Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Arrhythmia 2
Caricato da
Santi Galang GuadesTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Arrhythmia 2
Caricato da
Santi Galang GuadesCopyright:
Formati disponibili
Home > Chapter 16 > Self Assessment Quiz
Chapter 16
Self Assessment Quiz
Quizzes (See related pages)
Self Assessment Quiz
More Resources
Related Readings
Results Reporter
Out of 15 questions, you answered 15 correctly, for a final grade of 100%.
15 correct (100%)
0 incorrect (0%)
0 unanswered (0%)
Your Results:
The correct answer for each question is indicated by a .
You are following a patient who is receiving chronic oral
1 CORRECT amiodarone. Because of the toxicities of amiodarone, which of
the following tests would you monitor?
A)Chest x-ray
B)Thyroid function tests
C)Liver function tests
D)Ophthalmic examinations
E)All the above
F)a, b, and c only
G)a and b only
H)b and c only
2 CORRECT Which of the following properties does propafenone possess?
A)Vaughan-Williams type Ib only
B)Vaughan-Williams types Ic and II
C)Vaughan-Williams type III
D)Vaughan-Williams types Ia and IV
Intravenous verapamil is much more effective in terminating
reentrant PSVT than oral verapamil is in preventing recurrences
3 CORRECT
of this tachycardia. This can be explained by which of the
following?
A)
Oral verapamil is metabolized by CYP2D6, which is
polymorphic.
B)
Oral verapamil is eliminated primarily by the kidneys as
unchanged drug.
C)
Oral verapamil undergoes extensive first-pass metabolism,
particularly the more active L-isomer.
D)
Oral verapamil has an active metabolite that increases
conduction through the AV node.
Of the Vaughan-Williams type I agents, the Ics such as flecainide
4 CORRECT slow conduction velocity through sodium-dependent tissue the
most at normal heart rates. The reason for this is
A)flecainide has slow on/off kinetics for the sodium channel.
B)flecainide has fast on/off kinetics for the sodium channel.
C)
flecainde has rate-dependant effects in blocking the sodium
channel.
D)
flecainide blocks the sodium channel primarily in the
inactivated state.
You are asked to see a patient with new-onset atrial fibrillation, a
rapid ventricular response (179 beats/min), and thyrotoxicosis.
5 CORRECT
Currently, his only symptoms are weakness and palpitations.
Which of the following do you suggest as initial therapy?
A)Intravenous digoxin to decrease ventricular rate
B)Intravenous ibutilide to restore sinus rhythm
C)Intravenous esmolol to decrease ventricular rate
D)Intravenous amiodarone to control ventricular rate
You see a patient in clinic with atrial fibrillation receiving the
following medications: digoxin 0.25 mg/day (last digoxin level
6 CORRECT 1.3 ng/mL) and warfarin 6mg/day (INR 2-3 for the past 4
weeks). Now the physician would like to restore sinus rhythm
with oral amiodarone. You suggest
A)
avoiding the drug interactions by trying quinidine instead of
amiodarone.
B)decreasing the warfarin dose to 3 mg/day.
C)decreasing the dose of digoxin to 0.125 mg/day.
D)discontinuing the warfarin 1 day after restoring sinus rhythm.
E)a and d only.
F)c only.
G)b and c only.
H)c and d only.
What is the drug of choice to restore sinus rhythm in a patient
7 CORRECT
with AV nodal reentry or orthodromic AV reentry?
A)Adenosine
B)Procainamide
C)Lidocaine
D)Digoxin
A 19-year-old woman is seen in the emergency room with a
history of Wolff-Parkinson-White syndrome. She has no other
problems or known heart disease. Now she has a wide QRS
8 CORRECT tachycardia and irregular in rhythm (rate 178 beats/min). At
present, her blood pressure is stable, and she does not feel
syncopal. Which of the following agents best represents an
effective form of therapy prior to cardioversion?
A)Intravenous adenosine
B)Intravenous verapamil
C)Intravenous amiodarone
D)Intravenous lidocaine
For the patient in Question 8, which of the following represents
9 CORRECT
the best form of chronic therapy to prevent recurrences?
A)Oral flecainide
B)Radiofrequency ablation of the Kent bundle
C)Radiofrequency modification of the AV node
D)Automatic internal defibrillator
Type Ic agents such as flecainide can cause a highly lethal form
of proarrhythmia sometimes called sinusoidal or incessant
10 CORRECT ventricular tachycardia. Which of the following are risk factors for
its occurrence and should be considered contraindications to
flecainide treatment?
A)Wolff-Parkinson-White syndrome
B)Coronary artery disease
C)Preexisting long QT intervals
D)Congestive heart failure
E)a and b only
F)c only
G)b and d only
H)c and d only
The CAST was one of the most important studies ever completed.
11 CORRECT
Which of the following did not result from the CAST?
A)
We learned that we should not treat complex PVCs with the
type III agents such as D-sotalol.
B)
We learned that we should not treat complex PVCs with the
type Ic agents such as flecainide or moricizine.
C)
Drug companies stopped their efforts to find new type Ic
agents.
D)
Some agents such as encainide and indecainide were pulled
from the market or never marketed at all.
You are asked to see a patient who suffered a cardiac arrest and
was resuscitated successfully at O'Hare airport by paramedic
electrical defibrillation. He was transported to your hospital and
12 CORRECT
admitted to the CCU. Initial enzymes show that he has had a
myocardial infarction (MI). For long-term antiarrhythmic therapy,
you suggest
A)consideration for an internal defibrillator.
B)empirical amiodarone.
C)no specific therapy except beta blockers.
D)
electrophysiologic testing to see if the patient has sustained
ventricular tachycardia or fibrillation.
You are at a cardiac arrest of a patient with an MI and ventricular
fibrillation. The patient has had four defibrillations and 40 U of
13 CORRECT vasopressin with no response. Since you are attending the drug
cart, you anticipate what the physician will call for next and draw
up
A)300 mg amiodarone diluted in 20 cc of saline.
B)100 mg of lidocaine.
C)1 mg of epinephrine.
D)300 mg of bretylium.
During rounds, the following patient is presented: a 65-year-old
man with an MI 6 months ago and a history of recurrent
sustained ventricular tachycardia. During electrophysiologic
14 CORRECT studies, he had easily inducible sustained ventricular tachycardia
(rate 240 beats/min) that caused him to pass out. Which of the
following probably will be the treatment of choice for this
patient's arrhythmia?
A)Radiofrequency ablation of the Kent bundle
B)Internal defibrillator
C)Electrophysiologic drug testing
D)No therapy at present, close follow-up only
You are confronted with a patient with a history of atrial
fibrillation who is admitted for the restoration of sinus rhythm. In
the CCU he is given 2 mg of intravenous ibutilide that terminates
15 CORRECT
atrial fibrillation, but shortly thereafter he suffers several long
episodes of polymorphic ventricular tachycardia with a prolonged
QT interval during sinus rhythm. You suggest
A)intravenous epinephrine 1.0 mg.
B)intravenous amiodarone 300 mg.
C)intravenous lidocaine 100 mg.
D)intravenous magnesium 2 g.
Routing Information
Date: Wed Mar 11 08:25:25 EDT 2020
My name:
Section ID:
Email these results to:
Email address: Format:
Me: HTML
My Instructor: HTML
My TA: HTML
Other: HTML
E-Mail The Results
We welcome your feedback. Please send comments and questions to:
medical_education@mcgraw-hill.com.
To learn more about the book this website supports, please visit its Information Center.
Copyright 2020 McGraw-Hill Global Education Holdings, LLC. All rights reserved.
Any use is subject to the Terms of Use and Privacy Center | Report Piracy
Potrebbero piacerti anche
- Acute Respiratory Infection PDFDocumento12 pagineAcute Respiratory Infection PDFSanti Galang GuadesNessuna valutazione finora
- Communication and Documentation For An Ambulatory Practice PDFDocumento25 pagineCommunication and Documentation For An Ambulatory Practice PDFSanti Galang GuadesNessuna valutazione finora
- University of San Carlos School of Health Care Professions Department of Pharmacy SyllabusDocumento4 pagineUniversity of San Carlos School of Health Care Professions Department of Pharmacy SyllabusSanti Galang GuadesNessuna valutazione finora
- Ambulatory Care: Sample Format For Oral/Written Patient PresentationsDocumento1 paginaAmbulatory Care: Sample Format For Oral/Written Patient PresentationsSanti Galang GuadesNessuna valutazione finora
- Breast Cancer PDFDocumento37 pagineBreast Cancer PDFSanti Galang Guades50% (2)
- SCampus 2016 2017Documento110 pagineSCampus 2016 2017Santi Galang GuadesNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Brugada Syndrome: Dr. Kazi Alam NowazDocumento19 pagineBrugada Syndrome: Dr. Kazi Alam NowazMegawati AbubakarNessuna valutazione finora
- SVTDocumento8 pagineSVTJulieNessuna valutazione finora
- Antiarrhythmic Drugs 1Documento32 pagineAntiarrhythmic Drugs 1AliImadAlKhasakiNessuna valutazione finora
- Brugada Review Jacc 2018 PDFDocumento14 pagineBrugada Review Jacc 2018 PDFanon422Nessuna valutazione finora
- Pharmacology Review Questions For QuizDocumento14 paginePharmacology Review Questions For QuizusedforfunplocNessuna valutazione finora
- NCM 106 Cardiac DrugsDocumento111 pagineNCM 106 Cardiac DrugsKatie HolmesNessuna valutazione finora
- Diagnosis and Management Sudden Cardiac Death 2005Documento7 pagineDiagnosis and Management Sudden Cardiac Death 2005aminceloNessuna valutazione finora
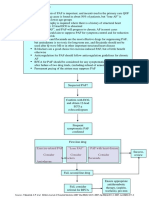
- Pathway DIAGNOSIS OF PAF FTRDocumento1 paginaPathway DIAGNOSIS OF PAF FTRYoan Eka Putra PalilingNessuna valutazione finora
- Anti Arrhythmia DrugsDocumento3 pagineAnti Arrhythmia DrugsFarid ZainuddinNessuna valutazione finora
- Lange Smart Charts: Pharmacology, 2e Medications Affecting Cardiac and Renal FunctionDocumento2 pagineLange Smart Charts: Pharmacology, 2e Medications Affecting Cardiac and Renal FunctionSaulNessuna valutazione finora
- Pharmacological Therapy For Rate and Rhythm Control For Atrial Fibrillation in 2017Documento8 paginePharmacological Therapy For Rate and Rhythm Control For Atrial Fibrillation in 2017UCI CONTINGENCIANessuna valutazione finora
- Supra Ventricular TachycardiaDocumento10 pagineSupra Ventricular TachycardiaJohn RobinsonNessuna valutazione finora
- Lippincott Antiarrhythmics 7Documento2 pagineLippincott Antiarrhythmics 7Wijdan HatemNessuna valutazione finora
- Antiarrhythmic DrugsDocumento42 pagineAntiarrhythmic DrugsKrakenzeN100% (1)
- Fibrilacioni Atrial Trajtimi Dhe Diagnoza e TijDocumento8 pagineFibrilacioni Atrial Trajtimi Dhe Diagnoza e TijMarsiano QendroNessuna valutazione finora
- Antiarrhythmic DrugsDocumento17 pagineAntiarrhythmic DrugsTarek G MustafaNessuna valutazione finora
- Algoritma SVTDocumento87 pagineAlgoritma SVTbonne_ameNessuna valutazione finora
- Antiarrhythmic DrugsDocumento50 pagineAntiarrhythmic DrugsamirNessuna valutazione finora
- Practice Essentials: Essential Updates: Distinguishing Between Left-And Right-Sided Atrial TachycardiaDocumento28 paginePractice Essentials: Essential Updates: Distinguishing Between Left-And Right-Sided Atrial TachycardiaRully SyahrizalNessuna valutazione finora
- Guaranteed To Pass: Exam Tidbits in Easy To Digest, Bite Sized MorselsDocumento2 pagineGuaranteed To Pass: Exam Tidbits in Easy To Digest, Bite Sized MorselsAmberNessuna valutazione finora
- 3,4 - Anti-Arrhythmic Drugs (Summary, SAQ and MCQS)Documento10 pagine3,4 - Anti-Arrhythmic Drugs (Summary, SAQ and MCQS)Mengot Ashu RoseNessuna valutazione finora
- Amiodarone: Reevaluation of An Old Drug: Ann Intern Med. 1995 122:689-700Documento12 pagineAmiodarone: Reevaluation of An Old Drug: Ann Intern Med. 1995 122:689-700DenisseRangelNessuna valutazione finora
- IV. Antiarrhythmic Drugs: PHRM 537 Summer 2020Documento19 pagineIV. Antiarrhythmic Drugs: PHRM 537 Summer 2020SaulNessuna valutazione finora
- Cardio PDFDocumento94 pagineCardio PDFSalwaNessuna valutazione finora
- Cardioversion For Atrial Fibrillation - ClinicalKeyDocumento27 pagineCardioversion For Atrial Fibrillation - ClinicalKeyAnthony Martin Corrales ParedesNessuna valutazione finora
- Anti ArrhythmicsDocumento46 pagineAnti Arrhythmicsnk999999Nessuna valutazione finora
- Junctional Ectopic Tachycardia in Infants and Children: Ranjit I. Kylat MD - Ricardo A. Samson MDDocumento8 pagineJunctional Ectopic Tachycardia in Infants and Children: Ranjit I. Kylat MD - Ricardo A. Samson MDCatherine MorrisNessuna valutazione finora
- Questions PharmcologyDocumento17 pagineQuestions Pharmcologylalitrajindolia100% (2)
- An Uncommon Stemi Masquerader: A Case of Imipramine Induced Brugada Phenocopy (BRP)Documento5 pagineAn Uncommon Stemi Masquerader: A Case of Imipramine Induced Brugada Phenocopy (BRP)IJAR JOURNALNessuna valutazione finora
- Pill in Pocket NEJMDocumento8 paginePill in Pocket NEJMn2coolohNessuna valutazione finora