Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Spinal Ultrasound in Infants
Caricato da
drrahulsshindeTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Spinal Ultrasound in Infants
Caricato da
drrahulsshindeCopyright:
Formati disponibili
The British Journal of Radiology, 75 (2002), 384–392 E 2002 The British Institute of Radiology
Pictorial review
Spinal ultrasound in infants
E A DICK, FRCR, K PATEL, ARDMS, C M OWENS, FRCR and R DE BRUYN, FRCR
Department of Radiology, Great Ormond Street Hospital for Children, Great Ormond Street,
London WC1N 3JH, UK
Abstract. This paper discusses the indications for spinal ultrasound, including its advantages and
disadvantages compared with spinal MRI. The features and ultrasound findings both in normal
infants and in those with spinal dysraphism are reviewed.
Spinal ultrasound (SUS) is becoming increas- practice [9, 10]. The examination is performed
ingly accepted as a first line screening test in using a 7.5–10 MHz linear probe in both the
neonates suspected of spinal dysraphism (SD) sagittal and axial plane along the entire spine.
[1, 2]. SUS can be useful in detecting tumours, Ideally the patient is laid prone on a pillow
vascular malformations and cases of trauma; with the neck flexed for craniocervical junction
however, as the indication in most cases is to imaging, but imaging with the patient in the
exclude SD, this article will concentrate on this decubitus position is also feasible. The examina-
group of abnormalities [2–4]. The advantages of tion can be performed in the Ultrasound
SUS are not only a diagnostic sensitivity equal to Department or on the ward with a portable
MRI [2] but that, unlike MRI, SUS can be machine. No sedation is necessary.
performed portably, without the need for sedation SUS is possible in the neonate owing to a lack
or general anaesthesia. In addition, MRI is highly of ossification of the predominantly cartilaginous
dependent on factors affecting resolution, includ- posterior arch of the spine [11, 12]. The quality of
ing patient movement, physiological motion from ultrasound assessment decreases after the first
cerebral spinal fluid (CSF) pulsation and vascular 3–4 months of life as posterior spinous elements
flow, factors that do not affect SUS [5]. New ossify, and in most children SUS is not possible
generation high frequency ultrasound machines beyond 6 months of age. However, the persisting
with extended field of view capability now permit acoustic window in children with posterior spinal
imaging of high diagnostic quality in young defects of SD enables ultrasound to be performed
babies. at any age [11, 12].
SD refers to abnormalities with imperfect fusion The normal neonatal spinal cord is displayed
of the midline neural and bony structures. It is on ultrasound as a tubular hypoechoic structure
the most common congenital central nervous with hyperechoic walls (Figure 1). The central
system abnormality, with myelomeningoceles canal is hyperechoic, the so-called central echo
occurring in up to 2 per 1000 live births in some complex [13]. The subarachnoid space surround-
studies, although the incidence in the Western ing the cord is hypoechoic. The caudal end of the
world is now likely to be lower [5, 6]. In infants spinal cord corresponds with the conus medul-
with occult SD, early diagnosis may be useful, as SD laris, which continues into the filum terminale.
may lead to distortion of the spinal cord and The cauda equina is seen as echogenic linear
nerve roots with growth, resulting in neurological structures surrounding a hyperechoic filum ter-
sequelae in the lower extremities, the lower urinary minale. The vertebral bodies are seen as echogenic
tract and the gastrointestinal tract. Because structures ventral to the spinal cord. Particular
some paediatric neurosurgeons believe that early features to note are:
surgical correction of SD may avoid these sequelae,
early diagnosis of SD could be important [7, 8]. (i) The level of the conus medullaris. In term
infants the tip of the conus medullaris
How to do it and what to look for normally lies above the mid level of the L2
vertebral body although there is a large range
SUS was first proposed in the early 1980s but of normality (from T10/11 to L2/3) [14]. In
it has taken some time to enter routine clinical pre-term infants the tip of the conus lies
between L2 and L4, i.e. the level of the conus
Received 5 January 2001 and in revised form 2 May moves proximally with age [15]. A low-lying
2001, accepted 25 June 2001.
cord may imply tethering.
Address correspondence to Dr R de Bruyn. (ii) The position of the cord in a dorsal/ventral
384 The British Journal of Radiology, April 2002
Pictorial review: Spinal ultrasound in infants
or anterior/posterior orientation. In normal of 38 cases. In five cases, SUS depicted the main
infants the cord lies a third to half way abnormality but MRI gave additional informa-
between the anterior and posterior walls of tion. Wherever SUS was normal, MRI was also
the spinal canal. If the cord lies more normal, i.e. SUS had a sensitivity of 100%.
posteriorly, tethering should be suspected Current literature therefore suggests that SUS
(Figure 2). may be used as a primary screening tool, with
(iii) The presence of normal pulsatile movement MRI being performed in any case where SUS
of the cord and nerve roots (tethering leads revealed an abnormality [1, 2, 24].
to an absence of pulsatility).
(iv) The thickness of the filum terminale (normal Embryogenesis
2 mm or less [16]).
The defects of SD occur in the first 8.5 weeks
Viewed axially, the spinal cord is hypoechoic of pre-natal life, as the fetal nervous system de-
and round or oval-shaped, lying within the velops. The neural tube and the subsequent spinal
anechoic subarachnoid space (Figure 3a). The cord arise from ectodermal cells. The surface
spinal cord is fixed by dentate ligaments that ectoderm separates from the neural tube, with
pass laterally from the spinal cord. Echogenic mesoderm coming to lie between the neural tube
nerve roots are seen below the level of L2 and the ectoderm. The mesoderm forms the bony
(Figure 3b). spine, meninges and muscle. Incomplete separa-
tion of the neural tube from the ectoderm may
result in cord tethering, diastematomyelia or a
Patient selection: who should be dermal sinus. Premature separation of the cu-
investigated for SD taneous ectoderm from the neural tube can result
Spinal MRI is a limited resource and cannot be in abnormal mesenchymal elements such as
used as a screening tool. Ward et al [17] suggested lipomas, forming between the neural tube and
that only patients with a clinically demonstrable skin [16]. If the neural tube fails to fold and fuse
neurological abnormality, such as increased tone in the midline, defects of posterior SD such as a
or hemiplegia, should be investigated for SD myelomeningocele occur. Finally, disorders of the
using MRI, as they found that only those with distal cord (so called ‘‘caudal cell mass’’) lead to
clinically demonstrable neurological defects demon- fibrolipomas of the filum terminale.
strated an abnormality on MRI. Other authors
concur with this suggestion. Schwend et al [18] Classification of SD
found that all patients who needed neurosurgical
SD can be classified into non-skin-covered,
intervention could be identified by abnormal
skin-covered and occult abnormalities (see
neurological findings on clinical examination.
Table 1) [5].
SUS has the advantage over MRI that it is a
less restricted resource and can therefore be used
as a screening tool in all babies suspected of SD. Low cord without tethering (Figure 4)
SD may be suspected if the infant has: (i) a In a term infant, the conus should lie above the
neurological deficit; (ii) cutaneous stigmata, such level of mid L2. The clinical significance of a low
as a haemangioma, sacral pit or tuft of hair; cord unaccompanied by any other abnormality is
or (iii) other abnormalities associated with SD unknown [7].
such as cloacal exstrophy [19] or anorectal or
sacral abnormalities and agenesis [12, 20]. Current Table 1. Classification of common types of spinal
Royal College of Radiologists guidelines are that dysraphism (SD)
all neonates with a hairy patch or sacral dimple
SD without a back mass (SD occulta)
should undergo SUS [21]. However, while more low cord
than 90% of patients with occult SD have a tethered cord
cutaneous abnormality over the lower spine [22], diastematomyelia
a cutaneous marker may have a low yield in anterior sacral meningocele
predicting the presence of a clinically significant spinal lipoma
abnormality. In a recent review of 200 SUS SD with a skin-covered back mass
examinations performed over an 11-year period, lipomyelomeningocele
SD was found in less than 1% of cases when a myelocystocele
cutaneous marker was the only clinically detected SD with a non-skin-covered back mass
abnormality [23]. myelomeningocele/myelocele
The diagnostic value of SUS has been shown to
Adapted with kind permission from Byrd SE, Darling CF,
be equal to MRI [2]. Rohrschneider et al [2] found McLone DG, Tomita T. MR imaging of the pediatric spine.
that SUS exactly correlated with MRI in 32 out Magn Reson Imaging Clin N Am 1996;4:797–833.
The British Journal of Radiology, April 2002 385
E A Dick, K Patel, C M Owens and R de Bruyn
Tethered cord syndrome (Figure 2) lipoma (4%) [25]. Unlike most other forms of SD,
which are commonest in the lumbar spine, spinal
In tethered cord syndrome, the conus is low,
lipomas are most commonly found in the cervical
the spinal cord is often displaced dorsally, there is
and thoracic spine. They can be large and may
a lack of normal spinal cord pulsatility as well as
cause local compression. Spinal lipomas are
thickening of the filum terminale (.2 mm) [6].
usually dorsal and subpial in situation. Where
This thickening may be fibrous or lipomatous in
they are associated with myeloceles and myelo-
nature.
meningoceles, the lipomatous mass is in conti-
nuity with a spinal cord that has not fused in the
Diastematomyelia (Figure 5) midline. In these cases the lipoma extends dorsally
through a spina bifida defect and is flush with
Diastematomyelia consists of partial or complete
the skin (lipomyelocele) or herniates beyond the
sagittal clefting of the spinal cord into symmetrical
skin (lipomyelomeningocele, associated with an
or assymetrical hemicords, which usually re-unite
enlarged dorsal subarachnoid space; Figure 7e).
caudally. Each segment has a central canal, and
50% of patients with lipomyeloceles or lipo-
dorsal and ventral nerve roots. In 50–60% of cases
meningoceles present with a lumbar soft tissue
the hemicords are contained in a single dural sac and
mass and 50% present with lower limb neurology
arachnoid covering without a dividing spur (type A)
or bladder symptoms, often in later childhood [8].
[6]. In 40–50% of cases (type B), each hemicord has
a separate dural and arachnoid covering with a
spur or septum between, which may be bony, Myelocystocele
cartilaginous or fibrous in nature. SUS in the Myelocystoceles are rare subtypes of myelo-
axial plane identifies the two hemicords and also meningoceles where the central canal dilates and
the spur, which is usually echogenic. Diastem- herniates through the posterior spinal bifida
atomyelia occurs most commonly in the thoraco- defect. The mass is covered by skin. Hydro-
lumbar region. 50–75% of patients have cutaneous myelia is present in all cases. On ultrasound,
stigmata at the site of diastematomyelia [16]. characteristic flaring of the anechoic central canal
Diastematomyelia is commonly associated with as it enlarges into a cystic mass is seen. Continuity
tethering in around 75% of patients and syringo- with the central canal is the key feature in
hydromyelia in around half of patients. Both differentiating it from myelomeningocele [16].
these abnormalities must therefore be looked for
and excluded in the presence of diastematomyelia.
Meningocele and myelomeningocele
(Figures 8a–c)
Anterior sacral meningocele (Figures 6a–c)
These are two of the most common SD
In anterior sacral meningoceles, there is hernia-
abnormalities, occurring in up to 2 of 1000 live
tion of a dural sac containing CSF through a
births [25]. They arise from localized failure of
bony sacral or coccygeal defect. The meningoceles
fusion of the neural folds dorsally. In meningocele
may be isolated or associated with neuro-
there is herniation of distended spinal meninges
fibromatosis or Marfans syndrome. Patients
but not neural tissue through a dysraphic spine.
may be asymptomatic or may present with
In myelomeningocele, portions of the spinal cord
bladder/bowel dysfunction or a pelvic mass.
and nerve roots lie within the sac. These
Plain radiographs often show a sacral defect.
anomalies occur most commonly at the lumbo-
SUS demonstrates an anechoic meningocele
sacral level. Ultrasound shows an anechoic,
anterior to the sacrum. MRI confirms that it is
lobulated meningocele in continuity with a
fluid-filled with signal isointense to CSF. The
tethered, low lying spinal cord. Myelomeningoceles
meningocele may be unilocular or multilocular.
and myeloceles are both associated with cord
Associated cord tethering and lipomata should be
tethering [5, 16].
looked for [16].
Myelocele
Spinal lipoma (Figures 7a–d), including
lipomyelomeningocele (Figure 7e)
In myeloceles, the spinal cord is openly exposed
Spinal lipomas comprise 20–50% of occult SD to the skin surface with the central canal lying
[16]. Lipomas are highly echogenic and easily open. There is no skin closure in the midline. This
discernible on ultrasound [13]. They are classified occurs most commonly in the lumbosacral region.
into the following groups: (i) lipomyelocele or Surgical repair is performed within 48 h of birth
lipomyelomeningocele (84%); (ii) fibrolipoma of because of the high risk of infection. Pre-operative
the filum terminale (12%) often associated with a imaging is rarely performed and should be
tethered cord (see Figures 7a–d); or (iii) intradural avoided owing to the risk of infection [25].
386 The British Journal of Radiology, April 2002
Pictorial review: Spinal ultrasound in infants
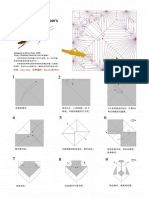
Figure 1. Normal sagittal neonatal spine on an extended field of view ultrasound. The L1 vertebral body is indi-
cated. Note the position of the cord in an anteroposterior direction as well as the echogenic nerve roots extending
beyond the tip of the conus medullaris. The spinal cord lies between short arrows. Hyperechoic central canal
(long arrow). A, anterior; P, posterior; S, superior; I, inferior. (Reproduced with kind permission from Dick EA,
de Bruyn R, Patel K, Owens CM. Spinal ultrasound in cloacal exstrophy. Clin Radiol 2001;56:289–94.
Figure 2. Sagittal spinal ultrasound
showing tethering of the cord with
dorsal displacement. The conus
medullaris lies at the level of L5
(long arrow). Cutaneous sacral
dimple is seen (short arrow).
The British Journal of Radiology, April 2002 387
E A Dick, K Patel, C M Owens and R de Bruyn
(a) (b)
Figure 3. (a) Normal axial neonatal spine at the level of T12 showing the dentate ligaments extending laterally
from the spinal cord (arrow). (b) Normal axial neonatal spine at the level of L3 showing echogenic nerve roots.
Left-sided nerve roots arrowed.
Figure 4. Sagittal spinal ultrasound showing a low Figure 5. Axial spinal ultrasound showing diastemato-
cord but no tethering. The tip of the conus lies at myelia. Both hemicords are arrowed. An echogenic
the lower level of L2 but the cord is not dorsally spur lies between the two hemicords.
displaced.
388 The British Journal of Radiology, April 2002
Pictorial review: Spinal ultrasound in infants
(a) (b)
(c)
Figure 6. (a) Plain radiograph showing partial absence of the right sacrum and coccyx (arrow) in a patient with
an anterior meningocele. (b) Sagittal spinal ultrasound (same patient) demonstrates an anechoic unilocular menin-
gocele anterior to the sacrum (long arrow), anterior to the inferior portion of the sacrum (short arrow).
(c) Sagittal T1 weighted MRI (same patient) demonstrates a low signal meningocele (arrow) anterior to the inferior
portion of the sacrum.
The British Journal of Radiology, April 2002 389
E A Dick, K Patel, C M Owens and R de Bruyn
(b)
(a) (c)
(d) (e)
Figure 7. (a) Sagittal spinal ultrasound showing lipoma of the filum terminale (arrow). (b) Sagittal T1 weighted
MRI (same patient) demonstrates high signal lipoma (arrow). (c) Sagittal T2 weighted MRI (same patient)
demonstrates lipoma of intermediate signal, and confirms that the cord is tethered, extending to level L5.
(d) Sagittal line diagram showing features of lipoma of the filum terminale. The lipoma (L) tethers a low lying
spinal cord (large arrow). The intradural lipoma is separated from subcutaneous fat of the back by a tissue plane
(small arrows). (e) Sagittal line diagram showing features of lipomyelomeningocele in the lumbosacral region.
There is a large dysraphic defect in the neural arches and a skin-covered herniated sac composed of fat that is
contiguous with the subcutaneous fat (asterisks) and a low lying tethered spinal cord (arrows). ((a–c) reproduced
with kind permission from Dick EA, de Bruyn R, Patel K, Owens CM. Spinal ultrasound in cloacal exstrophy.
Clin Radiol 2001;56:289–94. (d,e) reproduced with kind permission from Byrd SE, Darling CF, McLone DG,
Tomita T. MR imaging of the pediatric spine. Magn Reson Imaging Clin N Am 1996;4:797–833.)
390 The British Journal of Radiology, April 2002
Pictorial review: Spinal ultrasound in infants
(a) (b)
Figure 8. (a) Sagittal spinal ultrasound (SUS) showing
anechoic myelomeningocele in continuity with both a
tethered cord (the conus lies at L5) and a cutaneous
soft tissue mass. (b) Axial SUS (same patient) show-
ing anechoic myelomeningocele in continuity with
tethered cord. (c) Sagittal line diagram showing fea-
tures of a myelomeningocele. Note the large dysraphic
defect in the neural arches, the herniated sac of exposed
neural tissue posteriorly (arrows) and cerebrospinal
fluid (CSF) anteriorly. ((a,b) reproduced with kind
permission from Dick EA, de Bruyn R, Patel K, Owens
CM. Spinal ultrasound in cloacal exstrophy. Clin
Radiol 2001;56:289–94. (c) reproduced with kind per-
mission from Byrd SE, Darling CF, McLone DG,
Tomita T. MR imaging of the pediatric spine. Magn
Reson Imaging Clin N Am 1996;4:797–833.
(c)
References 8. Kriss VM, Kriss TC, Desai NS, Warf BC. Occult
spinal dysraphism in the infant. Clin Paediatr
1. Dick EA, de Bruyn R, Patel K, Owens CM. Spinal 1995;34:650–4.
ultrasound in cloacal exstrophy. Clin Radiol 2001; 9. Scheible W, James HE, Leopold GR, Hilton SV.
56:289–94. Occult spinal dysraphism in infants: screening with
2. Rohrschneider WK, Forsting M, Darge K, Troger high-resolution real-time ultrasound. Radiology
J. Diagnostic value of spinal US: comparative study 1983;146:743–6.
with MR imaging in pediatric patients. Radiology
10. Toma P, Lucigrai G. Ultrasound assessment of
1996;200:383–8.
spinal dysraphism. Riv Neuroradiol 1996;9:
3. Fotter R, Sorantin E, Schneider U, Ranner G, Fast
679–83.
C, Schober P. Ultrasound diagnosis of birthrelated
spinal cord trauma: neonatal diagnosis and follow- 11. Raghavendra BN, Epstein FJ, Pinto RS,
up and correlation with MRI. Pediatr Radiol Subramanyam BR, Greenberg J, Mitnick JS.
1994;24:241–4. The tethered spinal cord: diagnosis by high-
4. Filippigh P, Clapuyt P, Debauche C, Claus D. resolution real-time ultrasound. Radiology
Sonographic evaluation of traumatic spinal cord 1983;149:123–8.
lesions in the newborn infant. Pediatr Radiol 1994; 12. Karrer FM, Flannery AM, Nelson MD Jr, McLone
24:245–7. DG, Raffensperger JG. Anorectal malformations:
5. Byrd SE, Darling CF, McLone DG, Tomita T. MR evaluation of associated spinal dysraphic syn-
imaging of the pediatric spine. Magn Reson dromes. J Pediatr Surg 1988;23:45–8.
Imaging Clin N Am 1996;4:797–833. 13. Naidich TP, Fernbach SK, McLone DG, Shkolnik
6. Kirks DR. Practical pediatric imaging (3rd edn). A. John Caffey Award. Sonography of the caudal
Philadelphia, PA: Lippincott Raven, 1998:281–90. spine and back: congenital anomalies in children.
7. Satar N, Bauer SB, Shefner J, Kelly MD, Darbey AJR 1984;142:1229–42.
MM. The effects of delayed diagnosis and treatment 14. DiPietro MA. The conus medullaris: normal US
in patients with an occult spinal dysraphism. J Urol findings throughout childhood. Radiology 1993;
1995;154:754–8. 188:149–53.
The British Journal of Radiology, April 2002 391
E A Dick, K Patel, C M Owens and R de Bruyn
15. Wolf S, Schneble F, Troger J. The conus medullaris: 21. The Royal College of Radiologists. Making the best
time of ascendence to normal level. Pediatr Radiol use of a department of clinical radiology. Guidelines
1992;22:590–2. for doctors (4th edn). London: RCR, 1998.
16. Egelhoff JC. MR imaging of congenital anomalies 22. Anderson FM. Occult spinal dysraphism: a series of
of the pediatric spine. Magn Reson Imaging Clin N 73 cases. Paediatrics 1975;55:826–7.
Am 1999;7:459–79. 23. Robinson AJ. An audit of the value of ultrasonic
17. Ward PJ, Clarke NMP, Fairhurst JJ. The role of examination of the lumbar spine in infants with
magnetic resonance imaging in the investigation of specific reference to cutaneous markers of spinal
spinal dysraphism in the child with lower limb malformation. London, UK: British Medical Ultra-
abnormality. J Pediatr Orthop 1998;7:141–7. sound Society 2000:77.
18. Schwend RM, Hennrikus W, Hall JE, Emans JB. 24. Korsvik HE, Keller MS. Sonography of occult
Childhood scoliosis: clinical indications for mag- dysraphism in neonates and infants with MR imag-
netic resonance imaging. J Bone Joint Surg Am ing correlation. Radiographics 1992;12:297–306.
1995;77:46–53. 25. Unsinn KM, Geley T, Freund MC, Gassner I. US
19. Cohen AR. The mermaid malformation: cloacal of the spinal cord in newborns: spectrum of nor-
exstrophy and occult spinal dysraphism. Neuro- mal findings, variants, congenital anomalies and
surgery 1991;28:834–43. acquired diseases. Radiographics 2000;20:923–38.
20. Carson JA, Barnes PD, Tunell WP, Smith EI, Jolley
SG. Imperforate anus: the neurologic implication of
sacral abnormalities. J Pediatr Surg 1984;19:
838–42.
392 The British Journal of Radiology, April 2002
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Brian Chan-Locust PDFDocumento10 pagineBrian Chan-Locust PDFdrrahulsshindeNessuna valutazione finora
- Quarterly Oru Folding Diagrams Vol 1Documento199 pagineQuarterly Oru Folding Diagrams Vol 1drrahulsshinde95% (20)
- Quarterly Oru Folding Diagrams - Vol.2Documento186 pagineQuarterly Oru Folding Diagrams - Vol.2drrahulsshinde89% (19)
- Ultrasound Spectrum in Intraductal Papillary Neoplasms of BreastDocumento7 pagineUltrasound Spectrum in Intraductal Papillary Neoplasms of BreastdrrahulsshindeNessuna valutazione finora
- Surgical Anatomy PF PNSDocumento11 pagineSurgical Anatomy PF PNSdrrahulsshindeNessuna valutazione finora
- Tubeless Hypotonic DuodenographyDocumento12 pagineTubeless Hypotonic DuodenographydrrahulsshindeNessuna valutazione finora
- Frontal Sinus Drainage Pathway PDFDocumento9 pagineFrontal Sinus Drainage Pathway PDFdrrahulsshindeNessuna valutazione finora
- Kinematic Evaluation of Cervical Sagittal Balance and Thoracic Inlet AlignmentDocumento13 pagineKinematic Evaluation of Cervical Sagittal Balance and Thoracic Inlet Alignmentdr.s.russo5172Nessuna valutazione finora
- Shibb - E-Yamani (Alum) A Unique Drug and Its Utilization in Unani Medicine A Physicochemical and Pharmacological Review-MinDocumento6 pagineShibb - E-Yamani (Alum) A Unique Drug and Its Utilization in Unani Medicine A Physicochemical and Pharmacological Review-MinAkhtarAliNessuna valutazione finora
- Umbilical CordDocumento17 pagineUmbilical CordClaire Anne PunsalanNessuna valutazione finora
- Nurse Education in Practice: Book ReviewsDocumento1 paginaNurse Education in Practice: Book ReviewsUswatun HasanahNessuna valutazione finora
- Cleft Lip and Cleft PalateDocumento16 pagineCleft Lip and Cleft Palatemacuka08100% (3)
- Can I Play A Concept Analysis of Participation in Children With DisabilitiesDocumento16 pagineCan I Play A Concept Analysis of Participation in Children With DisabilitiesjcpaterninaNessuna valutazione finora
- ThesisDocumento271 pagineThesisRam ArulNessuna valutazione finora
- Peritoneal DialysisDocumento37 paginePeritoneal DialysisEm CastilloNessuna valutazione finora
- Assessment-Tool-For-Ambulance 2018 PDFDocumento12 pagineAssessment-Tool-For-Ambulance 2018 PDFDerrick ChavezNessuna valutazione finora
- Split Cast Metal Post and CoreDocumento5 pagineSplit Cast Metal Post and CoreRaul BatistaNessuna valutazione finora
- Comprehensive Nursing Board Exam Review 500 Page Test 111213225254 Phpapp02 PDFDocumento546 pagineComprehensive Nursing Board Exam Review 500 Page Test 111213225254 Phpapp02 PDF698rickyNessuna valutazione finora
- S. Kim Suvarna MBBS, B.SC., FRCP, FRCPath (Auth.), S. Kim Suvarna (Eds.) Cardiac Pathology - A Guide To Current Practice 2013Documento284 pagineS. Kim Suvarna MBBS, B.SC., FRCP, FRCPath (Auth.), S. Kim Suvarna (Eds.) Cardiac Pathology - A Guide To Current Practice 2013Bogdan Carabas100% (1)
- Reshmis ResumeDocumento2 pagineReshmis Resumeapi-566154298100% (1)
- FTS PDFDocumento2 pagineFTS PDFkukadiyaNessuna valutazione finora
- Infrared VeinviewerDocumento6 pagineInfrared VeinviewerMaimunah Novita SariNessuna valutazione finora
- Theraband Clinical Reference GuideDocumento48 pagineTheraband Clinical Reference GuideSan DyNessuna valutazione finora
- The Mulligan Concept of Manual TherapyDocumento6 pagineThe Mulligan Concept of Manual Therapydrshah85Nessuna valutazione finora
- Comparative Evaluation of Two Techniques in AchievingDocumento5 pagineComparative Evaluation of Two Techniques in AchievingNoland NaidooNessuna valutazione finora
- Prev Injuries 052407Documento124 paginePrev Injuries 052407Anonymous 1sd8foGfGNessuna valutazione finora
- Curriculum Vitae Nata (English)Documento3 pagineCurriculum Vitae Nata (English)Nata SanjayaNessuna valutazione finora
- Medical PrecriptionDocumento4 pagineMedical PrecriptionDimas Ajie PrasetyoNessuna valutazione finora
- Lithium Use in Pregnancy and The Risk of Cardiac MalformationsDocumento10 pagineLithium Use in Pregnancy and The Risk of Cardiac MalformationsRoberto López MataNessuna valutazione finora
- Disability Awareness and SensitivityDocumento37 pagineDisability Awareness and SensitivityIsaiah PeligrinoNessuna valutazione finora
- EpitheliumDocumento48 pagineEpitheliumdrpankaj28100% (1)
- RN ResumeDocumento1 paginaRN Resumeapi-661765354Nessuna valutazione finora
- Song 2016Documento19 pagineSong 2016MarwanNessuna valutazione finora
- Germantown Express News 08/08/15Documento20 pagineGermantown Express News 08/08/15Hometown Publications - Express NewsNessuna valutazione finora
- Option Volume Ventilation Pi 9066364 en 1506 3Documento2 pagineOption Volume Ventilation Pi 9066364 en 1506 3Abdullah AlsafiNessuna valutazione finora
- BS en 01618-1997Documento12 pagineBS en 01618-1997Samwel TarimoNessuna valutazione finora
- Medicolegal ProblemsDocumento2 pagineMedicolegal ProblemsBabith Moses WilbyNessuna valutazione finora