Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
EU MDR Checklist of Mandatory Documents
Caricato da
Albert MontanoTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
EU MDR Checklist of Mandatory Documents
Caricato da
Albert MontanoCopyright:
Formati disponibili
EU MDR Checklist of
Mandatory Documents
Copyright ©2020 Advisera Expert Solutions Ltd. All rights reserved.
Copyright © 2020 Advisera Expert Solutions Ltd. All rights reserved. 1
Table of Contents
Introduction ............................................................................................................................................3
What are the required EU MDR documents and records?........................................................................4
What is the best structure for EU MDR mandatory documents and records?...........................................6
General Requirements ............................................................................................................................6
Risk Management ...................................................................................................................................7
Clinical Evaluation ...................................................................................................................................9
Clinical Investigation .............................................................................................................................10
Post-Market Surveillance ......................................................................................................................11
Vigilance ...............................................................................................................................................13
Technical File Documentation ...............................................................................................................13
Sample Documentation Templates for ISO 13485 & MDR......................................................................14
Copyright © 2020 Advisera Expert Solutions Ltd. All rights reserved. 2
Introduction
If you are going to sell or distribute medical devices in the European Union, then implementing a Quality
Management System (QMS) will not be enough to meet the legal requirements. Even if you use ISO
13485:2016, the internationally recognized management system requirements for a QMS in the medical
device industry, you will still need to meet the requirements of the European Union Medical Device
Regulation (EU MDR) released in May 2017.
Without knowing exactly what is needed by this new EU regulation, it is easy to find yourself unnecessarily
documenting too much in the belief that this will improve your QMS, or your medical device management,
or you may even think that it is a requirement of the EU MDR regulation. It is true that the EU MDR has
some necessary documentation to be able to distribute medical devices in the European Union, so it is
helpful to know exactly what the regulation requires before you start.
Below is a listing of each of these mandatory pieces of information, and where it is identified in the EU
MDR standard.
Copyright © 2020 Advisera Expert Solutions Ltd. All rights reserved. 3
What are the required EU MDR
documents and records?
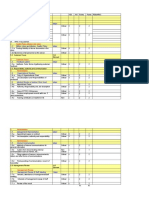
Mandatory Documents and EU MDR Articles, Chapters,
Category
Records and Annexes
EU Declaration of conformity Article 10, Paragraph 8
Quality management system Article 10, Paragraph 9
General
requirements
List of all UDIs Article 27, Paragraph 7
Summary of safety and clinical performance Article 32, Paragraph 1
Risk Management Plan Annex I, Chapter I, Requirement 3
Risk
Risk Management File Annex I, Chapter I, Requirement 3
management
Risk Management Report Annex I, Chapter I, Requirement 3
Clinical Evaluation Plan Annex XIV, Part A, Requirement 1 (a)
Clinical
evaluation Chapter VI, Article 61, Paragraph 12
Clinical Evaluation Report
Annex XIV, Section 4, Paragraph 4
Informed consent Article 63
Application form Annex XV, Chapter II, Paragraph 1
Investigator brochure Annex XV, Chapter II, Paragraph 2,
Article 72
Clinical investigation plan
Clinical Annex XV, Chapter II, Paragraph 3
investigation
Safety & performance statement Annex XV, Chapter II, Paragraph 4
Proof of insurance Annex XV, Chapter II, Paragraph 4
Arrangements description Annex XV, Chapter II, Paragraph 4
Clinical investigation report Annex XV, Chapter III, Paragraph 7
Copyright © 2020 Advisera Expert Solutions Ltd. All rights reserved. 4
Mandatory Documents and EU MDR Articles, Chapters,
Category
Records and Annexes
Post-Market Surveillance Plan Article 84, Annex III
Post-Market Surveillance Report Article 85
Post-Market
Surveillance
Periodic Safety Update Report Article 86
Post-Market Clinical Follow-up Plan Annex XIV, Part B, Paragraph 6
Vigilance Corrective action reports Article 87
Device description and specification Annex II, Paragraph 1
Labels and Instruction of Use Annex II, Paragraph 2
Design information Annex II, Paragraph 3
Technical file
documentation
Manufacturing process and validations Annex II, Paragraph 3
Site identification Annex II, Paragraph 3
Results of different pre/clinical testing Annex II, Paragraph 6
While these are the documents and records that the EU MDR has identified as mandatory, it is important
to note that this does not include any documented information necessary for the proper function of your
Quality Management System. For the listing of information required for an ISO 13485:2016-compliant
QMS, see this white paper: Checklist of Mandatory Documentation Required by ISO 13485:2016.
Copyright © 2020 Advisera Expert Solutions Ltd. All rights reserved. 5
What is the best structure for EU MDR
mandatory documents and records?
The documentation required by the EU MDR regulation needs to be in place before you apply for a CE
mark certification. While there is no perfect solution on how the documentation needs to look, below are
some important elements that you should understand and consider including within your documents
required by the EU MDR.
For more information on how ISO 13485 relates to the CE marking, see: How to use ISO 13485 to get your
devices approved for CE marking.
General Requirements
EU Declaration of Conformity
This is a formal document that officially certifies that your product fulfils the essential requirements
needed to meet the applicable CE directives. This allows you to obtain a CE mark for your medical device.
Quality Management System
EU MDR article 10 states what needs to be included, at a minimum, in a Quality Management System
(QMS) for medical device manufacturers. At the very least, the QMS needs to address aspects in the list
below:
A strategy for complying with regulations,
Safety and performance,
Management responsibility,
Resource management,
Risk management,
Clinical evaluation,
Product realization (planning, design, development, production and service),
Verification of unique device identity assignment,
Post-market surveillance system,
Communication with authorities,
Copyright © 2020 Advisera Expert Solutions Ltd. All rights reserved. 6
Incident reporting,
Corrective and preventive actions (with verification of effectiveness),
Monitoring and measurement, data analysis, and product improvement.
The easiest way to ensure a good QMS that meets all of these requirements is to use the ISO 13485:2016
standard, which is an internationally recognized set of requirements for a medical device manufacturer’s
QMS. It is also the only Quality Management System standard mentioned on the EU harmonized list, a
collection of all the standards that are applicable for the medical device industry published by the EU.
For more information on using ISO 13485 to meet the QMS requirements of the EU MDR, see the article:
How can ISO 13485 help with MDR compliance?
List of all UDIs
The EU MDR regulation includes a unique device identification (UDI) system for medical devices, and the
organization needs to maintain a listing of all the UDIs it manufactures or distributes.
Summary of safety and clinical performance
The organization needs to produce a summary of device performance for each medical device. EU medical
devices must achieve the performance intended by their manufacturers and need to be designed and
manufactured in such a way that, during normal conditions of use, they are suitable for their intended
purpose. Medical devices must be safe and effective and shall not compromise the clinical condition or
the safety of patients, or the safety and health of users or other persons. However, any residual risks that
may be associated with their use must be assessed and weighed against the benefits to the patient. The
reason for this is to determine if these risks constitute acceptable risks and are compatible with a high
level of protection of health and safety.
Risk Management
As a critical consideration of the EU MDR, risk management needs to be done for each medical device and
appropriately documented to demonstrate your abilities to assess and control the risks that are posed by
your medical device throughout the life cycle of the product. As risk is the effect of uncertainty, you must
consider what uncertainty exists that can lead to potential failures so that you can identify the controls
that are needed to mitigate these potential effects.
The purpose of providing the risk process is to describe the process of identification, evaluation, and
addressing of the risks that arise from design and production processes for your medical devices. The
intent of the risk assessment process is to verify that the right materials are being used, to conform to
Copyright © 2020 Advisera Expert Solutions Ltd. All rights reserved. 7
customer specifications, and to ensure that government regulations are being met, before finalizing the
product design. The overall goal is to identify any potential failures that could be caused by the
manufacturing processes, assembly processes, machines, fixtures, and production methods.
The general process for risk assessment includes the following:
Identify foreseeable hazards associated with the device,
Estimate and evaluate the risks,
Eliminate or control the risks,
Estimate the residual risk,
Define the benefit/risk ratio.
One common method of risk assessment is the failure modes and effects analysis (FMEA), which provides
a systematic way to identify and assess the potential failure. It is important that you choose a systematic
method, as this is the best way to ensure that nothing is missed during the risk assessment process.
Risk Management Plan
The Risk Management Plan needs to include all of the information required to assess the risk of a
particular medical device. For the best effect, the plan needs to include the following information:
Identification of the medical device,
Description of the medical device,
Lifecycle stages,
Risk assessment methodology,
Risk acceptance criteria,
Methods used to evaluate residual risk,
Verification activities, and
Methods for post-production information collection.
You want to ensure that the Risk Management Plan includes all details necessary that are unique to the
medical device in question. This allows your assessment to consider the risks that are present from the
raw material used through to the disposal of the medical device at the end of life, and it verifies that you
fully understand the potential impacts that the risks pose.
Risk Management File
The Risk Management File details all of your risk management activity for each of the medical devices you
produce. This file references back to your Risk Management Plan, and needs to include:
The results of risk assessment, including risk acceptance,
The controls you have put in place for the risks,
The risk/benefit analysis of any remaining risks.
Copyright © 2020 Advisera Expert Solutions Ltd. All rights reserved. 8
When compiling your Risk Management File, ensure that you have considered the intended use of your
medical device as well as the safety characteristics you have put in place.
Risk Management Report
The Risk Management Report compiles and summarizes the data obtained in the process of risk
management for formal review. All relevant functions in the organization must review to ensure that the
Risk Management Plan is properly implemented, that the overall residual risk is acceptable, and that
appropriate methods are in place for reviewed production and post-production data. Relevant senior
management needs to know and understand the risk management activities of the medical devices being
produced by the company.
For more information on risk management of medical devices, see: How to use ISO 14971 to manage risks
for medical devices.
Clinical Evaluation
How do you know that your medical device will function as planned? This is the purpose of clinical
evaluation. The purpose of clinical evaluation is to provide a system to demonstrate medical device safety
and effectiveness.
Clinical Evaluation Plan
The Clinical Evaluation Plan must include information concerning the safety or performance of the
medical device that is generated from actual use of the device. The plan needs to include performance
information from at least the following sources:
Clinical investigation(s) of the actual device,
Reports of equivalent devices reported in scientific literature,
Reports published in peer reviewed scientific literature, and
Relevant information from post-market surveillance.
Clinical evaluation must be planned once per year for implantable medical devices and class III medical
devices, and every two years for other medical devices.
Clinical Evaluation Report
After conducting the literature research, the Clinical Evaluation Report is created. The Clinical Evaluation
Report must outline:
Copyright © 2020 Advisera Expert Solutions Ltd. All rights reserved. 9
Description and technology of the medical device,
Intended use of the device,
Claims made about the device’s clinical performance or safety,
Nature and extent of the clinical data,
How the referenced information demonstrates the clinical performance and safety of the device,
Conclusion that the device(s) performs as intended,
Conclusion that the device(s) does not pose any undue safety concerns, and
Justification that any residual risks are acceptable when weighed against the benefits.
Clinical Investigation
Clinical investigation is the systematic evaluation or study using human subject to determine the safety
and performance of a medical device. This is a critical step in the EU MDR, before a device is allowed to
be distributed, which contains several required documents.
Informed consent
Each participant in a clinical investigation must agree to be part of that clinical investigation. This
document must be written, dated, and signed by the participant, and kept as a record of the consent.
Application form
Before starting the clinical investigation, an application form must be written and submitted. The form
includes a short description of the device, details of the investigation, responsibilities within the
investigation, and other important elements about the clinical investigation.
Investigator brochure
The investigator's brochure (IB) must contain all of the relevant clinical and non-clinical information on
the medical device being investigated that is available at the time of application. Any updates to the IB or
other relevant information that are newly available need to be brought to the attention of the
investigators in a timely manner.
Clinical investigation plan
The clinical investigation plan (CIP) is designed to set out the rationale, objectives, design methodology,
monitoring, conduct, record-keeping, and the method of analysis for the clinical investigation. In
particular, it must contain the information as laid down in the EU MDR, or include reference to other
documentation if part of the information is submitted in a separate document.
Copyright © 2020 Advisera Expert Solutions Ltd. All rights reserved. 10
Safety & performance statement
A signed statement by the natural or legal person responsible for the manufacture of the investigational
device that the device in question conforms to the general safety and performance requirements.
Proof of insurance
Proof of insurance coverage or indemnification of subjects in case of injury, pursuant to Article 69 and the
corresponding national law.
Arrangements description
Description of the arrangements to comply with the applicable rules on the protection and confidentiality
of personal data.
Clinical investigation report
The clinical investigation report, signed by the investigator, is intended to contain a critical evaluation of
all the data collected during the clinical investigation, and shall include any negative findings.
Post-Market Surveillance
Post-market surveillance needs to be done for all medical devices that you produce and distribute into
the European Union. Your post-market surveillance system allows your organization to know at all times
what happens to medical devices once they go out of production and are distributed.
Post-Market Surveillance Plan
Your plan for post-market surveillance needs to be inclusive of all information available about your
medical devices as they are in use. This data may include:
Serious field safety incidents,
Trend reporting,
Non-serious incidents,
Customer complaints and feedback, and
Scientific or technical literature.
When creating your plan, consider all the places that you can gather information and data about your
medical device that will help you to track what is happening to identify and address any potential field
usage problems early.
Copyright © 2020 Advisera Expert Solutions Ltd. All rights reserved. 11
Post-Market Surveillance Report
The Post-Market Surveillance Report is used to provide a record of your assessment of the post-market
information gathered about your medical devices. A Post-Market Surveillance Report must be created for
all class I medical devices. The critical information to be contained in your report includes:
A summary of the post-marketing surveillance data,
Conclusions of your assessment of each type of data,
Corrective actions taken to address issues identified.
There is no reason to collect data unless you are going to periodically review that information and gather
corrections and improvements for the medical devices you produce. Any new risks, changes to risks, or
changes to the frequency of occurrences must be noted and new documents for the clinical evaluation
report, risk analysis, or both must be prepared.
Periodic Safety Update Report
For class IIa, class IIb, and class III devices, you need to prepare a Periodic Safety Update Report for each
device or, where relevant, for each category or group of devices. This report must summarize the results
and conclusions of the analyses of the post-market surveillance data from the Post-Market Surveillance
Plan. In addition to the elements listed for the Post-Market Surveillance Report, the Periodic Safety
Update Report also requires the following:
Conclusions from the risk-benefit consideration,
Estimation of population size using the device, and
Usage frequency in the case of reusable devices.
The frequency of preparing the PSUR is every two years for class IIa, and once a year for class IIb and class
III.
Post-Market Clinical Follow-up
Maintaining your post-market surveillance aims to continuously verify the clinical benefits of medical
devices and to identify previously unknown risks by observing and analyzing daily practical usage.
However, if your procedure for post-market surveillance does not provide sufficient data, post-market
clinical follow-up studies regarding the manufacturer may become necessary. When you decide it is
necessary to initiate post-market clinical follow-up, you must prepare a Post-Market Clinical Follow-up
Plan. This plan needs to include:
The design for your study,
Sites to investigate,
Population of the study, number of subjects, and duration,
Criteria for patient inclusion,
Objectives of the study
Copyright © 2020 Advisera Expert Solutions Ltd. All rights reserved. 12
Details on data to be collected,
Criteria to terminate the study early, and
Data analysis methods.
Your post-market clinical follow-up must become a part of your QMS management review.
Vigilance
Corrective action reports
Reporting of serious incidents and field safety corrective actions is a necessity of the EU MDR regulations.
Manufacturers of medical devices must report, to the relevant competent authorities:
Any serious incident involving devices made available on the European Union market. This does
not include any expected side effects that are clearly documented in the product information
and quantified in the technical documentation. These are, however, subject to trend reporting.
Any field safety corrective action in respect of devices made available on the European Union
market. This includes any field safety corrective action undertaken in a third country in relation
to a device that is also legally made available in the EU, if the reason for the field safety corrective
action is not limited to the device being made available in the third country.
Technical File Documentation
Technical files need to be created in order to ensure compliance of the medical device(s) with the MDR.
Technical documentation for a medical device consists of a completed technical file summary and
applicable annexed reports (e.g., sterilization validation reports, biocompatibility report, packaging
validation report, etc.). If certain sections from the Technical File are applicable for the medical device,
but will not be included in the Technical File, justification must be provided.
The Technical File documentation includes:
Copyright © 2020 Advisera Expert Solutions Ltd. All rights reserved. 13
Device description and specification – this needs to include all variants and accessories applicable
to the medical device.
Labels and Instruction of Use – the labeling that will be on the device, and the instructions to use
your medical device, must be included.
Design information – the detailed design of the medical device needs to be included for
appropriate review and approval.
Manufacturing process and validations – the EU must know the processes you will use, and the
proof that these processes are validated to ensure consistently safe and functioning medical
devices.
Site identification – identification of all sites, including suppliers and sub-contractors, where
design and manufacturing activities are performed.
Results of different pre/clinical testing.
Technical files must be updated under the following situations (at a minimum):
Change in supplier of raw material,
Change in dimensions or other characteristics of the medical device,
Change in address of the manufacturer,
Change in relevant standards,
Update in certificates or accreditation of suppliers and/or testing laboratories, and
When new risks for safety of the medical device occur during post-market surveillance.
For more information on the related medical device files requirements of ISO 13485, see: How to meet
ISO 13485:2016 requirements for medical device files.
Sample Documentation Templates for
ISO 13485 & MDR
Here, you can download a free preview of the ISO 13485 & MDR Integrated Documentation Toolkit - in
this free preview, you will be able to see the Table of Contents of each of the above-mentioned
documents, as well as a few sections from each document.
Copyright © 2020 Advisera Expert Solutions Ltd. All rights reserved. 14
Advisera Expert Solutions Ltd Email: support@advisera.com
for electronic business and business consulting U.S. (international): +1 (646) 759 9933
Zavizanska 12, 10000 Zagreb United Kingdom (international): +44 1502 449001
Croatia, European Union Toll-Free (U.S. and Canada): 1-888-553-2256
Toll-Free (United Kingdom): 0800 808 5485
Australia: +61 3 4000 0020
Copyright © 2020 Advisera Expert Solutions Ltd. All rights reserved. 15
Potrebbero piacerti anche
- Post Marketing Surveillance Plan NMRA NewDocumento9 paginePost Marketing Surveillance Plan NMRA NewDeshal RanasingheNessuna valutazione finora
- MDR & Risk ManagementDocumento6 pagineMDR & Risk ManagementGagan Deep SinghNessuna valutazione finora
- ISO 9001 13485 and FDA QSR CompareDocumento71 pagineISO 9001 13485 and FDA QSR CompareNoorm MENessuna valutazione finora
- Post Market Surveillance SOPDocumento8 paginePost Market Surveillance SOPgopinathNessuna valutazione finora
- Medical Devices Harmonized StandardDocumento6 pagineMedical Devices Harmonized Standardhitham shehataNessuna valutazione finora
- FDA Guidance - 510 K ChecklistDocumento3 pagineFDA Guidance - 510 K ChecklistHila Cohen100% (3)
- Index IATF 16949:2016Documento4 pagineIndex IATF 16949:2016Albert MontanoNessuna valutazione finora
- Mini-Course MDRDocumento18 pagineMini-Course MDRAbid HussainNessuna valutazione finora
- Post Market Surveillance: Global Guidance For Adverse Event Reporting For Medical DevicesDocumento37 paginePost Market Surveillance: Global Guidance For Adverse Event Reporting For Medical DevicesSachin KumarNessuna valutazione finora
- Gap Analysis MDR 2017.745Documento157 pagineGap Analysis MDR 2017.745sbalNessuna valutazione finora
- MDR Readiness Checklist: Prepared by Cite Medical SolutionsDocumento37 pagineMDR Readiness Checklist: Prepared by Cite Medical SolutionsBeal100% (1)
- Bsi Smart Support Post Market SurveillanceDocumento10 pagineBsi Smart Support Post Market SurveillanceMauro CostaNessuna valutazione finora
- Risk Management For Medical Devices Webinar SlidesDocumento35 pagineRisk Management For Medical Devices Webinar Slideschit cat100% (1)
- EU New MDR White Paper EMERGODocumento28 pagineEU New MDR White Paper EMERGOFrancisco100% (2)
- Responsible - Sourcing - MONDELEZ (SAMPLE)Documento26 pagineResponsible - Sourcing - MONDELEZ (SAMPLE)Albert MontanoNessuna valutazione finora
- FDA Vs EU MDR Technical Documentation Matrix ENDocumento10 pagineFDA Vs EU MDR Technical Documentation Matrix ENAri CleciusNessuna valutazione finora
- Ebook - Ultimate Guide To EU MDR GSPRDocumento38 pagineEbook - Ultimate Guide To EU MDR GSPRMahmoud DomourNessuna valutazione finora
- 1.PMS Plan Template Anexo V. Plantilla Plan de Seguimiento Poscomercialización (PMSP)Documento18 pagine1.PMS Plan Template Anexo V. Plantilla Plan de Seguimiento Poscomercialización (PMSP)delal karaku100% (2)
- 7.post Market Clinical Follow Up ReportDocumento2 pagine7.post Market Clinical Follow Up Reportdelal karaku100% (1)
- Technical File of Wound Drainage SystemDocumento39 pagineTechnical File of Wound Drainage SystemDrMufaddal Rampurwala100% (3)
- ISO 14971 Risk Management Guidance Document Rev 1 (2016!06!27)Documento7 pagineISO 14971 Risk Management Guidance Document Rev 1 (2016!06!27)bhatnagar29Nessuna valutazione finora
- Usability Engineering FileDocumento8 pagineUsability Engineering Fileeko1980100% (1)
- Medical Device Regulations in The Main Global Markets - Whitepaper - Oct 2012Documento24 pagineMedical Device Regulations in The Main Global Markets - Whitepaper - Oct 2012RoxanaBurla100% (1)
- Bsi MD Risk Management For Medical Devices Webinar 131119 Uk enDocumento29 pagineBsi MD Risk Management For Medical Devices Webinar 131119 Uk enrakesh marwahNessuna valutazione finora
- Customer Lifetime Value ModelsDocumento50 pagineCustomer Lifetime Value Modelspraveen_bpgcNessuna valutazione finora
- Medical Device Software DevelopmentDocumento26 pagineMedical Device Software DevelopmentAdalnei GomideNessuna valutazione finora
- Psur Guidance CDocumento16 paginePsur Guidance CGhada JlassiNessuna valutazione finora
- Comparison Chart of ISO 13485 and FDA QSR RequirementsDocumento4 pagineComparison Chart of ISO 13485 and FDA QSR RequirementsjvivoloNessuna valutazione finora
- PMS SopDocumento8 paginePMS Sopstevekent40% (5)
- Clinical Evaluation Report-Surgical InstrumentsDocumento8 pagineClinical Evaluation Report-Surgical InstrumentsAlejandro Landinez0% (1)
- WP.026 Leveraging Post Market Surveillance and Post Market Clinical Follow Up Data - A01Documento20 pagineWP.026 Leveraging Post Market Surveillance and Post Market Clinical Follow Up Data - A01Neelakandan R100% (1)
- Europe IVD Regulatory ProcessDocumento1 paginaEurope IVD Regulatory Processpsp710Nessuna valutazione finora
- Managing Medical Devices within a Regulatory FrameworkDa EverandManaging Medical Devices within a Regulatory FrameworkBeth Ann FiedlerValutazione: 5 su 5 stelle5/5 (1)
- Sample SoP For Vigilance SystemDocumento4 pagineSample SoP For Vigilance Systemsogic100% (5)
- IEC 62304 Software Development: A Real-World PerspectiveDocumento42 pagineIEC 62304 Software Development: A Real-World Perspectivejchav004ucrNessuna valutazione finora
- Bsci Audit Sample ReportDocumento14 pagineBsci Audit Sample ReportAlbert Montano100% (1)
- Guidelines For Risk Management in Medical Electrical EquipDocumento123 pagineGuidelines For Risk Management in Medical Electrical Equipmhenig0% (1)
- An Introductory Guide To The Medical Device Regulation (MDR) and The in Vitro Diagnostic Medical Device Regulation (IVDR)Documento27 pagineAn Introductory Guide To The Medical Device Regulation (MDR) and The in Vitro Diagnostic Medical Device Regulation (IVDR)Shivaraj K Yadav100% (1)
- EU MDR Post-Market Surveillance: Best Practices For Medical Device Regulatory, Compliance & Quality SpecialistsDocumento50 pagineEU MDR Post-Market Surveillance: Best Practices For Medical Device Regulatory, Compliance & Quality SpecialistsMauro Costa100% (1)
- EU US PostMarket Surveillance Whitepaper PDFDocumento7 pagineEU US PostMarket Surveillance Whitepaper PDFLakshmana Perumal RamarajNessuna valutazione finora
- The Survival Guide to EU Medical Device RegulationsDa EverandThe Survival Guide to EU Medical Device RegulationsValutazione: 5 su 5 stelle5/5 (1)
- MDR SP 4-19 - First Experience With The Implementation of MDRDocumento40 pagineMDR SP 4-19 - First Experience With The Implementation of MDRMauro Costa100% (1)
- GDP For Medical DevicesDocumento33 pagineGDP For Medical DevicesВладимир Бургић50% (2)
- EMERGO ISO 14971 Webinar Sept 2017Documento40 pagineEMERGO ISO 14971 Webinar Sept 2017CeangoNessuna valutazione finora
- 8-Step Transition Process From The MDD To The MDR: White PaperDocumento11 pagine8-Step Transition Process From The MDD To The MDR: White Papervlsi_forever100% (1)
- Med-Info: Biological EvaluationDocumento4 pagineMed-Info: Biological EvaluationRand OmNessuna valutazione finora
- 03 REVAMIL Clinical Evaluation ReportDocumento40 pagine03 REVAMIL Clinical Evaluation Reportamit545100% (1)
- ISO 14971 RISK Management For Medical Devices: The Definitive GuideDocumento41 pagineISO 14971 RISK Management For Medical Devices: The Definitive GuideOrielson Cruz100% (2)
- 06 MDCG 2020-6 Guidance On Sufficient Clinical Evidence For Legacy DevicesDocumento22 pagine06 MDCG 2020-6 Guidance On Sufficient Clinical Evidence For Legacy DevicesSantiago IbañezNessuna valutazione finora
- TUV SUD - Technical Files and Design Dossiers Non Active Medical DevicesDocumento15 pagineTUV SUD - Technical Files and Design Dossiers Non Active Medical DevicesRoxanaBurla0% (1)
- SMTP en DNS Servers - BenlDocumento10 pagineSMTP en DNS Servers - BenlgeensrNessuna valutazione finora
- Checklist - of - Requirements - For - New - Gasoline - Stations (DOE) PDFDocumento2 pagineChecklist - of - Requirements - For - New - Gasoline - Stations (DOE) PDFAlbert Montano100% (1)
- SAP SD Blue PrintDocumento361 pagineSAP SD Blue Printamjadonline67% (3)
- Technical FilesDocumento15 pagineTechnical Fileshitham shehataNessuna valutazione finora
- Usability Best PracticesDocumento37 pagineUsability Best PracticesMashal PkNessuna valutazione finora
- Software Testing For Medical DevicesDocumento8 pagineSoftware Testing For Medical Devicesandrewd420% (1)
- ODFS Clinical EvaluationDocumento138 pagineODFS Clinical EvaluationValerica Zarnescu Creanga100% (2)
- The Definitive Guide To ISO 14971 Risk Management For Medical DevicesDocumento31 pagineThe Definitive Guide To ISO 14971 Risk Management For Medical DevicesMichael FadjarNessuna valutazione finora
- Applying Human Factors and Usability Engineering To Optimize Medical Device DesignDocumento37 pagineApplying Human Factors and Usability Engineering To Optimize Medical Device Designmclade01100% (1)
- FI - CA Config DocumentDocumento101 pagineFI - CA Config DocumentKarthik Selvaraj80% (5)
- (C) Qadvis: Iec 62304 and Iec 82304-1 - How To Make Them WorkDocumento33 pagine(C) Qadvis: Iec 62304 and Iec 82304-1 - How To Make Them Workkritz48Nessuna valutazione finora
- European Medical Device Usability RequirementsDocumento3 pagineEuropean Medical Device Usability RequirementsHong-Nam KimNessuna valutazione finora
- Medical Devices and IVDs: Fit for the new EU-Regulations: Your complete seminar for projekt, study and jobDa EverandMedical Devices and IVDs: Fit for the new EU-Regulations: Your complete seminar for projekt, study and jobNessuna valutazione finora
- MDR Namsa SlidesDocumento44 pagineMDR Namsa SlidesswarhiliNessuna valutazione finora
- Comparing Medical Device Law & Reg of Japan, US, and EUDocumento5 pagineComparing Medical Device Law & Reg of Japan, US, and EUpavan_baggaNessuna valutazione finora
- Iso 14971Documento1 paginaIso 14971Vivek Goud0% (1)
- Sedex Sample (Avon)Documento8 pagineSedex Sample (Avon)Albert MontanoNessuna valutazione finora
- 785E1 - C-Checklist ISO 50001 - 2011Documento10 pagine785E1 - C-Checklist ISO 50001 - 2011Albert MontanoNessuna valutazione finora
- Sedex Tool Kit Sample ChinaDocumento16 pagineSedex Tool Kit Sample ChinaAlbert MontanoNessuna valutazione finora
- DOH-QSS Checklist (Clinic)Documento14 pagineDOH-QSS Checklist (Clinic)Albert MontanoNessuna valutazione finora
- DOH-QSS Checklist (Clinic)Documento14 pagineDOH-QSS Checklist (Clinic)Albert MontanoNessuna valutazione finora
- Structure of Dairy IndustryDocumento10 pagineStructure of Dairy IndustryEmmanuel Asane OtooNessuna valutazione finora
- Tata Consultancy Services: Selling CertaintyDocumento10 pagineTata Consultancy Services: Selling CertaintyPraharsh ShahNessuna valutazione finora
- Standard NDADocumento1 paginaStandard NDAThiwakkaran MuaganNessuna valutazione finora
- Competitor Analysis v1Documento182 pagineCompetitor Analysis v1ShamsNessuna valutazione finora
- Presentation of Data of DmciDocumento16 paginePresentation of Data of DmciEricka Hazel OsorioNessuna valutazione finora
- Internship ReportDocumento27 pagineInternship ReportVijaya Lakshmi80% (5)
- Install Erp60sr3IDES Win OraDocumento29 pagineInstall Erp60sr3IDES Win OraMaxikrrogNessuna valutazione finora
- Sales & Distribution of Pepsico: Summer Internship Project Report OnDocumento54 pagineSales & Distribution of Pepsico: Summer Internship Project Report Onsubhankar daNessuna valutazione finora
- JPT Group v. Steven Madden - ComplaintDocumento20 pagineJPT Group v. Steven Madden - ComplaintSarah BursteinNessuna valutazione finora
- Practice Exercise 1.6Documento3 paginePractice Exercise 1.6leshz zynNessuna valutazione finora
- Mills Estruturas E Serviços de Engenharia S.A.: Minutes of The Board of Directors' Meeting Held On April 14, 2010Documento1 paginaMills Estruturas E Serviços de Engenharia S.A.: Minutes of The Board of Directors' Meeting Held On April 14, 2010MillsRINessuna valutazione finora
- Case 2:09-cv-00665-LKK - DAD Document 179-1 Filed 11/23/09 Page 75 of 147Documento73 pagineCase 2:09-cv-00665-LKK - DAD Document 179-1 Filed 11/23/09 Page 75 of 147Henry So E DiarkoNessuna valutazione finora
- Ashish FinalDocumento146 pagineAshish Finallokesh_045Nessuna valutazione finora
- Executive SummaryDocumento16 pagineExecutive Summaryanuj1820% (1)
- Balance-Sheet and Cash-Flow Planning With SAP NetWeaver BIDocumento6 pagineBalance-Sheet and Cash-Flow Planning With SAP NetWeaver BIManikandanNessuna valutazione finora
- 3rd Annual State of AppExchange Partners Report 2020 PDFDocumento28 pagine3rd Annual State of AppExchange Partners Report 2020 PDFGaurav KheterpalNessuna valutazione finora
- 8 4 Audit TemplateDocumento3 pagine8 4 Audit Templatedinaforproject2557Nessuna valutazione finora
- Transit Manual SupplementDocumento136 pagineTransit Manual SupplementMarian MocanuNessuna valutazione finora
- Riyaz Main Project PDFDocumento71 pagineRiyaz Main Project PDFATS PROJECT DEPARTMENTNessuna valutazione finora
- DS19 1006 001 Datacard Firmware Cross Reference v2Documento1 paginaDS19 1006 001 Datacard Firmware Cross Reference v2alvaro valeraNessuna valutazione finora
- 5.1 Swot AnalysisDocumento6 pagine5.1 Swot Analysisasyraf arasNessuna valutazione finora
- Adca PDFDocumento3 pagineAdca PDFASHISH KUMARNessuna valutazione finora
- Tally Accounting Package: Unit - 1Documento19 pagineTally Accounting Package: Unit - 1Harshal BorgaonNessuna valutazione finora
- ALL SubjectsDocumento11 pagineALL SubjectsMJ YaconNessuna valutazione finora
- Services Marketing Chapter 7Documento20 pagineServices Marketing Chapter 7raja89Nessuna valutazione finora
- Blade Logic Atrium Integration Guide Vs 8.1Documento88 pagineBlade Logic Atrium Integration Guide Vs 8.1Russell RoseNessuna valutazione finora