Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Massive Transfusion Protocol 9-1-10
Caricato da
weings01Descrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Massive Transfusion Protocol 9-1-10
Caricato da
weings01Copyright:
Formati disponibili
Attending or designee activates the Massive Transfusion Protocol (MTP) by calling the
blood bank. If the patient’s medical record number (MRN) is available, it should be given
to the blood bank staff during this phone call, otherwise it MUST accompany the staff
that picks up the first delivery.
Blood bank begins preparation of Delivery #1 immediately with the goal that it is
packaged and ready to be handed to the staff at the time of pickup.
The treating team will send staff to pick up each delivery. This staff member need not be
a physician, but can be any staff member with a EHC ID so long as they have a physician
or licensed independent practitioner (LIP)-signed massive transfusion form with them
that includes the patient name, MRN, age, and sex (preferably with a patient sticker). A
new MTP form is needed for each pickup.
The treating team should make every effort to have at least one and preferably two type
and screen specimens drawn as soon as possible. If at all possible, these sample(s) should
accompany the staff member who is picking up delivery #1. Plasma will not be thawed
until a sample is available.
At some point in the patient’s treatment course, the attending physician or designee will
call blood bank and tell them to “trigger part two.” This will trigger preparation of the
second delivery. Four units of Plasma will be placed in the thawing bath and the rest of
delivery # 2 will be prepared. In some patients this will occur during the initial call to
activate the MTP (e.g. a patient in traumatic arrest or peri-arrest). In other patients, the
team may wait to see the response to delivery #1 before triggering part two.
If the patient already has packed red blood cells available (e.g. a Surgery or OB/Gyn
patient in the operating room with type and crossed units in the OR refrigerator), the
treatment team may skip delivery 1 and immediately “trigger” delivery two.
Once part II is triggered, the MTP dictates that as soon as a delivery is picked up, the next
one will be prepared by the blood bank staff. This will continue until the MTP is
cancelled by the attending physician or designee. In some cases during rapid use of
products and since Plasma currently takes ~ 30 minutes to thaw, the blood bank should
already be thawing Plasma for future deliveries based on the speed of pick-ups and
communication with the clinicians.
If Plasma is not already thawed at the time of the second delivery, 1 bottle of PCC may
be substituted. If PCC is used, Plasma should still be thawed to prepare for subsequent
deliveries.
Blood Bank will continue to prepare shipment packs # 2-7 as described below until
notified that MTP has been discontinued. If more than 7 deliveries are needed, then the
protocol should start again at delivery # 3. All unused blood products are returned to the
Blood Bank as soon as possible.
Revision 10/3/2010 Page 1 of 4
All products should be transfused with a Hotline or Level I device if possible.
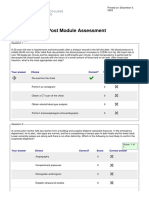
Deliveries
One 4 Units PRBC
Two 4 Units PRBC, 4 Units Plasma
Three 4 Units PRBC, 4 Units Plasma, 1 Donor Pack Platelets
Four 4 Units PRBC, 4 Units Plasma, 10 units Cryoprecipitate
Five 4 Units PRBC, 4 Units Plasma
Six 4 Units PRBC, 4 Units Plasma, 1 Donor Pack Platelets
Seven 4 Units PRBC, 4 Units Plasma, 10 units Cryoprecipitate
(If units are required past delivery 7, start back at delivery 3)
Note: Plasma can refer to FFP, FP24, or Thawed Plasma
Revision 10/3/2010 Page 2 of 4
Primary Indications
Adult patients requiring > 4 units of PRBCs in first hour of resuscitation (In other
words, patients who still need further resuscitation after Part I of the EHC
Massive Transfusion Protocol)
Adult patients who in the Attending’s opinion, have a high likelihood of requiring
transfusion of >10 units of PRBCs within the first 12-24 hours of resuscitation.
Examples of these patients include, but are not limited to:
o Traumatic Arrest or peri-arrest
o Massive blood loss with profound hemorrhagic/hypovolemic shock
o Unstable patients with anticipated massive blood loss
o Ongoing or uncontrollable gastrointestinal hemorrhage
Any patient who in the Attending’s judgment will benefit from Massive transfusion
protocol
Secondary Clinical Parameters that may Indicate the Need
for Massive Transfusion
ABC Score1,2
Penetrating Mechanism
Systolic Blood Pressure ≤ 90 mm Hg
Heart Rate ≥ 120 bpm
Positive FAST abdominal views
If 2 or more of the above are present, consider activating part one of the protocol
(Score of 2 predicts 38% chance of requiring massive transfusion, 3 predicts 45%, 4 predicts 100%)
TASH Score3
Systolic blood pressure <100 mm Hg
Heart rate >120
Hemoglobin <7 g/dL
Positive FAST Exam with hemodynamic instability
Complex long bone and/or pelvic fracture
Base excess < - 10 mmol/L
INR > 1.5 during resuscitation period
The more of these parameters that are present, the higher the likelihood that the
patient will require massive transfusion.
1
Nunez et al. Early Prediction of Massive Transfusion in Trauma: Simple as ABC (Assessment of Blood
Consumption) J Trauma 2009;66:346-352
2
J Trauma 2010;69(1 Supp):S33
3
Yucel et al. Trauma Associated Severe Hemorrhage (TASH)-Score. J Trauma 2006;60:1228-1236.
Revision 10/3/2010 Page 3 of 4
Obstetric Indications
Bleeding Placental Abruption
Bleeding Placenta Previa
Uterine Rupture
Placenta Accreta
Clinical Suspicion of DIC or Consumptive Coagulopathy
Estimated Blood Loss > 1500 ml
Any patient in the opinion of the obstetric physician or the obstetric
anesthesiologist who may require a transfusion of > 4 units of RBCs
Revision 10/3/2010 Page 4 of 4
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Incorrect - Right Answer: True: CorrectDocumento10 pagineIncorrect - Right Answer: True: CorrectAhmed - Sawalha100% (2)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- BDMS Trauma Algorithm Version 2.0Documento32 pagineBDMS Trauma Algorithm Version 2.0Aungkhena Noomnim100% (2)
- Atls Pre Test SolvedDocumento18 pagineAtls Pre Test SolvedDr.Mukesh KumarNessuna valutazione finora
- 013395417X Handouts ch01Documento6 pagine013395417X Handouts ch01inamNessuna valutazione finora
- Traumatic Brain InjuryDocumento3 pagineTraumatic Brain InjuryJill Eizavel BertisNessuna valutazione finora
- Advanced Trauma Life Support Update 2019 PDFDocumento20 pagineAdvanced Trauma Life Support Update 2019 PDFMayra HernandezNessuna valutazione finora
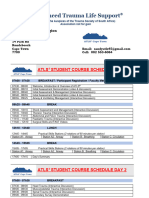
- 2021 Cape Town Atls Course ScheduleDocumento2 pagine2021 Cape Town Atls Course Schedulermullah23Nessuna valutazione finora
- Syllabus For EMT BasicDocumento10 pagineSyllabus For EMT BasicMichael B. San Juan100% (1)
- Glasgow Coma Scale GCSDocumento4 pagineGlasgow Coma Scale GCScardiacanesthesiaNessuna valutazione finora
- GREY BOOK August 2022 75th EditionDocumento155 pagineGREY BOOK August 2022 75th EditionMohamed AbdelmoniemNessuna valutazione finora
- Chapter 17 First AidDocumento104 pagineChapter 17 First AidMeg PNessuna valutazione finora
- TriageDocumento37 pagineTriagekyuleen05Nessuna valutazione finora
- A3 Mortality 2023-1Documento39 pagineA3 Mortality 2023-1marvie barbosaNessuna valutazione finora
- Acute Coronary Syndrome: History and Clinical Assessment Suggest ACSDocumento12 pagineAcute Coronary Syndrome: History and Clinical Assessment Suggest ACSginongNessuna valutazione finora
- Basic First Aid & CPR - A Guide: Indian Association of Occupational Health (IAOH)Documento6 pagineBasic First Aid & CPR - A Guide: Indian Association of Occupational Health (IAOH)Sandeep KumarNessuna valutazione finora
- Assessment-Task-1 SolutionDocumento29 pagineAssessment-Task-1 SolutionMirajur Rahman 1722007Nessuna valutazione finora
- Assisting in Endotracheal SuctioningDocumento38 pagineAssisting in Endotracheal SuctioningMargarita Limon BalunesNessuna valutazione finora
- Basic Life Support For Healthcare Providers (BLS) : Presented By: Youssef Youssef RT Respiratory Therapy DepartementDocumento43 pagineBasic Life Support For Healthcare Providers (BLS) : Presented By: Youssef Youssef RT Respiratory Therapy Departementkurt94764Nessuna valutazione finora
- Airway and Ventilatory ManagementDocumento24 pagineAirway and Ventilatory ManagementIma AriyaniNessuna valutazione finora
- Mortality July 2023Documento40 pagineMortality July 2023Tazin Ahmed AdnanNessuna valutazione finora
- Askep Shock Sepsis, AnafilaktikDocumento28 pagineAskep Shock Sepsis, AnafilaktikTomi KurniaNessuna valutazione finora
- Emergency Road Accident TrainingDocumento53 pagineEmergency Road Accident TrainingSubho SamantaNessuna valutazione finora
- DayaramDocumento15 pagineDayaramLANKAPATRUDU6772Nessuna valutazione finora
- Apache Tears Apache Tears Apache TearsDocumento1 paginaApache Tears Apache Tears Apache TearscanmyutNessuna valutazione finora
- Crash Cart Supplies and DrugsDocumento3 pagineCrash Cart Supplies and DrugsShrutiNessuna valutazione finora
- First AidDocumento5 pagineFirst AidDencio Jr. Gosing CayatNessuna valutazione finora
- BLS ChokingDocumento19 pagineBLS ChokingBernadette ArrojoNessuna valutazione finora
- Acls ExamDocumento42 pagineAcls ExamScribdTranslationsNessuna valutazione finora
- PBL Report Traumatology: Group 6Documento42 paginePBL Report Traumatology: Group 6anthy putrisriyantiNessuna valutazione finora
- Clinical Summary: Mark Agas, M.DDocumento1 paginaClinical Summary: Mark Agas, M.DMark DungoNessuna valutazione finora