Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
In Elderley Wiley
Caricato da
Noel Saúl Argüello SánchezTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
In Elderley Wiley
Caricato da
Noel Saúl Argüello SánchezCopyright:
Formati disponibili
Address for correspondence:
Clinical Investigations Aleksander Goch, PhD
Department of Cardiology
Medical University of Lodz-Poland
Sterlinga 1/3; 91–425 Lodz, Poland
The Clinical Manifestation of Myocardial a.goch@termedia.pl
Infarction in Elderly Patients
Aleksander Goch, PhD; Paweł Misiewicz, MD; Jacek Rysz, MD, FASN, FASA, FSGC;
Maciej Banach, MD, FESC, FASA, FSGC
Department of Cardiology, 1st Chair of Cardiology and Cardiac Surgery, Medical University of
Lodz, Poland (Goch); Emergency Department, Specialist Hospital, Radom, Poland (Misiewicz);
Department of Nephrology, Hypertension and Family Medicine, Medical University of Lodz, Lodz,
Poland (Rysz); Department of Molecular Cardionephrology and Hypertension, Medical University
of Lodz, Lodz, Poland (Banach)
Background and Hypothesis: The study aimed to compare the clinical picture and treatment differences in
elderly patients (aged 75 years or older) and younger patients (aged below 75 years).
Methods: The study included 80 consecutive patients with myocardial infarction (MI) treated in the Cardiology
Ward of the Specialist Hospital in Radom, Poland, in 2005. Analyses were performed retrospectively. The
patients were separated into 2 groups according to age. The group I study group consisted of 40 patients
aged 75 or over (aged 75–95; mean 81 years) and the group II control group consisted of 40 patients aged
below 75 years (aged 42–67; mean 60 years).
Results: In the elderly, as compared with younger subjects, dyspnea, fatigue, and other heart failure symptoms,
were more frequently the first symptoms of MI than typical chest pain (p<0.05). ST-segment elevation
myocardial infarction (STEMI) was also more common (p<0.05). Non-ST-segment elevation myocardial
infarction (NSTEMI) was more frequently diagnosed in the elderly (p<0.05). In elderly patients there were
more women (p<0.05), more patients with previously diagnosed ischemic heart disease (p<0.05), with
hypertension (p<0.05), and with diabetes mellitus (p<0.05). Obesity was less frequently diagnosed in the
elderly; however the difference was not statistically significant. Dyslipidemia and cigarette smoking were both
significantly less common among elderly patients (p<0.05). The elderly were significantly less frequently
revascularized (p<0.05). Both fibrinolysis and primary percutaneous coronary intervention (PCI) were less
commonly applied to the elderly (p<0.05). Time from symptom onset to hospital admission was significantly
longer in the case of elderly patients (p<0.05). The MI complications and side effects of treatment seemed to
be more frequent in the elderly, but only post-MI heart failure was observed more frequently in this group of
patients (p< 0.05).
Conclusions: Our observations confirm the differences in the clinical picture of MI in the elderly as described
previously. All patients of advanced age should be considered as having the highest risk of death and
complications occurrence.
Introduction Longevity in developed countries has improved signifi-
Myocardial infarction (MI) remains the leading cause of cantly in recent years. A large number of people with MIs
hospitalizations as well as the leading cause of death are older than 65 years and this number will be increasing.
worldwide. In Poland, more than 100,000 patients suffer It is estimated that the number of people aged >65 years
from MIs each year. A total of 25%–55% of these patients in 2015 will reach 540 million and in 2025 about 1 billion.
die in the pre-hospital period, 7%–15% in the hospital, and The process of societal aging is also seen in Poland. In 2004,
5%–10% within the following 12 mon.1 Both in-hospital and 14.8% of the people in Poland were older than 65.7 According
long-term mortality are significantly higher in the elderly, to the United Nations these data classify Polish society as
regardless of the type of treatment.2,3,4 In patients with an aging one. The percentage of elderly people in Poland is
acute myocardial infarction (AMI) who are older than 70 predicted to increase up to 26% by 2030.
years, mortality rates exceed 30%.5 Besides anterior MI, The incidence and prevalence of MI increase progres-
heart rate >100 beats/min, overt heart failure, and systolic sively with age. In the United States, over 60% of acute MIs
blood pressure <100 mm Hg, age >70 years is one of the occur in patients 65 years of age or older, and approximately
predictors of poor outcome after MI.2,6 one third occur in persons over age 75.8 Coronary heart
E46 Clin. Cardiol. 32, 6, E46–E51 (2009)
Published online in Wiley InterScience. (www.interscience.wiley.com)
Received: August 30, 2007
Accepted with revision: November 25, 2007
DOI:10.1002/clc.20354 2009 Wiley Periodicals, Inc.
disease is more advanced in the elderly than in younger history must have been documented in medical reports
patients. Three-vessel disease occurred in 44% of subjects (discharge chart from a hospital).
with ischemic heart disease aged 65–74 and in 63% of
subjects aged 75 and over.9 Statistical analysis
The clinical features of acute MI vary by age in many The results are presented as the number of patients charac-
aspects. Because of the increasing burden on health care terized by the analyzed feature. Statistical significances of
systems associated with MIs in the elderly, differences the differences between the groups were examined by the
in clinical picture, and difficulties in dealing with elderly Student t test or Mann-Whitney U test (when data were not
patients with MI, we analyzed the course of MIs in the normally distributed). A p value <0.05 was assumed to be
group of patients aged 75 years or older hospitalized in statistically significant.
the Cardiology Ward of the Specialist Hospital in Radom in
2005. The aim of our study was to determine presentation, Results
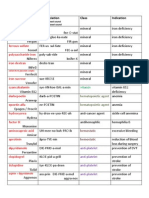
cardiac-risk factors, and management strategies in the First, clinical symptoms of MI differed in the elderly as
elderly (≥75 years) compared with those in younger patients compared to younger patients. Chest pain was reported
(<75 years). less frequently (19 [47.5%] versus 32 [80%]; p<0.05) and
dyspnea or fatigue was reported more frequently (18 [45%]
Materials and Methods versus 7 [17.5%]; p<0.05) by the elderly (Table 1). Also,
The study included 80 consecutive patients with MIs treated electrocardiographic presentation differed in the elderly.
in the Cardiology Ward of the Specialist Hospital in Radom ST-elevation was less frequently detected in the elderly
in 2005. Analyses were performed retrospectively. MI was (21 [52.5%] versus 26 [65%]; p<0.05), while ST-depression
defined according to the European Society of Cardiology was more frequently detected (15 [35%] versus 11 [27.5%];
(ESC) definition from 2000,10 by the significant elevation of p<0.05). The differences were statistically significant. LBBB
myocardial necrosis markers (troponin T/CK-MB) in addi- and negative T-waves tended to be more frequent in
tion to a history compatible with MI, electrocardiographic the elderly, but the differences did not reach statistical
abnormalities, or both. The history compatible with MI significance (p>0.05) in our observations. MI with LBBB
was defined as the presence of anginal chest pain lasting occurred in 3 elderly and 2 younger patients (Table 1).
more than 30 min. The electrocardiographic abnormalities In elderly patients there were more women (p<0.05),
were defined as: ≥1 mm ST-segment elevation in contigu- more patients with previously diagnosed ischemic heart
ous leads; ≥1 mm ST-segment depression; definite T-wave disease (p<0.05), with hypertension (p<0.05), and with
inversion; evolution of pathologic Q-waves (≥0.04 sec); or diabetes mellitus (p<0.05). Obesity was less frequently diag-
new left bundle branch block (LBBB). nosed in the elderly, but the difference was not statistically
The patients were separated into 2 groups according to
age. The group I study group consisted of 40 patients aged Table 1. MI symptoms and MI ECG presentation
75 or over (aged 75–95; mean 81 years) and the group II
MI symptoms Age ≥75 Age <75 p value
control group consisted of 40 patients aged below 75 years
(aged 42–67; mean 60 years). In this article, we have defined Chest pain 19 (47.5%) 32 (80%) p<0.05
elderly patients as being 75 or older. ST-segment elevation
(Typical/atypical/ 11/6/2 21/8/3 –
myocardial infarction (STEMI) occurred in 47 cases.
non-characteristic)∗ 27.5/15/5% 52.5/20/7.5%
All patients received standard therapy according to the
ESC standards and according to clinical setting. Dyspnea/fatigue 18 (45%) 7 (17.5%) p<0.05
Hypertension was defined according to JNC VII (the
Other symptoms∗∗ 3 (7.5%) 1 (2.5%) NS
seventh report of the Joint National Committee on Preven-
tion, Detection, Evaluation, and Treatment of High Blood ECG changes
Pressure)7 criteria (2 measurement values of blood pressure
STEMI 21 (52.5%) 26 (65%) p<0.05
≥140/90 mm Hg, or patient was on hypotension therapy
before MI). Dyslipidemia was defined according to ESC pre- NSTEMI 14 (35%) 11 (27.5%) p<0.05
vention guidelines11 (total cholesterol ≥190 mg/dl and/or
Acute LBBB 3 (7.5%) 2 (5%) NS
triglycerides ≥150 mg/dl, or patient was on hypolipidemic
therapy—statins/fibrates before MI). Obesity was defined ∗
Typical pain: 3 features, atypical pain: 2 features, non-characteristic
based on the body mass index ≥30 kg/m2 . Diabetes melli- pain: 1 feature of coronary pain.10 ∗∗ Other symptoms: anxiety, sweating,
tus (DM) was diagnosed if patient suffered from DM before palpitations. Abbreviations: ECG = electrocardiogram; LBBB = left
MI. The patient was assumed to be an addictive smoker if bundle branch block; MI = myocardial infarction; NSTEMI = non-ST-
segment elevation myocardial infarction; STEMI = ST-segment elevation
he/she smoked actively before MI. All episodes of ischemic
myocardial infarction.
heart disease and the episodes of invasive procedures in
Clin. Cardiol. 32, 6, E46–E51 (2009)
A. Goch et al.: Myocardial infarction in the elderly
E47
Published online in Wiley InterScience. (www.interscience.wiley.com)
DOI:10.1002/clc.20354 2009 Wiley Periodicals, Inc.
Clinical Investigations continued
significant. A family history of ischemic heart disease, PCI was performed on 42 patients in total, on 17 (44%) and 24
dyslipidemia, and cigarette smoking were significantly less (60%) of groups I and II, respectively. Elderly patients these
common (p<0.05) among elderly patients (Table 2). 2 invasive procedures performed—coronary angiography
Elderly patients had suffered from previous MIs more and PCI—significantly less frequently when compared to
frequently (p<0.05) and they had undergone coronary younger patients (p<0.05; Table 4).
angiography and PCI less frequently (p<0.05). Only 1 During the course of hospitalization, elderly patients
patient over 75 had had coronary artery bypass graft surgery rarely received angiotensin converting enzyme inhibitors
compared to none in the group of younger patients. There (ACE-I; p<0.05). Low molecular weight heparin was
was statistical significance in the higher frequency of elderly more often administered (p<0.05). Other medications
patients having been diagnosed with ischemic heart disease like aspirin, clopidogrel, beta-blockers, and unfractionated
before MI (p<0.05; Table 3). heparin (UFH), were used in both groups with the same
A total of 25 (31%) patients received thrombolytic treat- frequency (Table 5). As to MI complication, only recurrent
ment: 14 (34%) elderly and 11 (27%) younger patients, but the MI occurred more frequently in the elderly (p<0.05)
differences were not statistically significant (p>0.05). Coro- (Table 6).
nary angiography was performed on 54 (67.5%) patients in The time duration from symptom onset to hospital
total, on 20 (50%) and 34 (85%) of groups I and II, respectively. admission was significantly longer in the case of elderly
patients (p<0.05; Table 7). Mean time for the elderly was
5 h and 56 min contrasted to 3 h and 45 min for younger
Table 2. Cardiac risk factors profile
patients.
Risk factors Age ≥75 Age <75 p value The MI complications and side effects of treatment
seemed to be more frequent in the elderly, but only post-MI
Women 21 (52%) 14 (35%) p<0.05
heart failure was observed more frequently in patients of
Men 19 (65%) 26 (65%) p<0.05 group I (p<0.05).
Smoking 8 (20%) 21 (52%) p<0.05
Table 4. Reperfusion therapy
Hyperlipidemia 14 (35%) 17 (42%) p<0.05
Reperfusion therapy Age ≥75 Age <75 p value
History of IHD 28 (70%) 24 (60%) p<0.05
Thrombolysis 14 (34%) 11 (27%) NS
Hypertension 22 (55%) 18 (45%) p<0.05
Coronary angiography 20 (50%) 34 (85%) p<0.05
Diabetes mellitus 12 (30%) 5 (12%) p<0.05
PCI 17 (44%) 24 (60%) p<0.05
Obesity∗ 11 (27%) 12 (30%) NS
CABG 2 (5%) 1 (2.5%) NS
Family history∗∗ 8 (20%) 18 (45%) p<0.05
Abbreviations: CABG = coronary artery bypass grafting; PCI =
Abbreviation: IHD = ischemic heart disease. ∗ Obesity was defined as percutaneous coronary intervention.
BMI (body mass index) ≥30 kg/m2 . ∗∗ Family history is defined as any
clinical atherosclerosis in the family diagnosed in females before 65 and
in males before 55 years old.
Table 5. Medical treatment of MI
Medical treatment Age ≥75 Age <75 p value
Table 3. Episodes of ischemic heart disease and the episodes of invasive
procedures in history ASA 39 37 NS
History of IHD Age ≥75 Age <75 p value Clopidogrel 28 30 NS
MI 9 (23%) 6 (16%) p<0.05 ACE-I 26 21 p<0.05
Coronary angiography 2 (5%) 5 (12%) p<0.05 AT 1 antagonists 7 5 NS
PCI 2 (5%) 4 (10%) p<0.05 Beta-blockers 19 21 NS
CABG 1 (2.5%) 0 NS UFH 23 23 NS
IHD 28 (70%) 24 (60%) p<0.05 LMWH 5 12 p<0.05
Abbreviations: CABG = coronary artery bypass grafting; IHD = ischemic Abbreviations: ACE-I = angiotensin converting enzyme inhibitors; ASA
heart disease; MI = myocardial infarction; PCI = percutaneous coronary = aspirin; AT1 = antiotensin type 1 receptor; LMWH = low molecular
intervention. weight heparin; UFH = unfractionated heparin.
E48 Clin. Cardiol. 32, 6, E46–E51 (2009)
A. Goch et al.: Myocardial infarction in the elderly
Published online in Wiley InterScience. (www.interscience.wiley.com)
DOI:10.1002/clc.20354 2009 Wiley Periodicals, Inc.
Table 6. MI complications in the acute phase of MI.14,16 Even when classic ischemic
MI complications Age ≥75 Age <75 p value precordial discomfort is present, it tends to be less severe
and less well defined. The elderly appear to have reduced
Cardiogenic shock 5 (12%) 7 (18%) NS
pain perception.17 This phenomenon may result from the
Pulmonary edema 7 (18%) 9 (23%) NS increase of pain threshold of permanently ischemic sen-
sory nerves, ischemic dysfunction of the cerebral cortex,
VT/VI 10 (25%) 13 (33%) NS
and dysfunction of the autonomic nervous system.18 The
Recurrent MI 3 (8%) 5 (12%) p<0.05 last one is very likely exemplified in that the elderly who
did not describe chest pain also did not describe sweating,
Post-MI unstable angina pectoris 4 (10%) 5 (12%) NS
nausea, and vomiting.19 The older the population, the more
Heart failure* 5 (12%) 11 (27%) NS frequently the symptoms of heart failure exacerbation were
described in the acute phase of MI.20 Typical symptoms of
Stroke 1 (2.5%) 1 (2.5%) NS
chronic heart failure exacerbation were often accompanied
Serious bleeding 1 (2.5%) 2 (5%) NS by mental disorders, dizziness, presyncope, and syncope.20
Older patients are also more likely to have ‘‘silent’’ or
Death 2 (5%) 5 (12%) NS
unrecognized MIs compared to younger patients. These
Abbreviation: MI = myocardial infarction. ∗ Heart failure is defined as facts often result in delays in MI diagnosis in the elderly. The
clinical symptoms (rest dyspnea) and/or physical signs (pulmonary length of time from symptom onset to hospital admission
congestions) on the admission or ejection fraction (EF)<45% in was significantly longer for the elderly compared to the
echocardiography performed on the discharge. younger patients in our study (5 h 56 min versus 3 h 45
min). Such trends have been observed previously.21
Table 7. Time from symptom onset to hospital admission Apart from clinical presentation in the acute phase
of MI, the cardiac risk factor profile of elderly patients
Time Age ≥75 Age <75 p value
with MI is different. Older patients are mostly women
Time <1 h 3 (8%) 8 (20%) p<0.05 with a history of heart failure and MI, and risk factors
are predominantly diabetes mellitus and hypertension.
Time <2 h 10 (25%) 18 (44%) p<0.05
Smoking, dyslipidemia, and family history seem not to be
Time <6 h 14 (35%) 11 (28%) NS very important or widespread risk factors in the elderly. A
better understanding of the prevalence of various risk factors
Time >6 h 13 (32%) 3 (8%) p<0.05
among patients with MI may help to develop secondary
prevention programs to target different age groups with
different preventive methods.
Discussion
It was documented previously that with increasing age,
The clinical picture of MI in elderly patients differs in
the gender composition of patients with MI changed.5,22
many aspects as compared to younger patients. The factors
In middle-aged patients men dominate, whereas in patients
affecting the course of MI in the elderly have not been
aged 75 and over the definite predominance of women was
studied in detail. Clinical studies have incorporated very
revealed. Female predominance among the elderly is the
limited numbers of the elderly, since most of the studies
result of their longer lifespan in comparison to men.
excluded people over 65 years old,12,13 and some did not
Despite the fact that older patients constitute the group
have more than 10% older people.14
In the elderly, numerous disorders often coexist. of high coronary risk and that numerous observations and
Ischemic heart disease, hypertension, diabetes mellitus, studies proved that these patients benefit significantly from
chronic obstructive pulmonary disease, chronic renal fail- PCI in acute MI,23,24,25 invasive procedures in this group of
ure, digestive system disorders, as well as, joint and bone patients are performed relatively rarely. This was consistent
disorders occur more often in this group of patients. The with our observations. PCI was performed in 17 (44%)
coexistence of several diseases may cause the clinical pic- elderly patients and 24 (60%) younger ones, which made
ture of acute coronary syndrome to be uncharacteristic. In the difference statistically significant. Even thrombolysis
the first hours of MI, the elderly are more likely to com- is applied less frequently in the elderly because of the
plain about symptoms other than typical coronary chest threat of bleeding complications and the diagnosis delay
pain. They often describe dyspnea, fatigue, and dizziness. that causes exceeding of the therapeutic ‘‘window’’ of 12
Confusion or altered mental status may be the presenting h. Although several studies26,27 proved that elderly patients
manifestation of acute MI in up to 20% of patients over benefit from reperfusion therapy,23,24,25 they received both
85 years of age.15 It was observed previously that 75% of thrombolytic and invasive procedures less frequently when
patients over 85 with MIs did not complain about chest pain compared with younger patients. This paradox phenomenon
Clin. Cardiol. 32, 6, E46–E51 (2009)
A. Goch et al.: Myocardial infarction in the elderly
E49
Published online in Wiley InterScience. (www.interscience.wiley.com)
DOI:10.1002/clc.20354 2009 Wiley Periodicals, Inc.
Clinical Investigations continued
was observed in many clinical studies and registries27 and 7. Kowalski J, Banach M, Barylski M, et al. Neutrophil superoxide
anion generation during atorvastatin and fluvastatin therapy
was confirmed in our small sample as well.
used in coronary heart disease primary prevention. J Cardiovasc
In the previous observations, an increasing gradient of Pharmacol. 2006;48:143–147.
mortality with increasing age was seen.20 In our study, 5 8. Rich MW. Epidemiology, clinical features, and prognosis of
patients of the elderly group and 2 of the younger individuals acute myocardial infarction in the elderly. Am J Geriatr Cardiol.
died in the hospital. The differences were not statistically 2006;15:7–11.
9. Thompson RC, Holmus DR Jr, Gersh BJ, Mock MB, Bailey
significant. The incidence of recurrent angina was observed
KR. Percutaneous transluminal coronary angioplasty in the
previously20 to be less frequent in the elderly. Such a trend elderly: early and long term results. J Am Coll Cardiol. 1991;17:
was also observed in our study, but it was not statistically 1245–1250.
significant. The only statistically significant difference in 10. Myocardial infarction redefined: a consensus document of The
post-MI complications between the elderly and younger Joint European Society of Cardiology/American College of
Cardiology Committee for Myocardial Infarction Redefinition. Eur
patients was a higher incidence of post-MI heart failure.28
Heart J. 2000;21:1502–1513.
11. De Backer G, Ambrosioni E, Borch-Johnsen K, et al. European
Limitations of the Study guidelines on cardiovascular disease prevention in clinical practice:
The retrospective nature of the study is an obvious Third joint task force of European and other societies on
cardiovascular disease prevention in clinical practice. European
methodological limitation. We also realized that the number
Heart J. 2003;24:1601–1610.
of patients in the study groups was small, which significantly 12. AIMS Trial Study Group. Effect of intravenous APSAC on mortality
limits our conclusions from the observations. However, after acute myocardial infarction: preliminary report of a placebo
the results of our observations are consistent with those controlled trial. Lancet. 1989;1:545–549.
reported previously. 13. Chesbro JH; TIMI Investigators. Thrombolysis in Myocardial
Infarction (TIMI) trial. Phase I: a comparison between intravenous
In conclusion, our observations confirmed the differences
tissue plasminogen activator and intravenous streptokinase.
in the clinical picture of MI between older and younger Circulation. 1987;76:142–154.
individuals in many aspects. The elderly present less typical 14. Akiyama J, Aonuma K, Nogami A, et al. Thrombolytic therapy
symptoms of MI, which is followed by the significant delay can reduce the arrhythmogenic substrate after acute myocardial
in diagnosis and initiation of the treatment. This group infarction: a study using the signal-averaged electrocardiogram,
endocardial catheter mapping and programmed ventricular
also has different cardiac risk factor profile characteristics. stimulation. Circ J. 1999;63:838–842.
Despite the fact that the elderly constitute a group at 15. Banach M, Drożdż J, Okonski P, Rysz J. Immunological aspects
high cardiovascular risk, the most effective methods of of the statins’ function in patients with heart failure: a report from
MI treatment, such as reperfusion procedures including the Annual Conference of ESC—Heart Failure 2005. Cell Mol
PCI, are performed significantly less often when compared Immunol. 2005;2:433–437.
16. Muller RT, Gould LA, Betzu RY, Vacek T, Pradeek V. Painless
to younger MI patients. The majority of differences noticed myocardial infarction in the elderly. Am Heart J. 1990;119:
in our small sample have been observed previously. 202–204.
17. Gregoratos G. Clinical manifestations of acute myocardial
References infarction in older patients. Am J Geriatr Cardiol. 2001;10:
1. Kitazume H, Kubo I, Iwama T, Ageishi Y, Suzuki A. Percutaneous 345–347.
transluminal coronary angioplasty for elderly patients. Circ J. 18. Miller PF, Sheps DS, Bragdon EE, et al. Aging and pain perception
1988;52:449–453. in ischemic heart disease. Am Heart J. 1990;12:22–27.
2. Batchelor WB, Anstrom KJ, Muhlbaier LH, et al. Contemporary 19. Bayer AL, Chadha JS, Farag RR, Pathy MS. Changing presentation
outcome trends in the elderly undergoing percutaneous coronary of myocardial infarction with increasing old age. J Am Geriatr Soc.
interventions: results in 7,472 octogenarians. J Am Coll Cardiol. 1986;34:263–269.
2000;36:723–30. 20. Paul DS, O’Gara PT, Mahjoub ZA, et al. Geriatric patients with
3. DeGeare VS, Stone GW, Grines L. Angiographic and clinical acute myocardial infarction: cardiac risk profiles, presentation,
characteristics associated with increased in-hospital mortality thrombolysis, coronary interventions, and prognosis. Am Heart J.
in elderly patients with acute myocardial infarction undergoing 1996;131:710–715.
percutaneous intervention (A pooled analysis of the primary 21. Haase KK, Schiele R, Wagner S, et al. In-hospital mortality of
angioplasty in myocardial infarction trials). Am J Cardiol. elderly patients with acute myocardial infarction: data from MITRA
2000;86:30–34. (Maximal Individual Therapy in Acute Myocardial Infarction)
4. Lee KL, Woodlief LH, Topol EJ, et al. Predictors of 30-day registry. Clin Cardiol. 2000;23:831–836.
mortality in the era of reperfusion for acute myocardial infarction: 22. Smith SC, Gilpin E, Ahnve S, et al. Outlook after acute myocardial
results from an international trial of 41,021 patients. Circulation. infarction in the very elderly compared with that in patients aged
1995;91:1659–1668. 65 to 75 years. J Am Coll Cardiol. 1990;16:784–792.
5. Devlin W, Cragg D, Jacks M. Comparison of outcome in patients 23. Matetzky S, Sharir T, Moc M, et al. Primary angioplasty for
with acute myocardial infarction aged 75 years with that in younger acute myocardial infarction in octogenarians. Am J Cardiol.
patients. Am J Cardiol. 1995;75:573–576. 2001;88:680–683.
6. Grines CL, Westerhausen DR, Grines LL, et al; Air PAMI Study 24. Banach M, Goch A, Misztal M, et al. Low output syndrome
Group. A randomized trial of transfer for primary angioplasty following aortic valve replacement: predictors and prognosis. Arch
versus on-site thrombolysis in patients with high-risk myocardial Med Sci. 2007;3:117–122.
infarction: the air primary angioplasty in myocardial infarction 25. Harpaz D, Rozenman Y, Behar S, et al. Israeli Working Group on
study. J Am Coll Cardiol. 2002;39(11):1713–1719. Intensive Cardiac Care, Israel Heart Society: coronary angiography
E50 Clin. Cardiol. 32, 6, E46–E51 (2009)
A. Goch et al.: Myocardial infarction in the elderly
Published online in Wiley InterScience. (www.interscience.wiley.com)
DOI:10.1002/clc.20354 2009 Wiley Periodicals, Inc.
in the elderly with acute myocardial infarction. Int J Cardiol. 27. Mehta SR, Cannon CP, Fox KA, et al. Routine vs selective strategies
2007;116:249–256. in patients with acute coronary syndromes: a collaborative meta-
26. Kosuge M, Kimura K, Kojima S, et al. Japanese Acute analysis of randomised trials. JAMA. 2005;293:2908–2917.
Coronary Syndrome Study (JACSS) Investigators: beneficial 28. Goch A, Banach M, Piotrowski G, Szadkowska I, Goch JH.
effect of preinfarction angina on in-hospital outcome is Echocardiographic evaluation of left atrium and left atrium
preserved in elderly patients undergoing coronary intervention appendage function in patients with atrial septum aneurysm:
for anterior acute myocardial infarction. Circ J. 2005;69(6): implications for thromboembolic complications. Thorac Cardiovasc
630–635. Surg. 2007;55:365–370.
Clin. Cardiol. 32, 6, E46–E51 (2009)
A. Goch et al.: Myocardial infarction in the elderly
E51
Published online in Wiley InterScience. (www.interscience.wiley.com)
DOI:10.1002/clc.20354 2009 Wiley Periodicals, Inc.
Potrebbero piacerti anche
- Omersa2016 Article MortalityAndReadmissionsInHearDocumento7 pagineOmersa2016 Article MortalityAndReadmissionsInHearAhmad FathoniNessuna valutazione finora
- Congestive Heart Failure in The ElderlyDocumento13 pagineCongestive Heart Failure in The ElderlyKezia MarsilinaNessuna valutazione finora
- PAD Current InsightsDocumento15 paginePAD Current InsightsMaria PopNessuna valutazione finora
- Premature Coronary Artery Disease Among Angiographically Proven Atherosclerotic Coronary Artery Disease in North East of Peninsular MalaysiaDocumento10 paginePremature Coronary Artery Disease Among Angiographically Proven Atherosclerotic Coronary Artery Disease in North East of Peninsular MalaysiaLili YaacobNessuna valutazione finora
- Managementul Pacientilor Boala Arteriala PerifericaDocumento5 pagineManagementul Pacientilor Boala Arteriala PerifericaIrina NeamtuNessuna valutazione finora
- Contemporaryandoptimal Medicalmanagementof PeripheralarterialdiseaseDocumento18 pagineContemporaryandoptimal Medicalmanagementof PeripheralarterialdiseaseAnonymous kdBDppigENessuna valutazione finora
- Pattern of Stroke in Type 2 Diabetic Subjects Versus Non Diabetic SubjectsDocumento4 paginePattern of Stroke in Type 2 Diabetic Subjects Versus Non Diabetic SubjectsRobbi OcktadinataNessuna valutazione finora
- Jurnal Coronary Angiography Findings in Patients at Robert Wolter Monginsidi Hospital-ManadoDocumento4 pagineJurnal Coronary Angiography Findings in Patients at Robert Wolter Monginsidi Hospital-ManadoRettyNessuna valutazione finora
- Complementary and Alternative Medical Lab Testing Part 4: VascularDa EverandComplementary and Alternative Medical Lab Testing Part 4: VascularNessuna valutazione finora
- Seminar: John J V Mcmurray, Marc A PfefferDocumento13 pagineSeminar: John J V Mcmurray, Marc A Pfefferjvasco_santos8178Nessuna valutazione finora
- PNM 2018 358-360 PDFDocumento3 paginePNM 2018 358-360 PDFputriNessuna valutazione finora
- Causes of Heart FailureDocumento4 pagineCauses of Heart Failurejana7-7Nessuna valutazione finora
- Heart Failure With Preserved Ejection Fraction - Concept, Pathophysiology, Diagnosis and Challenges For TreatmentDocumento7 pagineHeart Failure With Preserved Ejection Fraction - Concept, Pathophysiology, Diagnosis and Challenges For TreatmentOngky AristianNessuna valutazione finora
- Secondary HypertensionDa EverandSecondary HypertensionAlberto MorgantiNessuna valutazione finora
- Association Between Acute Myocardial Infarction, Lipid Profile and Smoking HabitDocumento5 pagineAssociation Between Acute Myocardial Infarction, Lipid Profile and Smoking HabitIOSRjournalNessuna valutazione finora
- Cardiovascular Disease PHD ThesisDocumento6 pagineCardiovascular Disease PHD Thesisafknawjof100% (2)
- Medicina 55 00687 v2 PDFDocumento16 pagineMedicina 55 00687 v2 PDFAwatiful AzzaNessuna valutazione finora
- Postural Tachycardia Syndrome: A Concise and Practical Guide to Management and Associated ConditionsDa EverandPostural Tachycardia Syndrome: A Concise and Practical Guide to Management and Associated ConditionsNicholas GallNessuna valutazione finora
- Faktor Dominan Risiko Terjadinya Penyakit Jantung Koroner (PJK) Ros Endah Happy Patriyani, David Ferry PurwantoDocumento8 pagineFaktor Dominan Risiko Terjadinya Penyakit Jantung Koroner (PJK) Ros Endah Happy Patriyani, David Ferry PurwantoBaiq RianaNessuna valutazione finora
- Research ArticleDocumento9 pagineResearch Articleinterna unpadNessuna valutazione finora
- Familial Hypercholesterolemia in Premature Acute Coronary Syndrome. Insights From Cholestemi RegistryDocumento12 pagineFamilial Hypercholesterolemia in Premature Acute Coronary Syndrome. Insights From Cholestemi RegistryTeodor BicaNessuna valutazione finora
- CMJ 128 2588Documento7 pagineCMJ 128 2588Le DungNessuna valutazione finora
- ECG and VCG in Left Ventricular Hypertrophy LVHDocumento78 pagineECG and VCG in Left Ventricular Hypertrophy LVHNguyen TuanNessuna valutazione finora
- 8353-Article Text-29333-1-10-20130721Documento12 pagine8353-Article Text-29333-1-10-20130721Bhumsen ThapaNessuna valutazione finora
- JournalDocumento11 pagineJournalewetNessuna valutazione finora
- PVDI Scientific AbstractsDocumento2 paginePVDI Scientific AbstractsBombinTallerdeTeatroNessuna valutazione finora
- Ischemic 39!Documento6 pagineIschemic 39!Adina Alexandra CNessuna valutazione finora
- Journal 4Documento7 pagineJournal 4Denys PutraNessuna valutazione finora
- In Patients With Acute Myocardial Infarction, The Impact of Hyperglycemia As A Risk Factor For Mortality Is Not Homogeneous Across Age-GroupsDocumento3 pagineIn Patients With Acute Myocardial Infarction, The Impact of Hyperglycemia As A Risk Factor For Mortality Is Not Homogeneous Across Age-Groupsatika_Nessuna valutazione finora
- Hypertension in ElderlyDocumento13 pagineHypertension in ElderlybookwormMD100% (2)
- Complementary and Alternative Medical Lab Testing Part 3: CardiologyDa EverandComplementary and Alternative Medical Lab Testing Part 3: CardiologyValutazione: 1 su 5 stelle1/5 (1)
- Early Vascular Aging (EVA): New Directions in Cardiovascular ProtectionDa EverandEarly Vascular Aging (EVA): New Directions in Cardiovascular ProtectionPedro Guimarães CunhaNessuna valutazione finora
- Cardiooo1 PDFDocumento9 pagineCardiooo1 PDFsaarita lozano piedraNessuna valutazione finora
- Serum Concentrations of Adiponectin and Risk of Type 2 Diabetes Mellitus and Coronary Heart Disease in Apparently Healthy Middle-Aged MenDocumento15 pagineSerum Concentrations of Adiponectin and Risk of Type 2 Diabetes Mellitus and Coronary Heart Disease in Apparently Healthy Middle-Aged MenEcha MagungNessuna valutazione finora
- The Open Dermatology JournalDocumento7 pagineThe Open Dermatology JournalTri SulistiyawatiNessuna valutazione finora
- Heart Failure in Older Adults PDFDocumento23 pagineHeart Failure in Older Adults PDFcuisilaisNessuna valutazione finora
- En Do Card It IsDocumento30 pagineEn Do Card It IsPamela LusungNessuna valutazione finora
- JAH3 5 E003347Documento13 pagineJAH3 5 E003347AllahbesertkitaNessuna valutazione finora
- Ipi315870 PDFDocumento5 pagineIpi315870 PDFAnnisa AuraNessuna valutazione finora
- Manuscript Mohamed TantawieyDocumento13 pagineManuscript Mohamed TantawieyMohamed TantawieyNessuna valutazione finora
- Risk Factors For Hypertension and Its Complications Case Control StudyDocumento4 pagineRisk Factors For Hypertension and Its Complications Case Control StudyutarinuNessuna valutazione finora
- Gender Differences in the Pathogenesis and Management of Heart DiseaseDa EverandGender Differences in the Pathogenesis and Management of Heart DiseaseNessuna valutazione finora
- Arterial Hypertension and Aortic Valve Stenosis: Shedding Light On A Common "Liaison"Documento6 pagineArterial Hypertension and Aortic Valve Stenosis: Shedding Light On A Common "Liaison"Adriana VasilicaNessuna valutazione finora
- Role of Hypertension and Obesity As Risk Factors For IhdDocumento5 pagineRole of Hypertension and Obesity As Risk Factors For IhdMohammad Mujtaba GhaffariNessuna valutazione finora
- 2359 4802 Ijcs 34 05 s01 0012.x98175Documento10 pagine2359 4802 Ijcs 34 05 s01 0012.x98175Suryati HusinNessuna valutazione finora
- 21.0 A+'mini-brain'+traces+the+link+between+concussion+and+Alzheimer's+disease+ - +ScienceDailyDocumento3 pagine21.0 A+'mini-brain'+traces+the+link+between+concussion+and+Alzheimer's+disease+ - +ScienceDailyAna Caroline FerreiraNessuna valutazione finora
- Cardiac Sarcoidosis: Key Concepts in Pathogenesis, Disease Management, and Interesting CasesDa EverandCardiac Sarcoidosis: Key Concepts in Pathogenesis, Disease Management, and Interesting CasesNessuna valutazione finora
- Pr2 Chapter 1 3 Peta Icamina 2Documento21 paginePr2 Chapter 1 3 Peta Icamina 2JOHN ICAMINANessuna valutazione finora
- Review WellenDocumento10 pagineReview WellenJihanirani LubisNessuna valutazione finora
- QT Dispersion in Patients With Systemic Lupus Erythematosus: The Impact of Disease ActivityDocumento5 pagineQT Dispersion in Patients With Systemic Lupus Erythematosus: The Impact of Disease ActivityWahyubudi PratamaNessuna valutazione finora
- Corazon EnvejecidoDocumento13 pagineCorazon EnvejecidoAntonio AlonsoNessuna valutazione finora
- Article For Journal - CETDocumento9 pagineArticle For Journal - CETawuahbohNessuna valutazione finora
- Karakteristik Radiologi Penderita Fraktur Femur Di Rsup Dr. Wahidin Sudirohusodo Periode Januari-Desember 2012Documento13 pagineKarakteristik Radiologi Penderita Fraktur Femur Di Rsup Dr. Wahidin Sudirohusodo Periode Januari-Desember 2012Marwan FebrianNessuna valutazione finora
- Original Article: Hyponatremia in Stroke Patients and Its Association With Early MortalityDocumento7 pagineOriginal Article: Hyponatremia in Stroke Patients and Its Association With Early Mortalitykholis rizqullahNessuna valutazione finora
- ICC Cronica Fisiopatologia 2014Documento11 pagineICC Cronica Fisiopatologia 2014Karen Grissell Serrano RamosNessuna valutazione finora
- 10 Iajps10072017Documento5 pagine10 Iajps10072017Baru Chandrasekhar RaoNessuna valutazione finora
- Epidemiology of Coronary Heart Disease and Acute Coronary SyndromeDocumento6 pagineEpidemiology of Coronary Heart Disease and Acute Coronary SyndromeAnonymous GpgioaDAbNessuna valutazione finora
- Coronary Artery Disease Cad2Documento182 pagineCoronary Artery Disease Cad2Mamot MotNessuna valutazione finora
- 8931 26614 2 PB PDFDocumento7 pagine8931 26614 2 PB PDFMaferNessuna valutazione finora
- Prevalensi Sindrom Koroner Akut Di RSUP Prof. Dr. R. D. Kandou Manado Periode 1 Januari 2014 - 31 Desember 2014Documento8 paginePrevalensi Sindrom Koroner Akut Di RSUP Prof. Dr. R. D. Kandou Manado Periode 1 Januari 2014 - 31 Desember 2014lulukNessuna valutazione finora
- Monoclonal Gammopathy of Renal Significance: Review ArticleDocumento11 pagineMonoclonal Gammopathy of Renal Significance: Review ArticleNoel Saúl Argüello SánchezNessuna valutazione finora
- Cannabis Induced Cardiac Arrhythmias: A Case SeriesDocumento9 pagineCannabis Induced Cardiac Arrhythmias: A Case SeriesNoel Saúl Argüello SánchezNessuna valutazione finora
- MOOC PP en 3.5Documento7 pagineMOOC PP en 3.5Noel Saúl Argüello SánchezNessuna valutazione finora
- A Critical Care Echocardiography-Driven Approach To Undifferentiated ShockDocumento7 pagineA Critical Care Echocardiography-Driven Approach To Undifferentiated ShockNoel Saúl Argüello SánchezNessuna valutazione finora
- Cannabis Induced Cardiac Arrhythmias: A Case SeriesDocumento9 pagineCannabis Induced Cardiac Arrhythmias: A Case SeriesNoel Saúl Argüello SánchezNessuna valutazione finora
- Neonatal Genetic SyndromesDocumento11 pagineNeonatal Genetic SyndromesNoel Saúl Argüello SánchezNessuna valutazione finora
- EAU Pocket Guidelines On Urological Infections 2021Documento25 pagineEAU Pocket Guidelines On Urological Infections 2021Noel Saúl Argüello SánchezNessuna valutazione finora
- Fallone 2019Documento10 pagineFallone 2019Noel Saúl Argüello SánchezNessuna valutazione finora
- Neuroprosthesis For Decoding Speech in A Paralyzed Person With AnarthriaDocumento11 pagineNeuroprosthesis For Decoding Speech in A Paralyzed Person With AnarthriaNoel Saúl Argüello SánchezNessuna valutazione finora
- Chapmarinum 2017 ASMDocumento18 pagineChapmarinum 2017 ASMNoel Saúl Argüello SánchezNessuna valutazione finora
- Relationship Between Cannabis Use and Erectile Dysfunction: A Systematic Review and Meta-AnalysisDocumento7 pagineRelationship Between Cannabis Use and Erectile Dysfunction: A Systematic Review and Meta-AnalysisNoel Saúl Argüello SánchezNessuna valutazione finora
- Mechanisms of The Post-Antibiotic Effects Induced by Rifampicin and Gentamicin in Escherichia ColiDocumento5 pagineMechanisms of The Post-Antibiotic Effects Induced by Rifampicin and Gentamicin in Escherichia ColiNoel Saúl Argüello SánchezNessuna valutazione finora
- String Theory For DummiesDocumento1 paginaString Theory For DummiesNoel Saúl Argüello SánchezNessuna valutazione finora
- Clinical Research: Heart Failure/cardiomyopathyDocumento8 pagineClinical Research: Heart Failure/cardiomyopathyNoel Saúl Argüello SánchezNessuna valutazione finora
- dkh130 PDFDocumento7 paginedkh130 PDFNoel Saúl Argüello SánchezNessuna valutazione finora
- Review of Bilirubin Neurotoxicity II: Preventing and Treating Acute Bilirubin Encephalopathy and Kernicterus Spectrum DisordersDocumento6 pagineReview of Bilirubin Neurotoxicity II: Preventing and Treating Acute Bilirubin Encephalopathy and Kernicterus Spectrum DisordersNoel Saúl Argüello SánchezNessuna valutazione finora
- Personal View: Mark Abie Horowitz, David TaylorDocumento9 paginePersonal View: Mark Abie Horowitz, David TaylorNoel Saúl Argüello SánchezNessuna valutazione finora
- Ahfs Hid Sample Monograph PDFDocumento2 pagineAhfs Hid Sample Monograph PDFNoel Saúl Argüello SánchezNessuna valutazione finora
- Comparative Study of Bactericidal Activities, Postantibiotic Effects, and Effects On Bacterial Virulence of Penicillin G and Six Macrolides Against Streptococcus PneumoniaeDocumento4 pagineComparative Study of Bactericidal Activities, Postantibiotic Effects, and Effects On Bacterial Virulence of Penicillin G and Six Macrolides Against Streptococcus PneumoniaeNoel Saúl Argüello SánchezNessuna valutazione finora
- Jccnursing v11n1p1 FaDocumento9 pagineJccnursing v11n1p1 FaNoel Saúl Argüello SánchezNessuna valutazione finora
- Presentations of Acute Myocardial Infarction in Men and WomenDocumento9 paginePresentations of Acute Myocardial Infarction in Men and WomenNoel Saúl Argüello SánchezNessuna valutazione finora
- Acute Myocardial Infarction: Review ArticleDocumento12 pagineAcute Myocardial Infarction: Review ArticleNoel Saúl Argüello SánchezNessuna valutazione finora
- Jama BuenoDocumento7 pagineJama BuenoNoel Saúl Argüello SánchezNessuna valutazione finora
- Prevalence, Clinical Features, and Prognosis of Acute Myocardial Infarction Attributable To Coronary Artery EmbolismDocumento10 paginePrevalence, Clinical Features, and Prognosis of Acute Myocardial Infarction Attributable To Coronary Artery EmbolismNoel Saúl Argüello SánchezNessuna valutazione finora
- FDNY Strategic Plan 2009 2010 FinalDocumento29 pagineFDNY Strategic Plan 2009 2010 Finalبيدرو اسبينوزا مات بيدروNessuna valutazione finora
- Quick Management Guide in Emergency Medicine v1.0.25 20111208 (Build13)Documento156 pagineQuick Management Guide in Emergency Medicine v1.0.25 20111208 (Build13)Anselm Su100% (14)
- Angina PectorisDocumento20 pagineAngina PectorisJyoti singhNessuna valutazione finora
- Angina PectorisDocumento25 pagineAngina PectorisPC NNessuna valutazione finora
- Media Bulletin 11.07.2020 27 Pages English 491 KBDocumento27 pagineMedia Bulletin 11.07.2020 27 Pages English 491 KBKathirasan RamalingamNessuna valutazione finora
- CMDT FC Toc Sample ChapterDocumento14 pagineCMDT FC Toc Sample Chapterbencleese0% (7)
- Koskinas, 2019Documento11 pagineKoskinas, 2019Amro MahmoudNessuna valutazione finora
- Angina PectorisDocumento12 pagineAngina Pectorismardsz93% (14)
- Ischemic Heart Disease (IHD)Documento55 pagineIschemic Heart Disease (IHD)rameshbmc100% (5)
- 2005 Heart+Disease+Diagnosis+and+TherapyDocumento537 pagine2005 Heart+Disease+Diagnosis+and+TherapyrominNessuna valutazione finora
- Fundamentals of Nursing 1Documento6 pagineFundamentals of Nursing 1Fatima Medriza DuranNessuna valutazione finora
- Pharmacy Technician Pronunciation Guide of Drugs Common To The Blood SystemDocumento2 paginePharmacy Technician Pronunciation Guide of Drugs Common To The Blood SystemskdiddenNessuna valutazione finora
- ANGINADocumento33 pagineANGINAAnonymous mIw67bMXNessuna valutazione finora
- Waksman 2018Documento7 pagineWaksman 2018harry pribadiNessuna valutazione finora
- CSAP Full 2002Documento125 pagineCSAP Full 20022012Nessuna valutazione finora
- Presentation Syntax Score TCT 2008 PDFDocumento33 paginePresentation Syntax Score TCT 2008 PDFElla MihNessuna valutazione finora
- Sirajrej Leg LockDocumento8 pagineSirajrej Leg LockUsman ohorellaNessuna valutazione finora
- Coronary Artery DiseaseDocumento22 pagineCoronary Artery DiseaseMamoon RashidNessuna valutazione finora
- HEALTH PROC 7 Surgical Procedures (Shortlist)Documento25 pagineHEALTH PROC 7 Surgical Procedures (Shortlist)Anonymous QKsY8ENessuna valutazione finora
- CGHS Rates 2014 ChandigarhDocumento45 pagineCGHS Rates 2014 Chandigarhsanjeeta.chauhan22Nessuna valutazione finora
- 2536 FullDocumento14 pagine2536 FullPaulo DNessuna valutazione finora
- CardiologyDocumento62 pagineCardiologysee yinNessuna valutazione finora
- Innov Barrier Med DevDocumento23 pagineInnov Barrier Med DevStephen WattNessuna valutazione finora
- Brochure - MagicTouch, Concept MedicalDocumento6 pagineBrochure - MagicTouch, Concept MedicalBUSHRA ILYASNessuna valutazione finora
- Acls LectureDocumento15 pagineAcls LectureVincent BautistaNessuna valutazione finora
- Treatment Strategies of Acute Myocardial Infarction Updates OnDocumento11 pagineTreatment Strategies of Acute Myocardial Infarction Updates OnLilasNessuna valutazione finora
- Emergency Protocols Book FinalDocumento137 pagineEmergency Protocols Book Finalsilverbat91Nessuna valutazione finora
- Enhanced External Counterpulsation NewDocumento11 pagineEnhanced External Counterpulsation NewRinda Putri AnggrainiNessuna valutazione finora
- Scalamogna Et Al. 2022 - CRM - IsAR-CALC-2 DesignDocumento6 pagineScalamogna Et Al. 2022 - CRM - IsAR-CALC-2 DesignPraveenVeeraNessuna valutazione finora
- Rsud Abdul Wahab Sjahranie Samarinda: Case Report Acute Myocardial Infraction With ST Elevation Cardiogenic ShockDocumento16 pagineRsud Abdul Wahab Sjahranie Samarinda: Case Report Acute Myocardial Infraction With ST Elevation Cardiogenic ShockYusty AdNessuna valutazione finora