Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Combined Hormonal Contraception
Caricato da
Juan Pablo RealDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Combined Hormonal Contraception
Caricato da
Juan Pablo RealCopyright:
Formati disponibili
CONTRACEPTION
Combined hormonal What’s new ?
contraception • Transdermal, vaginal and injectable methods
containing both estrogen and progestogen are now
Anna Glasier available
• Amenorrhoea is becoming more acceptable among
women using hormonal contraception
• WHO medical eligibility criteria are replacing the
concept of relative and absolute contraindications to
use of all contraceptive methods
The combined oral contraceptive pill (COCP) was introduced in
the early 1960s and is currently used by more than 60 million • The risk of cervical cancer is increased in women using
women worldwide. In the UK, 25% of women using a revers- the combined pill, particularly if they have persistent
ible method of contraception take an oral contraceptive pill. The human papillomavirus infection
COCP is popular because of its efficacy, ease of use and additional
health benefits beyond those of contraception. In recent years,
new delivery systems for combined hormonal contraception have Progestogens used in currently available COCPs are divided into
become available. The contraceptive patch Evra was marketed in four groups:
the UK in 2004. The combined contraceptive vaginal ring Nuvar- • first-generation progestogens (norethindrone)
ing is available in much of Europe and in the USA. There are no • second-generation norgestrel derivatives (e.g. levonorgestrel)
plans to market the combined injection Lunelle in the UK. The • third-generation progestogens (e.g. gestodene, desogestrel,
mechanism of action and efficacy of these relatively new delivery norgestimate)
systems are similar to those of the COCP. Few data are available • the newest progestogen, drospirenone (has anti-androgenic and
on the long-term risks, but it is sensible to assume that they too antimineralocorticoid activity; the term ‘fourth generation’ is
are no different from the COCP. avoided by the manufacturer).
Different progestogens differ in potency and thus contraceptive
effectiveness is achieved at different doses. At equivalent contra-
Available preparations
ceptive efficacies, the progestogens are said to have slightly differ-
Combined hormonal contraceptives contain both estrogen (usually ent side-effects, but the evidence is unconvincing, except possibly
ethinylestradiol) and a progestogen (a synthetic compound that for side-effects clearly associated with relative differences in andro-
behaves like progesterone). genicity (e.g. acne). The anti-androgenic properties of drospirenone
may make it particularly beneficial for acne and hirsutism.
Combined oral contraceptive pill
Estrogen: the dose of estrogen used in the COCP is 15–50 µg; most Formulations: classically, the COCP is taken for 21 days followed by
women now use so-called ‘low-dose pills’ containing 30–35 µg. a 7-day break (the pill-free interval, PFI), when withdrawal bleed-
Low-dose pills are potentially safer, because the cardiovascular ing usually occurs. Combined pills are available in monophasic
risks of the COCP result mainly from estrogen. However, the lower preparations (in which every pill in the packet contains the same
the dose of estrogen, the higher the risk of poor cycle control, dose of steroids), and biphasic and triphasic preparations (in which
breakthrough bleeding and, at least theoretically, pregnancy if the dose of both estrogen and progestogen changes once or twice
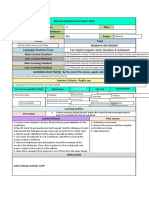
compliance is poor. This is reflected in the new rules for missed over the 21-day period). Biphasic and triphasic pills were intro-
pills, which distinguish between pills containing less than 30 µg of duced to reduce the total dose of progestogens, and in the belief
ethinylestradiol and those containing 30 µg or more (Figure 1). that a regimen that mimicked the normal cycle would produce
better cycle control. However, there is no evidence for better cycle
control, and some women find such preparations confusing, par-
ticularly when they want to take two packets of pills consecutively
to postpone menstruation. In an attempt to improve compliance,
everyday preparations are used widely in the USA and Australia.
Anna Glasier is Honorary Professor in the Department of Obstetrics and These regimens involve the taking of inactive tablets, rather than
Gynaecology at the University of Edinburgh, UK and in the Department 7 days without pills.
of Public Health and Policy at the University of London School of Hygiene In the USA, an 84-day packet of pills (followed by a 7-day PFI)
and Tropical Medicine, London, and Lead Clinician for Sexual Health in is marketed as Seasonale. Only four withdrawal bleeds per year is
NHS Lothian. She qualified from the University of Bristol, and trained in a pattern increasingly popular with many European women and
obstetrics and gynaecology, specializing in reproductive medicine. Her can be achieved simply by taking 21-day packets of pills consecu-
research interests are contraception, including emergency contraception, tively.
and reproductive health care. Conflicts of interest: none declared. One manufacturer is now evaluating a combined pill which is
taken continuously with no breaks and therefore with no with-
This article has been reproduced from: Medicine 2006; 34(1): 1–5. drawal bleeds.
WOMEN’S HEALTH MEDICINE 3:6 257 © 2006 Elsevier Ltd
CONTRACEPTION
Guidance for women who have missed pills
If one or two 30–35 µg ethinylestradiol pills If three or more 30–35 µg ethinylestradiol pills have been
have been missed at any time missed at any time
or or
One 20 µg ethinylestradiol pill is missed Two or more 20 µg ethinylestradiol pills are missed
She should take the most recent missed pill as soon as She should take the most recent missed pill as soon as she remembers
she remembers She should continue taking the remaining pills daily at her usual time 1
She should continue taking the remaining pills daily at She should be advised to use condoms or abstain from sex until she has
her usual time1 taken pills for 7 consecutive days
She does not require additional contraceptive
protection In addition (because extending the pill-free interval is risky)
She does not require emergency contraception
If pills are missed in week 1 If pills are missed in week 3
(days 1–7) (because the pill-free (days 15–21) (to avoid extending
interval has been extended) the pill-free interval)
Emergency contraception should She should finish the pills in her
be considered if she had current pack and start a new
unprotected sex in the pill-free pack on the next day, thereby
interval or in week 1 omitting the pill-free interval
1Depending on when she remembers her missed pill, she may take two pills on the same day (one at the moment of remembering and the other at the regular time)
or even at the same time
Figure 1
Combined injectable contraceptive
Combined contraceptive patch A once-monthly injectable contraceptive containing 25 mg of
Only one contraceptive patch is currently available. Evra is medroxyprogesterone acetate and 5 mg of estradiol cypionate
20 cm2 in area and delivers 20 µg of ethinylestradiol and 150 µg (Lunelle) is available in some parts of the world, but not in the
of norelgestromin (17-deacetylnorgestimate) per day. Each patch UK. Injections are administered intramuscularly every 28 days.
lasts 7 days; three patches are used consecutively, followed by a Bleeding episodes occur 18–22 days after injection when estrogen
placebo patch or patch-free interval in week four, when withdrawal concentrations decline to 50 pg/ml or less. About 70% of women
bleeding occurs. Contraceptive protection lasts for up to 10 days, experience one bleeding episode per month.
allowing for errors in changing the patch. In a randomized trial
comparing the patch with a COCP, there was no significant differ-
Mode of action
ence in effectiveness; overall pearl indices were 1.24/100 women-
years for the patch and 2.18/100 women-years for the COCP. The Combined hormonal contraception acts mainly by inhibiting
efficacy may be reduced in heavier women. Bleeding patterns and ovulation. The estrogen component inhibits secretion of pituitary
side-effects are similar to those associated with the COCP. follicle-stimulating hormone, thereby suppressing the develop-
ment of ovarian follicles; progestogen inhibits the development
Combined contraceptive vaginal ring of the luteinizing hormone surge. Other mechanisms of action of
Nuvaring releases 15 µg of ethinylestradiol and 120 µg of combined hormonal contraception are shown in Table 1.
etonorgestrel per day and is now licensed in much of Europe. The In some women, the 7-day hormone-free interval is long enough
ring is made of soft ethylene-vinyl-acetate co-polymer and meas- to allow follicle growth; on the last day of the PFI, 25% of women
ures 54 mm in diameter. It is designed to last for 3 weeks; a 7-day using the COCP exhibit ultrasonographical evidence of follicles of
ring-free interval is associated with bleeding patterns that appear 10 mm in diameter. If the PFI is extended beyond 7 days, these
superior to those associated with the COCP. In all other respects, follicles continue to grow and, despite restarting the pill, ovula-
including efficacy, the ring is no different from the COCP. tion may occur. The same is likely to be true of the hormone-free
WOMEN’S HEALTH MEDICINE 3:6 258 © 2006 Elsevier Ltd
CONTRACEPTION
Mechanisms of action of combined oral WHO medical eligibility criteria category 3 and 4
contraceptives conditions for combined oral contraception
• Inhibition of ovulation Category 3 conditions
• Changes in cervical mucus that interfere with sperm transport • Breast-feeding 6 weeks to 6 months post-partum
• Tubal motility may be altered • Before 3 weeks after childbirth
• Atrophy of endometrium • Smoking < 15 cigarettes/day and > 35 years of age
• Uterine receptivity essential for successful implantation may • Adequate controlled hypertension
be impaired • Blood pressure > 140/90 mm Hg, < 160/100 mm Hg
• Severe hyperlipidaemia
• Non-migraine with aura and > 35 years of age
Table 1 • Previous breast cancer – 5 years without recurrence
• Current or medically treated gallbladder disease
interval following patch or ring use. In women who appear to have • Past combined oral contraception-related cholestasis
conceived as a result of a genuine COCP failure (rather than as a • Mild cirrhosis
result of an error in pill-taking) and who wish to continue using
the COCP after the pregnancy is over, the PFI can be shortened to Category 3/4 conditions
4 or 5 days to ensure suppression of follicular development. Some • Multiple risk factors for cardiovascular disease
brands of low-dose COCP have a shorter PFI as standard. • Diabetes with retinopathy, nephropathy, neuropathy or other
Because the risks of the COCP are mainly from estrogen, manu- vascular disease, or of > 20 years’ duration
facturers have steadily reduced the dose. In recognition of the risk
of compromising contraceptive efficacy, one formulation (Mircette, Category 4 conditions
currently available only in the USA) comprises 21 days of 20 µg • Breast-feeding before 6 weeks post-partum
ethinylestradiol in combination with desogestrel, but includes five • Smoking > 15 cigarettes/day and > 35 years of age
daily doses of 10 µg ethinylestradiol alone during the ‘pill-free’ • Blood pressure > 160/100 mm Hg
week to maintain suppression of follicle growth. • Hypertension with vascular disease
• History of or current deep vein thrombosis
• Major surgery with prolonged immobilization
Efficacy
• History of or current myocardial infarction
When used correctly, combined hormonal contraceptives are • History of stroke
almost 100% effective. The failure rate during ‘perfect’ use is • Complicated valvular heart disease
0.1%. In practice, methods of contraception that make demands • Migraine with aura
of users have a higher failure rate, because mistakes are made • Current breast cancer
during ‘typical use’. Because of errors in pill-taking, the failure • Severe cirrhosis
rate associated with typical use of the COCP is about 8%. There • Liver tumour
is evidence that use of the patch or ring may be less demanding,
so typical-use failure rates (not yet available for either method)
Table 2
may be lower. This should be a clear advantage for the combined
injectable contraceptive.
Combined hormonal contraception has an effect on almost every
system in the body. Most side-effects are minor; mood change,
Contraindications
weight gain or fluid retention, nausea and vomiting, headache,
Absolute contraindications (WHOMEC category 4 conditions) loss of libido, mastalgia, breast enlargement and greasy skin are
to the COCP are listed in Figure 3. Relative contraindications common complaints that also occur in the absence of contraceptive
(WHOMEC category 3 conditions) include serious or multiple risk use. Many improve or disappear within 3–6 months of starting
factors for arterial disease, including hypertension, family history, the method, but side-effects often lead to discontinuation. Some
diabetes mellitus, smoking, age over 35 years, obesity and migraine side-effects may be alleviated by changing to a different delivery
(Table 2). The Faculty of Family Planning & Reproductive Health- system. The patch, for example, should be associated with less
care adapted the WHOMEC for use in the UK. The categories are nausea. In women who use the COCP, the dose of estrogen or type
essentially the same but a few additional conditions have been of progestogen can be altered by changing to a different brand
added – the UKMEC is available on www.ffprhc.org.uk. of pill, and it is worth trying this if time alone does not solve
Women with hyperprolactinaemia who want to avoid pregnancy the problem. Chloasma is much less common and is definitely
should be advised to use progestogen-only contraception, because related to steroid hormones. It can also occur with progestogen-
estrogen stimulates lactotrophs (prolactin-secreting cells in the only methods.
pituitary gland), thereby increasing the prolactin concentration. Serious side-effects involve mainly the cardiovascular system.
Combined hormonal contraception affects both the venous (venous
thromboembolism (VTE)) and the arterial (myocardial infarction
Risks and side-effects
(MI), cerebrovascular accident) circulation. Although the aetiology
WOMEN’S HEALTH MEDICINE 3:6 259 © 2006 Elsevier Ltd
CONTRACEPTION
and epidemiology of venous and arterial disease differ, in both hypertension, but the relationship between MI and COCP use is
cases the increased risk appears to be related to an increased controversial in women with no other risk factors.
thrombotic tendency. Contraceptive steroids are metabolized by • A recent meta-analysis of 23 studies concluded that the risk
the liver and affect the metabolism of carbohydrates, lipids, plasma of MI was increased in current COCP users vs never-users (odds
proteins, amino acids, vitamins and clotting factors. Changes in ratio 2.48, 95% CI 1.91–3.22).
clotting factors create a tendency to hypercoagulability, which is • The risk in past-users was not increased, nor was the risk in
partly balanced by an increase in fibrinolysis. The adverse effect women using third-generation COCPs or COCPs containing 20 µg
on clotting is related to the dose of estrogen; low-dose pills are of ethinylestradiol.
associated with a reduced risk compared with pills containing • The risk of MI was increased in women using second-generation
50 µg of ethinylestradiol. COCPs, and in smokers (by nine times) and women with
In a recent analysis of 25 years’ follow-up of 46,000 women hypertension (tenfold).
who took part in the Royal College of General Practitioners (RCGP) The risk of stroke attributable to COCP use is small. The rela-
Oral Contraceptive Study (comparing 517,519 years of COCP use tive risk of haemorrhagic stroke is not increased in women under
with 335,998 years of never-use), the risk of death from all causes 35 years of age and is only slightly increased in older women. The
was similar in ever-users and never-users of oral contraception. risk of ischaemic stroke is slightly increased (relative risk 1.5) and
In current or recent users, however, there was an increase in the is also slightly higher in the over-35s. Smoking and hypertension
relative risk of death from two conditions – cervical cancer (rela- increase the risk of stroke by tenfold and threefold, respectively.
tive risk 2.5) and haemorrhagic stroke (1.9).
Migraine
Venous disease Women who have migraine with aura may be at increased risk
The COCP is associated with a threefold increase in the relative of stroke. Migraine with aura is a category 4 condition for use of
risk of VTE. Risk is unaffected by age, smoking and duration of combined hormonal contraception.
COCP use, but is higher in obese women (body mass index, BMI
> 30 kg/m2) and in women with a history of pregnancy-induced Breast cancer
hypertension. Opinion varies acrimoniously on the validity and Overviews of the risks of COCPs are dominated by breast cancer.
interpretation of several studies published in the mid-1990s show- Data are difficult to interpret because COCP formulations and
ing differing VTE risk with different types of progestogen. On patterns of reproduction (particularly age at first pregnancy) have
balance, most experts agree that the difference in risk of VTE is changed with time. A meta-analysis of 54 studies involving more
real but small. COCPs containing the third-generation progestogen than 53,000 women with breast cancer and 100,000 controls con-
gestodene or desogestrel carry about a twofold increased risk of cluded that use of the COCP was associated with a small increased
VTE compared with pills containing levonorgestrel. Although the risk of breast cancer that persisted for 10 years after stopping the
reason for this difference is unclear, it is known that oral contra- COCP. The relative risk was 1.24 in current users, 1.16 1–4 years
ceptive use reduces the efficiency with which activated protein C after stopping and 1.07 5–9 years after stopping. After 10 years,
down-regulates in vitro thrombin formation, and this phenomenon the relative risk was the same as that in never-users. Although the
appears to be more pronounced in women using a COCP contain- relative risk was higher in women who started taking the COCP
ing desogestrel rather than levonorgestrel. at a young age (because breast cancer is uncommon in this age
The absolute risk of VTE in COCP users is very low group), there was little added effect from the duration of use, or
(15/10,000 woman-years) and considerably less than that during the dose or type of hormone. Women who had ever used the COCP
pregnancy (60/10,000 woman-years). The risk returns to normal were significantly less likely (relative risk 0.88) than never-users
within 3 months of stopping the COCP. The Committee on Safety of to develop cancer that spread beyond the breast, even if they had
Medicines warns that women should be informed of the increased stopped the COCP more than 10 years earlier. In the 25-year RCGP
risk of VTE when third-generation pills are prescribed. It is possible follow-up study, ever-users were not more likely to die from breast
that COCPs containing anti-androgens may be associated with an cancer than never-users.
even higher risk of VTE. This certainly appears to be the case for A large case-control study from the USA involving 8000 women
Dianette, a combination of ethinylestradiol and cyproterone acetate (published after the 1996 meta-analysis) suggested no increase in
licensed for treatment of hirsutism and severe acne that acts as breast cancer risk (relative risk 1.0, 95% CI 0.8–1.3); however, the
a combined oral contraceptive. There is no reason to believe that upper limit of the confidence intervals is in line with the findings of
the risk of VTE is any different with other routes of administration the much larger meta-analysis. Again, the association with breast
of combined hormonal contraception (patch, ring or injectable). cancer is probably independent of the route of administration of
Women with inherited thrombophilias (e.g. factor V Leiden) the contraceptive method.
are at increased risk of VTE, and a family history of VTE is an The relationship between the COCP and breast cancer is dif-
indication for testing for various thrombophilias. Population-level ficult to explain, because the risk appears to increase soon after
screening is considered neither practical nor economical. exposure, does not increase with duration of use, and returns to
normal after 10 years of no exposure. It has been suggested that
Arterial disease starting the COCP may accelerate the appearance of breast cancer in
Arterial disease in COCP users is much more serious than venous susceptible women. It is also possible that tumours are diagnosed
disease, though the absolute risk of MI and stroke in young earlier in women who are using the COCP, though it is difficult
women is tiny. There is widespread agreement that the risk of MI to explain why a tendency to earlier diagnosis would persist for
is increased in women who take the COCP and smoke or have years after stopping. A biological effect of combined hormonal
WOMEN’S HEALTH MEDICINE 3:6 260 © 2006 Elsevier Ltd
CONTRACEPTION
contraception has not been excluded. Information: women should be carefully instructed how to use
the COCP and what to do when pills are forgotten (Figure 1).
Cervical cancer Many women choose (or are ‘advised’) to take a break from using
Data on the risk of cervical cancer in COCP users are difficult to the COCP for a few months. Although most cardiovascular risks
interpret, because barrier methods confer some protection and the decrease when the pill is stopped, they recur as soon as it is started
aetiology of cervical cancer is connected with sexual activity. In again, and unplanned pregnancies commonly occur during such
the 25-year follow-up study, the relative risk of dying from cervical breaks. Most women who stop the COCP regain normal fertility
cancer was 2.5 in ever-users. A meta-analysis of ten case-control within 3 months. Secondary, so-called ‘post-pill’ amenorrhoea is
studies showed an increased risk of cervical cancer in women almost always the result of abnormalities that were present before
with persistent human papillomavirus infection using hormonal the COCP was started (e.g. polycystic ovary syndrome), but which
contraception. The relative risk was 2.8 after 5 years of use of the were masked by regular artificial withdrawal bleeds.
COCP and 4.0 after 10 years. There is no evidence for any adverse effect on the fetus as a
result of previous COCP use. When conception occurs during COCP
Liver cancer use, the risk of teratogenesis is low or non-existent.
Benign hepatic adenoma is an uncommon consequence of COCP
use. In countries where hepatocellular carcinoma is rare, this
disease is occasionally associated with the COCP. In populations
where liver cancer is common (e.g. the Far East), short-term use of
COCPs does not affect the incidence of hepatocellular carcinoma;
data on long-term use are scarce.
Practical prescribing
History: a full history, including family history, should be taken to
exclude risk factors that might contraindicate combined hormonal FURTHER READING
contraception use or indicate further investigations. Beral V, Hermon C, Kay C et al. Mortality associated with oral
contraceptive use: 25 year follow up of a cohort of 46,000
Examination: blood pressure should be measured, and it may women from Royal College of General Practitioners’ Oral
be helpful to record baseline weight. BMI of more than 30 kg/m2 Contraception Study. BMJ 1999; 318: 96–100.
is considered a relative contraindication to combined hormo- Etminan M, Takkouche B, Isorna F C et al. Risk of ischaemic stroke
nal contraception, and BMI more than 40 kg/m2 is an absolute in people with migraine: systematic review and meta-analysis
contraindication because of the increased risk of CVD. of observational studies. BMJ 2005; 330: 63–5.
Pelvic examination is not routinely indicated at the first (or any) Faculty of Family Planning and Reproductive Health Care Clinical
visit unless gynaecological pathology is suspected. Women do not Effectiveness Unit. FFPRHC guidance (October 2003) first
like pelvic examinations and some, particularly the young, may be prescription of combined oral contraception. J Fam Plann
deterred from starting or continuing with the COCP if examination Reprod Health Care 2003; 29: 209–23.
is seen as a prerequisite. Breast examination is also unnecessary Khader Y S, Rice J, John L et al. Oral contraceptive use and risk of
unless the woman has symptoms of breast disease. Cervical smears myocardial infarction: a meta-analysis. Contraception 2003;
should be taken in accordance with national policy. 68: 11–17.
Marchbanks P A, McDonald J A, Wilson H G et al. Oral
Choice of preparation: new users should usually start with a contraceptives and the risk of breast cancer. N Eng J Med
low-dose (30–35 µg) pill containing a second-generation pro- 2002; 346: 2025–32.
gestogen. If breakthrough bleeding occurs and persists beyond O’Brien P A. The third generation oral contraceptive controversy.
the first 3 months, and a gynaecological cause is excluded, a BMJ 1999; 319: 795–6.
COCP containing a higher dose of estrogen or a different type of Rosing J, Middeldorp S, Curvers J et al. Low-dose oral
progestogen may be tried. contraceptives and acquired resistance to activated protein C:
Women taking long-term enzyme-inducing drugs (e.g. some a randomised cross-over study. Lancet 1999; 354: 2036–40.
anticonvulsants) should use a preparation containing 50 µg of Skegg D C G. Third generation oral contraceptives. BMJ 2000; 321:
estrogen, to ensure best efficacy (this may necessitate taking 190–1.
two pills each day, one containing 30 µg and the other 20 µg of WHO. Improving access to quality care in family planning. Selected
ethinylestradiol, if a 50 µg preparation is not available). practice recommendations for contraceptive use. Geneva:
The patch should be considered if nausea or vomiting is a per- WHO, 2005.
sistent side-effect of pill use or if there is a potential problem with WHO. Improving access to quality care in family planning. Medical
oral absorption. The patch may also be useful in women who want eligibility criteria for contraceptive use. Geneva: WHO, 2004.
to use combined hormonal contraception, but who have difficulty WHO. Cardiovascular disease and steroid hormone contraception.
remembering to take a pill every day. Report of a scientific group. WHO Tech Rep Ser 1998; 877.
Progestogen-only contraception may be considered in women WHO. Oral contraceptives and neoplasia. WHO Tech Rep Ser 1992;
with contraindications to the COCP. 817.
WOMEN’S HEALTH MEDICINE 3:6 261 © 2006 Elsevier Ltd
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Nielsen Esports Playbook For Brands 2019Documento28 pagineNielsen Esports Playbook For Brands 2019Jean-Louis ManzonNessuna valutazione finora
- Agreement of PurchaseDocumento8 pagineAgreement of PurchaseAdv. Govind S. TehareNessuna valutazione finora
- Café Management System Full and Final ReportDocumento18 pagineCafé Management System Full and Final ReportMuhammad Xalman Xhaw100% (3)
- 5 L&D Challenges in 2024Documento7 pagine5 L&D Challenges in 2024vishuNessuna valutazione finora
- Official Memo: From: To: CCDocumento4 pagineOfficial Memo: From: To: CCrobiNessuna valutazione finora
- Makalah Soal Soal UtbkDocumento15 pagineMakalah Soal Soal UtbkAndidwiyuniarti100% (1)
- Sjögren's SyndromeDocumento18 pagineSjögren's Syndromezakaria dbanNessuna valutazione finora
- The Relationship Between Law and MoralityDocumento12 pagineThe Relationship Between Law and MoralityAnthony JosephNessuna valutazione finora
- 11-03-25 PRESS RELEASE: The Riddle of Citizens United V Federal Election Commission... The Missing February 22, 2010 Judgment...Documento2 pagine11-03-25 PRESS RELEASE: The Riddle of Citizens United V Federal Election Commission... The Missing February 22, 2010 Judgment...Human Rights Alert - NGO (RA)Nessuna valutazione finora
- PH Scale: Rules of PH ValueDocumento6 paginePH Scale: Rules of PH Valuemadhurirathi111Nessuna valutazione finora
- UNIT VI. Gunpowder and ExplosivesDocumento6 pagineUNIT VI. Gunpowder and ExplosivesMariz Althea Jem BrionesNessuna valutazione finora
- Fort St. John 108 Street & Alaska Highway IntersectionDocumento86 pagineFort St. John 108 Street & Alaska Highway IntersectionAlaskaHighwayNewsNessuna valutazione finora
- FCI - GST - Manual On Returns and PaymentsDocumento30 pagineFCI - GST - Manual On Returns and PaymentsAmber ChaturvediNessuna valutazione finora
- 3RD Last RPHDocumento5 pagine3RD Last RPHAdil Mohamad KadriNessuna valutazione finora
- R. K. NarayanDocumento9 pagineR. K. NarayanCutypie Dipali SinghNessuna valutazione finora
- Eva Karene Romero (Auth.) - Film and Democracy in Paraguay-Palgrave Macmillan (2016)Documento178 pagineEva Karene Romero (Auth.) - Film and Democracy in Paraguay-Palgrave Macmillan (2016)Gabriel O'HaraNessuna valutazione finora
- Goldilocks and The Three BearsDocumento2 pagineGoldilocks and The Three Bearsstepanus delpiNessuna valutazione finora
- Wa0006.Documento8 pagineWa0006.Poonm ChoudharyNessuna valutazione finora
- Duck 2019Documento52 pagineDuck 2019Adrian BAGAYANNessuna valutazione finora
- PFASDocumento8 paginePFAS王子瑜Nessuna valutazione finora
- Apply Study and Learning SkillsDocumento58 pagineApply Study and Learning SkillsSelf-DeveloperNessuna valutazione finora
- OatDocumento46 pagineOatHari BabuNessuna valutazione finora
- Persian NamesDocumento27 paginePersian NamescekrikNessuna valutazione finora
- Snap Fasteners For Clothes-Snap Fasteners For Clothes Manufacturers, Suppliers and Exporters On Alibaba - ComapparelDocumento7 pagineSnap Fasteners For Clothes-Snap Fasteners For Clothes Manufacturers, Suppliers and Exporters On Alibaba - ComapparelLucky ParasharNessuna valutazione finora
- Lae 3333 2 Week Lesson PlanDocumento37 pagineLae 3333 2 Week Lesson Planapi-242598382Nessuna valutazione finora
- 215 Final Exam Formula SheetDocumento2 pagine215 Final Exam Formula SheetH.C. Z.Nessuna valutazione finora
- STD 4 Maths Half Yearly Revision Ws - 3 Visualising 3D ShapesDocumento8 pagineSTD 4 Maths Half Yearly Revision Ws - 3 Visualising 3D ShapessagarNessuna valutazione finora
- RS485 Soil 7in1 Sensor ES SOIL 7 in 1 Instruction ManualDocumento15 pagineRS485 Soil 7in1 Sensor ES SOIL 7 in 1 Instruction ManualĐoàn NguyễnNessuna valutazione finora
- Campus Design: School of Architecture & Planning at PondicherryDocumento9 pagineCampus Design: School of Architecture & Planning at Pondicherrynadhir sulaimanNessuna valutazione finora
- Introduction To Communication Systems: James Flynn Sharlene KatzDocumento15 pagineIntroduction To Communication Systems: James Flynn Sharlene KatzAnisari MeiNessuna valutazione finora