 pagineGastritis and Gastropathy Perspectives From The Endoscopisthenrique.uouNessuna valutazione finora
- Managing IBD: A Case Study on Diagnosis and TreatmentDocumento4 pagineManaging IBD: A Case Study on Diagnosis and TreatmentBejan CorinaNessuna valutazione finora
- Both Fecal Calprotectin and Imuno Test in Children IBDDocumento13 pagineBoth Fecal Calprotectin and Imuno Test in Children IBDdichafrNessuna valutazione finora
- A Cross-Sectional Study On Evaluation of Complete Blood Count-Associated Parameters For The Diagnosis of Acute AppendicitisDocumento6 pagineA Cross-Sectional Study On Evaluation of Complete Blood Count-Associated Parameters For The Diagnosis of Acute AppendicitisJordan SugiartoNessuna valutazione finora
- Clinical, Imaging, and Endoscopic Profile of Patients With Abdominal TuberculosisDocumento6 pagineClinical, Imaging, and Endoscopic Profile of Patients With Abdominal TuberculosisINDRINessuna valutazione finora
- Cal Protect in ADocumento9 pagineCal Protect in AAnonymous Sgiok7Nessuna valutazione finora
- FOXP3 Variants Are Independently Associated With Transforming Growth Factor B1 Plasma Levels in Female Patients With Inflammatory Bowel DiseaseDocumento9 pagineFOXP3 Variants Are Independently Associated With Transforming Growth Factor B1 Plasma Levels in Female Patients With Inflammatory Bowel DiseasePaula KikuchiNessuna valutazione finora
- Primary Biliary CholangitisDocumento12 paginePrimary Biliary CholangitisJuan J. H. AzpeitiaNessuna valutazione finora
- 1Documento11 pagine1Nejc KovačNessuna valutazione finora
- 10.1007@s00384 019 03481 1Documento11 pagine10.1007@s00384 019 03481 1Bernadett FarkasNessuna valutazione finora
- Complications of Pancreatic SurgeryDocumento5 pagineComplications of Pancreatic Surgeryhenok seifeNessuna valutazione finora
- PraktLik 2013 4 8Documento4 paginePraktLik 2013 4 8mustafi28Nessuna valutazione finora
- 6 - Mi - 2021 - Id 6917919 - 8Documento8 pagine6 - Mi - 2021 - Id 6917919 - 8mihail.boldeanuNessuna valutazione finora
- Association Between Proton Pump Inhibitor Use and Spontaneous Bacterial PeritonitisDocumento5 pagineAssociation Between Proton Pump Inhibitor Use and Spontaneous Bacterial PeritonitisMuhammad Rehan AnisNessuna valutazione finora
- Nanoparticle-Mediated-Therapeutic-Approach-for-Ulcerative-Colitis-TreatmentDocumento22 pagineNanoparticle-Mediated-Therapeutic-Approach-for-Ulcerative-Colitis-TreatmentAchudan JiiNessuna valutazione finora
- Crohn 1 EspDocumento8 pagineCrohn 1 EspRomina GonzálezNessuna valutazione finora
- International Journal of Diabetes ResearchDocumento9 pagineInternational Journal of Diabetes Researchfedir.grynchukNessuna valutazione finora
- Tgi Erc 3Documento10 pagineTgi Erc 3Adrian LaimeNessuna valutazione finora
- Outcome and Clinical Characteristics in Pleural Empyema: A Retrospective StudyDocumento7 pagineOutcome and Clinical Characteristics in Pleural Empyema: A Retrospective StudylestarisurabayaNessuna valutazione finora
- Abdominal Tuberculosis in Nepal Medical College Teaching Hospital, KathmanduDocumento4 pagineAbdominal Tuberculosis in Nepal Medical College Teaching Hospital, KathmanduSavitri Maharani BudimanNessuna valutazione finora
- 05 - 203perkembangan Terkini Diagnosis Dan Penatalaksanaan Imflammatory Bowel Disease PDFDocumento6 pagine05 - 203perkembangan Terkini Diagnosis Dan Penatalaksanaan Imflammatory Bowel Disease PDFrisda aulia putriNessuna valutazione finora
- Crohn ReviewDocumento39 pagineCrohn Reviewdrkoral751Nessuna valutazione finora
- Potential Role of Thermography in Evaluation of Disease Activity in Inflammatory Bowel Disease A Case ReportDocumento3 paginePotential Role of Thermography in Evaluation of Disease Activity in Inflammatory Bowel Disease A Case ReportChristian MarchiNessuna valutazione finora
- Systematic Review: Tuberculous Peritonitis - Presenting Features, Diagnostic Strategies and TreatmentDocumento16 pagineSystematic Review: Tuberculous Peritonitis - Presenting Features, Diagnostic Strategies and TreatmenthendraNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Recurrent Hyponatremia As Presenting Manifestation of Pituitary MacroadenomaDocumento4 pagine(03241750 - Acta Medica Bulgarica) Recurrent Hyponatremia As Presenting Manifestation of Pituitary MacroadenomaTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Non-Invasive Diagnostics of Liver FibrosisDocumento7 pagine(03241750 - Acta Medica Bulgarica) Non-Invasive Diagnostics of Liver FibrosisTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Pulse Oximetry and Electric Pulp Test in Intact Teeth and Teeth With Hyperaemia Pulpae PDFDocumento4 pagine(03241750 - Acta Medica Bulgarica) Pulse Oximetry and Electric Pulp Test in Intact Teeth and Teeth With Hyperaemia Pulpae PDFTeodorNessuna valutazione finora
- Clinical and Etiological Structure of Nosocomial Infections in Bulgaria For The Period 2011-2016Documento5 pagineClinical and Etiological Structure of Nosocomial Infections in Bulgaria For The Period 2011-2016TeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Comparative Assessment of uNGAL, uNAG and Cystatin C As Early Biomarkers in Renal Post-Transplant PatientsDocumento8 pagine(03241750 - Acta Medica Bulgarica) Comparative Assessment of uNGAL, uNAG and Cystatin C As Early Biomarkers in Renal Post-Transplant PatientsTeodorNessuna valutazione finora
- Recreation Therapy Reduces Smoking and Symptoms in SchizophreniaDocumento5 pagineRecreation Therapy Reduces Smoking and Symptoms in SchizophreniaTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Cardiovascular Risk Factors in White Collar Workers Under Shift WorkDocumento5 pagine(03241750 - Acta Medica Bulgarica) Cardiovascular Risk Factors in White Collar Workers Under Shift WorkTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) T Helper Cells in The Immunopathogenesis of Systemic Sclerosis - Current TrendsDocumento7 pagine(03241750 - Acta Medica Bulgarica) T Helper Cells in The Immunopathogenesis of Systemic Sclerosis - Current TrendsTeodorNessuna valutazione finora
- Role of miR-15A in Prostate Cancer Cell Proliferation & SignalingDocumento5 pagineRole of miR-15A in Prostate Cancer Cell Proliferation & SignalingTeodorNessuna valutazione finora
- Loss of P16 in Esophageal Adenocarcinoma Detected by Fluorescence in Situ Hybridization and ImmunohistochemistryDocumento6 pagineLoss of P16 in Esophageal Adenocarcinoma Detected by Fluorescence in Situ Hybridization and ImmunohistochemistryTeodorNessuna valutazione finora
- Patterns in The Diagnosis and Treatment of Osteoporosis in Men: A Questionnaire-Based Survey in Central and Eastern European CountriesDocumento8 paginePatterns in The Diagnosis and Treatment of Osteoporosis in Men: A Questionnaire-Based Survey in Central and Eastern European CountriesTeodorNessuna valutazione finora
- [03241750 - Acta Medica Bulgarica] Antiproliferative Properties Against Human Breast, Cervical and Ovarian Cancer Cell Lines, and Antioxidant Capacity of Leaf Aqueous Ethanolic Extract from Cotinus coggygria Scop..pdfDocumento6 pagine[03241750 - Acta Medica Bulgarica] Antiproliferative Properties Against Human Breast, Cervical and Ovarian Cancer Cell Lines, and Antioxidant Capacity of Leaf Aqueous Ethanolic Extract from Cotinus coggygria Scop..pdfTeodorNessuna valutazione finora
- Medial Orbital Epidermoid Cyst: Case ReportDocumento3 pagineMedial Orbital Epidermoid Cyst: Case ReportTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Altruistic Surrogacy - Ethical Issues and Demographic Differences in Public OpinionDocumento5 pagine(03241750 - Acta Medica Bulgarica) Altruistic Surrogacy - Ethical Issues and Demographic Differences in Public OpinionTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Influence of Citric Acid On The Vitality of Stem Cells From Apical PapillaDocumento5 pagine(03241750 - Acta Medica Bulgarica) Influence of Citric Acid On The Vitality of Stem Cells From Apical PapillaTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Comprehensive Analysis of Pain Syndrome in Patients With Mandibular Fractures Treated With Nucleo CMP ForteDocumento6 pagine(03241750 - Acta Medica Bulgarica) Comprehensive Analysis of Pain Syndrome in Patients With Mandibular Fractures Treated With Nucleo CMP ForteTeodorNessuna valutazione finora
- Patients' Satisfaction As A Tool of Dental Setting and Dental Services Assessment in The Dental College of MangaloreDocumento9 paginePatients' Satisfaction As A Tool of Dental Setting and Dental Services Assessment in The Dental College of MangaloreTeodorNessuna valutazione finora
- Basic Mechanisms of Antiepileptic DrugsDocumento7 pagineBasic Mechanisms of Antiepileptic DrugsTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Aesthetic Reconstruction of The Hairline With Local TissueDocumento4 pagine(03241750 - Acta Medica Bulgarica) Aesthetic Reconstruction of The Hairline With Local TissueTeodorNessuna valutazione finora
- Relation of Serum 25 (Oh) - Vitamin D To Fat Mass and Lean Mass, Bone Mineral Content and Body Composition in Adults - A Dxa-Based StudyDocumento7 pagineRelation of Serum 25 (Oh) - Vitamin D To Fat Mass and Lean Mass, Bone Mineral Content and Body Composition in Adults - A Dxa-Based StudyTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) EU Paediatric Investigation Plans (Pips) Might Harm ChildrenDocumento6 pagine(03241750 - Acta Medica Bulgarica) EU Paediatric Investigation Plans (Pips) Might Harm ChildrenTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Influence of Citric Acid On The Vitality of Stem Cells From Apical PapillaDocumento5 pagine(03241750 - Acta Medica Bulgarica) Influence of Citric Acid On The Vitality of Stem Cells From Apical PapillaTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) EU Paediatric Investigation Plans (Pips) Might Harm ChildrenDocumento6 pagine(03241750 - Acta Medica Bulgarica) EU Paediatric Investigation Plans (Pips) Might Harm ChildrenTeodorNessuna valutazione finora
- Patients' Satisfaction As A Tool of Dental Setting and Dental Services Assessment in The Dental College of MangaloreDocumento9 paginePatients' Satisfaction As A Tool of Dental Setting and Dental Services Assessment in The Dental College of MangaloreTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Aesthetic Reconstruction of The Hairline With Local TissueDocumento4 pagine(03241750 - Acta Medica Bulgarica) Aesthetic Reconstruction of The Hairline With Local TissueTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Extensive Proliferation of Cd4+ Lymphocyte by Both Phytohaemagglutinin A and Anti-Cd2 - Cd3 - Cd28 Macsibeads PDFDocumento4 pagine(03241750 - Acta Medica Bulgarica) Extensive Proliferation of Cd4+ Lymphocyte by Both Phytohaemagglutinin A and Anti-Cd2 - Cd3 - Cd28 Macsibeads PDFTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Superluminous Devices Versus Low-Level Laser For Temporomandibular DisordersDocumento5 pagine(03241750 - Acta Medica Bulgarica) Superluminous Devices Versus Low-Level Laser For Temporomandibular DisordersTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Superluminous Devices Versus Low-Level Laser For Temporomandibular DisordersDocumento5 pagine(03241750 - Acta Medica Bulgarica) Superluminous Devices Versus Low-Level Laser For Temporomandibular DisordersTeodorNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Aesthetic Reconstruction of The Hairline With Local TissueDocumento4 pagine(03241750 - Acta Medica Bulgarica) Aesthetic Reconstruction of The Hairline With Local TissueTeodorNessuna valutazione finora
- International Journal of Pharmaceutics: Shuai Qian, Yin Cheong Wong, Zhong ZuoDocumento11 pagineInternational Journal of Pharmaceutics: Shuai Qian, Yin Cheong Wong, Zhong ZuomoazrilNessuna valutazione finora
- Hairy Leukoplakia As An Early OralDocumento4 pagineHairy Leukoplakia As An Early OralJessicaLisaNugrohoNessuna valutazione finora
- Mental Health Term PaperDocumento8 pagineMental Health Term Paperchememartinez29100% (2)
- Case 3 - Sinus HeadacheDocumento6 pagineCase 3 - Sinus HeadacheJohn FightakisNessuna valutazione finora
- Hip Fracture Case Study: 39-Year-Old Male with EpilepsyDocumento9 pagineHip Fracture Case Study: 39-Year-Old Male with EpilepsyufuNessuna valutazione finora
- Hospital Pharmacy ManagementDocumento17 pagineHospital Pharmacy ManagementMuhammad MuhlisNessuna valutazione finora
- A Day in Occupational Therapy Analice BurdDocumento5 pagineA Day in Occupational Therapy Analice Burdapi-518311936Nessuna valutazione finora
- DefinitionDocumento15 pagineDefinitionSimona IonitaNessuna valutazione finora
- Algoritma Penanganan Kejang AkutDocumento1 paginaAlgoritma Penanganan Kejang AkutEwa ClaudiaNessuna valutazione finora
- Navrekar - LWM PPT For Workshop 16 JulyDocumento40 pagineNavrekar - LWM PPT For Workshop 16 JulyQudratullah ShaikNessuna valutazione finora
- Positive PsychologyDocumento4 paginePositive PsychologySpiridon Andrei CristianNessuna valutazione finora
- Topik 1. Pengantar Epidemiologi Penyakit Menular - 2015Documento47 pagineTopik 1. Pengantar Epidemiologi Penyakit Menular - 2015Arini Idza SafarinaNessuna valutazione finora
- Treating Chronic Femur Osteomyelitis and Bone LossDocumento4 pagineTreating Chronic Femur Osteomyelitis and Bone LossmaudiaNessuna valutazione finora
- Drug Study - CiprofloxacinDocumento2 pagineDrug Study - CiprofloxacinryanNessuna valutazione finora
- Unit 10 Fist AidDocumento81 pagineUnit 10 Fist AidillimooniteNessuna valutazione finora
- Cerebrolysin in Patients With Hemorrhagic StrokeDocumento7 pagineCerebrolysin in Patients With Hemorrhagic StrokeZeynep Emirhan ŞenyüzNessuna valutazione finora
- Fluoridation Mind Control of The MassesDocumento14 pagineFluoridation Mind Control of The Massesstevens106Nessuna valutazione finora
- History of Illness and Admissions for ThalassemiaDocumento2 pagineHistory of Illness and Admissions for ThalassemiaReylan GarciaNessuna valutazione finora
- A New Understanding and A Minimalist Approach For.17Documento9 pagineA New Understanding and A Minimalist Approach For.17diego.guerra.smithNessuna valutazione finora
- CDHO Factsheet LupusDocumento3 pagineCDHO Factsheet LupusWayan Sutresna YasaNessuna valutazione finora
- Joining Bupa GlobalDocumento16 pagineJoining Bupa GlobalMayar RagabNessuna valutazione finora
- NRP HandoutDocumento10 pagineNRP HandoutElisabeth F. OjhaNessuna valutazione finora
- Kesling AlineadoresDocumento8 pagineKesling AlineadoresJazmin ArciniegaNessuna valutazione finora
- Buenas ReciproDocumento60 pagineBuenas ReciproChristianOcampodaCruzNessuna valutazione finora
- Generic Name: Acetaminophen Brand Name: Tylenol: ActionDocumento22 pagineGeneric Name: Acetaminophen Brand Name: Tylenol: Actionp_dawg100% (14)
- Comparative Health Information Management 4th Edition Peden Solutions Manual DownloadDocumento15 pagineComparative Health Information Management 4th Edition Peden Solutions Manual DownloadVickie Montejo100% (28)
- Raphex Answers 2010 PDFDocumento15 pagineRaphex Answers 2010 PDFcarlosqueiroz7669100% (4)
- Pocket Tutor Understanding ABGs and Lung Function TestsDocumento170 paginePocket Tutor Understanding ABGs and Lung Function Testsdanelv100% (1)
- Pavlostathi Pharmaceutical Portfolio 1Documento3 paginePavlostathi Pharmaceutical Portfolio 1api-255607190Nessuna valutazione finora
- Introduction To Theories of Neurological RehabilitationDocumento30 pagineIntroduction To Theories of Neurological RehabilitationHibaAli67% (3)







































































![[03241750 - Acta Medica Bulgarica] Antiproliferative Properties Against Human Breast, Cervical and Ovarian Cancer Cell Lines, and Antioxidant Capacity of Leaf Aqueous Ethanolic Extract from Cotinus coggygria Scop..pdf](https://imgv2-1-f.scribdassets.com/img/document/472638617/149x198/0304f4148d/1597599706?v=1)