Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Gordon's Functional Health Assessment
Caricato da
Raquel M. Mendoza100%(1)Il 100% ha trovato utile questo documento (1 voto)
885 visualizzazioni11 paginelecture
Copyright
© © All Rights Reserved
Formati disponibili
DOC, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentolecture
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOC, PDF, TXT o leggi online su Scribd
100%(1)Il 100% ha trovato utile questo documento (1 voto)
885 visualizzazioni11 pagineGordon's Functional Health Assessment
Caricato da
Raquel M. Mendozalecture
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOC, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 11
GORDON’S FUNCTIONAL HEALTH ASSESSMENT
Pattern Information from History Information from Examination
Health Perception-Health Clients description of general health status Observe general appearance
Management Past illness, operations and hospitalizations This health pattern is determined
Includes health status; health promotion Changes in health status over time from history
and illness prevention practices; medical Health promotion activities Examination of patient generally
or nursing prescriptions; follow-up care Illness prevention activities (last pap smear, follows the history interview
breast self exam, last physical exam, last
tetanus shot, etc)
Current medications and supplements
Current therapeutic interventions
Allergies to food/medicines/other
Perception of cause(s) of current illness and
actions taken
How current encounter might be helpful
Anticipated plans for discharge or further care
Use of alcohol, tobacco, and illicit drugs
Significant family history of illnesses
Ob – gravida, para, time and type of delivery
if postpartum, gestation at first prenatal visit,
compliance with prenatal care
Pedi – gestational age at birth, apgar scores,
compliance with child care
Pattern Information from History Information from Examination
Page 1 of 11 Gordons Functional Health Assessment
Nutritional-Metabolic Typical daily food intake Assess overall appearance (well
Last intake of food and fluid nourished, well developed,
Includes food and fluid consumption; Types and quantity of foods overweight, underweight)
types and quantities of food and fluid; Types and quantity of fluids Assess skin appearance: color,
food preferences and timing of intake; Restricted diet or type of diet prescribed lesions, pressure areas, moisture,
special diet(s) Timing of meals and snacks texture, open areas, dressings,
Use of supplements, i.e. Vitamins, energy rashes, scars, ecchymosis, diaphoresis
Also includes hydration status, skin and foods, hyperail, tube feedings, etc Obtain body temperature
tissue integrity, and thermoregulation. Appetite status, loss of or change in Obtain height and weight, calculate
Difficulties swallowing, chewing, digesting, bmi
Recent weight loss or gain Observe condition of mouth, lips and
Use of artificial nutritional devices other mucous membrane areas
Use of dentures, partial plates, etc. (include moistness)
Problems with nausea, heartburn, indigestion, Assess skin turgor
excessive hunger or thirst etc Observe condition of teeth; present,
Family or personal history of diabetes, thyroid absent, gum problems, dentures,
problems partial plates, obvious decay or
Lab results including hct, hgb, thyroid levels, bleeding
blood sugars, blood chemistries, cholesterol Inspect for evidence of tissue healing
levels, urinalysis (sp grav, protein, glucose, processes
ketones) Inspect integrity of hair and nails
Problems with skin or healing (rashes, open Record intake of oral and intravenous
areas, lesions) fluids if applicable.
Ob – prepregnant weight, weight gain/loss in Ob – assess condition of nipples and
pregnancy, perception of breastfeeding breasts, assess effectiveness of
Pedi – birth weight, type of formula or breast breastfeeding
as infant, introduction of solid foods, self
feeding behaviors, pattern of weight gain
Page 2 of 11 Gordons Functional Health Assessment
Pattern Information from History Information from Examination
Elimination Frequency, character of bowel movements, Examine, if indicated, color,
Includes patterns of bowel, bladder, and including last bowel movement consistency, character, frequency, and
skin excretory functions; devices used for Frequency, character of urine excretion, any quantity of feces and urine
elimination difficulty, incontinence or dsyuria Examine, if indicated, color, character
Any changes in usual patterns, or history of and quantity of output from other
problems, kidney or liver disease excretory sites
Use of laxatives/ diuretics Abdominal assessment including
Use of artificial excretory devices, e.g. bowel sounds, flatus, softness,
Colostomy, ureterostomy distention, masses, girth,
Degree of perspiration hemorrhoids, drains, or collection
Any other excretory sites, e.g. Drains, chest devices.
tubes suction, ng drainage, vomiting
Lab/ test results including urinalysis, stool for
occult blood, stool cultures, kidney function
tests, liver function tests, gi studies, etc
Ob – note any difficulties with nausea,
constipation, hemorrhoids, urinary frequency
or stress incontinence.
Pedi – note diapering or toileting routines,
note special words utilized
Page 3 of 11 Gordons Functional Health Assessment
Pattern Information from History Information from Examination
Activity-Exercise Type and regularity of exercise Observe function in areas listed in
Includes exercise pattern; activities of Usual activity requirements at home and work history and code each according to
daily living; leisure/recreation activities, Perceived response to activity ( sob, dizzy, level 0, 1, 2, 3, or 4
energy balance; focus on activities of weak ,etc) Examine gait, posture
importance. Perceived energy level (note any changes) Note any joint deformity or missing
Also includes cardiac and pulmonary Recreational activities body structures, e.g. Amputee
status and responses to activity. Leisure activities, i.e. Hobbies, clubs Test range of motion of joints
Perceived ability to carry out feeding, Test muscle strength, mass and tone
bathing, toileting, bed mobility, dressing, Test equilibrium/balance
grooming, cooking, shopping, home Palpate pulse; note rate, rhythm, and
maintenance quality
0 Level 0 = full self care Note heart sounds and presence of
1 Level 1 = requires use of equipment or device murmur
2 Level 2 = requires supervision from a person Record bp, note any changes with
3 Level 3 = requires assistance from a person position or activity
4 Level 4 = dependent/does not participate Auscultate breath sounds; note
Use of prosthesis presence of adventitious sounds
History of joint and back problems or Note rate and character of
weakness respirations, presence of any
Use of tobacco-, how much, for how long? difficulties (retractions, coughing,
Family or personal history of heart disease, sputum, use of accessory muscles,
hypertension, asthma or tb flaring, etc), and any oxygen
Lab/test results including chest xray, ekg, requirement.
abgs, cardiac enzymes, pulse oximetry, peak Assess vascular status, e.g.
flow, pft’s, sputum cultures. Peripheral pulses, varicosities,
Ob – changes in mobility related to capillary refill in nail beds, signs of
pregnancy, any symptoms of preeclampsia atrophic skin changes, color of skin
(headache, changes in vision, epigastric pain, and nail beds, edema, dryness or
nausea, edema), knowledge of exercises to moistness of skin, and homan’s sign.
restore tone. Observe general hygiene, dress, and
Pedi – note age when met various gross grooming appearance
motor and fine motor milestones
Page 4 of 11 Gordons Functional Health Assessment
Pattern Information from History Information from Examination
Sleep-Rest Number of hours of sleep/24 hours Observe sleep/rest pattern if possible
Frequency of rest periods; do they include Observe sleep/rest disruptions
Includes frequency and duration of sleep sleeping? Observe alertness and mental status
and rest periods; use of sleep-inducing Time of night retire
medications; environmental sleeping Time of day awake
conditions Any perceived problems – difficulty falling
asleep, frequent or early waking
Sleep/ rest reversal, e.g. Sleep day, work
night
Degree of perceived energy upon awakening
Frequency of dreams or nightmares, what
seems to aggravate them or induce them
Use of sleeping aids such as medications
Use of other sleep-inducing practices
Environmental conditions such as number of
pillows to sleep, type of bed used
Pedi – bedtime routine and rituals, security
items,
Ob – difficulty sleeping as a result of
pregnancy, timing of labor in relation to sleep,
length of labor
Page 5 of 11 Gordons Functional Health Assessment
Pattern Information from History Information from Examination
Cognitive-Perceptual Hearing status; need for hearing devices, Test special senses of hearing, vision,
date of last hearing test taste, touch and smell
Includes sensory function (hearing, Vision status; need for eyewear, last eye Test orientation to person, time, and
vision, taste, smell, touch); comfort and exam place
pain perception; cognitive functions Problems with taste or smells Determine level of consciousness as
(language, memory, judgment, decision- Problems with touch sensation, any measured by responses to various
making) numbness or tingling stimuli
Pain (level, location, frequency, duration, Listen to language used
character, aggravating circumstances, relief Listen to quality, pace, articulation of
methods, and tolerance level) speech
Cognitive function in terms of memory, short Test recent memory, remote
term and long term memory, and new learning, as
History of any changes in level of indicated
consciousness or periods of confusion Perform developmental screening
Communication – primary language spoken, tests, as indicated
other languages spoken, educational level, Determine ability to comprehend
perceived ability to read and write words, read and write, thought
Degree of problem-solving capabilities processes
Degree of decision-making capabilities Access behavioral clues to pain level
Perceived attention span and tolerance (grimacing, guarding,
History of fainting, seizures or dizziness irritability, distractibility, etc)
History of headaches – location, frequency,
associated factors
Ob – attendance at prenatal classes,
knowledge of self care and baby care.
Pedi – note age when various language
milestones met, grade level, any behavioral or
learning difficulties in school.
Page 6 of 11 Gordons Functional Health Assessment
Pattern Information from History Information from Examination
Self-Perception/Self-Concept How do you feel about self most of the time? Observe use or nonuse of eye contact
What can you tell me about yourself? Note attention span or distraction
Includes feelings of general self-worth; How will this issue affect your life? Observe body posturing
attitudes about self, image, identity; Description of self Note voice and speech quality, intensity
general emotional pattern Any fears, anxieties, reason to be depressed or Rate on scale of 1-5, relaxed to nervous
feel loss of control Rate on scale of 1-5, assertive to passive
Measures used to improve feelings regarding self- Note both verbal and nonverbal cues to
concept indicate expressions of self-concept
Experiences related to feelings of hopelessness
Role-Relationship Construct of family structure Observe interaction between family
Living arrangements, e.g. Alone, family, members
Includes family and social roles; work roommates, etc. Ob/pedi – evidence of bonding and
role; satisfaction or not with roles; Role within family, e.g. Father, mother, financial attachment behaviors of both mother and
perception of major roles in life earner father of baby, assess parenting skills
Self or family care-giver or care-receiver role
Perception of effect of current health problem or
current situation on role(s)
Occupation/profession/work role
Student role
Satisfaction or non-satisfaction with all roles
Difficulties or problems in maintaining roles
defined
Health insurance status and influence on current
encounter and role-relationships
Financial income sufficient to meet current needs
or not
Family relationships sufficient to meet current
needs or not
Ob – pregnancy planned?, feelings about and
Page 7 of 11 Gordons Functional Health Assessment
plans for pregnancy/labor and delivery / childcare,
relationship with father of baby, plans for feeding
baby
Pattern Information from History Information from Examination
Sexuality-Reproductive Any sexual concerns Usually no examination indicated
Sexual orientation unless skilled and capable of doing
Includes a male & female focus related Sexual relationships and degree of pelvic examination of female or
to satisfaction or dissatisfaction with satisfaction testicular and prostrate examination
sexuality; describes reproductive pattern; Female phase of reproductive cycle, such as of male
if female, phase of reproductive cycle child-bearing, premenses, peri or post If pregnant - fundal height, vaginal
menopausal exams, palpation of contractions, fetal
Female menstrual history; age of menarche, heart tracing (rate, variability, periodic
duration, frequency, regularity, problems changes), discharge, bleeding or
Female reproductive history; past leaking of fluid
pregnancies and deliveries, any difficulties If postpartum – fundus (location and
Family history of multiple birth, congenital firmness), lochia (color, amount and
anomalies or genetic disorders presence of clots), perineum,
Birth control practices both male and female, episiotomy and/or lacerations
in past and planned If newborn – circumcised?, testes
Type of practices used to prevent sexually descended?, vaginal discharge or
transmitted diseases, both male and female swelling?
History of sexually-transmitted diseases
Frequency and perceived thoroughness of
performing either self-breast examination or
self-testicular exam
OB – LMP, EDC, pregnancy planned ?,
problems with current or past pregnancies or
deliveries (spotting, PIH, diabetes,
hemorrhage, surgery, etc), Lab/test results –
pregnancy test, AFP, amniocentesis,
ultrasound results (amniotic fluid volume,
estimated fetal weight), non stress tests,
biophysical profile, L/S ratio, culture results,
Page 8 of 11 Gordons Functional Health Assessment
GBS status
PEDI – circumcised?, Tanner stage of
development
Pattern Information from History Information from Examination
Coping-Stress Tolerance recent changes, problems, or events causing conduct stress scale analysis, as
concern or stress indicated
Includes methods or ways to handle or any crisis recently, i.e. illness or note behavioral or physiological
cope with stress; defines stressors or hospitalization manifestations of mood, affect,
events that threaten a person; coping is description of current stress level anxiety and stress.
how one responds to stressors; stress use of medications or alcohol to cope
tolerance is level of effective coping methods used to cope with stress that are not
drug or alcohol-related, e.g. taking walks,
reading, engaging in hobbies, talking to
someone
degree of success of current coping strategies
perception of stress tolerance level
perception of safety status at home, i.e.
episodes of physical and/or emotional abuse
OB – plans for coping during labor,
perception of coping during labor and delivery
PEDI – parents plans for dealing with various
childhood stages and issues
Value-Belief religious choice, if indicated none indicated, according to Gordon
Includes values, goals, and beliefs as spiritual beliefs that influence health decisions determine cultural, ethnic
related to choices or decisions made; or practices background
spiritual beliefs, issues of life importance; degree of goals of life attainment
relationship of such value-belief pattern perception of satisfaction with life and the
on health issues and practices way “things are”
cultural beliefs that reflect on health or values
cultural beliefs that reflect on choices for
health promotion and illness prevention
Page 9 of 11 Gordons Functional Health Assessment
Pattern Information from History Information from Examination
Safety/Protection exposure to hazards at home or work temperature
(including xrays, chemicals, machinery, any signs and symptoms of injury to
Includes environmental hazards, pollutants, animals) tissue (scars, bruises, swelling,
potential sources of physical harm or possible exposure to communicable diseases wounds)
injury, exposure to communicable and pathogens (including blood transfusions, any signs and symptoms of infection
diseases and pathogens, allergies, and ingestion of raw meats, animal or insect bites, (enlarged lymph nodes, odor,
the body’s attempts to protect itself and exposure to infectious persons) discharge, redness, warmth, rashes,
respond to pathogens history of accidents and injuries, at risk for etc)
falls
history of allergies, communicable diseases,
STDs, and immunizations
Lab results – WBC with differential, culture
results, sensitivities, titers, HIV tests, sickle
cell screen, lead level, PPD results,
OB/Newborn - Rh factor, ABO
incompatibility, Coombs test, length of time
membranes ruptured, meconium in fluid?
PEDI – Is environment safe, childproofed?
exposure to lead?, immunizations up to date?
Growth/Development age when pertinent milestones or tasks assessment depends on the particular
achieved. milestones or developmental tasks
that are appropriate in a variety of
Includes age appropriateness of physical areas including physical, cognitive,
and psychosocial development and emotional, social, language, and
attainment of developmental milestones moral development.
in various areas
Page 10 of 11 Gordons Functional Health Assessment
Page 11 of 11 Gordons Functional Health Assessment
Potrebbero piacerti anche
- Medical Surgical Nursing 7th Edition Ignatavicius Test BankDocumento9 pagineMedical Surgical Nursing 7th Edition Ignatavicius Test Bankqocax0% (1)
- GORDON'sDocumento7 pagineGORDON'siura echinNessuna valutazione finora
- Health Perception and Management in PregnancyDocumento4 pagineHealth Perception and Management in PregnancySheila_Marie_L_45075% (4)
- Gordon's Functional Pattern PneumoniaDocumento6 pagineGordon's Functional Pattern PneumoniaLei Ortega86% (14)
- Gordon’s Functional Health Pattern AssessmentDocumento12 pagineGordon’s Functional Health Pattern AssessmentLoyloy D Man100% (1)
- Complete - Gordon's Functional Health Pattern - Group 4Documento7 pagineComplete - Gordon's Functional Health Pattern - Group 4TaanzNessuna valutazione finora
- Soapie, Assessment and NCP On PAINDocumento7 pagineSoapie, Assessment and NCP On PAINAna100% (2)
- Gordons Functional Health PatternDocumento2 pagineGordons Functional Health PatternMaryneth Evangelista80% (5)
- Gordon's Functional Health PatternsDocumento4 pagineGordon's Functional Health PatternsFlourence Zafran100% (1)
- The Framework of Life Course (Kuan, 2005): 3 ComponentsDocumento1 paginaThe Framework of Life Course (Kuan, 2005): 3 ComponentsGracia Maya0% (1)
- Nursing Research 1: Module 4: Conceptual Phase Week 6: The Research ProblemDocumento4 pagineNursing Research 1: Module 4: Conceptual Phase Week 6: The Research ProblemLEMUEL GLENN BAUTISTANessuna valutazione finora
- Cell Ab ActivitiesDocumento7 pagineCell Ab ActivitiesJanelle Cabida Supnad100% (1)
- NCM 111 - Nursing Research 1 Research WritingDocumento10 pagineNCM 111 - Nursing Research 1 Research WritingissaiahnicolleNessuna valutazione finora
- GI NursingDocumento14 pagineGI NursingKarl Bayonito100% (5)
- Guidelines in PortfolioDocumento3 pagineGuidelines in PortfolioRaquel M. Mendoza100% (1)
- Strahlenfolter Stalking - TI - Mechanising The Mind - Brave New World of ESB - Exerpt From As Man Becomes Machine by David RorvikDocumento10 pagineStrahlenfolter Stalking - TI - Mechanising The Mind - Brave New World of ESB - Exerpt From As Man Becomes Machine by David RorvikKurt-SchneiderNessuna valutazione finora
- Phasing PrimerDocumento40 paginePhasing Primertruby100% (1)
- Gordon's 11 Functional Health PatternDocumento4 pagineGordon's 11 Functional Health PatternSitti Nauhar Aukasa100% (1)
- Gordon's 11 Functional Health AssessmentDocumento4 pagineGordon's 11 Functional Health AssessmentJehn Pauleen Fernandez RollanNessuna valutazione finora
- Gordon's Functional Health PatternsDocumento2 pagineGordon's Functional Health Patternsserarrist100% (2)
- Gordon's AssessmentDocumento2 pagineGordon's AssessmentNikka GutierrezNessuna valutazione finora
- Gordon's Functional Health PatternsDocumento4 pagineGordon's Functional Health PatternsJamaica Leslie NovenoNessuna valutazione finora
- Gordon's Functional Health PatternDocumento3 pagineGordon's Functional Health PatternAiko NishinoNessuna valutazione finora
- Course in The WardDocumento2 pagineCourse in The WardshanabsinNessuna valutazione finora
- Gordon's Functional Health PatternDocumento2 pagineGordon's Functional Health PatternAnn Michelle Tarrobago100% (1)
- Health History by Gordon's Functional Health PatternDocumento7 pagineHealth History by Gordon's Functional Health PatternAveriAlonzoNessuna valutazione finora
- Prenatal Care for AdolescentsDocumento15 paginePrenatal Care for AdolescentsSara DayonNessuna valutazione finora
- Pattern Before Present Interpretation AnalysisDocumento8 paginePattern Before Present Interpretation AnalysisJorelyn FriasNessuna valutazione finora
- Gordons Functional Health PatternDocumento7 pagineGordons Functional Health PatternJosephine Valdez HanrathNessuna valutazione finora
- Gordon's 11 Functional Health PatternsDocumento4 pagineGordon's 11 Functional Health Patternsnina angelaNessuna valutazione finora
- Choledolithiasis Cs 103 1Documento34 pagineCholedolithiasis Cs 103 1Merlene Sarmiento SalungaNessuna valutazione finora
- Gordon's Pattern of Health: He Assumes Total Responsibility For Decision-Making and Self-Care - NotDocumento6 pagineGordon's Pattern of Health: He Assumes Total Responsibility For Decision-Making and Self-Care - NotleibogiciousNessuna valutazione finora
- GordonsDocumento3 pagineGordonsKevin Gonzales DiamosNessuna valutazione finora
- Gordon S Health AssessmentDocumento13 pagineGordon S Health AssessmentMaria Visitacion100% (3)
- Case Study (MCN II)Documento16 pagineCase Study (MCN II)Gabrielle SandovalNessuna valutazione finora
- Gordons Pattern of Functioning (518 - Sanvitores Victoria)Documento7 pagineGordons Pattern of Functioning (518 - Sanvitores Victoria)Anthony Jay Luz Foronda100% (1)
- Case Study MCN IIDocumento19 pagineCase Study MCN IIAthena SaturdayNessuna valutazione finora
- III. Physical Assessment FindingsDocumento8 pagineIII. Physical Assessment FindingsBilly Joe SincoNessuna valutazione finora
- Application of Dorothea Orem-PRELIMSDocumento6 pagineApplication of Dorothea Orem-PRELIMSJessica Ella Hernandez Agunday0% (1)
- Demonstrate: Pain Coping TechniquesDocumento4 pagineDemonstrate: Pain Coping TechniquesMae Therese B. MAGNO100% (1)
- A Patient's Bill of RightsDocumento4 pagineA Patient's Bill of RightsMark ElbenNessuna valutazione finora
- Case Study (1166)Documento17 pagineCase Study (1166)ساره معنNessuna valutazione finora
- Elderly Nursing Case StudyDocumento13 pagineElderly Nursing Case StudyAlreem AlhajryNessuna valutazione finora
- 2NF - Grand Case Presentation Written OutputDocumento99 pagine2NF - Grand Case Presentation Written OutputKyra Bianca R. FamacionNessuna valutazione finora
- Gordons Functional Health PatternDocumento8 pagineGordons Functional Health PatterniamjenivicNessuna valutazione finora
- Ateneo de Davao University College of NursingDocumento161 pagineAteneo de Davao University College of Nursingnevajane100% (1)
- Gordons Functional Health AssessmentDocumento73 pagineGordons Functional Health Assessmentdigracia manatigaNessuna valutazione finora
- General Description of Client: A. Nursing Health HistoryDocumento3 pagineGeneral Description of Client: A. Nursing Health HistoryDianneNessuna valutazione finora
- Gordon's Functional Assessment HistoryDocumento5 pagineGordon's Functional Assessment HistoryJachel Kathleen Laguio100% (1)
- Drug-Study-Ncp-And-Fdar - Sir WencyDocumento21 pagineDrug-Study-Ncp-And-Fdar - Sir WencyBiway RegalaNessuna valutazione finora
- Family Nursing Care PlanDocumento34 pagineFamily Nursing Care PlanJai - Ho57% (14)
- What Health Promotion Strategies Would You Recommend To Promote Successful AgingDocumento1 paginaWhat Health Promotion Strategies Would You Recommend To Promote Successful AgingRoselyn Yu QuintoNessuna valutazione finora
- Assignment5.1 - Comfort Theory CritiqueFinalDocumento8 pagineAssignment5.1 - Comfort Theory CritiqueFinalRacheal100% (1)
- Gordon'S 11 Functional Pattern Health Perception-Health Management PatternDocumento4 pagineGordon'S 11 Functional Pattern Health Perception-Health Management PatternAnonymous UeEPCPNessuna valutazione finora
- Jessa Abasola's Personal History and Postpartum CareDocumento9 pagineJessa Abasola's Personal History and Postpartum CareJajangNessuna valutazione finora
- Case Study (HOSPITAL)Documento4 pagineCase Study (HOSPITAL)Reyna Mee AhiyasNessuna valutazione finora
- Ineffective Breathing PatternDocumento185 pagineIneffective Breathing PatternSusi LambiyantiNessuna valutazione finora
- History and Physical ExaminationDocumento18 pagineHistory and Physical ExaminationadesamboraNessuna valutazione finora
- Teaching Plan.Documento13 pagineTeaching Plan.Maria Rogine Elopre100% (2)
- Metro Manila developmental screening test case studyDocumento50 pagineMetro Manila developmental screening test case studyShy DawnNessuna valutazione finora
- IV. Physical Assessment Norms Actual Findings Interpretation and Analysis General Appearance Posture / GaitDocumento9 pagineIV. Physical Assessment Norms Actual Findings Interpretation and Analysis General Appearance Posture / GaitMarianne_Miraflo_154Nessuna valutazione finora
- Xiii. Discharge Planning: Carbohydrates NutrientsDocumento4 pagineXiii. Discharge Planning: Carbohydrates Nutrientsgroupbsection1Nessuna valutazione finora
- PEDIA Clerks Revalida Review 2023Documento106 paginePEDIA Clerks Revalida Review 2023Raven EvangelistaNessuna valutazione finora
- Prenatal Substance Dependence AbuseDocumento13 paginePrenatal Substance Dependence Abusenursereview100% (2)
- The Family Nursing Process GuideDocumento17 pagineThe Family Nursing Process GuideRaquel M. MendozaNessuna valutazione finora
- Growth and Dev Theories2Documento34 pagineGrowth and Dev Theories2Raquel M. MendozaNessuna valutazione finora
- ExpandedroleofnursesDocumento17 pagineExpandedroleofnursesRaquel M. MendozaNessuna valutazione finora
- 3 Problems With The Passenger and Powers of LaborDocumento105 pagine3 Problems With The Passenger and Powers of LaborRaquel M. MendozaNessuna valutazione finora
- Case Scenario GRP 3Documento1 paginaCase Scenario GRP 3Raquel M. MendozaNessuna valutazione finora
- Menstrual CycleDocumento5 pagineMenstrual CycleRaquel M. MendozaNessuna valutazione finora
- Growth and Development of Children in the First YearDocumento53 pagineGrowth and Development of Children in the First YearRaquel M. MendozaNessuna valutazione finora
- 1 The High Risk MotherDocumento161 pagine1 The High Risk MotherRaquel M. MendozaNessuna valutazione finora
- 6 Infancy Diseases 1Documento135 pagine6 Infancy Diseases 1Raquel M. MendozaNessuna valutazione finora
- Unit Ii Leadership in Nursing: A. Nurse in The OrganizationDocumento25 pagineUnit Ii Leadership in Nursing: A. Nurse in The OrganizationRaquel M. MendozaNessuna valutazione finora
- Difference Between Adult and Fetal CirculationDocumento6 pagineDifference Between Adult and Fetal CirculationRaquel M. MendozaNessuna valutazione finora
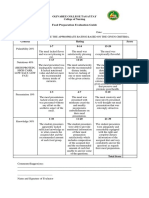
- Criteria Grading Scale Completion 5 4 3 2: Total PTS: 20Documento1 paginaCriteria Grading Scale Completion 5 4 3 2: Total PTS: 20Raquel M. MendozaNessuna valutazione finora
- Growth and Dev Theories2Documento34 pagineGrowth and Dev Theories2Raquel M. MendozaNessuna valutazione finora
- Care of The NewbornDocumento163 pagineCare of The NewbornRaquel M. MendozaNessuna valutazione finora
- Care of The NewbornDocumento163 pagineCare of The NewbornRaquel M. MendozaNessuna valutazione finora
- 1 The High Risk MotherDocumento161 pagine1 The High Risk MotherRaquel M. MendozaNessuna valutazione finora
- Grief, Loss, Death and DyingDocumento47 pagineGrief, Loss, Death and DyingRaquel M. MendozaNessuna valutazione finora
- Criteria Grading Scale Completion 5 4 3 2: Total PTS: 20Documento1 paginaCriteria Grading Scale Completion 5 4 3 2: Total PTS: 20Raquel M. MendozaNessuna valutazione finora
- Med AcronymsDocumento15 pagineMed AcronymsRaquel M. MendozaNessuna valutazione finora
- Activity and Exercise PatternDocumento20 pagineActivity and Exercise PatternRaquel M. MendozaNessuna valutazione finora
- Nursing Responsibilities For Medication AdministrationDocumento9 pagineNursing Responsibilities For Medication AdministrationRaquel M. MendozaNessuna valutazione finora
- Activity and Exercise PatternDocumento20 pagineActivity and Exercise PatternRaquel M. MendozaNessuna valutazione finora
- Activity and ExerciseDocumento36 pagineActivity and ExerciseRaquel M. MendozaNessuna valutazione finora
- Qualities of Health Care ProfessionalsDocumento23 pagineQualities of Health Care ProfessionalsRaquel M. MendozaNessuna valutazione finora
- The Healthcare ProviderDocumento14 pagineThe Healthcare ProviderRaquel M. MendozaNessuna valutazione finora
- Qualities of A Healthcare ProviderDocumento6 pagineQualities of A Healthcare ProviderRaquel M. Mendoza50% (2)
- Communicable DiseasesDocumento14 pagineCommunicable DiseasesRaquel M. MendozaNessuna valutazione finora
- Food Preparation Evaluation Guide: Olivarez College Tagaytay College of NursingDocumento2 pagineFood Preparation Evaluation Guide: Olivarez College Tagaytay College of NursingRaquel M. MendozaNessuna valutazione finora
- Ipt2 U4Documento9 pagineIpt2 U4Paulina BogaczNessuna valutazione finora
- SampleDocumento30 pagineSampleazlizaNessuna valutazione finora
- Yogi Tat Wale BabaDocumento92 pagineYogi Tat Wale BabaTanaNessuna valutazione finora
- How To Improve Your MemoryDocumento8 pagineHow To Improve Your MemorysietuNessuna valutazione finora
- 8 Reasons Why Rich People Hate Their Lives - 4c94778b1e0c4Documento31 pagine8 Reasons Why Rich People Hate Their Lives - 4c94778b1e0c4Ernani Fagundes RodriguesNessuna valutazione finora
- Normal Eeg WavesDocumento23 pagineNormal Eeg WavesvijaykalpanaNessuna valutazione finora
- Impulse 2 SB U1-2Documento32 pagineImpulse 2 SB U1-2marcin.karpowicz0412Nessuna valutazione finora
- Psychiatry Paper-I: Final Exam National Board of Examinations December 2020Documento1 paginaPsychiatry Paper-I: Final Exam National Board of Examinations December 2020isbegin. comNessuna valutazione finora
- What Is The Definition of InsomniaDocumento24 pagineWhat Is The Definition of InsomniaHaniv Prasetya AdhiNessuna valutazione finora
- NCP Risk For FallDocumento20 pagineNCP Risk For FallRen Ren Determinado86% (7)
- The Vivago Watch A Telecare Solution For Cost-Efficient CareDocumento1 paginaThe Vivago Watch A Telecare Solution For Cost-Efficient CareGeronTechnoPlatformNessuna valutazione finora
- By: Reashnaa A/P Loganathan Yunisa Meutia Putri Zahra Fitrianti Preseptor: R.M. Haryadi Karyono, DR., SPKJDocumento51 pagineBy: Reashnaa A/P Loganathan Yunisa Meutia Putri Zahra Fitrianti Preseptor: R.M. Haryadi Karyono, DR., SPKJmeutiaputripuyNessuna valutazione finora
- Polysomnography: Understanding This Technology's Past Might Guide Future DevelopmentsDocumento3 paginePolysomnography: Understanding This Technology's Past Might Guide Future DevelopmentsPhạm Văn HiệpNessuna valutazione finora
- A Read These Statements. How Would You Define The Boldfaced Words?Documento8 pagineA Read These Statements. How Would You Define The Boldfaced Words?Leo GonellNessuna valutazione finora
- NCPDocumento10 pagineNCPMack Jhed AnarconNessuna valutazione finora
- Assessment in Sleep and Rest NeedsDocumento5 pagineAssessment in Sleep and Rest NeedsMaudyMelissa100% (4)
- The Strange Cypher Deck Self PrintDocumento34 pagineThe Strange Cypher Deck Self PrintVernonWilliamReichNessuna valutazione finora
- Test Taking StrategyDocumento7 pagineTest Taking Strategymaría del pilar león riveraNessuna valutazione finora
- The Impact of Sleep Deprivation On Decision Making - ReviewDocumento14 pagineThe Impact of Sleep Deprivation On Decision Making - ReviewAna Viegas100% (1)
- Physical & Cognitive Development in Middle AdulthoodDocumento26 paginePhysical & Cognitive Development in Middle AdulthoodHafsa Awan100% (1)
- Adolescent Sleep Patterns and Insomnia Rates in a Large Population StudyDocumento8 pagineAdolescent Sleep Patterns and Insomnia Rates in a Large Population StudyPradipta ShivaNessuna valutazione finora
- CCM Study Guide Foundations of NursingDocumento46 pagineCCM Study Guide Foundations of NursingAlexandra BrowneNessuna valutazione finora
- Exploring The Sub-Conscious Using New TechnologyDocumento188 pagineExploring The Sub-Conscious Using New TechnologyJuan Pablo Ortiz100% (1)
- Paper 2 FinalDocumento11 paginePaper 2 Finalapi-675118082Nessuna valutazione finora
- Neurobiologically Guided Play TherapyDocumento68 pagineNeurobiologically Guided Play TherapyJen Zhou100% (1)
- How To StudyDocumento28 pagineHow To StudyNadeem Muhammad NadzNessuna valutazione finora
- 961 983 HealthySleepForBabiesDocumento4 pagine961 983 HealthySleepForBabiesAmr GamalNessuna valutazione finora