Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Assignment For OB Assessment
Caricato da
Erika Anne Mercado CadawanTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Assignment For OB Assessment
Caricato da
Erika Anne Mercado CadawanCopyright:
Formati disponibili
Centro Escolar University – Malolos
Nursing Department
HEALTH ASSESSMENT LECTURE
Name: Erika Anne M. Cadawan Date: April 17, 2020
Section: BSN-STEM1A Score: ___________________
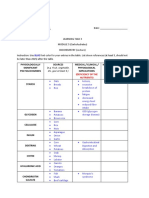
ASSESSMENT FOR PREGNANT WOMEN
A. Identify the GTPAL (10 points; 2 points each)
1. A 20 year old female is currently 8 weeks pregnant. She had a miscarriage at 12 weeks
gestation two years ago. She has no living children. What is her GTPAL?
- Her GTPAL is: G=2, T=0, P=0, A=1, L=0
2. A 26 year old female is currently 26 weeks pregnant. She had a miscarriage at 10 weeks
gestation five years ago. She has a three year old who was born at 39 weeks. What is her
GTPAL?
- Her GTPAL is: G=3, T=1, P=0, A=1, L=1
3. A 29 year old female is currently 9 weeks pregnant. She has no living children. Two years
ago she had 2 miscarriages at 10 and 12 weeks gestation. What is her GTPAL?
- Her GTPAL is: G=3, T=0, P=0, A=2, L=0
4. A 30 year old female is 25 weeks pregnant with twins. She has 5 living children. Four of the
5 children were born at 39 weeks gestation and one child was born at 27 weeks gestation.
Two years ago she had a miscarriage at 10 weeks gestation. What is her GTPAL?
- Her GTPAL is: G=7, T=4, P=1, A=1, L=5
5. A 35 year old female is currently pregnant with twins. She has 10 year old triplets who were
born at 32 weeks gestation, and a 16 year old who was born at 41 week gestation. Twelve
years ago she had a miscarriage at 19 weeks gestation. What is her GTPAL?
- Her GTPAL is: G=4, T=1, P=1, A=1, L=4
B. Compute for EDC or EDD using Naegele’s Rule. Show your computation. (10 points;
2 points each)
1. LMP: January 20, 2016
- ECD or EDD: January 20, 2016 – 3 months = October 20, 2015
October 20, 2015 + 7 days = October 27, 2015
October 27, 2015 + 1 year = October 27, 2016
2. LMP: March 14, 2016
- ECD or EDD: March 14, 2016 – 3 months = December 14, 2015
December 14, 2015 + 7 days = December 21, 2015
December 21, 2015 + 1 year = December 21, 2016
3. LMP: August 28, 2016
- ECD or EDD: August 28, 2016 – 3 months = May 28, 2016
May 28, 2016 + 7 days = June 4, 2016
June 4, 2016 + 1 year = June 4, 2017
4. LMP: August 15, 2016
- ECD or EDD: August 15, 2016 – 3 months = May 15, 2016
May 15, 2016 + 7 days = May 22, 2016
May 22, 2016 + 1 year = May 22, 2017
5. LMP: January 30, 2016
- ECD or EDD: January 30, 2016 – 3 months = October 30, 2015
October 30, 2015 + 7 days = November 6, 2015
November 6, 2015 + 1 year = November 6, 2016
C. Differentiate the 3, presumptive, probable and positive signs of pregnancy (10
points)
Presumptive signs of maternity refers to signs and symptoms that may
match pregnancy signs and symptoms, however could after all be caused by
something else. One of these presumptive signs of maternity is that the
absence of a period. Whereas this can be a sign of maternity, missing a
period may result from things corresponding to illness or stress during a
woman's life, thus this can be not a reliable sign of suspected maternity.
Probable signs of pregnancy are signs that indicate pregnancy the majority of
the time. However, there's still the possibility they'll be false or caused by one
thing other than pregnancy, like presumptive signs. A positive pregnancy test
could be a probable sign of pregnancy. However, in some instances,
pregnancy tests will offer off false positives for a variety of reasons, similar to
the urine being too diluted once the test is taken, or the directions not being
followed fully.
Positive signs of pregnancy are signs that can't, beneath any circumstances,
be mistaken for alternative conditions, and are proof that pregnancy has
occurred. These signs embody fetal heart sounds by a Doppler within the
doctor's office, ultrasound detection of the fetus, or the movement of the fetus
felt by a doctor. These signs can't be brought on by the other condition.
There's no interpretation or "faking" the sound of a fetal heartbeat, or seeing a
fetus on an ultrasound screen.
D. Identify signs and symptoms of pregnancy according to: Presumptive, probable and
positive (20 points)
Presumptive Probable Positive
Amenorrhea (no Increased frequency Fetal Heart
period) of urination Sounds
Nausea — with or Soft cervix Ultrasound
without vomiting Abdominal Scanning of the
Breast bloating/enlargement Fetus
enlargement and Mild uterine Palpation of the
tenderness cramping/discomfort Entire Fetus
Fatigue without bleeding Palpation of Fetal
Poor sleep Increased skin
Back pain pigmentation in the Movement
Constipation face, stomach, X-ray
Food cravings and and/or areola Actual Delivery of
aversions Tender and swollen An Infant
Mood changes or breasts/chest
"mood swings" Nausea and Food
Heartburn Aversions
Nasal congestion Mood changes
Shortness of
breath
Lightheadedness
Elevated basal
body temperature
(BBT)
Spider veins
Reddening of the
palms
E. Discuss the different lie and presentation of the fetus.(10 points)
Longitudinal lie: the fetus lies horizontally across the birth canal and
presents shoulder first. A cesarean delivery is done, unless the fetus is the
second in a set of twins. In such a case, the fetus may be turned to be
delivered through the vagina.
Oblique lie: in an oblique lie there is an anatomical relationship in which the
fetal axis crosses the maternal axis at an angle other than a right angle. i.e.
no fetal presenting part is palpable in the lower pole and the head or the
breech is in an iliac fossa.
Unstable lie: Refers to the frequent changing of fetal lie and presentation in
late pregnancy. (usually refers to pregnancies > 37 weeks)1. Lie. Refers to
the relationship between the longitudinal axis of the fetus and that of its
mother, which may be longitudinal, transverse or oblique.
Transverse lie: is a sideways position. The baby has his head to one of his
mother's sides and the bottom across her abdomen at her other side.
Anterior position: This position means the fetus's head is down in the pelvis,
facing the woman's back. The fetus's back will be facing the woman's belly.
This position means the fetus's head can be tucked in, allowing the top of it to
press down on the cervix, which encourages it to open during labor.
Posterior position: When a baby is head-down but facing your abdomen,
she's said to be in the occiput posterior (OP) position – or posterior position,
for short. The term refers to the fact that the back of your baby's skull (the
occipital bone) is in the back (or posterior) of your pelvis.
Shoulder presentation: The fetus is positioned normally (head first) for
delivery, but the fetus’s shoulder becomes lodged against the woman’s pubic
bone as the fetus’s head comes out. Consequently, the head is pulled back
tightly against the vaginal opening. The baby cannot breathe because the
chest and umbilical cord are compressed by the birth canal. As a result,
oxygen levels in the baby’s blood decrease.
Face presentation: The neck arches back so that the face presents first.
Brow presentation: The neck is moderately arched so that the brow
presents first.
Occiput or cephalic posterior position: Sometimes the baby is positioned
head down as it should be, but other times it is facing the mother's abdomen.
With the head in this position, the baby is looking at the ceiling. You may hear
this position nicknamed sunny-side-up.
Breech position: The breech position is when the fetus remains with the
head up instead of down in the woman’s pelvis. There are different types of
breech position, including:
o Frank breech: When the baby's legs are folded flat up against his head
and his bottom is closest to the birth canal.
o Complete breech: When both of the baby's knees are bent and his feet
and bottom are closest to the birth canal.
o Footling breech: Sometimes, one or both of the baby's feet are pointed
down toward the birth canal. This increases the chances of the umbilical
cord slithering down into the mouth of the womb, cutting off blood supply
to the baby.
Potrebbero piacerti anche
- Walang Kwentang NotesDocumento107 pagineWalang Kwentang NotesAnonymousTargetNessuna valutazione finora
- Signs of PregnancyDocumento4 pagineSigns of Pregnancybreanna zyreNessuna valutazione finora
- OB Exam 2Documento14 pagineOB Exam 2Katie GermanNessuna valutazione finora
- LaborDocumento45 pagineLaborDakayu Amin LugitNessuna valutazione finora
- Common Terms and Abbreviations Used in ObstetricsDocumento4 pagineCommon Terms and Abbreviations Used in ObstetricsRemedios NillusguinNessuna valutazione finora
- PPP NCM 107Documento2 paginePPP NCM 107Anna YepisNessuna valutazione finora
- NCM107 Lecture II LAB-RLE Signs of Pregnancy'Documento21 pagineNCM107 Lecture II LAB-RLE Signs of Pregnancy'Mary Ann G. CorsanesNessuna valutazione finora
- Primary ObstetricsDocumento62 paginePrimary ObstetricsGill Bulanan - PeñaNessuna valutazione finora
- Labor and Delivery: IMS Murah-ManoeDocumento48 pagineLabor and Delivery: IMS Murah-ManoeNurul Husna RashidNessuna valutazione finora
- Leopold's ManueDocumento13 pagineLeopold's ManueFatima Diane S. MondejarNessuna valutazione finora
- Assessment of Fetal WellbeingDocumento177 pagineAssessment of Fetal Wellbeingvrutipatel100% (1)
- Ante Natal Care: by Naveen Sharma J.N - Medical College Belgaum, IndiaDocumento37 pagineAnte Natal Care: by Naveen Sharma J.N - Medical College Belgaum, IndiaNaveen SharmaNessuna valutazione finora
- Labor and DeliveryDocumento7 pagineLabor and Deliveryplethoraldork100% (20)
- Abnormal Delivery - Zhahrullail ShahidDocumento12 pagineAbnormal Delivery - Zhahrullail ShahidBadrul MunirNessuna valutazione finora
- Exam 1 Midterm Study Guide OBDocumento23 pagineExam 1 Midterm Study Guide OBAnnissaLarnardNessuna valutazione finora
- Pregnancy A To ZDocumento42 paginePregnancy A To Zhemant8487Nessuna valutazione finora
- Mannikin Notes Precourse MaterialDocumento42 pagineMannikin Notes Precourse MaterialSyed Shahmeer RazaNessuna valutazione finora
- MCN Lec MidtermDocumento14 pagineMCN Lec Midtermnaomie manaliliNessuna valutazione finora
- Obstetrics NotesDocumento14 pagineObstetrics Notescheruiyotdenis2002Nessuna valutazione finora
- Common Terms and Abbreviations Used in ObstetricsDocumento4 pagineCommon Terms and Abbreviations Used in ObstetricsJerome MansibangNessuna valutazione finora
- Finals MCNDocumento48 pagineFinals MCNAlvin Josh CalingayanNessuna valutazione finora
- Notes For The New Exam.: DR Swamy PLAB CoursesDocumento44 pagineNotes For The New Exam.: DR Swamy PLAB CoursesBeaulah100% (1)
- AntepartalDocumento43 pagineAntepartalxing414Nessuna valutazione finora
- Maternal Newborn NursingDocumento11 pagineMaternal Newborn NursingRaf Luis100% (4)
- The Diagnosis of PregnancyDocumento76 pagineThe Diagnosis of PregnancyCnette S. LumboNessuna valutazione finora
- Leopolds ManueverDocumento9 pagineLeopolds ManueverJonah R. Merano100% (3)
- Gynecological ProceduresDocumento17 pagineGynecological Proceduresjeelani saima100% (5)
- OB Final Exam Study GuideDocumento14 pagineOB Final Exam Study GuideMarissa SolanoNessuna valutazione finora
- Maternal Child NursingDocumento14 pagineMaternal Child NursingTina TalmadgeNessuna valutazione finora
- Infant Care and Feeding PPT 2021 Part 1Documento313 pagineInfant Care and Feeding PPT 2021 Part 1Matt Andrey100% (2)
- C (Also Called,, or Ú Is The Culmination of A HumanDocumento26 pagineC (Also Called,, or Ú Is The Culmination of A HumanEdherlynNessuna valutazione finora
- Basic Terminologies of ObstetricsDocumento40 pagineBasic Terminologies of ObstetricsBindu PhilipNessuna valutazione finora
- Third TrimesterDocumento13 pagineThird Trimestersingh1582Nessuna valutazione finora
- OB Study GuideDocumento43 pagineOB Study Guidelilchibaby3161100% (1)
- Diagnosis of PregnancyDocumento53 pagineDiagnosis of PregnancyAdrija MukherjeeNessuna valutazione finora
- Pregnancy PowerPointDocumento59 paginePregnancy PowerPointHervis FantiniNessuna valutazione finora
- Case 2 Guide Questions ChangedDocumento9 pagineCase 2 Guide Questions ChangedReyzel PahunaoNessuna valutazione finora
- Lecture Notes Signs and Symptoms of PregnancyDocumento8 pagineLecture Notes Signs and Symptoms of PregnancyMiguel LigasNessuna valutazione finora
- Basic Gynaecological and Obstetrical TerminologyDocumento67 pagineBasic Gynaecological and Obstetrical TerminologyCricket Highlights Full HD100% (1)
- LaborDocumento69 pagineLaborzamurd76Nessuna valutazione finora
- OB - GYN (1) - Alaa SalmanDocumento6 pagineOB - GYN (1) - Alaa Salmanmotasem.med120Nessuna valutazione finora
- Ob Exam Study Guide The Bible 001 49pgsDocumento50 pagineOb Exam Study Guide The Bible 001 49pgsVin Lorenzo CampbellNessuna valutazione finora
- It's Not Just a Heavy Period; The Miscarriage HandbookDa EverandIt's Not Just a Heavy Period; The Miscarriage HandbookValutazione: 2 su 5 stelle2/5 (1)
- Conception & Pregnancy - Ovulation, Fertilization, and MoreDocumento17 pagineConception & Pregnancy - Ovulation, Fertilization, and MoreZakaria FarahNessuna valutazione finora
- MidtermsDocumento12 pagineMidtermsMarga PalomaNessuna valutazione finora
- Normal Labour and Birth UohDocumento148 pagineNormal Labour and Birth UohCaamir Dek HaybeNessuna valutazione finora
- Normal Labour and Birth Uoh 2023Documento159 pagineNormal Labour and Birth Uoh 2023Caamir Dek HaybeNessuna valutazione finora
- Pregnancy PowerPointDocumento32 paginePregnancy PowerPointJireh NoelleNessuna valutazione finora
- Antenatal Care 1Documento8 pagineAntenatal Care 1jibson2354Nessuna valutazione finora
- Maternal and Fetal Assessment During LaborDocumento66 pagineMaternal and Fetal Assessment During LaborHazelynne Mamucud100% (2)
- DR Power PointDocumento30 pagineDR Power PointlezahazelNessuna valutazione finora
- Ante, Intra, PostpartumDocumento64 pagineAnte, Intra, PostpartumJaypee Fabros EdraNessuna valutazione finora
- DR Case Presentation FinalDocumento35 pagineDR Case Presentation FinalLord Allen B. GomezNessuna valutazione finora
- What Goes On Inside Pregnant Mommy's Tummy? Big Ideas Explained Simply - Science Book for Elementary School | Children's Science Education booksDa EverandWhat Goes On Inside Pregnant Mommy's Tummy? Big Ideas Explained Simply - Science Book for Elementary School | Children's Science Education booksNessuna valutazione finora
- Goals of Prenatal CareDocumento16 pagineGoals of Prenatal CareLhea Marie Trinidad100% (1)
- Labor and DeliveryDocumento128 pagineLabor and Deliveryalimk528950% (2)
- Pregnancy: Signs and Symptoms Detection of Abnormalities Diagnosis, Physio Changes, CareDocumento67 paginePregnancy: Signs and Symptoms Detection of Abnormalities Diagnosis, Physio Changes, CareJovim Cervantes LanaNessuna valutazione finora
- Makalah Partus NormalDocumento29 pagineMakalah Partus NormalAnna AndanyNessuna valutazione finora
- Daddy Happiness Ahoy: All About Pregnancy, Birth, Breastfeeding, Hospital Bag, Baby Equipment and Baby Sleep! (Pregnancy Guide For Expectant Parents)Da EverandDaddy Happiness Ahoy: All About Pregnancy, Birth, Breastfeeding, Hospital Bag, Baby Equipment and Baby Sleep! (Pregnancy Guide For Expectant Parents)Valutazione: 5 su 5 stelle5/5 (3)
- Line Width: Key FactorsDocumento22 pagineLine Width: Key FactorsErika Anne Mercado CadawanNessuna valutazione finora
- The Postpartal Family Maybelle B. AnimasDocumento43 pagineThe Postpartal Family Maybelle B. AnimasErika Anne Mercado CadawanNessuna valutazione finora
- List of RequirementsDocumento1 paginaList of RequirementsErika Anne Mercado CadawanNessuna valutazione finora
- Hospital DietsDocumento451 pagineHospital DietsErika Anne Mercado Cadawan100% (1)
- Ob ToolDocumento5 pagineOb ToolErika Anne Mercado CadawanNessuna valutazione finora
- NCM 107 Case Scenario-Hospital: Rina Lagadon Is A Part-Time Model Who Has Come To Your Clinic TodayDocumento3 pagineNCM 107 Case Scenario-Hospital: Rina Lagadon Is A Part-Time Model Who Has Come To Your Clinic TodayErika Anne Mercado CadawanNessuna valutazione finora
- Cardio Vascular DiseaseDocumento4 pagineCardio Vascular DiseaseErika Anne Mercado CadawanNessuna valutazione finora
- Hyperemesis Gravidarum: Mrs - Jagadeesw Ari.j M.SC NursingDocumento28 pagineHyperemesis Gravidarum: Mrs - Jagadeesw Ari.j M.SC NursingErika Anne Mercado CadawanNessuna valutazione finora
- JHDocumento2 pagineJHErika Anne Mercado CadawanNessuna valutazione finora
- LsDocumento2 pagineLsErika Anne Mercado CadawanNessuna valutazione finora
- Ob AssessmentDocumento206 pagineOb AssessmentErika Anne Mercado CadawanNessuna valutazione finora
- Learning Task 1 Module 5Documento2 pagineLearning Task 1 Module 5Erika Anne Mercado CadawanNessuna valutazione finora
- Production Efficiency - DetailedDocumento1 paginaProduction Efficiency - DetailedErika Anne Mercado CadawanNessuna valutazione finora
- Total Logged in Hours Cell 1: TO: FromDocumento26 pagineTotal Logged in Hours Cell 1: TO: FromErika Anne Mercado CadawanNessuna valutazione finora
- Case Study: Picky Eater. She Is Underweight Based On The Records at The Health CenterDocumento5 pagineCase Study: Picky Eater. She Is Underweight Based On The Records at The Health CenterErika Anne Mercado CadawanNessuna valutazione finora
- Production Efficiency Report - by Routes: Fabrication 93.57 11,240.04 12,013.00Documento1 paginaProduction Efficiency Report - by Routes: Fabrication 93.57 11,240.04 12,013.00Erika Anne Mercado CadawanNessuna valutazione finora
- ConscienceDocumento6 pagineConscienceErika Anne Mercado CadawanNessuna valutazione finora
- Case Study 2Documento2 pagineCase Study 2Erika Anne Mercado CadawanNessuna valutazione finora
- Innovation For Computer EthicsDocumento1 paginaInnovation For Computer EthicsErika Anne Mercado CadawanNessuna valutazione finora
- Assignment For OB AssessmentDocumento4 pagineAssignment For OB AssessmentErika Anne Mercado CadawanNessuna valutazione finora
- Learning Task 3 Module 5Documento2 pagineLearning Task 3 Module 5Erika Anne Mercado CadawanNessuna valutazione finora
- Amniotiv Fluid DisorderDocumento22 pagineAmniotiv Fluid DisorderLiangkiuwiliu100% (1)
- 2023 PDFDocumento8 pagine2023 PDFDamesa MiesaNessuna valutazione finora
- Definition of Terms FPDocumento2 pagineDefinition of Terms FPPiao Liang JingNessuna valutazione finora
- Management Ectopic Pregnancy SLCOGDocumento9 pagineManagement Ectopic Pregnancy SLCOGMelissa Aina Mohd YusofNessuna valutazione finora
- Prenatal Cell-Free DNA Screening: Should I Undergo Prenatal Screening For Genetic Conditions?Documento2 paginePrenatal Cell-Free DNA Screening: Should I Undergo Prenatal Screening For Genetic Conditions?Derrick ThompsonNessuna valutazione finora
- Aicog 2020 PDFDocumento29 pagineAicog 2020 PDFDr.Shubhi SrivastavaNessuna valutazione finora
- DR Muhabat Salih Saeid MRCOG-London-UKDocumento28 pagineDR Muhabat Salih Saeid MRCOG-London-UKYastriAmaliaAngkasahNessuna valutazione finora
- Molar Pregnancy - SB Guideline 2020Documento11 pagineMolar Pregnancy - SB Guideline 2020Narjina BegamNessuna valutazione finora
- Induction of Labor Algorithm: Appendix RDocumento1 paginaInduction of Labor Algorithm: Appendix RBrolie BarsebaNessuna valutazione finora
- A Study To Assess Effectiveness of Information Booklet Regarding Use of Partograph Among Midwives Working in Labour Room of Selected Hospital of Bhopal M.PDocumento8 pagineA Study To Assess Effectiveness of Information Booklet Regarding Use of Partograph Among Midwives Working in Labour Room of Selected Hospital of Bhopal M.PEditor IJTSRDNessuna valutazione finora
- DR Amit Gupta - Medical Institute For Screening TestDocumento122 pagineDR Amit Gupta - Medical Institute For Screening TestEducation PlazaNessuna valutazione finora
- Second-Trimester Pregnancy Termination - Dilation and Evacuation - UpToDateDocumento21 pagineSecond-Trimester Pregnancy Termination - Dilation and Evacuation - UpToDateKadek Erlin Putri FebriantiNessuna valutazione finora
- Ivf and Icsi Consent FormDocumento10 pagineIvf and Icsi Consent FormSantosoNessuna valutazione finora
- Partograph FormDocumento2 paginePartograph FormEduard100% (5)
- Abortion ResearchDocumento21 pagineAbortion ResearchCharu GuptaNessuna valutazione finora
- Family PlanningDocumento192 pagineFamily PlanningPatricia Ann Factor-TarucNessuna valutazione finora
- Assessments of Puerperal Sepsis in Women at Kampala International University Teaching Hospital Western Campus, Uganda.Documento11 pagineAssessments of Puerperal Sepsis in Women at Kampala International University Teaching Hospital Western Campus, Uganda.KIU PUBLICATION AND EXTENSIONNessuna valutazione finora
- Ob 2Documento17 pagineOb 2Rizza Mae SalvaniaNessuna valutazione finora
- Oxytocin Drug StudyDocumento2 pagineOxytocin Drug StudyRem remNessuna valutazione finora
- The Grand MultiparaDocumento5 pagineThe Grand MultiparaIndhumathiNessuna valutazione finora
- Multiple PregnancyDocumento32 pagineMultiple PregnancyRebbeccah NafulaNessuna valutazione finora
- Delivery Room E-Portfolio: Bartolaba, Lyca RDocumento17 pagineDelivery Room E-Portfolio: Bartolaba, Lyca RLRBNessuna valutazione finora
- Complications of Twin Pregnancy: by Harsh SharmaDocumento19 pagineComplications of Twin Pregnancy: by Harsh SharmakushalNessuna valutazione finora
- AoW 12 - 13 38 Morning After PillDocumento2 pagineAoW 12 - 13 38 Morning After PillWan SyazwanNessuna valutazione finora
- Doula and Midwife: What Is A Doula? Can A Doula Deliver Babies?Documento4 pagineDoula and Midwife: What Is A Doula? Can A Doula Deliver Babies?tiur safitriNessuna valutazione finora
- 1215李茂盛教授住診Documento24 pagine1215李茂盛教授住診peipeipoorNessuna valutazione finora
- Provision of ATSMs in WoS September 2009Documento2 pagineProvision of ATSMs in WoS September 2009WAGS CommitteeNessuna valutazione finora
- 2-Complications of Pregnancy Pt1Documento37 pagine2-Complications of Pregnancy Pt1pavi7muruganathanNessuna valutazione finora
- Medical Termination of Pregnancy Act and RuleDocumento2 pagineMedical Termination of Pregnancy Act and Rulemollymaheshwari00Nessuna valutazione finora
- Commercial Surrogacy Power PointDocumento13 pagineCommercial Surrogacy Power Pointjiadong98Nessuna valutazione finora