Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
4
Caricato da
api-502171898Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
4
Caricato da
api-502171898Copyright:
Formati disponibili
CHIR12007
Clinical Assessment and Diagnosis
Portfolio Exercises Week 4
Exercise 1
A 58 year old woman presented with a gradual onset of low back pain which refers to the top of the
buttocks bilateral. She has had low back stiffness for years which is usually worse in the morning. The
intensity of the discomfort has increased over the past few months. The pain is worse with
prolonged standing, lifting, bending and on long walks. Discomfort is relieved by lying down. An ache
can be felt into the right buttock, hip and posterior thigh but only occasionally. The patient does not
experience pain in the night, no bowel or bladder changes are reported. The pain does not increase
with coughing or sneezing
List your differentials
- Degenerative disc or spondylosis
What is the significance of stiffness in the morning?
- The disc has rehydrated during the night so there is subsequent increased pressure
Is there anything in the history that suggests this is not mechanical low back pain
- The onset of mechanical back pain is generally associated with a physical task
- Mechanical back pain is usually characterised by pain that is worse on movement and
coughing
Does this history warrant x-rays?
Clarify your answer with reasoning.
- No. Patients with persistent low back pain and signs or symptoms of radiculopathy or spinal
stenosis shoulder undergo MRI or CT only if positive results would potentially lead to surgery
or epidural steroid injection for suspected radiculopathy.
Exercise 2
A 62 year old male presents with acute onset low back pain which began the previous evening and
was still present on waking with some mild progression of the pain. He is a government worker with
primarily a desk job. He was unable to identify any specific onset or event that caused the pain. No
identifiable position or activity relieves the pain. Although he works a sedentary job, he reports he
has recently begun 30 minutes of cardiovascular exercise 7 days a week and weight training 5 days a
week as his GP is concerned about his high blood pressure. His father passed from a heart attack at
age 65. Pain is rated on a verbal numeric scale of 6/10, does not change and feels very deep and
boring although every now and then there is a temporary spike in the pain. On review of systems,
vague abdominal pain is mentioned which seems to have increased with this episode of low back
pain.
What areas would you examine in this patient and why
- Would examine his lower back region and abdominal region
From the history provided, is there evidence of mechanical origin of pain? Please clarify your answer
with reasoning
- Yes there is evidence of mechanical low back pain
- Sedentary job and a recent change in fitness routine could cause mechanical lower back pain
e.g. sprain, strain
- Boring pain is a characteristic of muscles, fascia, periosteum, ligaments, joints, vessels, dura
From the history provided, is there evidence to suggest possible non-mechanical origin of the low
back pain? Please clarify your answers with reasoning
- Yes, possible infection
- Pain is continuous, day and night
- Abdominal pain which is worse now with the LBP
- Pain was not precipitated by anything
-
Exercise 3
Exercise 4
What is a Chiropractor’s role in the care of LBP
- Spinal manipulation therapy
Exercise 5
There is an article in your week 4 Reading list “Primary care management of non-specific Low Back
Pain: Key message from recent guidelines
Using this source, complete the following statements:
a. Episodes of acute LBP usually have a good prognosis with rapid improvement within the first
six weeks.
b. A diagnostic triage approach is used to identify patients whose LBP arises beyond the lumbar
spine, those with neurological deficit, those with suspected or confirmed serious spinal
pathology, and those with inflammatory disease; remaining patients are considered to have
non-specific LBP.
c. First line care:
Guidelines also reinforce the importance of teaching patients how to self-manage their LBP.
Important messages to convey to the patients are that non-specific LBP is benign; most
people have favourable prognosis with substantial improvement in the first month; it is
unlikely that there is a serious disease present; and imaging is not required and will not
change management.
d. Second line care:
There are now more consistent recommendations in favour of manual therapy and
psychological therapies as second line non-pharmacological options, as they can provide
small to moderate improvements for pain and function with mostly low to moderate quality
evidence.
Exercise 6
Label each diagram with the correct stage of disc injury:
1. Stage 1
2. Stage 2
3. Stage 3
4. Stage 4
Exercise 7
Briefly list the typical features of lumbar radiculopathy
- Nearly always unilateral
- Often feels different quality to any local LBP (referred pain from other structures often feels
same as LBP)
- Most often involves one nerve root. However, lumbar spine is more common to involve two
roots than in cervical spine
- The more distal the pain goes, the more severe the neuropathic pain process. Therapeutic
goal is to get the pain to centralise
- Be more cautious if multiple NR levels involved – may indicate greater canal stenosis (e.g.
larger disc pathology or sequestration)
- Beware bilateral radicular features – often a sign of central canal compromise – increased
likelihood of cauda equina compromise, particularly look for saddle anaesthesia, decreased
sphincter tone, rectal or bladder incontinence, constipation, urinary stasis, erectile
dysfunction
Exercise 8
Potrebbero piacerti anche
- CASE STUDY AND QUESTIONS: To Be Completed by The 13 September Week 8 Case Study 8 AllanDocumento8 pagineCASE STUDY AND QUESTIONS: To Be Completed by The 13 September Week 8 Case Study 8 Allanapi-468597987Nessuna valutazione finora
- Week 5 Case Study Chir13009Documento8 pagineWeek 5 Case Study Chir13009api-468597987Nessuna valutazione finora
- Chir13009 - Case Study Week 3Documento3 pagineChir13009 - Case Study Week 3api-479754549Nessuna valutazione finora
- Case Study 6 Chir13009 Tutor Notes 1Documento7 pagineCase Study 6 Chir13009 Tutor Notes 1api-502171898Nessuna valutazione finora
- Week 7 Case Study 7 Chir13009 Tutors Notes 1Documento10 pagineWeek 7 Case Study 7 Chir13009 Tutors Notes 1api-502171898Nessuna valutazione finora
- Quiz - MyotomesDocumento6 pagineQuiz - Myotomesapi-502171898Nessuna valutazione finora
- Week 4 Case 4 Chir13009 Tutors NotesDocumento10 pagineWeek 4 Case 4 Chir13009 Tutors Notesapi-502171898Nessuna valutazione finora
- Reflection 1Documento3 pagineReflection 1api-502171898Nessuna valutazione finora
- Week 1 Weekly QuestionsDocumento6 pagineWeek 1 Weekly Questionsapi-502171898Nessuna valutazione finora
- PCP Questions Week 10Documento2 paginePCP Questions Week 10api-502171898Nessuna valutazione finora
- Reflection 2Documento2 pagineReflection 2api-502171898Nessuna valutazione finora
- Week 9 10 Q ADocumento5 pagineWeek 9 10 Q Aapi-477982644Nessuna valutazione finora
- Week 2 Weekly QuestionsDocumento13 pagineWeek 2 Weekly Questionsapi-502171898Nessuna valutazione finora
- PCP Weekly Questions WK 9Documento6 paginePCP Weekly Questions WK 9api-502171898Nessuna valutazione finora
- Exercise 1: CHIR12007 Clinical Assessment and Diagnosis Portfolio Exercises Week 7Documento4 pagineExercise 1: CHIR12007 Clinical Assessment and Diagnosis Portfolio Exercises Week 7api-502171898Nessuna valutazione finora
- PCP Week 8 Study Guide QuestionsDocumento3 paginePCP Week 8 Study Guide Questionsapi-502171898Nessuna valutazione finora
- Intro - Facet Joint SyndromeDocumento2 pagineIntro - Facet Joint Syndromeapi-502171898Nessuna valutazione finora
- Week 7 - PCP Study Guide QuestionsDocumento2 pagineWeek 7 - PCP Study Guide Questionsapi-502171898Nessuna valutazione finora
- PCP - Week 2 - QsDocumento4 paginePCP - Week 2 - Qsapi-502171898Nessuna valutazione finora
- Personl ReflectionDocumento1 paginaPersonl Reflectionapi-502171898Nessuna valutazione finora
- Week 6 PCP Study Guide QuestionsDocumento9 pagineWeek 6 PCP Study Guide Questionsapi-502171898Nessuna valutazione finora
- History:: Exercise 1Documento13 pagineHistory:: Exercise 1api-477982644Nessuna valutazione finora
- Portfolio Exercises Week 8Documento3 paginePortfolio Exercises Week 8api-502171898Nessuna valutazione finora
- Portfolio Exercises Week 5Documento4 paginePortfolio Exercises Week 5api-502171898Nessuna valutazione finora
- Week 3 Weekly QsDocumento2 pagineWeek 3 Weekly Qsapi-502171898Nessuna valutazione finora
- PCP - Week 2 - QsDocumento4 paginePCP - Week 2 - Qsapi-502171898100% (1)
- Week 4 Weekly QsDocumento4 pagineWeek 4 Weekly Qsapi-502171898Nessuna valutazione finora
- Week 5 QuestionsDocumento2 pagineWeek 5 Questionsapi-502171898Nessuna valutazione finora
- Cad Week 1 - QsDocumento4 pagineCad Week 1 - Qsapi-502171898Nessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Oral Mucosal Ulceration - A Clinician's Guide To Diagnosis and TreatmentDocumento9 pagineOral Mucosal Ulceration - A Clinician's Guide To Diagnosis and TreatmentAnonymous pvuOXZNessuna valutazione finora
- 01a Calgary Cambridge Framework - BasicDocumento3 pagine01a Calgary Cambridge Framework - BasicJohn Sebastian Bittner SolisNessuna valutazione finora
- EDV022302Documento31 pagineEDV022302Smith Quanco AlexsanderNessuna valutazione finora
- Critical Illness BrochureDocumento2 pagineCritical Illness BrochureBrijesh RaiNessuna valutazione finora
- Advanced Tung Style Acupuncture Vol. 2 - Obstetrics & Gynecology PDFDocumento556 pagineAdvanced Tung Style Acupuncture Vol. 2 - Obstetrics & Gynecology PDFnhung_nguyen_12260% (5)
- 3 Biological Macromolecules: Chapter OutlineDocumento35 pagine3 Biological Macromolecules: Chapter OutlineMarkus EvanNessuna valutazione finora
- Acutepainmanagement: Nabil Moussa,, Orrett E. OgleDocumento13 pagineAcutepainmanagement: Nabil Moussa,, Orrett E. OgleMahmoud AbouelsoudNessuna valutazione finora
- Gambaran Peran Tenaga Kesehatan SebagaiDocumento10 pagineGambaran Peran Tenaga Kesehatan SebagaiNur Rahmy OktavianiNessuna valutazione finora
- Wilson Soap Jordan SimDocumento8 pagineWilson Soap Jordan Simapi-704711481Nessuna valutazione finora
- Logistics HandbookDocumento196 pagineLogistics Handbooknikolaos13100% (1)
- Assigmnt. On Cardiac RehabilitationDocumento15 pagineAssigmnt. On Cardiac RehabilitationSachin Singh100% (1)
- STG 4thDocumento1.239 pagineSTG 4thFentahun workieNessuna valutazione finora
- Ceap Classification For Venous DiseaseDocumento3 pagineCeap Classification For Venous Diseasemyat25Nessuna valutazione finora
- ExodontiaDocumento32 pagineExodontiaahmed amerNessuna valutazione finora
- Crisis ManagementDocumento39 pagineCrisis ManagementbolutifeNessuna valutazione finora
- Incentive SpirometryDocumento5 pagineIncentive Spirometryrachelmores12Nessuna valutazione finora
- Equine Field SurgeryDocumento6 pagineEquine Field SurgeryRuchiNessuna valutazione finora
- Nursing Care Plan and Diagnosis For Substance AbuseDocumento87 pagineNursing Care Plan and Diagnosis For Substance AbuseZohrahLiaqatNessuna valutazione finora
- Oculofacial Plastic and Reconstructive SurgeryDocumento562 pagineOculofacial Plastic and Reconstructive SurgeryGimena Dapena100% (3)
- The Human Circulatory System: Teacher: D.Bleau School: ST Anthony's Secondary SchoolDocumento10 pagineThe Human Circulatory System: Teacher: D.Bleau School: ST Anthony's Secondary SchoolCaiden HenryNessuna valutazione finora
- Abduraham Rayyan-Module-Cardiovascular-SystemDocumento17 pagineAbduraham Rayyan-Module-Cardiovascular-SystemRAYYAN ENIL ABDURAHAMNessuna valutazione finora
- Internal Medicine 1, Conrad FischerDocumento35 pagineInternal Medicine 1, Conrad Fischerdukelist566100% (3)
- Adenomiosis CX ConservadoraDocumento12 pagineAdenomiosis CX Conservadorajuan carlos pradaNessuna valutazione finora
- Freud and AnesthesiaDocumento5 pagineFreud and AnesthesiaRaluca LNessuna valutazione finora
- Tugas Bahasa Inggris Mandiri Speech Class Program Gouty ArthritisDocumento3 pagineTugas Bahasa Inggris Mandiri Speech Class Program Gouty ArthritisWisnu 12Nessuna valutazione finora
- Radiology ReviewerDocumento26 pagineRadiology ReviewerSean Jodi CosepeNessuna valutazione finora
- NCMC103 Prelims ReviewerDocumento13 pagineNCMC103 Prelims ReviewerVeronica ShaneNessuna valutazione finora
- Rheumatology MCQs - Waleed HafizDocumento7 pagineRheumatology MCQs - Waleed Hafizanan100% (1)
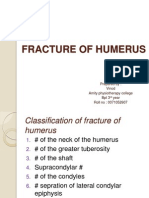
- Fracture of HumerusDocumento56 pagineFracture of HumerusDr. Vinod Gupta100% (2)
- NCM 114-A Module 4Documento8 pagineNCM 114-A Module 4Aycee ElardoNessuna valutazione finora