Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
B Hand Out Care of High Risk Newborn
Caricato da
Lecery Sophia WongTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
B Hand Out Care of High Risk Newborn
Caricato da
Lecery Sophia WongCopyright:
Formati disponibili
HAND-OUT (READ AND REVIEW)
B. NURSING CARE OF THE HIGH RISK NEWBORN
ASSESSMENT:
1. APGAR score- provides immediate assessment for the need of resuscitation; done in
1 & 5 minutes of life. It has five parameters : Skin color, Respiration, Cardiac rate, Muscle
tone, reflex irritability
2. Ballatd’s Scoring – assesses the age of gestation of the newborn with 2 components:
PRIORITY NEEDS OF THE NEWBORN:
1. Initiation of Respiration- 40-60/min
- Most deaths occurring during the first 48 hours after birth result from the newborn’s
inability to maintain adequate respirations. If he survives, the child may experience
residual neurologic difficulties because of cerebral hypoxia. Prompt and thorough care
is necessary for effective intervention
- Sneezing, coughing are mechanism to clear the airway. A vigorous , strong cry is a proof
that lung expansion is good because vocal sounds are produced by a free flow of air
- Efforts to prevent hypothermia by wiping the baby dry will help the newborn initiate and
sustain respiratory effort and prevent acidosis
- An infant who breathes spontaneously but then cannot sustain effective respirations
may need oxygen by bag and mask to aid lung expansion at a rate of 40-60 compressions
per minute.
- An infant with difficulty maintaining respirations should be placed under a radiant warmer
and position on his back with the head of the bed elevated approximately 15 degrees.
This would allow the abdominal contents to fall away from the diaphragm and allow
additional breathing space
- If respiratory depression appears to be related to the administration of a narcotic such
as morphine sulfate, Demerol to the mother during labor, a narcotic antagonist may be
given, NALOXONE (Narcan) injected into an umbilical vessel or intramuscularly into the
thigh.
- Note: If with Meconium aspiration syndrome, do not give oxygen under pressure
because it will push the meconium further , may give oxygen by face mask.
- An increasing RR, is often a first sign of obstruction or or respiratory compromise. Check
for chest indrawing or retractions (inward sucking of the anterior chest wall on inspiration).
This reflects the difficulty of the newborn to draw in air.
- An adequate respiration will lead to the closure of the patent ductus arteriosus and
foramen ovale (open structures during fetal circulation)
2. Establish extrauterine circulation- 120-160 beats /minute
- If no audible heartbeat or 80 beats/min, do closed chest massage at a rate of 100x/min,
lung ventilation at arate of 30x/min
- Palpate femoral pulse to check return of pulse
- If heart sound does not resume above 80 beats/min after 30 secs of cardiac
compression, 0.3 ml/kg of Epinephrine may be given endotracheally to stimulate cardiac
function
3. Maintaining Fluid and Electrolyte Balance
- Note for Hypoglycemia- < 40 mg/dl. There is increase energy expenditure to initiate
breathing. Early breastfeeding would help maintain calorie needs.
- Dehydration may result from insensible fluid loss from rapid respiration. It may be
monitored by urine output and urine specific gravity measures. An output of < 2ml/kg/hr
or a Specific gravity of >1.015-1.020 suggests inadequate fluid intake.
4. Regulating temperature – maintained at 36.5 C or 97.8 F (97-99.5F)
(Process of Heat Loss: Evaporation, Conduction, Convection, Radiation)
- Keep the NB in a neutral temperature environment. Rationale: Cold temp increases
metabolism to warm body cells; Hot temp decrease metabolism to cool their body
- Wipe baby dry and cover head with bonnet.
- Do Kangaroo Mother Care- skin to skin contact
- Radiant heat sources are kept at 36.5 C
5. Establishing Adequate Nutritional Intake
- Infant should not lose > 10% of bodyweight
- All infants should be breastfed. Preterm infants with good sucking can be breastfeed
early.
- Intravenous feeding is given to infants who suffered from asphyxia
- Gavage feeding may be given : may use expressed breastmilk
6. Establishing waste elimination
- Voids 6-8 /day; defecates 2-3x/day
- Infants void within 24 hours of birth, but preterm infants may void later as a result of
procedures and resuscitation, their blood pressure are not adequate to optimally supply
their kidneys.
- Immature infants may pass stool later than term infants because their stool has not yet
reached the end of the intestine at birth
7. Preventing Infection
- Infection stresses the immature immune system of the newborn
- Review labor and delivery history; presence of prolonged labor and rupture of
membranes because this poses a risk to infection
-Common causes: TORCH infections, Group B streptococcus (Septicemia), Candidiasis
(NB oral thrush), Herpes infections, Gonorrhea & chlamydial infections (Opthalmia
Neonatorum)
- Prevent skin breakdown, care of cord stump: Handwashing, no binders, clean with clean
water
- Observe handwashing to reduce infection transmission
8. Establishing Parent–Infant Bonding
> Be certain that the parents of a high-risk newborn are kept informed of what is
happening during resuscitation at birth.
> They should be able to visit the special nursing unit to which the child is admitted as
often as they choose, and, after washing and gowning, hold and touch their child.
1. POOR APGAR SCORE
(REVIEW THE APGAR SCORING & ITS INTERPRETATION – 5 PARAMETERS:
COLOR,
CR, RR, REFLEX IRRITABILITY , MUSCLE TONE,
INTERPRETATION: 0-3 =SEVERE DISTRESS; 4-6 = MODERATE DISTRESS; 7-10
WELL ADJUSTED TO EXTRAUTERINE LIFE
CAUSES:
A. Hypothermia- contributes to sluggish circulation added to the immaturity of the
peripheral circulation , this leads to cyanosis or acrocyanosis altering the color of
the skin
B. Congenital Defects/ malformations - presence of congenital heart problem such
as Transposition of the great vessels leading to cyanosis altering the color of the
skin
C. Altered respiration/Poor gas exchange
REF. e- book- Pilliteri
/ecferrer
Potrebbero piacerti anche
- CARE OF THE NEWBORN - ncm107Documento6 pagineCARE OF THE NEWBORN - ncm107Jasmin NatocNessuna valutazione finora
- The NeonatesDocumento117 pagineThe NeonatesAirene AalaNessuna valutazione finora
- Neonatal ResuscitationDocumento15 pagineNeonatal Resuscitationpriyanka88% (8)
- Newborn Resuscitation EssentialsDocumento34 pagineNewborn Resuscitation EssentialsVarna MohanNessuna valutazione finora
- Immediate Nursing Care of The NewbornDocumento29 pagineImmediate Nursing Care of The NewbornDrei Lanuzo100% (1)
- Immediate Newborn Care and Breastfeeding InitiationDocumento45 pagineImmediate Newborn Care and Breastfeeding InitiationRouquia ManzoorNessuna valutazione finora
- 2.1A Newborn Care: Emilio Aguinaldo College - School of MedicineDocumento6 pagine2.1A Newborn Care: Emilio Aguinaldo College - School of MedicineBea SamonteNessuna valutazione finora
- Neonatal ResuscitationDocumento16 pagineNeonatal ResuscitationPrecilla C. Stephen100% (3)
- New Born CareDocumento17 pagineNew Born CareHarrison Tallod100% (1)
- Newborn CareDocumento120 pagineNewborn CareMike CalipayanNessuna valutazione finora
- Nursing Care of High-Risk NewbornsDocumento83 pagineNursing Care of High-Risk NewbornsChari RivoNessuna valutazione finora
- Care of The Newborn PDFDocumento5 pagineCare of The Newborn PDFzhai bambalan100% (2)
- Nursing Care of The High Risk NewbornDocumento8 pagineNursing Care of The High Risk NewbornFebie GonzagaNessuna valutazione finora
- Apgar and BallardDocumento16 pagineApgar and Ballardcarlos ponceNessuna valutazione finora
- Newborn CareDocumento49 pagineNewborn CareJohn Mark PocsidioNessuna valutazione finora
- Immediate Newborn Care Updates at San Isidro CollegeDocumento11 pagineImmediate Newborn Care Updates at San Isidro CollegeMay Princes Torregosa Abucejo100% (1)
- Newborn CareDocumento51 pagineNewborn CareHurley ReefNessuna valutazione finora
- Newborn Care: Essential Steps for Healthy BabiesDocumento42 pagineNewborn Care: Essential Steps for Healthy BabiesGurpreet kaur100% (9)
- Essential Newborn Care GuideDocumento120 pagineEssential Newborn Care Guidejuly3ciaNessuna valutazione finora
- Newborns Undergo Profound Physiologic Changes at The Moment of BirthDocumento8 pagineNewborns Undergo Profound Physiologic Changes at The Moment of BirthUri ELNessuna valutazione finora
- Newborn ResuscitationDocumento32 pagineNewborn ResuscitationVarna MohanNessuna valutazione finora
- NEONATAL RESUSCITATION GUIDELINESDocumento5 pagineNEONATAL RESUSCITATION GUIDELINESDoc Prince CaballeroNessuna valutazione finora
- Newborn Lecture HandoutDocumento57 pagineNewborn Lecture HandoutChesca LayosaNessuna valutazione finora
- Chapter 18: Nursing Care of A Family With A NewbornDocumento32 pagineChapter 18: Nursing Care of A Family With A NewbornAlyssaGrandeMontimor100% (1)
- Immediate Newborn Care (Autosaved)Documento183 pagineImmediate Newborn Care (Autosaved)mftaganasNessuna valutazione finora
- Neonatal Danger SignsDocumento6 pagineNeonatal Danger Signsmarkus_danusantosoNessuna valutazione finora
- Neonatal Resuscitation: Vineetha.T 1 Year MSC NursingDocumento106 pagineNeonatal Resuscitation: Vineetha.T 1 Year MSC NursingVineetha ThachedathNessuna valutazione finora
- Neonatal ResuscitationDocumento15 pagineNeonatal ResuscitationAmruta GadeNessuna valutazione finora
- Newborn Nursing CareDocumento12 pagineNewborn Nursing CareedenpearlcastilloNessuna valutazione finora
- Essential Intrapartum and Newborn Care (Einc) 2Documento8 pagineEssential Intrapartum and Newborn Care (Einc) 2Alphine DalgoNessuna valutazione finora
- NEWBORNDocumento212 pagineNEWBORNNicole MapiliNessuna valutazione finora
- PEDIAPrelims - 2. Care of The Newborn 1 (First 24 Hours To Vital Signs)Documento7 paginePEDIAPrelims - 2. Care of The Newborn 1 (First 24 Hours To Vital Signs)RenatoCosmeGalvanJuniorNessuna valutazione finora
- Immediate Care of NewbornsDocumento30 pagineImmediate Care of NewbornsKome Ngambe RandyNessuna valutazione finora
- NB Nursing DiagnosisDocumento2 pagineNB Nursing Diagnosisnursingmvd92% (13)
- NewbornDocumento193 pagineNewbornKenneth Myro Garcia100% (1)
- Thermoregulation For The Maintenance of BodyDocumento2 pagineThermoregulation For The Maintenance of BodyVince Matt BaguioNessuna valutazione finora
- Assessment Scientific Basis Plan of Care Intervention With Rationale Evaluation Subjective: IndependentDocumento16 pagineAssessment Scientific Basis Plan of Care Intervention With Rationale Evaluation Subjective: IndependentAbdullah Mascardo BarabagNessuna valutazione finora
- Neonatal ResuscitationDocumento5 pagineNeonatal Resuscitationabdirahiim ahmedNessuna valutazione finora
- New Born Care 1Documento12 pagineNew Born Care 1Tsuyoshi BangNessuna valutazione finora
- New Born Care 1Documento12 pagineNew Born Care 1gilbertgarciaNessuna valutazione finora
- Immediate Care of The NewbornDocumento11 pagineImmediate Care of The NewbornHannahKarizaNessuna valutazione finora
- NCM 107 SL Finals EincDocumento7 pagineNCM 107 SL Finals EincAngel DumlaoNessuna valutazione finora
- Immediate Care of The NewbornDocumento99 pagineImmediate Care of The NewbornVializa Abanilla BuladoNessuna valutazione finora
- MCN FinalsDocumento40 pagineMCN Finalsmolderoirish600Nessuna valutazione finora
- New Born ResuscitationDocumento49 pagineNew Born ResuscitationdivyamuthyalaNessuna valutazione finora
- 10 LPDocumento20 pagine10 LPFayad AlmohamedNessuna valutazione finora
- Birth AsphyxiaDocumento10 pagineBirth Asphyxiasarita Singh MaharjanNessuna valutazione finora
- NCM 107 Care of The Newborn Guide QuestionDocumento5 pagineNCM 107 Care of The Newborn Guide QuestionMiguel LigasNessuna valutazione finora
- Newborn Acute Conditions GuideDocumento46 pagineNewborn Acute Conditions GuideCamille Joy BaliliNessuna valutazione finora
- Resucition 2Documento8 pagineResucition 2sudeepminz15Nessuna valutazione finora
- 39 Neonatal ResuscitationDocumento38 pagine39 Neonatal ResuscitationbenNessuna valutazione finora
- Care of the NewbornDocumento6 pagineCare of the NewbornJankie Obina Alcaba100% (1)
- NeonatalresuscitationDocumento67 pagineNeonatalresuscitationfidaNessuna valutazione finora
- Care of Normal NewbornDocumento13 pagineCare of Normal NewbornTanu BhatiaNessuna valutazione finora
- Lesson (5) Neonatal ResuscitationDocumento14 pagineLesson (5) Neonatal ResuscitationDrmirfat AlkashifNessuna valutazione finora
- Baby at Risk - Koros E.k-1-1-1-1Documento132 pagineBaby at Risk - Koros E.k-1-1-1-1victorNessuna valutazione finora
- General Objecti-Wps OfficeDocumento3 pagineGeneral Objecti-Wps OfficeSumit YadavNessuna valutazione finora
- Einc-Word 054847Documento4 pagineEinc-Word 054847Jane OrsalNessuna valutazione finora
- Managing Birth Asphyxia August 2022Documento21 pagineManaging Birth Asphyxia August 2022f.abrahamNessuna valutazione finora
- The Care and Feeding of Children - A Catechism for the Use of Mothers and Children’s NursesDa EverandThe Care and Feeding of Children - A Catechism for the Use of Mothers and Children’s NursesNessuna valutazione finora
- Pediatric CAP Diagnostic and Treatment ChallengesDocumento2 paginePediatric CAP Diagnostic and Treatment ChallengesLecery Sophia WongNessuna valutazione finora
- Wong - NCP Pneumonia RedoDocumento5 pagineWong - NCP Pneumonia RedoLecery Sophia WongNessuna valutazione finora
- Wong Worksheet PediaDocumento3 pagineWong Worksheet PediaLecery Sophia WongNessuna valutazione finora
- Wong CusDocumento1 paginaWong CusLecery Sophia WongNessuna valutazione finora
- Wong - NCP Pneumonia RedoDocumento5 pagineWong - NCP Pneumonia RedoLecery Sophia WongNessuna valutazione finora
- Wong - NCP Pneumonia RedoDocumento5 pagineWong - NCP Pneumonia RedoLecery Sophia WongNessuna valutazione finora
- Case Study ONLINEDocumento2 pagineCase Study ONLINELecery Sophia WongNessuna valutazione finora
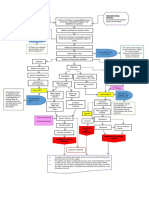
- WONG Concept MapDocumento1 paginaWONG Concept MapLecery Sophia WongNessuna valutazione finora
- WONG, LECERY C. Significance of Studying LiDocumento1 paginaWONG, LECERY C. Significance of Studying LiLecery Sophia WongNessuna valutazione finora
- The Ten Commandments and Other Biblical PassagesDocumento2 pagineThe Ten Commandments and Other Biblical PassagesLecery Sophia WongNessuna valutazione finora
- Wong - Activity Checklist Pediatric WardDocumento2 pagineWong - Activity Checklist Pediatric WardLecery Sophia WongNessuna valutazione finora
- LSCW - Hand Out - Postpartum ComplicationsDocumento2 pagineLSCW - Hand Out - Postpartum ComplicationsLecery Sophia WongNessuna valutazione finora
- Post Partum Journal (Drnur)Documento4 paginePost Partum Journal (Drnur)Lecery Sophia WongNessuna valutazione finora
- Isbar Galanza PediaDocumento1 paginaIsbar Galanza PediaLecery Sophia WongNessuna valutazione finora
- WONG, LECERY C. Significance of Studying LiDocumento1 paginaWONG, LECERY C. Significance of Studying LiLecery Sophia WongNessuna valutazione finora
- 10 Reasons To Read The BibleDocumento3 pagine10 Reasons To Read The BibleLauren CarlosIINessuna valutazione finora
- WONG BrochureCovid 19Documento2 pagineWONG BrochureCovid 19Lecery Sophia WongNessuna valutazione finora
- Pediatric CAP Diagnostic and Treatment ChallengesDocumento2 paginePediatric CAP Diagnostic and Treatment ChallengesLecery Sophia WongNessuna valutazione finora
- Wongl C - Act2-Respiratory-DisordersDocumento2 pagineWongl C - Act2-Respiratory-DisordersLecery Sophia WongNessuna valutazione finora
- Etiologic Agent: Tuberculosis Is A Disease Caused by Mycobacterium Tuberculosis. Although TB IsDocumento3 pagineEtiologic Agent: Tuberculosis Is A Disease Caused by Mycobacterium Tuberculosis. Although TB IsLecery Sophia WongNessuna valutazione finora
- WONG BrochureCovid 19Documento2 pagineWONG BrochureCovid 19Lecery Sophia WongNessuna valutazione finora
- Wong, L.C - Perioperative NursingDocumento5 pagineWong, L.C - Perioperative NursingLecery Sophia WongNessuna valutazione finora
- Wong, L.C. - Philippine Health SituationDocumento1 paginaWong, L.C. - Philippine Health SituationLecery Sophia WongNessuna valutazione finora
- That May Used in Neurological Ward: Miguelito M. GultianoDocumento32 pagineThat May Used in Neurological Ward: Miguelito M. GultianoLecery Sophia WongNessuna valutazione finora
- College Nursing Learning Contract GuideDocumento2 pagineCollege Nursing Learning Contract GuideLecery Sophia WongNessuna valutazione finora
- Wong, Lecery Sophia C. Obward BSN 2-I1 Iii. Drug Study 1. Naproxen SodiumDocumento3 pagineWong, Lecery Sophia C. Obward BSN 2-I1 Iii. Drug Study 1. Naproxen SodiumLecery Sophia WongNessuna valutazione finora
- Pediatric CAP Diagnostic and Treatment ChallengesDocumento2 paginePediatric CAP Diagnostic and Treatment ChallengesLecery Sophia WongNessuna valutazione finora
- Wong, Lecery Sophia C. Obward BSN 2-I1 Iii. Drug Study 1. Naproxen SodiumDocumento3 pagineWong, Lecery Sophia C. Obward BSN 2-I1 Iii. Drug Study 1. Naproxen SodiumLecery Sophia WongNessuna valutazione finora
- Promissory NoteDocumento1 paginaPromissory NoteLecery Sophia WongNessuna valutazione finora
- WONG TeachingCarePlanCOVID 19Documento3 pagineWONG TeachingCarePlanCOVID 19Lecery Sophia WongNessuna valutazione finora
- Byram Enteral - NutritionDocumento7 pagineByram Enteral - NutritionGrace XieNessuna valutazione finora
- ParestesiDocumento1 paginaParestesiYolanda YiNessuna valutazione finora
- Oligospermia Case StudyDocumento7 pagineOligospermia Case StudyMariah GolzNessuna valutazione finora
- Pathology Lecture 7 - LiverDocumento11 paginePathology Lecture 7 - Livercgao30Nessuna valutazione finora
- MCPS COVID-19 Simplified Decision Making ModelDocumento2 pagineMCPS COVID-19 Simplified Decision Making ModelNBC MontanaNessuna valutazione finora
- Food Safety: HABC Level 2 Award in Food Safety in Catering (QCF)Documento3 pagineFood Safety: HABC Level 2 Award in Food Safety in Catering (QCF)Caroline FrostNessuna valutazione finora
- Recommended Texts / Useful Resources For Psychiatry TraineesDocumento5 pagineRecommended Texts / Useful Resources For Psychiatry TraineesTemesgen EndalewNessuna valutazione finora
- Companion Animal Parasitology: A Clinical Perspective: Peter J. IrwinDocumento13 pagineCompanion Animal Parasitology: A Clinical Perspective: Peter J. IrwinAngela SanchezNessuna valutazione finora
- Restorative dentistry for worn teethDocumento7 pagineRestorative dentistry for worn teethSohrab KhanNessuna valutazione finora
- Tranexamic Acid Drug StudyDocumento3 pagineTranexamic Acid Drug Studyswitchlers anneNessuna valutazione finora
- Hearing ImpairementDocumento8 pagineHearing ImpairementMARY KENNETH SILVOSANessuna valutazione finora
- Alyssa Macdonald - Smith - Career Options UpdatedDocumento2 pagineAlyssa Macdonald - Smith - Career Options Updatedapi-529186757Nessuna valutazione finora
- CT Scan: Preperation and ProceduresDocumento8 pagineCT Scan: Preperation and ProceduresAj PlacidoNessuna valutazione finora
- Module 17 Practice CPC Exam PDFDocumento54 pagineModule 17 Practice CPC Exam PDFNitish Rajani Chunilal Metha74% (31)
- Hiv Testing Laboratory LawsDocumento41 pagineHiv Testing Laboratory LawsMarian GarciaNessuna valutazione finora
- Lot 6 Block 6 Sta. Catalina Homes Tabing IlogDocumento12 pagineLot 6 Block 6 Sta. Catalina Homes Tabing IlogAina De LeonNessuna valutazione finora
- Fever in Pregnancy and Its Maternal and Fetal Outcomes: Original Research ArticleDocumento5 pagineFever in Pregnancy and Its Maternal and Fetal Outcomes: Original Research ArticleKeerthanaNessuna valutazione finora
- Phase I and Phase Ii Clinical TrialsDocumento41 paginePhase I and Phase Ii Clinical Trialsrahil_khan797Nessuna valutazione finora
- 2015 ESC Guidelines For The ManagementDocumento59 pagine2015 ESC Guidelines For The ManagementSri WahyuniNessuna valutazione finora
- Sheehan SyndromeDocumento6 pagineSheehan SyndromeArvie TagnongNessuna valutazione finora
- Memorandum of Agreement - Brgy and SalisDocumento3 pagineMemorandum of Agreement - Brgy and SalisBARANGAY MOLINO IINessuna valutazione finora
- Awareness During General Anesthesia Concepts andDocumento8 pagineAwareness During General Anesthesia Concepts andR KNessuna valutazione finora
- Preboard Exam NP 4 MsDocumento20 paginePreboard Exam NP 4 MsDavid Lopez50% (2)
- Dental Trauma WorksheetDocumento2 pagineDental Trauma WorksheetSteliana CaramanNessuna valutazione finora
- Woman With DysuriaDocumento26 pagineWoman With DysuriaAlFi KamaliaNessuna valutazione finora
- Fluoroquinolone-Associated Tendon-Rupture: A Summary of Reports in The Food and Drug Administration's Adverse Event Reporting SystemDocumento9 pagineFluoroquinolone-Associated Tendon-Rupture: A Summary of Reports in The Food and Drug Administration's Adverse Event Reporting SystemMadalinaMadaNessuna valutazione finora
- Parts A and B Should Be Answered in Separate Answer Books. All Questions Carry Equal MarksDocumento13 pagineParts A and B Should Be Answered in Separate Answer Books. All Questions Carry Equal MarksjishnuchandNessuna valutazione finora
- Monthly Accomplishment ReportDocumento11 pagineMonthly Accomplishment ReportAlexandria P. OrcajadaNessuna valutazione finora
- Unit 2A - Course NotesDocumento162 pagineUnit 2A - Course Notesrashid zaman100% (5)
- Drugs and Cosmetics ActDocumento29 pagineDrugs and Cosmetics ActRanvidsNessuna valutazione finora