Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Ultrasound Spectrum of Intraductal Papillary Neoplasms
Caricato da
drrahulsshindeDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Ultrasound Spectrum of Intraductal Papillary Neoplasms
Caricato da
drrahulsshindeCopyright:
Formati disponibili
The British Journal of Radiology, 79 (2006), 843–849
PICTORIAL REVIEW
Ultrasound spectrum in intraductal papillary neoplasms of breast
S GANESAN, MD, G KARTHIK, DNB, M JOSHI, MD, DNB and V DAMODARAN, MS, FRCS
Department of Radiology and Imaging, G.K.N.M Hospital and Research Centre, PN Palayam,
Coimbatore – 641037, India
ABSTRACT. Intraductal papillary neoplasms (IPNs) of breast form a wide spectrum of
pathological changes with benign intraductal papilloma occupying one end of the
spectrum and papillary carcinoma at the other end. Intraductal papillomas are known
to occur anywhere within the ductal system and are broadly classified into central and
peripheral types. Intraductal papillary carcinoma is an uncommon ductal malignancy
forming papillary structures, and these lesions characteristically lack the myoepithelial
layer present in benign papillary neoplasms. Three basic patterns of IPNs are recognized
on ultrasound – intraductal mass with or without ductal dilatation, intracystic mass and
a predominantly solid pattern with the intraductal mass totally filling the duct. Benign
papillomas are known to exhibit calcifications which tend to be extremely dense and
Received 24 November
coarse. IPNs are highly vascular tumours and have a propensity to bleed spontaneously. 2004
A distinct vascular pedicle is identified within the central core of IPNs, with branching Revised 16 May 2005
vessels arborising within the mass. In an older age group, presence of a large solid Accepted 1 June 2005
component and evidence of spontaneous intracystic bleed are more suggestive of
DOI: 10.1259/bjr/69395941
papillary carcinomas than benign papillomas. We have serially studied 42 cases of
intraductal papillary neoplasms with sonomammography and mammography from ’ 2006 The British Institute of
2001 to 2004. Radiology
Intraductal papillomas are common neoplasms with a to a single breast, while bilateral lesions are reported in
relative incidence of 2–3% [1]. In elderly patients, up to 14% of cases [4].
intraductal papillomas are often asymptomatic and are Central papillomas are subareolar in location within a
seen commonly as an incidental finding in biopsy major duct. On macroscopic examination, a papilloma
specimens [2]. Even though intraductal papillomas are appears as a round to oval, small mass usually
primarily benign, these lesions can pose problems in measuring a few millimetres in size within a dilated
view of their similarity to intraductal papillary carci- duct. Larger lesions dilate the duct more and extend
noma clinically, on ultrasound and histologically [3]. along the long axis of the duct presenting a spheroidal
Intraductal papillary carcinoma (IPC) is a rare ductal shape. With ductal obstruction, the dilated duct with a
carcinoma forming papillary structures, with reported papillary lesion may resemble a cyst with an intracystic
incidence of 1–4% of breast carcinomas [4]. These solid component, this variant being termed as an
neoplasms have certain characteristic imaging features intracystic papilloma. Histologically, papillomas show
which help to differentiate these lesions from other focal hyperplastic proliferation of ductal epithelium, having
breast abnormalities. an arborescent growth pattern with branching fibromus-
cular core of myoepithelial and epithelial cells. Lesions
may be pedunculated or broad based [3, 4].
Pathological observations Multiple peripheral papillomas are a rare entity in
which the lesions are located in the peripheral duct
Papillomas are essentially benign proliferations of system within the terminal ductal lobular unit. Several
ductal epithelium. They may occur at any age between adjacent ducts are involved with segmental dilatation of
30 years and 77 years [4], but are commonly seen the ducts, often resulting in a peripherally located mass.
between 30 years and 55 years [3]. They are known to The incidence of nipple discharge is lower in these
occur anywhere within the ductal system and are patients compared with the papillomas in larger ducts.
broadly classified into central and peripheral types. There is an increased risk of carcinoma in peripheral
Central types are usually solitary, while the peripherally papillomas which is directly related to the degree of
located papillomas tend to be multiple within the cellular atypia. Peripheral papillomas are often asso-
terminal duct lobular unit. Lesions are often confined ciated with coexisting malignancy with a reported
incidence of 10–30% [3–6].
Address correspondence to: Dr Karthik Ganesan, Department of
Intraductal papillary carcinoma (IPC) is an uncommon
CT and MRI, Jaslok Hospital and Research Centre, 15, Dr G ductal malignancy forming papillary structures.
Deshmukh Marg, Mumbai – 400026, Maharashtra, India. Histologically papillary carcinoma shows multilayered
The British Journal of Radiology, October 2006 843
S Ganesan, G Karthik, M Joshi and V Damodaran
papillary projections with microscopic frond formations
extending from the vascularized stalks. These lesions
characteristically lack the myoepithelial layer present in
benign lesions. IPCs are reported in patients from 25 years
to 89 years of age with a peak incidence between 40 years
and 75 years [4]. IPCs have a wide spectrum of presenta-
tions varying from a focally invasive lesion with micro-
scopic frond formation to a large mass located within a
cystically dilated duct. Multiple lesions tend to occur
within the same duct with papillary configurations.
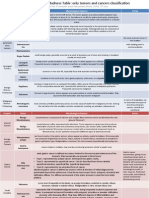
Ultrasound features
Ultrasound features of intraductal papillary neo-
plasms (IPN) primarily depend on the gross macroscopic
appearance of the lesion. Three basic patterns of IPNs are
recognized on ultrasound – intraductal mass with or
without ductal dilatation, intracystic mass and a pre-
dominantly solid pattern with the intraductal mass
totally filling the duct [3, 7]. If the tumour is small, a
focally dilated duct may be the only observation. A
solitary dilated duct, even in the absence of a demon-
strable intraductal mass, is highly suggestive of an
intraductal papilloma, especially, if the patient is Figure 2. Papillary carcinoma. A moderately large mass is
presenting with a serosanguinous nipple discharge [3]. seen to almost totally fill the entire dilated duct. Relatively
Dilated duct with an intraductal mass or a cyst with an hypoechoic debris is seen to fill the peripheral duct adjacent
intracystic solid mass is the hallmark of intraductal to the mass. A short segment of proximal duct is noted at 10–
papillomas (Figure 1). The ductal component may vary 11 o’clock position.
in size from a minimally dilated duct to a large cystically
dilated, obstructed duct. Similarly the intraductal soft
relationship between the mass and the duct on ultra-
tissue component may range in size from a very small
sound and classified the masses into four categories: type
lesion which may be impossible to image to a large mass
I – intraluminal mass; type II – extraductal mass; type III
completely filling the dilated duct or the cyst obscuring
– purely solid mass; type IV – mixed variety [9]. Benign
the ductal or cystic component simulating other
papillomas are known to exhibit calcifications. These
solid masses (Figure 2) [3, 8]. Han et al analysed the
calcifications tend to be dense and coarse (Figures 3–5).
Figure 3. Benign intraductal papilloma with calcification.
Figure 1. A focal mass arising from the ductal wall with Focal dilatation of a solitary duct with intraluminal echo-
relatively narrow base of attachment is present. Note the genic debris. Note small focal mass with dense, coarse
branching pattern and peripheral fronding typical of calcifications in the proximal duct, with ductal obstruction
intraductal papilloma/papillary carcinoma (D-Duct). (small arrows).
844 The British Journal of Radiology, October 2006
Pictorial review: Intraductal papillary neoplasms of breast
(a) (b)
Figure 4. Benign calcified intraductal papilloma with adjacent oil cyst. (a) Small focal mass with coarse, irregular and dense
calcifications (small arrows) adjacent to a cystic mass (C). Echogenic floating debris within the cyst with floating fat-fluid level
(long arrows). (b) Colour flow studies – focal increase in flow within the mass.
Small IPNs are often mammographically negative. A mammography (Figure 7). Calcified IPNs exhibit dense,
minimal to moderate duct dilatation may be observed on central, peripheral or combined form of coarse calcifica-
mammography as a progressively tapering band-like tion similar to those seen in cases of calcified fibro-
density extending from the nipple-subareolar region adenomas (Figure 8). Boonjuwetat et al described the
towards the breast parenchyma for a variable distance mammographic appearances of papillary neoplasms in a
(Figure 6). Larger lesions in a dilated duct may resemble series of 15 cases. They reported that most lesions
any other focal well-circumscribed dense mass on presented as solitary dense masses with no evidence of
(a) (b)
Figure 5. Calcified giant intraductal papilloma. (a) Ultrasound and (b) mammography demonstrate a large, bilobed, densely
calcified mass with distal shadowing (arrows).
The British Journal of Radiology, October 2006 845
S Ganesan, G Karthik, M Joshi and V Damodaran
(a) (b)
(c)
Figure 6. Benign intraductal papilloma. (a) Mammography – oblique band like density along inferolateral quadrant of the left
breast. (b) Ultrasound – focal dilatation of a solitary duct with an intraluminal mass arising from the ductal wall. (c) Doppler
studies – distinct vascular pedicle within the central core with branching vessels arborising within the mass.
calcification in any of these lesions. A few lesions were bleed into the cyst, is virtually suggestive of a mural
mammographically negative either due to the size of the proliferative lesion (Figures 9 and 10) [11]. IPNs have a
lesion or due to the dense parenchymal pattern [10]. characteristic flow pattern on colour flow studies. A
IPNs are highly vascular and have a propensity to bleed distinct vascular pedicle is identified in IPNs within the
spontaneously. Spontaneous haemorrhage into a dilated central core with branching vessels arborising within the
duct characteristically produces a fluid–debris level due to mass. Colour flow studies are sensitive in identifying even
the denser cellular components settling down to the very small IPNs, in view of its characteristic vascularity
dependant position. The supernatant serum is anechoic (Figure 11). Intraductal papillomas and papillary carcino-
while the dependant cellular debris is echogenic. Presence mas have considerable overlap in imaging features and it
of fluid–debris level in a cyst, representing spontaneous may not be possible to differentiate them on ultrasound. In
846 The British Journal of Radiology, October 2006
Pictorial review: Intraductal papillary neoplasms of breast
(a) (b)
Figure 7. (a) Mammography – focal well circumscribed dense mass along the retroareolar region of the left breast.
(b) Ultrasound – large cystic mass with echogenic debris totally filling the cyst.
an older age group presence of a larger solid component vascularity. A cystically dilated duct may resemble a
and evidence of spontaneous intracystic bleed are more simple cyst when the intracystic component is very
suggestive of papillary carcinomas than benign papillo- small. This has to be differentiated from other cystic
mas (Figure 12) [9]. masses like a simple cyst, complex cyst, haematoma,
The differential diagnosis of IPNs depends upon the abscess and fat necrosis. A dilated duct with an
basic imaging appearances. Presence of sectoral dilata- intraductal solid component consisting of a central core
tion of ducts with no demonstrable intraductal mass has and peripheral fronds, with characteristic flow on colour
to be differentiated from mammary duct ectasia, which is flow studies, is virtually diagnostic of IPNs. When the
a chronic inflammatory condition. Bleeding into a duct, mass is large enough to fill the dilated duct or the cyst, it
inspissated material in mammary duct ectasia and ductal may not be possible to delineate the peripheral ductal or
carcinoma in situ may produce dilated ducts with cystic component. These lesions have to be differentiated
intraductal filling defects resembling IPNs. Mammary from other solid masses [3].
ductectasia is often bilateral and tends to affect multiple Fine needle aspiration cytology (FNAC) or core biopsy is
ducts. In intraductal carcinoma, ductal dilatation is required in all cases to arrive at a definitive diagnosis even
unilateral, sectoral and irregular with ductal wall though the imaging findings are suggestive of IPNs.
thickening. Colour flow studies reveal lack of flow in FNAC from non-palpable small masses and from the solid
inspissated intraductal debris. Increased or variable component in large cystic lesions can be performed under
periductal flow may be present in intraductal carcinomas ultrasound control. At our institution, small papillary
while the IPNs reveal the characteristic arborescent lesions within a minimally dilated duct, observed as
The British Journal of Radiology, October 2006 847
S Ganesan, G Karthik, M Joshi and V Damodaran
Figure 10. Colour flow studies in intraductal papillary
neoplasms (IPNs). Distinct vascular pedicle within the central
core with branching vessels arborising within the mass.
a core B3 are the following: papillary lesion, atypical
Figure 8. Mammography. Well circumscribed peripherally
calcified lesion within a progressively tapering band-like intraductal epithelial proliferations, radial scar, lobular
density extending from the nipple-subareolar region neoplasia and fibroepithelial lesions. Lee et al reported that
towards the breast parenchyma. the B3 core group is a more heterogeneous group and has a
lower rate of malignancy on further biopsy. However, they
incidental findings in an asymptomatic patient on sono- concluded that the majority of lesions categorised as B3
mammography are not subjected to FNAC or core biopsy. required excision [12]. Agoff et al evaluated the need for
These patients are advised serial follow up with sono- surgical excision in intraductal papillary neoplasms and
mammography. Larger lesions, lesions with atypical suggested that all such lesions with atypical ductal
characteristics and lesions in symptomatic patients are hyperplasia required excision owing to the high rate of
subjected to FNAC and core biopsy. The criteria for calling associated neoplasia [13]. Although some lesions cate-
gorised as B3 lesions on core biopsy may be re-categorised
Figure 11. Benign intraductal papilloma in a cystically
Figure 9. Intracystic papillary carcinoma. A moderately large dilated duct. Cystically dilated duct with a small focal mass
cystic mass in the central breast region with large intracystic attached to the ductal wall with a narrow base between 10
solid component is present. The mass is attached to the wall and 11 o’clock position. A short segment of dilated proximal
by a broad base and shows irregular branching pattern with duct is identified with dependant echogenic debris with
peripheral fronding. (D – Cystically dilated duct). layering effect forming a fluid-debris level.
848 The British Journal of Radiology, October 2006
Pictorial review: Intraductal papillary neoplasms of breast
on excision biopsy as B2 lesions, all lesions categorised as Sloane JP, editors. Ultrasound diagnosis of breast diseases.
B3 and above are subjected to excision biopsy at our Edinburgh: Churchill Livingstone, 1994:94.
institution. 8. Yang WT, Suen M, Metrewell C. Sonographic features of
benign papillary neoplasms of the breast: review of 22
patients. J Ultrasound Med 1997;16:161–8.
References 9. Han BK, Choe YH, Ko YH, Yang JH, Nam SJ. Benign
1. Cilotti A, Bagnolesi P, Napoli V, et al. Solitary intraductal papillary lesions of the breast: sonographic-pathologic
papilloma of breast. An echographic study of 12 cases. correlation. J Ultrasound Med 1999;18:217–23.
Radiol Med (Torino) 1991;82:617–20. 10. Boonjunwetwat D, Prathombutr A. Imaging of benign
2. Kramer WM, Rush BF. Mammary duct proliferation in the papillary neoplasm of the breast: mammographic, galacto-
elderly: a histopathologic study. Cancer 1973;31:130–7. graphic and sonographic findings. J Med Assoc Thai
3. Tohno E, Cosgrove DO, Sloane JP. Benign processes- 2000;83:832–8.
tumors. In: Tohno E, Cosgrove DO, Sloane JP, editors. 11. Tohno E, Cosgrove DO, Sloane JP. Diagnostic features on
Ultrasound diagnosis of breast diseases. Edinburgh: ultrasound. In: Tohno E, Cosgrove DO, Sloane JP, editors.
Churchill Livingstone, 1994:94–7. Ultrasound diagnosis of breast diseases. Edinburgh:
4. Dahnert W. Breast disorders. In: Dahnert W. Radiology Churchill Livingstone, 1994:58–9.
review manual, 4th edn. Philadelphia, PA: Williams and 12. Lee AH, Denley HE, Pinder SE, Ellis IO, Elston CW, Vujovic
Wilkins, 1999:458–74. P, et al. Excision biopsy findings of patients with breast
5. Haegenson CD. Diseases of the breast, 3rd edn. needle core biopsies reported as suspicious of malignancy
Philadelphia, PA: W.B. Saunders, 1986:136–75. (B4) or lesion of uncertain malignant potential (B3).
6. Murad TM, Contesso G, Mouriesse H. Papillary tumors of Histopathology 2003;42:331–6.
large lactiferous ducts. Cancer 1981;48:122–33. 13. Agoff SN, Lawton TJ. Papillary lesions of the breast with
7. Kasumi F. Ultrasound of breast diseases. Shinohara – and without atypical ductal hyperplasia: can we accurately
shuppan Co., Tokyo, 1983. Cited in Benign processes – predict benign behaviour from core needle biopsy? Am J
Tumors, Intraductal Papilloma, In: Tohno E, Cosgrove DO, Clin Pathol 2004;122:440–3.
The British Journal of Radiology, October 2006 849
Potrebbero piacerti anche
- Gleason ScoreDocumento6 pagineGleason ScoreajeethNessuna valutazione finora
- PAROTID GLAND NEOPLASM IMAGINGDocumento107 paginePAROTID GLAND NEOPLASM IMAGINGigorNessuna valutazione finora
- MD Forensic Medicine Sample Question PapersDocumento12 pagineMD Forensic Medicine Sample Question PapersKumar KP50% (2)
- Carcinoma of NasopharynxDocumento15 pagineCarcinoma of NasopharynxAmeliana KamaludinNessuna valutazione finora
- Histopathology Services GuideDocumento23 pagineHistopathology Services GuidegauravNessuna valutazione finora
- 5 Prelims-Clinical Laboratory LawDocumento58 pagine5 Prelims-Clinical Laboratory LawJay Andrea Vea Dayuday-IsraelNessuna valutazione finora
- Tall Cell Variant Papillary Thyroid Carcinoma in A Pediatricpatient: A Case Report and Review of The LiteratureDocumento6 pagineTall Cell Variant Papillary Thyroid Carcinoma in A Pediatricpatient: A Case Report and Review of The LiteratureIJAR JOURNALNessuna valutazione finora
- Polymorphous Low Grade Adenocarcinoma - Case Report and Review of LiteratureDocumento6 paginePolymorphous Low Grade Adenocarcinoma - Case Report and Review of LiteratureeditorompjNessuna valutazione finora
- Aruns PL - Ade FinalDocumento9 pagineAruns PL - Ade FinaldrarunsinghNessuna valutazione finora
- Canine Perineal TumoursDocumento11 pagineCanine Perineal TumoursSUSANA SAM RODRIGUEZNessuna valutazione finora
- 49 Kishor EtalDocumento4 pagine49 Kishor EtaleditorijmrhsNessuna valutazione finora
- Field Cancerization: Evidence for Multicentric Origin in Oral Squamous Cell CarcinomaDocumento6 pagineField Cancerization: Evidence for Multicentric Origin in Oral Squamous Cell CarcinomaSandipta MitraNessuna valutazione finora
- Sureka Pleural TumorsDocumento8 pagineSureka Pleural Tumorslaila.forestaNessuna valutazione finora
- The Bizarre Case of Warthins Tumor in Submandibular Gland-Case ReportDocumento9 pagineThe Bizarre Case of Warthins Tumor in Submandibular Gland-Case ReportInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Case Report 2022Documento5 pagineCase Report 2022Reyes Ivan García CuevasNessuna valutazione finora
- Adenosquamous Carcinoma in Buccal Mucosa-A Case: KeywordsDocumento3 pagineAdenosquamous Carcinoma in Buccal Mucosa-A Case: KeywordsPatrico Rillah SetiawanNessuna valutazione finora
- Pictorial Review Pleural TumorsDocumento8 paginePictorial Review Pleural TumorsDinda Anita SeptianaNessuna valutazione finora
- Clinical Case CAPDocumento82 pagineClinical Case CAPIna GargNessuna valutazione finora
- ENGLISH REFARAT 3.2 - Sem 5 - Septina - Malignant Tumours With Follicular DifferentiationDocumento28 pagineENGLISH REFARAT 3.2 - Sem 5 - Septina - Malignant Tumours With Follicular DifferentiationAffan Akbar TalamiNessuna valutazione finora
- Normal Mediastinal Anatomy, Pathologies and Diagnostic MethodsDocumento9 pagineNormal Mediastinal Anatomy, Pathologies and Diagnostic MethodsJuma AwarNessuna valutazione finora
- (12204749 - Romanian Journal of Internal Medicine) Multiple Histological Subtypes of Dermatofibrosarcoma Protuberans Occurring in The Same TumorDocumento10 pagine(12204749 - Romanian Journal of Internal Medicine) Multiple Histological Subtypes of Dermatofibrosarcoma Protuberans Occurring in The Same TumordrelvNessuna valutazione finora
- Malignant Epithelial Non-Odontogenic Tumors 2Documento11 pagineMalignant Epithelial Non-Odontogenic Tumors 2samamustafa.2003Nessuna valutazione finora
- (WWW - Entrance Exam - Net) QpmathDocumento7 pagine(WWW - Entrance Exam - Net) QpmathdennisNessuna valutazione finora
- Parotid Gland Tumor Case ReportDocumento4 pagineParotid Gland Tumor Case ReportmitaNessuna valutazione finora
- 1 PBDocumento4 pagine1 PBLidia CampeanNessuna valutazione finora
- Friedberg 1940Documento14 pagineFriedberg 1940YPramudiyaNessuna valutazione finora
- Primary Fibrosarcoma of Breast: A Rare Case Presentation: Cash ReportDocumento4 paginePrimary Fibrosarcoma of Breast: A Rare Case Presentation: Cash ReportBastiaanNessuna valutazione finora
- Table 1 Benign Tumors in The 2017 WHO Classification of Tumors of The Nasal Cavity, Paranasal SinusesDocumento7 pagineTable 1 Benign Tumors in The 2017 WHO Classification of Tumors of The Nasal Cavity, Paranasal SinusesNazliah SyarbinNessuna valutazione finora
- ReferatDocumento35 pagineReferatYuni AurraNessuna valutazione finora
- Benign Paratesticlar Cyst - A Mysterical FindingDocumento2 pagineBenign Paratesticlar Cyst - A Mysterical FindingInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Tuberculous Mastitis A Case ReportDocumento4 pagineTuberculous Mastitis A Case ReportLmao DNessuna valutazione finora
- CA Sinonasal PDFDocumento2 pagineCA Sinonasal PDFGek DewiNessuna valutazione finora
- Unusual Variants of Fibroadenoma Breast Diagnosed on CytologyDocumento5 pagineUnusual Variants of Fibroadenoma Breast Diagnosed on CytologyEnvhy WinaNessuna valutazione finora
- Unusually Large Mandibular Lipoma CaseDocumento4 pagineUnusually Large Mandibular Lipoma CaseBruna FerreiraNessuna valutazione finora
- Practical No 28 - Respiratory SystemDocumento8 paginePractical No 28 - Respiratory Systemkartik.patil151106Nessuna valutazione finora
- Updates on Tumors of the Anal CanalDocumento11 pagineUpdates on Tumors of the Anal CanalSuparna NareshNessuna valutazione finora
- Fibrolipoma On Upper Eyelid in Child: Rafael Corredor-Osorio Nelly Ramos-Pineda María Eugenia OrellanaDocumento4 pagineFibrolipoma On Upper Eyelid in Child: Rafael Corredor-Osorio Nelly Ramos-Pineda María Eugenia OrellanaAdjhy Aji AchmadNessuna valutazione finora
- Basal Cell AdenomawDocumento3 pagineBasal Cell AdenomawDrRobin SabharwalNessuna valutazione finora
- 6 Endometrial Polyp - Libre PathologyDocumento4 pagine6 Endometrial Polyp - Libre PathologyfadoNessuna valutazione finora
- Review For The 2° Semester Exam Alessandro Mo6a, UVVG, 3 YearDocumento9 pagineReview For The 2° Semester Exam Alessandro Mo6a, UVVG, 3 Yeardjxela89Nessuna valutazione finora
- Nevus Spitz Diagnostic ChallengesDocumento6 pagineNevus Spitz Diagnostic ChallengesCristi PopescuNessuna valutazione finora
- Aisha Tabassum EtalDocumento4 pagineAisha Tabassum EtaleditorijmrhsNessuna valutazione finora
- 1 Tmu - JD - 039 PDFDocumento4 pagine1 Tmu - JD - 039 PDFKristina SabuNessuna valutazione finora
- 1 Tmu - JD - 039Documento4 pagine1 Tmu - JD - 039Hasan BlackNessuna valutazione finora
- Interactive Microscopy Session:: Second Edition: Modern Surgical Pathology Through The Expert Eyes of Apss-UscapDocumento10 pagineInteractive Microscopy Session:: Second Edition: Modern Surgical Pathology Through The Expert Eyes of Apss-UscapalfonsoNessuna valutazione finora
- Pleomorphic Adenoma of A Minor Salivary Gland-Report of A CaseDocumento3 paginePleomorphic Adenoma of A Minor Salivary Gland-Report of A CasePriya BabyNessuna valutazione finora
- World's Largest Science, Technology & Medicine Open Access Book PublisherDocumento21 pagineWorld's Largest Science, Technology & Medicine Open Access Book PublisherNicoleta MunteanuNessuna valutazione finora
- PathReport4 PDFDocumento4 paginePathReport4 PDFGohar Ali UsmanNessuna valutazione finora
- Usg Imaging: Cervical and Endometrial PolypsDocumento10 pagineUsg Imaging: Cervical and Endometrial Polypsnajihah muzairi souzaNessuna valutazione finora
- Polymorphous Low Grade Adenocarcinoma of The Parotid in A TeenagerDocumento4 paginePolymorphous Low Grade Adenocarcinoma of The Parotid in A Teenagersara luciaNessuna valutazione finora
- 45syam EtalDocumento3 pagine45syam EtaleditorijmrhsNessuna valutazione finora
- FibrolipomaDocumento5 pagineFibrolipomaNarendra ChaudhariNessuna valutazione finora
- Mucinous Cystadenoma of The AppendixDocumento3 pagineMucinous Cystadenoma of The AppendixKriti KumariNessuna valutazione finora
- Resident Short Reviews: Adenocarcinoma of the Urinary BladderDocumento5 pagineResident Short Reviews: Adenocarcinoma of the Urinary BladdererikafebriyanarNessuna valutazione finora
- Imaging Features of Benign Mass Lesions in The NasDocumento21 pagineImaging Features of Benign Mass Lesions in The NasJose ManuelNessuna valutazione finora
- Huge Cervical Swelling Hiding A Tonsillated Cyst About 01caseDocumento3 pagineHuge Cervical Swelling Hiding A Tonsillated Cyst About 01caseInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Adenoid Cystic Carcinoma of Hard Palate: A Case ReportDocumento5 pagineAdenoid Cystic Carcinoma of Hard Palate: A Case ReportHemant GuptaNessuna valutazione finora
- Benign Extrapleural Solitary Fibrous Tumorofthe Headand NeckDocumento7 pagineBenign Extrapleural Solitary Fibrous Tumorofthe Headand NeckCara Danielle PabellanoNessuna valutazione finora
- Pleomorphic Adenoma 5Documento6 paginePleomorphic Adenoma 5Mita NurizaNessuna valutazione finora
- Breast Fibroadenoma Diagnosis GuideDocumento12 pagineBreast Fibroadenoma Diagnosis GuideRahman Az ZamNessuna valutazione finora
- Intraductal Papillary Carcinoma Payudara: Temuan Pada Pencitraan UltrasonografiDocumento6 pagineIntraductal Papillary Carcinoma Payudara: Temuan Pada Pencitraan UltrasonografiBastiaanNessuna valutazione finora
- Pleomorphic Sarcoma in Paratesticular Region: Case Report Open AccessDocumento5 paginePleomorphic Sarcoma in Paratesticular Region: Case Report Open AccessNurulDiniaPutriNessuna valutazione finora
- Diffuse Multiple Giant Adenomyomatous Endometrial Polyps: A Rare Case ReportDocumento3 pagineDiffuse Multiple Giant Adenomyomatous Endometrial Polyps: A Rare Case ReportNuke YolandaNessuna valutazione finora
- Salivary Gland Cancer: From Diagnosis to Tailored TreatmentDa EverandSalivary Gland Cancer: From Diagnosis to Tailored TreatmentLisa LicitraNessuna valutazione finora
- CT Main Pulm Art DiameterDocumento3 pagineCT Main Pulm Art DiameterdrrahulsshindeNessuna valutazione finora
- Contrast Media and The Kidney European Society ofDocumento6 pagineContrast Media and The Kidney European Society ofdrrahulsshindeNessuna valutazione finora
- Adult Intussusception CT DiagnosisDocumento6 pagineAdult Intussusception CT DiagnosisdrrahulsshindeNessuna valutazione finora
- Lobar AtelectasisDocumento9 pagineLobar AtelectasisGusti Ngurah PNessuna valutazione finora
- Scrotal Calci CationDocumento6 pagineScrotal Calci CationdrrahulsshindeNessuna valutazione finora
- Soft Tissue Tumours and Mass-Like Lesions of The Chest WallDocumento7 pagineSoft Tissue Tumours and Mass-Like Lesions of The Chest WalldrrahulsshindeNessuna valutazione finora
- Colour Doppler Ultrasound Ow Patterns in The Portal VeinDocumento11 pagineColour Doppler Ultrasound Ow Patterns in The Portal VeindrrahulsshindeNessuna valutazione finora
- Sister Mary Joseph NoduleDocumento4 pagineSister Mary Joseph NoduledrrahulsshindeNessuna valutazione finora
- Trigeminal Nerve Anatomy and PathologyDocumento10 pagineTrigeminal Nerve Anatomy and PathologydrrahulsshindeNessuna valutazione finora
- Imaging Features of Pelvic EndometriosisDocumento7 pagineImaging Features of Pelvic EndometriosisdrrahulsshindeNessuna valutazione finora
- Female Genital Tuberculosis HysterosalpingiographyDocumento6 pagineFemale Genital Tuberculosis HysterosalpingiographydrrahulsshindeNessuna valutazione finora
- Imaging of The Petrous ApexDocumento9 pagineImaging of The Petrous ApexdrrahulsshindeNessuna valutazione finora
- Spinal Ultrasound in InfantsDocumento9 pagineSpinal Ultrasound in InfantsdrrahulsshindeNessuna valutazione finora
- Cancer Risks From Diagnostic RadiologyDocumento17 pagineCancer Risks From Diagnostic RadiologydrrahulsshindeNessuna valutazione finora
- Ultrasound Evaluation of The Brosis Stage in Chronic LiverDocumento9 pagineUltrasound Evaluation of The Brosis Stage in Chronic LiverdrrahulsshindeNessuna valutazione finora
- CT of Duodenal PathologyDocumento7 pagineCT of Duodenal PathologydrrahulsshindeNessuna valutazione finora
- CT Findings in Pulmonary TuberculosisDocumento13 pagineCT Findings in Pulmonary TuberculosisdrrahulsshindeNessuna valutazione finora
- Vesicoureteric Reflux in The AdultDocumento9 pagineVesicoureteric Reflux in The AdultdrrahulsshindeNessuna valutazione finora
- Contrast Media and The Kidney European Society ofDocumento6 pagineContrast Media and The Kidney European Society ofdrrahulsshindeNessuna valutazione finora
- Trigeminal Nerve Anatomy and PathologyDocumento10 pagineTrigeminal Nerve Anatomy and PathologydrrahulsshindeNessuna valutazione finora
- CT of A Thickened-Wall Gall BladderDocumento7 pagineCT of A Thickened-Wall Gall BladderdrrahulsshindeNessuna valutazione finora
- Tubeless Hypotonic DuodenographyDocumento12 pagineTubeless Hypotonic DuodenographydrrahulsshindeNessuna valutazione finora
- Radiographic Assessment of CTEVDocumento6 pagineRadiographic Assessment of CTEVdrrahulsshindeNessuna valutazione finora
- Imaging Features of Pelvic EndometriosisDocumento7 pagineImaging Features of Pelvic EndometriosisdrrahulsshindeNessuna valutazione finora
- CT of Thoracic Lymph Nodes AnatomyDocumento7 pagineCT of Thoracic Lymph Nodes AnatomydrrahulsshindeNessuna valutazione finora
- CT Scanning of Middle Ear CholesteatomaDocumento6 pagineCT Scanning of Middle Ear CholesteatomadrrahulsshindeNessuna valutazione finora
- Cancer Risks From Diagnostic RadiologyDocumento17 pagineCancer Risks From Diagnostic RadiologydrrahulsshindeNessuna valutazione finora
- Surgical Anatomy PF PNSDocumento11 pagineSurgical Anatomy PF PNSdrrahulsshindeNessuna valutazione finora
- Multiplanar Sinus CT AJRDocumento10 pagineMultiplanar Sinus CT AJRdrrahulsshindeNessuna valutazione finora
- Role of Intraoperative Imprint Cytology in Diagnosis ofDocumento3 pagineRole of Intraoperative Imprint Cytology in Diagnosis ofNorman AjxNessuna valutazione finora
- Histochemistry: Historical Development and Current Use in PathologyDocumento10 pagineHistochemistry: Historical Development and Current Use in PathologyiuventasNessuna valutazione finora
- II. Subdivisions of PathologyDocumento2 pagineII. Subdivisions of PathologySiegNessuna valutazione finora
- F. Clinical Laboratory Laws (AO 2007-0027)Documento93 pagineF. Clinical Laboratory Laws (AO 2007-0027)Armie Joy ManingatNessuna valutazione finora
- Kanker Payudara PDFDocumento20 pagineKanker Payudara PDFbabehNessuna valutazione finora
- Carcinomul Bazoscuamos (Metatipic) Basosquamous (Metatypical) CarcinomaDocumento4 pagineCarcinomul Bazoscuamos (Metatipic) Basosquamous (Metatypical) CarcinomaAnca BulaiNessuna valutazione finora
- Medtech laws & bioethics document summarizedDocumento10 pagineMedtech laws & bioethics document summarizedMarjan CalzadoNessuna valutazione finora
- Tissue Processing and StainingDocumento29 pagineTissue Processing and StainingMuhammad kamran ameerNessuna valutazione finora
- Frozen SectionDocumento9 pagineFrozen SectionBabatunde AjibolaNessuna valutazione finora
- Ra4688 Reyes, Jeanneclaire Mmls2-1Documento46 pagineRa4688 Reyes, Jeanneclaire Mmls2-1Jeanne ClaireNessuna valutazione finora
- K - 2 Gambar Histopatologi (Ilmu Penyakit Kulit-Kelamin)Documento14 pagineK - 2 Gambar Histopatologi (Ilmu Penyakit Kulit-Kelamin)Monika AyuningrumNessuna valutazione finora
- Aims, Goals and Methods of Pathological AnatomyDocumento11 pagineAims, Goals and Methods of Pathological AnatomydangerpragyeshNessuna valutazione finora
- Trans EsDocumento27 pagineTrans Espenales.andrei.oNessuna valutazione finora
- Lab 4 DIFFERENTIAL & Special STAINDocumento21 pagineLab 4 DIFFERENTIAL & Special STAINAAANessuna valutazione finora
- Utility of Fine Needle Aspiration Cytology of Lymph Nodes: Dr. Ripunjaya Mohanty, Dr. Anne WilkinsonDocumento6 pagineUtility of Fine Needle Aspiration Cytology of Lymph Nodes: Dr. Ripunjaya Mohanty, Dr. Anne WilkinsonAmanda AlmaNessuna valutazione finora
- Ritcha Saxena, MD Forensic PathologyDocumento2 pagineRitcha Saxena, MD Forensic PathologyDr. Ritcha SaxenaNessuna valutazione finora
- Contoh EBLDocumento4 pagineContoh EBLsalsabila fabianca alsaidNessuna valutazione finora
- Nabl 600Documento350 pagineNabl 600Gian Pierre CuevaNessuna valutazione finora
- Pathology: HematologyDocumento1 paginaPathology: HematologyMubashar AliNessuna valutazione finora
- 8 RA 4688 (Clinical Laboratory Law)Documento32 pagine8 RA 4688 (Clinical Laboratory Law)AIRRA CLAIRE ALVAREZNessuna valutazione finora
- Daftar Pustaka Sitologi Massa LeherDocumento3 pagineDaftar Pustaka Sitologi Massa LeherRegina YunitaNessuna valutazione finora
- Pathways Winter 2015Documento24 paginePathways Winter 2015taliancichNessuna valutazione finora
- MEDTECH LAW: KEY POINTS AND ISSUESDocumento14 pagineMEDTECH LAW: KEY POINTS AND ISSUESMONICA VILLANUEVANessuna valutazione finora
- CMSA Regulations for Fellowship Examination in Anatomical PathologyDocumento10 pagineCMSA Regulations for Fellowship Examination in Anatomical PathologymatentenNessuna valutazione finora
- Journal Reading: "A Case of Hanging With Creeper in Secluded Place: Suicide or Homicide?"Documento21 pagineJournal Reading: "A Case of Hanging With Creeper in Secluded Place: Suicide or Homicide?"Azam alausyNessuna valutazione finora
- MT Laws and Lab ManDocumento8 pagineMT Laws and Lab ManGene Narune GaronitaNessuna valutazione finora