Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Pituitary Gigantism: A Case Series From Hospital de San José (Bogotá, Colombia)
Caricato da
Naila SalsaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Pituitary Gigantism: A Case Series From Hospital de San José (Bogotá, Colombia)
Caricato da
Naila SalsaCopyright:
Formati disponibili
original article
Pituitary gigantism: a case
series from Hospital de San
José (Bogotá, Colombia)
1 Head of the Endocrinology
William Rojas García1
http://orcid.org/0000-0001-7120-9432 Unit, Hospital de San José;
associate professor, Fundación
Henry Tovar Cortes2 Universitaria de Ciencias de la
http://orcid.org/0000-0003-0591-2562
Salud, Bogotá, DC, Colombia
Andrés Florez Romero3 2 Hospital de San José;
http://orcid.org/0000-0001-6946-7993 assistant professor, Fundación
Universitaria de Ciencias de la
Salud, Bogotá, DC, Colombia
ABSTRACT 3 Hospital de San José,
Bogotá, DC, Colombia
Introduction: Gigantism is a rare pediatric disease characterized by increased production of growth
hormone (GH) before epiphyseal closure, that manifests clinically as tall stature, musculoskeletal
abnormalities, and multiple comorbidities. Materials and methods: Case series of 6 male patients with
gigantism evaluated at the Endocrinology Service of Hospital de San José (Bogotá, Colombia) between 2010
and 2016. Results: All patients had macroadenomas and their mean final height was 2.01 m. The mean age
at diagnosis was 16 years, and the most common symptoms were headache (66%) and hyperhidrosis (66%).
All patients had acral changes, and one had visual impairment secondary to compression of the optic chiasm.
All patients underwent surgery, and 5 (83%) required additional therapy for biochemical control, including
radiotherapy (n = 4, 66%), somatostatin analogues (n = 5, 83%), cabergoline (n = 3, 50%), and pegvisomant
(n = 2, 33%). Three patients (50%) achieved complete biochemical control, while 2 patients showed IGF-1
normalization with pegvisomant. Two patients were genetically related and presented a mutation in the aryl
hydrocarbon receptor-interacting protein (AIP) gene (pathogenic variant, c.504G>A in exon 4, p.Trp168*), Correspondence to:
fulfilling the diagnostic criteria of familial isolated pituitary adenoma. Conclusions: This is the largest case Andrés Florez Romero
Hospital de San José, Bogotá,
series of patients with gigantism described to date in Colombia. Transsphenoidal surgery was the first-choice DC, Colombia Street 10 #. 18-
procedure, but additional pharmacological therapy was usually required. Mutations in the AIP gene should be 75
considered in familial cases of GH-producing adenomas. Arch Endocrinol Metab. 2019;63(4):385-93 andresflorez25@hotmail.com
Received on Jan/3/2018
Accepted on Apr/24/2019
Keywords
Pituitary diseases; gigantism; growth hormone; pituitary neoplasms; acromegaly DOI: 10.20945/2359-3997000000150
INTRODUCTION treatment for gigantism is transsphenoidal surgery
G igantism is a rare pediatric disease, with an incidence of 8
(TSS) (4). However, complete remission of the disease
is not usually achieved with surgical intervention alone
to 11 cases per million individuals per year.
This disease is characterized by increased production of and pharmacological therapy becomes necessary (2,5-
growth hormone (GH) when the epiphyses are still open, 7), of which somatostatin analogues (SSA) is the most
and in most cases is secondary to a pituitary adenoma (1). common. If no response is obtained with SSAs,
Gigantism can occur sporadically or have a hereditary dopamine receptor agonists (cabergoline) or GH
component (2); in a case series by Rostomyan and cols. receptor antagonists (pegvisomant) can be added (8-
(3), a genetic cause was identified in 46% of the cases, of 10). In cases that fail to respond to surgery and
which the most common was a mutation in the pharmacological treatment, radiotherapy is used;
hydrocarbon receptor-interacting protein (AIP) gene however, the risk of hypopituitarism should be taken
(28%), followed by X-linked acrogigantism (X-LAG; into account (8).
10%). McCune-Albright syndrome (5%), Carney The purpose of this study is to present 6 cases of
Copyright © AE&M all rights reserved.
complex (1%), and multiple endocrine neoplasia type 1 gigantism treated in Colombia, including a 6-year
(1%) are less common causes of gigantism (3). The main follow-up and treatment outcomes. We also present the
symptom of the disease is abnormal accelerated growth clinical history of 2 patients with gigantism secondary
affecting the musculoskeletal system associated with to familial isolated pituitary adenoma (FIPA) and AIP
some other comorbidities (1). The first-choice mutation.
Arch Endocrinol Metab. 2019;63/4 385
Pituitary gigantism: a case series
MATERIALS AND METHODS using the Colombian height and weight chart (11).
We present a review of 6 cases of gigantism secondary
Biochemical and imaging diagnostic tests included
increased serum GH and insulin-like growth factor-1
to pituitary adenomas, managed at the Endocrinology
(IGF-1) levels and evidence of a pituitary adenoma in
Department of Hospital de San José (Bogotá, Colombia),
the sella turcica on magnetic resonance imaging (MRI)
a tertiary referral center, between January 2010 and
(2,3). Since no standard criteria are available to define
December 2016. At this institution, we see an average of
controlled disease in patients in gigantism, the
110 cases of acromegaly per year. All patients provided a
biochemical diagnostic criteria for acromegaly were
written informed consent for picture release. Data,
used for follow-up (12), i.e., IGF-1 in the normal range
including medical history and laboratory results, were
and GH level below 1 ng/mL.
collected retrospectively. Additional information was
obtained directly from the patients.
AIP testing was requested from all patients but was RESULTS
only obtained from patients #1 and #5 (Table 1), In all, 6 cases of gigantism were managed at our Unit
confirming a diagnosis of FIPA with AIP mutation. Total according to established criteria between 2010 and 2016.
genomic DNA extraction was performed from venous The patients were all male and had a mean age at
blood samples using conventional techniques, and an symptom onset of 12.3 years. Their mean age at diagnosis
analysis of the complete AIP gene coding sequence was 16 years, and their mean final height was 2.01 meters
(exons 1-6) was done including all exon-intron junctions. (m). All patients had pituitary macroadenomas. The
The exon sequences were compared against the GenBank tumor sizes are described in Table 1. No record is
accession number NM_003977.2, with the A of the ATG available regarding the tumor sizes of patients #3 and #5
translation initiation codon in position 1. To test for the since they arrived at our center after undergoing surgical
c.504G>A (p.Trp168*) variant of the AIP gene, total procedures at another institution, so initial MRI reports
genomic DNA was extracted from venous blood samples were not available. The most common symptoms were
following a conventional technique. A conventional PCR headache and hyperhidrosis, which were present in 4
assay was developed to amplify exon 4 of the AIP gene patients, followed by acroparesthesia in 3 patients, and
(wild type sequence, ENST00000279146) from DNA in arthralgia and fatigue in 2 patients each.
both cases. The amplified product was purified and All 6 patients showed acral changes. One patient
sequenced. (patient #1) had visual impairment secondary to
The diagnosis of gigantism was established based compression of the optic chiasm by the adenoma. Only 2
on a height above 2 or more standard deviations for patients (#1 and #5), had a family history of tall stature or
age (> 97th percentile), or a final height greater than 2 other endocrine disorders. Table 1 presents a summary of
standard deviations above the general population, the main clinical and laboratory findings of each patient.
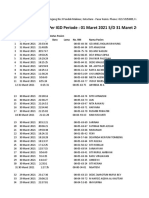
Table 1. Demographic characteristics of patients with gigantism
Age at Age at Final Height Height Z-score Z-score Body BMI Tumor
symptom - mean
Patient Gender diagnosis height - father population weight (kg/ size ST RT MED
onset mother parental
(years) (meters) (meters) mean (kg) m2) (mm)
(years) (meters) height
1 M 12 12 1.96 1.71 NA 4.2 NA 107 27.8 5 x 17.3 TSS YES LAR,
x 29 (2)1 PEG
2 M 13 21 2.2 1.68 1.68 5.9 6.17 108 22.3 18 x 20 FC NO NA
x 20
3 M 11 11 2.1 1.58 1.5 4.5 6.69 103 23.3 NA FC YES OCT,
CAB
4 M 14 17 1.93 1.7 1.5 2.26 3.63 75 20.35 16 x 15 TSS NO OCT
x 17
Copyright © AE&M all rights reserved.
5 M 14 23 1.91 NA 1.53 1.98 NA 122 33 NA TSS YES NO
6 M 10 12 2 1.65 1.5 3.2 2.78 107 27.2 25 x 20 TSS YES LAR,
x 20 (2)1 PEG
CAB: Cabergoline, FC: Frontal craniotomy, LAR: Lanreotide, M: Male, MED: Medical treatment, NA: Not available, OCT: octreotide long-acting (LAR), PEG: Pegvisomant, ST: Surgical treatment, RT:
Radiotherapy, TSS: Transsphenoidal surgery. 1. Number of surgeries performed.
386 Arch Endocrinol Metab. 2019;63/4
Pituitary gigantism: a case series
All 6 patients were initially managed with surgical radiotherapy (patients #1 and #6). One patient (#4),
resection of the tumor, including TSS in 4 patients (#1, who received treatment with TSS and octreotide LAR,
#4, #5, and #6) and frontal craniotomy in 2 patients (#2 showed fluctuating IGF-1 levels, but since he was
and #3). Two patients required a second surgical asymptomatic, pegvisomant was not recommended.
intervention via TSS (patients #1 and #6). Patient #5 interrupted the follow-up at our institution.
Immunohistochemistry confirmed exclusive production Four patients (#1, #3, #4, and #6) underwent regular
of GH by the adenomas in all patients, and none of the monitoring for more than 3 years, and their IGF-1
patients had increased serum prolactin. values are presented in Table 2. Patient #3 started
All 6 patients had only partial improvement of following up at our center after undergoing surgical
symptoms after surgery and required other treatments. intervention, radiotherapy, and pharmacological
Four patients (#1, #3, #5, and #6) received radiotherapy, treatment at another institution, therefore, his initial
and 5 required additional medical management with IGF-1 levels at our institution were normal.
SSAs (3 patients with lanreotide Autogel and 2 with Regarding associated comorbidities, one patient
long-acting release [LAR] octreotide). Due to the absence (#5) had class 1 obesity, 2 (#1 and #6) were
of clinical response, cabergoline was added to the therapy overweight, and one (#1) had hyperglycemia.
in 3 patients (#1, #3, #6) and pegvisomant was added to 2 Cholelithiasis was investigated with hepatobiliary
patients (#1 and #6, both at a dose of ultrasound, but none of the patients presented this
20 mg/day). comorbidity. No other comorbidities associated with
Normal GH (< 1 ng/mL) and IGF-1 levels were GH excess were found. Two patients presented
achieved in 4 patients, one after frontal craniotomy hypopituitarism (patients #1 and #3, who had thyroid
(patient #2); one after frontal craniotomy, radiotherapy, and gonadal dysfunctions, respectively).
octreotide LAR, and cabergoline (patient #3); and 2 after Figure 1 shows pictures of 5 out of the 6 patients. A
TSS, lanreotide Autogel, pegvisomant, and summary of the clinical history of the 2 patients (#1 and
Table 2. IGF-1 levels (in ng/mL) and upper limit of normal in patients followed up for more than 36 months
Months
Patient 0 6 12 18 24 30 36 42
ng/mL ULN ng/mL ULN ng/mL ULN ng/mL ULN ng/mL ULN ng/mL ULN ng/mL ULN ng/mL ULN
1 794 1.6 824 1.6 1017 2 876 1.7 1084 2.1 692 1.4 700 1.4 130 N
3 61 N 85 N 39 N 26.2 N 25.9 N
4 337 N 367 N 147 N 444 N 501 1.01 303 N 180 N 513 1.03
6 753 1.5 677 1.3 610 1.2 511 1.02 950 1.9 543 1.09 402 N 150 N
N: Normal, ULN: Upper limit of normal.
Copyright © AE&M all rights reserved.
Figure 1. Photograph of 5 of the patients. From left to right: patient 1, patient 2, patient 3, patient 5 and patient 6.
Arch Endocrinol Metab. 2019;63/4 387
Pituitary gigantism: a case series
#5) who had familial pituitary adenomas is presented during postsurgical follow-up, his cabergoline dose was
below. A genealogical tree of these patients (who increased to 2 mg weekly. A follow-up MRI after the
belonged to the same family), from whom a sample of second surgery showed a lesion of 36 x 30 x 20 mm and
the AIP gene was requested, is presented in Figure 2. optic chiasm compression (Figure 3C). Due to the
Patient 1: His symptoms began at the age of 12 years increase in tumor size and poor biochemical control,
with headache, hyperhidrosis, lower limb paresthesia, and radiotherapy was performed at the age of 14 years.
tall stature (1.74 m). His initial laboratory tests showed Pegvisomant was also initiated and cabergoline was
GH levels greater than 40 ng/mL (reference range 0-5 suspended, resulting in a decrease in IGF-1 levels and
ng/mL), IGF-1 level 794 ng/mL (reference range 111-498 control of the symptoms. A contrast MRI performed 2
ng/mL), and normal levels of TSH, free T4, FSH, LH, years after the radiotherapy is shown in Figure 3D. The
prolactin, cortisol, ACTH, and glucose. An MRI of the final height of the patient was 1.96 m. Given the
sella turcica showed an expansive lesion of 5.0 x 17.3 x occurrence of gigantism in a second-degree uncle (patient
29.0 mm compressing the optic chiasm and infiltrating the #5) and acromegaly in a second-degree aunt, an AIP gene
left cavernous sinus (Figures 3A and 3B). Monthly sequencing was requested, which showed the
lanreotide (90 mg, intramuscular) was initiated and TSS heterozygous pathogenic variant c.504G>A in exon 4
was performed at the age of 12 years. (p.Trp168*) generating a nonsense substitution of
Immunohistochemistry analysis of the adenoma was tryptophan causing a premature stop codon.
positive for GH. After surgery, the patient persisted with Patient 5: The onset of his symptoms occurred at
symptoms and acral growth and presented serum levels of the age of 14 years, manifesting as tall stature. The
GH > 40 ng/mL and IGF-1 of 1165 ng/mL; based on that, patient was diagnosed with a pituitary macroadenoma
the lanreotide dose was increased to 120 mg and at the age of 23 years and treatment with TSS was
cabergoline 0.5 mg weekly was initiated. A new MRI performed. He required radiotherapy at the age of 27
showed a residual tumor infiltrating the left cavernous years and used SSA for 1 year. Adequate biochemical
sinus, and a second TSS was performed at the age of 13 and imaging control were observed at follow-up, and
years. Due to poor biochemical control his final height was 1.91 m. Given the family history
I 87
1 2
II 67 65 62 60 59 57 53 53 51 51 51 56 45
1 2 3 4 5 6 7 8
9 10 11 12 13 14 15
G A 19 31 11 24 28 26 17 16 16 22
III 37 35 30 38 36 42 34 28 26 33 33 27 35
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23
G
IV 13 4m 13 18 3 5 3 16 13 9 9 7 3 14 12 6 5 4 4
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19
Conventions G: Gigantism
Woman A: Acromegaly
Copyright © AE&M all rights reserved.
Man M: Months
Deceased IV 4: Patient 1
(+) variant c. 504G>A (p. Trp168*) AIP gene III 7: Patient 5
X Age (years) III 13: Patient 1 – second-grade aunt
Figure 2. Genealogical family tree with mutation of the AIP gene.
388 Arch Endocrinol Metab. 2019;63/4
Pituitary gigantism: a case series
of gigantism on a second-degree nephew (patient #1) In most recent case series, there was a predominance of
and acromegaly on a second-degree female cousin, the male patients, as in the series by Nagata and cols. (Japan;
variant c.504G> A (p.Trp168*) of the AIP gene was 7 out of 13 patients [54%]) (14), Creo and Lteif (USA; 9
tested and resulted positive. The same variant was out of 13 patients [69%]) (15), Rostomyan and cols.
tested in the patient’s relatives (patient #1 and patient (Belgium; 163 out of 208 patients [78%]) (3), Patt and
#5, who was diagnosed with acromegaly at the age of cols. (India; 13 out of 14 patients [92%]) (16), Mangupli
25 years), and resulted positive. and cols. (Venezuela) (6 out of 8 patients [75%]) (6), and
in the present case series (Colombia; 6 out of 6 patients
[100%]). The diagnosis of gigantism is usually
DISCUSSION established around the age of 14 years, and was reported
Between 5-15% of the pediatric pituitary adenomas at a mean age of 13.6 years by Creo and Lteif (15), 13
produce GH. Most cases (90%) comprise years by Rostomyan and cols. (3), 18 years by Mangupli
macroadenomas, and 30-60% are invasive. A higher and cols. (6), and 21.9 ± 6.1 years by Patt and cols. (16).
frequency in males is reported in the literature (13). In our case series, the diagnosis
A B
C D
Copyright © AE&M all rights reserved.
Figure 3. (A) Initial coronal T1-weighted magnetic resonance imaging (MRI). (B) Initial sagittal T1-weighted post-contrast
MRI. (C) Coronal T1-weighted MRI 1 year after the second surgical procedure. (D) Coronal T1-weighted post-contrast
MRI postcontrast 3 years after the second surgical procedure and 2 year after radioterapy plus medical treatment.
Arch Endocrinol Metab. 2019;63/4 389
Pituitary gigantism: a case series
of gigantism was established at a mean age of 16 years. A of the patients in the series by Creo and Lteif (15), 66.7%
delayed diagnosis of gigantism may occur due to poor (118 out of 208) reported by Rostomyan and cols. (3), and
perception of the magnitude of the symptoms, delayed 23% (3 out of 13) in the study by Nagata and cols. (14).
consultations, and limited knowledge of the disease by In our series, none of the patients had biochemical control
healthcare providers, all of which are important factors in with SSA alone, which is aligned to the results by Creo
Latin America. The most common symptoms presented and Lteif (15) and Mangupli and cols. (6); in contrast, in
by our patients were headache (66%) and hyperhidrosis the study by Rostomyan and cols., 34% of the patients
(66%), unlike the series by Rostomyan and cols. (3), in were controlled with SSA alone (3). Rates of biochemical
which headache was less frequent (23%). control in patients with acromegaly have been reported at
In gigantism, TSS is the first-choice procedure, and 63.9% with octreotide and 78.1% with lanreotide Autogel
biochemical control is obtained in 70% of the patients (17). Of note, one case report of a girl with gigantism and
with intrasellar microadenomas, although this rate is microadenoma showed biochemical control and
lower with macroadenomas (13). TSS was the most disappearance of the tumor with octreotide LAR for 3
common procedure performed in our patients (66%), and years (7). A prospective study conducted in Japan with 32
none of the patients obtained biochemical control with patients with acromegaly (29 patients) and gigantism (3
this treatment alone. The only case with biochemical patients) assessed the efficacy of lanreotide Autogel;
control followed a frontal craniotomy. In the series by although separate data for patients with gigantism were
Nagata and cols., 92% (12 out of 13) of the patients were not reported, the efficacy was reported to be similar in
managed with TSS and 53% (7 out of 13) achieved both groups (acromegaly and gigantism) (18).
biochemical control; this was the case series with best
reported response with TSS (14). In the study by Creo and Dopamine receptor agonists are useful in cases with
Lteif, 92% (12 out of 13) of the patients were treated with associated hyperprolactinemia or as an adjunct therapy to
TSS, and only 23% (3 out of 13) achieved biochemical SSAs in cases with lack of biochemical control and IGF-1
control (15). In the publication by Rostomyan and cols., levels up to 1.5 times above the normal range (19). None
surgery was performed in 82% (177 out of 208) of the of our patients presented hyperprolactinemia, in contrast
patients and only 15% obtained biochemical control (3). to the finding by Mangupli and cols., in which 50% (4 out
In the series by Patt and cols., surgery was performed in of 8) of the patients had hyperprolactinemia
92% (13 out of 14) of the patients and 21% obtained (6). Cabergoline was administered to 3 of our patients,
biochemical control (16). In the cases described by and biochemical control was obtained in 1 (patient #3)
Mangupli and cols. (6), none of the patients who with concomitant use of octreotide LAR. Cabergoline
underwent surgery obtained control. In our series, surgical was administered to 4 patients by Mangupli and cols.
reintervention was required in 33% (2 out of 6) of the (6) and 2 patients by Nagata and cols. (14), and none
patients, compared with 30% (4 out of 13) in the series by of the patients obtained biochemical control. The
Creo and Lteif (15) and 64% in the series by Rostomyan effectiveness of cabergoline in the management of
and cols. (3). Only 7.5% of our patients had a biochemical gigantism without associated hyperprolactinemia lacks
response to the surgical reintervention, while 2 patients evidence.
(33%) presented hypopituitarism with thyroid and Pegvisomant (a GH receptor antagonist) has been
gonadal dysfunction, a rate that is similar to that reported used in pediatrics to obtain IGF-1 normalization and
by Creo and Lteif, who described a 38% rate of symptom improvement in patients without a response
hypopituitarism (5 out of 13 patients) (15). to surgical treatment, radiotherapy, and SSAs, although
the possibility of an increase in tumor size with this
Given the low biochemical control with surgery, medication should be considered (9,13,20). In a report
patients with gigantism usually require additional of 3 patients treated with pegvisomant, linear growth
management. SSAs were used in 83% of our patients (5 was interrupted after 6 months of treatment, and
improvement in diaphoresis and facial features of
reserved.
out of 6; 3 were treated with lanreotide Autogel and 2
acromegaly was observed, along with normalization of
all rights
with octreotide LAR). This finding was similar in the
series by Mangupli and cols. (6), in which 100% (8 out IGF-1 levels in 2 of them, while the other one showed
Copyright© AE&M
of 8) of the patients used SSAs. Still, the use of SSA an increase in tumor size (9). Effectiveness was
was less frequent in other studies: 50% (6 out of 12) confirmed in 2 of our patients in whom this medication
390 Arch Endocrinol Metab. 2019;63/4
Pituitary gigantism: a case series
was administrated (patients #1 and #6), a result that is (78%) include men. The mean age at diagnosis was
similar to the one reported by Creo and Lteif (15) and 15.1 years, and the mean final height was 1.95 m. TSS
Mangupli and cols. (6). A lower rate of biochemical was the most frequent initial procedure (83%), and
control (50% of the patients) was observed by only 18% of the patients obtained biochemical control
Rostomyan and cols. (3), and absence of response was with this procedure alone, while 122 out of 219
observed on a single patient treated with pegvisomant patients (56%) required surgical reintervention. Half of
by Nagata and cols. (14). The combination of SSAs the patients (53%) received SSAs, and only 1
with pegvisomant seems to be the most effective successful case of treatment with SSA monotherapy
association for the treatment of gigantism, as reported was reported. Pegvisomant was administered to 17.5%
by Mangupli and cols. in 8 patients with gigantism. of the patients, with IGF-1 normalization in 58% of
Early (1 to 4 months) symptom control was observed, them, which is a lower rate than the 67.5% response
with an absence of tumor growth and normalization of reported in a “real world” study in patients with
IGF-1 levels in all patients (6). acromegaly (21), possibly related to inadequate dose
Radiotherapy was administered to 66% (4 out of 6) titration. Radiotherapy was used in 30% of the patients
of our patients, which is a higher rate than reported by (Table 3), which is a high percentage taking into
other authors of case series: 46% (6 out of 13) of the account the risk of hypopituitarism in this population.
patients by Creo and Lteif (15), 30% (63 out of
208) by Rostomyan and cols. (3), 35% (5 out of 14) Familial isolated pituitary adenomas
by Patt and cols. (16), and one patient by Mangupli The diagnosis of FIPA should be suspected when 2 or
and cols. (6) and Nagata and cols. (14). The risk of more relatives have pituitary adenomas in the absence
hypopituitarism, which can occur in 30-50% of the of known genetic causes, such as multiple endocrine
patients, should be considered (13). Table 3 presents a neoplasia type 1, Carney complex, or McCune-
comparison of case series of gigantism (3,6,14-16), Albright syndrome (22). The main causes of FIPA are
including the present study. Most of the cases reported X-LAG and AIP gene mutations.
Table 3. Comparison of case series of gigantism reported in the literature
Rostomyan Mangupli and Rojas and
Nagata and cols.
and Daly Patt and cols. Creo and cols. cols.
cols. (Japan) (Colombia) Total
(multicentric) (India) 2015 (USA) 2016 (Venezuela)
2017 2018 (current
2015 2016
study)
Male gender 163/208 14/14 9/13 6/8 7/13 6/6 205/262 (78%)
Mean final height (meters) NA 1.87 2.05 1.9 NA 2.01 1.95
Mean age at diagnosis (years) 13 21.9 ± 6.1 13.6 18 NA 16 15.1
TSS 177/208 13/14 12/13 1/8 12/13 4/6 219/262 (83%)
Biochemical control after first 27/177 3/13 3/12 0/1 7/13 0/4 40/219 (18%)
surgery
Surgical reintervention 113/177 2/13 4/13 NA 1/7 2/6 122/219a
Biochemical control after 8/113 1/2 3/4 NA NA 0/2 12/122a
second surgery
SSA 118/208 0/14 6/12 8/8 3/13 5/6 140/262 (53%)
SSA biochemical control 0/118 0/14 1/6 0/8 NA 0/6 1/140a
PEG 37/208 0/14 2/6 4/8 1/13 2/6 46/262 (17.5%)
IGF-1 normalization with PEG 19/37 0 2/2 4/4 0/1 2/2 27/46 (58%)
RT 63/208 5/14 6/13 1/8 1/13 4/6 80/262 (30%)
Copyright © AE&M all rights reserved.
Response to RT 27/63 3/5 NA NA 1/1 2/4 33/80a
AIP mutation 42/208 NA NA 3/8 5/13 2/6 52
AIP: aryl hydrocarbon receptor-interacting protein, NA: not available, PEG: Pegvisomant, RT: radiotherapy, SSA: somatostatin analogues, TSS:
transsphenoidal surgery. a Percentage not reported due to incomplete data.
Arch Endocrinol Metab. 2019;63/4 391
Pituitary gigantism: a case series
X-LAG, which may occur isolated or associated with gigantism, a pathology with a high functional and
FIPA, is characterized by pituitary adenomas or pituitary psychological impact on affected patients. Like other
hyperplasia producing most frequently increased levels case series, men were more affected than women. It is
of GH, GH releasing hormone (GHRH), and prolactin. important to note that the diagnosis was established
The patients affected by this condition exhibit rapid late (at the age of 16 years) in our population compared
growth starting in childhood. X-LAG is more frequent with other studies. TSS was the first-choice procedure,
in women and responds poorly to treatment with SSAs but given a low biochemical control rate,
(2,23,24). pharmacological therapy was often required. It should
Regarding mutations in the AIP gene, patients with be noted that the use of SSAs is less effective in
these mutations inactivating the AIP gene generally gigantism than acromegaly, and that there are no
have adenomas that produce GH and/or prolactin. significant differences in effectiveness between
Mutations of the AIP gene were reported in 5 out of available analogues. In case of lack of response to
13 patients (38%) by Nagata and cols. (14), in 3 out SSAs, the association of pegvisomant is recommended.
of 8 (38%) patients by Mangupli and cols. (6), and in Even with an adequate biochemical response and
42 out of 208 patients (20%) by Rostomyan and cols. symptom improvement, appropriate monitoring with
(3). These mutations are characterized by early onset tests should be performed due to the risk of tumor
(before the age of 20 years) and frequent occurrence growth. The use of cabergoline (in patients with
of gigantism, and for affecting males more frequently associated hyperprolactinemia) and radiotherapy as
than females. Most tumors (93%) are macroadenomas third-line management should be considered, but the
and, compared with patients without AIP mutation, high probability of radiotherapy-induced
have a more aggressive behavior including greater hypopituitarism in the pediatric population should be
extrasellar growth and lower response to surgical and taken into consideration. To avoid continued vertical
medical treatment requiring a subsequent operation, growth in patients with gigantism in cases of residual
and more frequent use of radiotherapy (2,25,26).
tumor and no response to surgery and SSA
This was evident in one of our patients (patient #1),
management, we consider that the best option in case
whom even after two surgeries showed an increase in
of residual tumors is combined therapy with SSAs and
tumor size and absence of response to SSA, but finally
pegvisomant. Pegvisomant as monotherapy can be
responded to pegvisomant and radiotherapy. For
considered in the absence of residual tumor, as well as
these reasons, early screening of relatives of affected
in patients with the AIP gene mutation, given the high
patients is important (26-28). Multiple mutations
probability of therapeutic failure of SSA.
of this gene have been described. The heterozygous
Mutations of the AIP gene should be considered in
pathogenic variant of the AIP gene c.504G>A in
familial cases of GH-producing adenomas. Multiple
exon 4 (p.Trp168*), found in our patients, has not
been previously reported in the literature or in other pathogenic variants of this gene have been described,
patients in Colombia. but this is the first time that these mutations have been
In our case series, sequencing of the AIP gene was documented in Colombia.
requested from patients #1 and #5, taking into account Ethical approval: all procedures performed in studies involving
the association of mutations of this gene with FIPA. human participants were in accordance with the ethical
Gene sequencing was also requested from all other standards of the institutional and/or national research
committee, and with the 1964 Helsinki Declaration and its later
patients, given the evidence of mutations of the AIP amendments or com-parable ethical standards.
gene in children under 18 years of age with pituitary
adenomas, and in those under 30 years of age with Informed consent: informed consent was obtained from all parti-
macroadenomas (29,30). However, this test was not cipants included in the study.
rightsreserved.
approved by the health insurance of patients #2 and
Acknowledgments: we thank the patients who agreed to partici-
pending at the time of the study, but these patients did
#3. Authorization for the test in patients #4 and #6 was
pate in the study and who consented to the publication of their
all
not follow up at our Unit. pictures, diagnostic images, and genealogical trees.
Copyright© AE&M
In conclusion, this is the largest case series
Disclosure: no potential conflict of interest relevant to this article
described to date in Colombia of patients with was reported.
392 Arch Endocrinol Metab. 2019;63/4
Pituitary gigantism: a case series
REFERENCES 16. Patt HP, Bothra N, Goel AH, Kasaliwal R, Lila AR, Bandgar TR,
et al. Pituitary gigantism – Experience of a single center from
1. Hannah-Shmouni F, Trivellin G, Stratakis CA. Genetics of gigantism Western India. Endocr Pract. 2015;21(6):621-8.
and acromegaly. Growth Horm IGF Res. 2016;30-31:37-41.
17. Tutuncu Y, Berker D, Isik S, Ozuguz U, Akbaba G, Kucukler FK,
2. Rostomyan L, Daly AF, Beckers A. Pituitary gigantism: causes and et al. Comparison of octreotide LAR and lanreotide autogel as
clinical characteristics. Ann Endocrinol (Paris). 2015;76(6):643-9. post-operative medical treatment in acromegaly. Pituitary.
3. Rostomyan L, Daly AF, Petrossians P, Nachev E, Lila AR, Lecoq 2012;15(3):398-404.
AL, et al. Clinical and genetic characterization of pituitary 18. Shimatsu A, Teramoto A, Hizuka N, Kitai K, Ramis J, Chihara K.
gigantism: an international collaborative study in 208 patients. Efficacy, safety, and pharmacokinetics of sustained-release
Endocr Relat Cancer. 2015;22(5):745-57. lanreotide (lanreotide Autogel) in Japanese patients with
4. Dyer EH, Civit T, Visot A, Delalande O, Derome P. acromegaly or pituitary gigantism. Endocr J. 2013;60(5):651-63.
Transsphenoidal surgery for pituitary adenomas in children. 19. Sandret L, Maison P, Chanson P. Place of cabergoline in
Neurosurgery. 1994;34(2):207-12; discussion 12. acromegaly: a meta-analysis. J Clin Endocrinol Metab.
5. Lodish MB, Trivellin G, Stratakis CA. Pituitary gigantism: update 2011;96(5):1327-35.
on molecular biology and management. Curr Opin Endocrinol 20. Rix M, Laurberg P, Hoejberg AS, Brock-Jacobsen B.
Diabetes Obes. 2016;23(1):72-80. Pegvisomant therapy in pituitary gigantism: successful treatment
6. Mangupli R, Rostomyan L, Castermans E, Caberg JH, Camperos in a 12-year-old girl. Eur J Endocrinol. 2005;153(2):195-201.
P, Krivoy J, et al. Combined treatment with octreotide LAR and 21. Freda PU, Gordon MB, Kelepouris N, Jonsson P, Koltowska-
pegvisomant in patients with pituitary gigantism: clinical Haggstrom M, van der Lely AJ. Long-term treatment with pegvisomant
evaluation and genetic screening. Pituitary. 2016;19(5):507-14. as monotherapy in patients with acromegaly: experience from
7. Ciresi A, Amato MC, Galluzzo A, Giordano C. Complete ACROSTUDY. Endocr Pract. 2015;21(3):264-74.
biochemical control and pituitary adenoma disappearance in a 22. Daly AF, Jaffrain-Rea ML, Ciccarelli A, Valdes-Socin H, Rohmer V,
child with gigantism: efficacy of octreotide therapy. J Endocrinol Tamburrano G, et al. Clinical characterization of familial isolated
Invest. 2011;34(2):162-3. pituitary adenomas. J Clin Endocrinol Metab. 2006;91(9):3316-23.
8. Barrande G, Pittino-Lungo M, Coste J, Ponvert D, Bertagna X, 23. Trivellin G, Daly AF, Faucz FR, Yuan B, Rostomyan L, Larco DO,
Luton JP, et al. Hormonal and metabolic effects of radiotherapy et al. Gigantism and acromegaly due to Xq26 microduplications
in acromegaly: long-term results in 128 patients followed in a and GPR101 mutation. N Engl J Med. 2014;371(25):2363-74.
single center. J Clin Endocrinol Metab. 2000;85(10):3779-85.
24. Beckers A, Lodish MB, Trivellin G, Rostomyan L, Lee M, Faucz
9. Goldenberg N, Racine MS, Thomas P, Degnan B, Chandler W, FR, et al. X-linked acrogigantism syndrome: clinical profile and
Barkan A. Treatment of pituitary gigantism with the GH receptor therapeutic responses. Endocr Relat Cancer. 2015;22(3):353-67.
antagonist pegvisomant. J Clin Endocrinol Metab.
25. Guaraldi F, Salvatori R. Familial isolated pituitary adenomas:
2008;93(8):2953-6.
from genetics to therapy. Clin Transl Sci. 2011;4(1):55-62.
10. Müssig K, Gallwitz B, Honegger J, Strasburger CJ, Bidlingmaier
26. Chahal HS, Chapple JP, Frohman LA, Grossman AB, Korbonits
M, Machicao F, et al. Pegvisomant treatment in gigantism
M. Clinical, genetic and molecular characterization of patients
caused by a GH-secreting giant pituitary adenoma. Exp Clin
with familial isolated pituitary adenomas (FIPA). Trends
Endocrinol Diabetes. 2007;115(3):198-202.
Endocrinol Metab. 2010;21(7):419-27.
11. Durán P, Merker A, Briceño G, Colón E, Line D, Abad V, et al.
27. Igreja S, Chahal HS, King P, Bolger GB, Srirangalingam U,
Colombian reference growth curves for height, weight, body mass
Guasti L, et al. Characterization of aryl hydrocarbon receptor
index and head circumference. Acta Paediatr. 2016;105(3):e116-25.
interacting protein (AIP) mutations in familial isolated pituitary
12. Katznelson L, Laws ER, Melmed S, Molitch ME, Murad MH, Utz adenoma families. Hum Mutat. 2010;31(8):950-60.
A, et al. Acromegaly: an endocrine society clinical practice
28. Fajardo-Montañana C, Daly AF, Riesgo-Suárez P, Gómez-Vela
guideline. J Clin Endocrinol Metab. 2014;99(11):3933-51. J, Tichomirowa MA, Camara-Gómez R, et al. [AIP mutations in
13. Guaraldi F, Storr HL, Ghizzoni L, Ghigo E, Savage MO. familial and sporadic pituitary adenomas: local experience and
Paediatric pituitary adenomas: a decade of change. Horm Res review of the literature]. Endocrinol Nutr. 2009;56(7):369-77.
Paediatr. 2014;81(3):145-55. 29. Korbonits M, Storr H, Kumar AV. Familial pituitary adenomas –
14. Nagata Y, Inoshita N, Fukuhara N, Yamaguchi-Okada M, who should be tested for AIP mutations? Clin Endocrinol (Oxf).
Nishioka H, Iwata T, et al. GH-producing pituitary adenomas in 2012;77(3):351-6.
childhood and young adulthood: clinical features and outcomes. 30. Tichomirowa MA, Barlier A, Daly AF, Jaffrain-Rea ML, Ronchi C,
Pituitary. 2017. Yaneva M, et al. High prevalence of AIP gene mutations following
15. Creo AL, Lteif AN. Pituitary gigantism: a retrospective case focused screening in young patients with sporadic pituitary
series. J Pediatr Endocrinol Metab. 2016;29(5):597-602. macroadenomas. Eur J Endocrinol. 2011;165(4):509-15.
Copyright © AE&M all rights reserved.
Arch Endocrinol Metab. 2019;63/4 393
Potrebbero piacerti anche
- AACR 2022 Proceedings: Part A Online-Only and April 10Da EverandAACR 2022 Proceedings: Part A Online-Only and April 10Nessuna valutazione finora
- Abstracts of The 2020 Annual Meeting (AMH) / Annals of Hepatology 19 (2020) 1-28 3Documento1 paginaAbstracts of The 2020 Annual Meeting (AMH) / Annals of Hepatology 19 (2020) 1-28 3Jhosept Perez AlvaNessuna valutazione finora
- A Model for Gene Therapy: Gene Replacement in the Treatment of Sickle Cell Anemia and ThalassemiaDa EverandA Model for Gene Therapy: Gene Replacement in the Treatment of Sickle Cell Anemia and ThalassemiaNessuna valutazione finora
- Review: Maria Fleseriu, Fabienne Langlois, Dawn Shao Ting Lim, Elena V Varlamov, Shlomo MelmedDocumento23 pagineReview: Maria Fleseriu, Fabienne Langlois, Dawn Shao Ting Lim, Elena V Varlamov, Shlomo MelmedAaron PeñaNessuna valutazione finora
- World Journal of Surgical Oncology: Abnormal HCG Levels in A Patient With Treated Stage I Seminoma: A Diagnostic DilemmaDocumento3 pagineWorld Journal of Surgical Oncology: Abnormal HCG Levels in A Patient With Treated Stage I Seminoma: A Diagnostic DilemmaarakbaeNessuna valutazione finora
- Enf TrofoblasticaDocumento10 pagineEnf TrofoblasticaDaniela CovarrubiasNessuna valutazione finora
- Clinical Endocrinology - 2022 - Coopmans - Molecular Genetic Testing in The Management of Pituitary DiseaseDocumento12 pagineClinical Endocrinology - 2022 - Coopmans - Molecular Genetic Testing in The Management of Pituitary DiseasegarrobosNessuna valutazione finora
- Gastrointestinal Stromal Tumors-A Mini ReviewDocumento14 pagineGastrointestinal Stromal Tumors-A Mini ReviewThomas KlebNessuna valutazione finora
- Ojped 2024030813565746Documento6 pagineOjped 2024030813565746Nicolás Mosso F.Nessuna valutazione finora
- Tirotoxicosis Mayo Clinic Proceedings. Harma2019Documento17 pagineTirotoxicosis Mayo Clinic Proceedings. Harma2019Salome GarciaNessuna valutazione finora
- Clinical Case Reports - 2020 - GiuffridaDocumento6 pagineClinical Case Reports - 2020 - GiuffridaAhmed SabryNessuna valutazione finora
- Arar0332 Jco 2021 DR RaulDocumento14 pagineArar0332 Jco 2021 DR RaulLeonardo Müller RodriguesNessuna valutazione finora
- Acromegaly Pathogenesis, Diagnosis, and ManagementDocumento23 pagineAcromegaly Pathogenesis, Diagnosis, and ManagementPaolo MessinaNessuna valutazione finora
- Pituitary Incidentalomas Best Practices and Looking AheadDocumento9 paginePituitary Incidentalomas Best Practices and Looking AheadJulieta LopezNessuna valutazione finora
- AACE Clinical Case ReportsDocumento5 pagineAACE Clinical Case ReportsSameerNessuna valutazione finora
- Prognostic Factors For Recurrence in Patients With Papillary Thyroid CarcinomaDocumento8 paginePrognostic Factors For Recurrence in Patients With Papillary Thyroid CarcinomaLeonardo LeónNessuna valutazione finora
- Radio-Contrast Agent-Induced Hyperthyroidism: Case Report and Review of The LiteratureDocumento3 pagineRadio-Contrast Agent-Induced Hyperthyroidism: Case Report and Review of The LiteratureIwan SaputeraNessuna valutazione finora
- Cushing's Syndrome (Lancet)Documento16 pagineCushing's Syndrome (Lancet)Irma OnofreNessuna valutazione finora
- Congenital Hyperinsulinism of The Newborn: A Case ReportDocumento6 pagineCongenital Hyperinsulinism of The Newborn: A Case ReportEdi SetiawanNessuna valutazione finora
- Cripe2017 2750523Documento4 pagineCripe2017 2750523فرجني موغNessuna valutazione finora
- Unexpected Immunohistochemical Surprise of A Cushings Disease Macroadenoma Co-Expressing Acth and Prolactin: A Case ReportDocumento5 pagineUnexpected Immunohistochemical Surprise of A Cushings Disease Macroadenoma Co-Expressing Acth and Prolactin: A Case ReportIJAR JOURNALNessuna valutazione finora
- Pathol 2020 03 166Documento20 paginePathol 2020 03 166Juan Mendia OssioNessuna valutazione finora
- Adrenal Histoplasmosis A Therapeutic Restoration of - 2022 - AACE Clinical CaseDocumento2 pagineAdrenal Histoplasmosis A Therapeutic Restoration of - 2022 - AACE Clinical CaseMohammed Shuaib AhmedNessuna valutazione finora
- Gallbladder CancerDocumento22 pagineGallbladder Cancercarlos.alberto.palacios.serratNessuna valutazione finora
- Prenatal Imaging Features Suggestive of Liver Gestational Allo Immune DiseaseDocumento4 paginePrenatal Imaging Features Suggestive of Liver Gestational Allo Immune DiseaseEuis NoorhayatyNessuna valutazione finora
- Clinical Characterization Cohort Systemic Lupus Erythematosus. PLoS One-2023Documento14 pagineClinical Characterization Cohort Systemic Lupus Erythematosus. PLoS One-2023Jorge Ricardo Parra CamachoNessuna valutazione finora
- Comparison of MUST and Nutriscore For The Screening of Malnutrition in Hospitalized Oncology PatientsDocumento7 pagineComparison of MUST and Nutriscore For The Screening of Malnutrition in Hospitalized Oncology Patientssergedemirdjian1990Nessuna valutazione finora
- An Evidence-Based Approach To The Medical Management of Fibroids: A Systematic ReviewDocumento23 pagineAn Evidence-Based Approach To The Medical Management of Fibroids: A Systematic ReviewMarco Julcamoro AsencioNessuna valutazione finora
- Ijgo 13877Documento8 pagineIjgo 13877rutujaNessuna valutazione finora
- Acromegaly PRIMERDocumento17 pagineAcromegaly PRIMERtaagrettaaNessuna valutazione finora
- New Directions in The Treatment of HypoparathyroidismDocumento6 pagineNew Directions in The Treatment of Hypoparathyroidismmiguel saba sabaNessuna valutazione finora
- Group 6 1Documento48 pagineGroup 6 1baldosangelique14Nessuna valutazione finora
- Bankoglu 2018Documento8 pagineBankoglu 2018Ronald Echeverria IbazetaNessuna valutazione finora
- Insight Into The Pathogensis of Polycystic OvarianDocumento10 pagineInsight Into The Pathogensis of Polycystic OvarianHAVIZ YUADNessuna valutazione finora
- Hipofisis 3Documento23 pagineHipofisis 3RafaelPetitNessuna valutazione finora
- 10 1002@pbc 28709Documento10 pagine10 1002@pbc 28709Ahmed BaghdadiNessuna valutazione finora
- Seminar: Michael J Seckl, Neil J Sebire, Ross S BerkowitzDocumento13 pagineSeminar: Michael J Seckl, Neil J Sebire, Ross S BerkowitzFelicia HalimNessuna valutazione finora
- 331-Book Chapter-3614-2-10-20210406Documento20 pagine331-Book Chapter-3614-2-10-20210406Yolla GitamayaNessuna valutazione finora
- Fostamatinib For The Treatment of Warm Antibody Autoimmune Hemolytic Anemia Phase 2Documento9 pagineFostamatinib For The Treatment of Warm Antibody Autoimmune Hemolytic Anemia Phase 2Maria Eugenia VelisNessuna valutazione finora
- Antioxidant Supplementation and Premature Rupture of The Membranes A Planned Secondary AnalysisDocumento8 pagineAntioxidant Supplementation and Premature Rupture of The Membranes A Planned Secondary AnalysisizulNessuna valutazione finora
- 10 1016@j Jacc 2017 11 011Documento16 pagine10 1016@j Jacc 2017 11 011Anita YolandhaNessuna valutazione finora
- Reaction Paper IN People and The Earth'S EcosystemDocumento9 pagineReaction Paper IN People and The Earth'S EcosystemGianna MaeNessuna valutazione finora
- Honokiol Inhibits Melanoma Growth by Targeting KerDocumento11 pagineHonokiol Inhibits Melanoma Growth by Targeting Kerdaniela santurioNessuna valutazione finora
- Trisomy 18 With Multiple Congenital Anomalies A Rare Case Report-3Documento4 pagineTrisomy 18 With Multiple Congenital Anomalies A Rare Case Report-3Elna EstherNessuna valutazione finora
- Diagnosis of Hirschsprung Disease: Lusine Ambartsumyan, Caitlin Smith, and Raj P KapurDocumento15 pagineDiagnosis of Hirschsprung Disease: Lusine Ambartsumyan, Caitlin Smith, and Raj P KapurGhina Mauizha WulandariNessuna valutazione finora
- 9325-Article Text-68347-1-10-20200725Documento7 pagine9325-Article Text-68347-1-10-20200725drchandrusNessuna valutazione finora
- Hipopituitarismo Lectura Motivadora1)Documento13 pagineHipopituitarismo Lectura Motivadora1)Daniela Romero RiosNessuna valutazione finora
- Cancer Epidemiol Biomarkers Prev 2004 Ley 4 10Documento8 pagineCancer Epidemiol Biomarkers Prev 2004 Ley 4 10Cristian BorrelliNessuna valutazione finora
- JCRPE 13 119 enDocumento5 pagineJCRPE 13 119 enAhmed BaghdadiNessuna valutazione finora
- 2000 - Frankel - Re Radical Prostatectomy For Localized Prostate Cancer Provides Durable Cancer Control With Excellent Quality of Life A STRDocumento2 pagine2000 - Frankel - Re Radical Prostatectomy For Localized Prostate Cancer Provides Durable Cancer Control With Excellent Quality of Life A STRPoljarLijanNessuna valutazione finora
- Case 12-2016: An 8-Year-Old Boy With An Enlarging Mass in The Right BreastDocumento10 pagineCase 12-2016: An 8-Year-Old Boy With An Enlarging Mass in The Right BreastbayutrihatmajaNessuna valutazione finora
- Rodriguez-Galindo2005, Ribeiro, BonaldDocumento9 pagineRodriguez-Galindo2005, Ribeiro, BonaldLeonardo Müller RodriguesNessuna valutazione finora
- Biomarker 4Documento6 pagineBiomarker 4Devianti TandialloNessuna valutazione finora
- Hormonal Therapies in Septic Shock: Review ArticleDocumento8 pagineHormonal Therapies in Septic Shock: Review ArticleJhon3xNessuna valutazione finora
- Effectiveness of High-Dose Glucocorticoids On Hemolysis, Elevating Liver Enzymes, and Reducing Platelets SyndromeDocumento10 pagineEffectiveness of High-Dose Glucocorticoids On Hemolysis, Elevating Liver Enzymes, and Reducing Platelets SyndromeAlfa FebriandaNessuna valutazione finora
- Enfermedad de Creutzfeldt-Jakob Iatrogénica Secundaria A Hormonas Hipofisiarias Cadavéricas.Documento3 pagineEnfermedad de Creutzfeldt-Jakob Iatrogénica Secundaria A Hormonas Hipofisiarias Cadavéricas.JuanCk7Nessuna valutazione finora
- Papillary Thyroid Carcinoma Hobnail Variant A Report of Two Cases 5816 PDFDocumento5 paginePapillary Thyroid Carcinoma Hobnail Variant A Report of Two Cases 5816 PDFriswani tangibaliNessuna valutazione finora
- Publication Lipidemia PDFDocumento6 paginePublication Lipidemia PDFMasnaeni AwaliahNessuna valutazione finora
- Peritoneal Tuberculosis: The Great Mimicker: Case StudyDocumento5 paginePeritoneal Tuberculosis: The Great Mimicker: Case StudyDumitru RadulescuNessuna valutazione finora
- Mehu131 U1 T6 Obesidad4Documento16 pagineMehu131 U1 T6 Obesidad4Valeria Moretto VegaNessuna valutazione finora
- Tata Kelola DM Di FKTPDocumento29 pagineTata Kelola DM Di FKTPRSTN BoalemoNessuna valutazione finora
- Guanavante GeniusDocumento270 pagineGuanavante Geniusartisanicview100% (3)
- International Journal of Pharmaceutics: Yuqing Ye, Ying Ma, Jesse ZhuDocumento17 pagineInternational Journal of Pharmaceutics: Yuqing Ye, Ying Ma, Jesse ZhuAlina CiugureanuNessuna valutazione finora
- Triase IGD Maret 2021Documento33 pagineTriase IGD Maret 2021IRAYANANessuna valutazione finora
- Cleft Lip and Cleft PalateDocumento8 pagineCleft Lip and Cleft PalateRAJU33% (3)
- Ch.4 Physical Education and Sports For CWSN: Meaning of DisabilityDocumento9 pagineCh.4 Physical Education and Sports For CWSN: Meaning of Disabilitydarksound6Nessuna valutazione finora
- RHS Exam OutlineDocumento10 pagineRHS Exam Outlinefree booksNessuna valutazione finora
- TCCC Quick Reference Guide 2017Documento54 pagineTCCC Quick Reference Guide 2017https://www.t-medical.orgNessuna valutazione finora
- Efektivitas Aromaterapi Lemon Untuk Mengatasi Emesis GravidarumDocumento8 pagineEfektivitas Aromaterapi Lemon Untuk Mengatasi Emesis Gravidarumsri yulinar pakuNessuna valutazione finora
- 2011 Efficacy and Augmentation During 6 Months of Double-Blind Pramipexole For Restless Legs SyndromeDocumento10 pagine2011 Efficacy and Augmentation During 6 Months of Double-Blind Pramipexole For Restless Legs SyndromeAga_tthaNessuna valutazione finora
- Orthodontics-Gurkeerat Singh, 2nd EditionDocumento704 pagineOrthodontics-Gurkeerat Singh, 2nd Editionkeralaapple85% (34)
- Chief Complaint: Problem VisitDocumento2 pagineChief Complaint: Problem VisitChirra WilliamsNessuna valutazione finora
- Nursing Care Plan For Pregnancy Induced HypertensionDocumento9 pagineNursing Care Plan For Pregnancy Induced HypertensionMurugham DineshNessuna valutazione finora
- Capitulo 5 StudervantDocumento23 pagineCapitulo 5 StudervantDiegoMoralesNessuna valutazione finora
- PNGIMR 40th Anniversary and ColloquiumDocumento116 paginePNGIMR 40th Anniversary and ColloquiumJamie CrossNessuna valutazione finora
- Emerging Trends in Patient Counselling: Current Scenario: Journal Club - PresentationDocumento12 pagineEmerging Trends in Patient Counselling: Current Scenario: Journal Club - PresentationRaju BaiNessuna valutazione finora
- NCP For PostpartumDocumento9 pagineNCP For PostpartumYzel Vasquez AdavanNessuna valutazione finora
- Ovr New MohDocumento2 pagineOvr New MohhyNessuna valutazione finora
- Standardized Nursing TerminologyDocumento5 pagineStandardized Nursing TerminologyDaniel WainainaNessuna valutazione finora
- Nurse Deployment Program NDP Examination NotesDocumento44 pagineNurse Deployment Program NDP Examination NotesAngelo Quixote100% (1)
- Retaining WallDocumento10 pagineRetaining Wallsandip patilNessuna valutazione finora
- Drug Study Table OkDocumento29 pagineDrug Study Table OkRifa'atul Mahmudah100% (1)
- TFN Dorothea OremDocumento22 pagineTFN Dorothea OremRaphael SevillaNessuna valutazione finora
- 61Documento205 pagine61Carlos HernándezNessuna valutazione finora
- Esthetic Impact of Premolar Extraction and Nonextraction Treatments On Korean Borderline PatientsDocumento8 pagineEsthetic Impact of Premolar Extraction and Nonextraction Treatments On Korean Borderline Patientsblogger bloggerNessuna valutazione finora
- GINA - Global Initiative For AsthmaDocumento82 pagineGINA - Global Initiative For AsthmaRiham Mohye Eldeen MohammedNessuna valutazione finora
- Ineffective Tissue Perfusion Related To Decrease Hemoglobin Concentration in The BloodDocumento2 pagineIneffective Tissue Perfusion Related To Decrease Hemoglobin Concentration in The BloodYllejann Manez60% (20)
- Incidence of Malaria Among Children Under Five Years Old in Paediatric Medical WardDocumento41 pagineIncidence of Malaria Among Children Under Five Years Old in Paediatric Medical WardUsman Ahmad TijjaniNessuna valutazione finora
- If Ppih Covid 19 Flu ColdDocumento1 paginaIf Ppih Covid 19 Flu ColdkelvinkinergyNessuna valutazione finora
- The Role of A Specialist in PeriodontologyDocumento2 pagineThe Role of A Specialist in Periodontologykevin1678Nessuna valutazione finora
- Glucose Revolution: The Life-Changing Power of Balancing Your Blood SugarDa EverandGlucose Revolution: The Life-Changing Power of Balancing Your Blood SugarValutazione: 5 su 5 stelle5/5 (351)
- Forever Strong: A New, Science-Based Strategy for Aging WellDa EverandForever Strong: A New, Science-Based Strategy for Aging WellNessuna valutazione finora
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyDa EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyValutazione: 4.5 su 5 stelle4.5/5 (3)
- Eat & Run: My Unlikely Journey to Ultramarathon GreatnessDa EverandEat & Run: My Unlikely Journey to Ultramarathon GreatnessNessuna valutazione finora
- The Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonDa EverandThe Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonValutazione: 3.5 su 5 stelle3.5/5 (33)
- Summary of Mary Claire Haver's The Galveston DietDa EverandSummary of Mary Claire Haver's The Galveston DietValutazione: 5 su 5 stelle5/5 (1)
- Instant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookDa EverandInstant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookValutazione: 3.5 su 5 stelle3.5/5 (2)
- Grit & Grace: Train the Mind, Train the Body, Own Your LifeDa EverandGrit & Grace: Train the Mind, Train the Body, Own Your LifeValutazione: 4 su 5 stelle4/5 (3)
- The Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyDa EverandThe Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyNessuna valutazione finora
- Sugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthDa EverandSugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthValutazione: 4 su 5 stelle4/5 (6)
- Metabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeDa EverandMetabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeNessuna valutazione finora
- Summary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisDa EverandSummary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisValutazione: 3 su 5 stelle3/5 (2)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Da EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Valutazione: 4 su 5 stelle4/5 (378)
- Find Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeDa EverandFind Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeValutazione: 4 su 5 stelle4/5 (3)
- The Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodDa EverandThe Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodNessuna valutazione finora
- Body Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomDa EverandBody Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomValutazione: 4 su 5 stelle4/5 (1)
- The Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsDa EverandThe Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsValutazione: 4 su 5 stelle4/5 (49)
- Secrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainDa EverandSecrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainValutazione: 3.5 su 5 stelle3.5/5 (38)
- Molecules of Emotion: Why You Feel the Way You FeelDa EverandMolecules of Emotion: Why You Feel the Way You FeelValutazione: 4 su 5 stelle4/5 (128)
- The Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingDa EverandThe Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingValutazione: 4 su 5 stelle4/5 (3)
- Eat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouDa EverandEat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouNessuna valutazione finora
- The Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthDa EverandThe Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthNessuna valutazione finora
- The Volumetrics Eating Plan: Techniques and Recipes for Feeling Full on Fewer CaloriesDa EverandThe Volumetrics Eating Plan: Techniques and Recipes for Feeling Full on Fewer CaloriesNessuna valutazione finora
- The End of Craving: Recovering the Lost Wisdom of Eating WellDa EverandThe End of Craving: Recovering the Lost Wisdom of Eating WellValutazione: 4.5 su 5 stelle4.5/5 (81)
- Keto Friendly Recipes: Easy Keto For Busy PeopleDa EverandKeto Friendly Recipes: Easy Keto For Busy PeopleValutazione: 3.5 su 5 stelle3.5/5 (2)
- How to Be Well: The 6 Keys to a Happy and Healthy LifeDa EverandHow to Be Well: The 6 Keys to a Happy and Healthy LifeValutazione: 5 su 5 stelle5/5 (1)
- How Not to Die by Michael Greger MD, Gene Stone - Book Summary: Discover the Foods Scientifically Proven to Prevent and Reverse DiseaseDa EverandHow Not to Die by Michael Greger MD, Gene Stone - Book Summary: Discover the Foods Scientifically Proven to Prevent and Reverse DiseaseValutazione: 4.5 su 5 stelle4.5/5 (84)
- Glucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingDa EverandGlucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingValutazione: 5 su 5 stelle5/5 (61)