Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
CXR Made Easy
Caricato da
jaimejmCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
CXR Made Easy
Caricato da
jaimejmCopyright:
Formati disponibili
Education
Chest x rays made easy
In the first of a five part series, Elizabeth Dick takes you through a normal chest x ray
he aim of this five part series is to
L
T give you a basic system for looking
at chest x ray films. They should
enable you to say something sensible
when presented with a film in your finals
and be confident that you are not missing
serious disease when you view a film on
your own as a house officer.
Looking at chest x ray films—the
system
By the time you do finals you will have
learnt a system for examining the
abdomen; you also need to develop a sys-
tem for looking at x ray films. This will
reduce your chances of missing abnor-
malities and it will provide a structured
patter to come out with in exams when
you are under pressure.
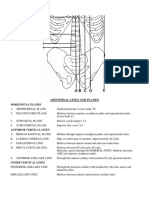
Let’s start by looking at a normal chest
x ray film (fig 1). Use this film as a refer-
ence point during the rest of the article.
Firstly, some technical details: Quickly
look at the film to get some useful infor-
mation about the patient: Trachea
● Male or female? Look for the
presence of breast shadows (this will
help you to notice a mastectomy Superior vena cava
too). Aortic arch
● Old or young? Try to use the patient’s
age to your advantage by making Right hilum and Left hilum
right main bronchus Pulmonary artery
sensible suggestions. A 20 year old is
much less likely to have malignancy branches fan out
1/3
than someone who is 70. Left atrium
● Good inspiration? It’s easy to get tied Right atrium 2/3 Lung peripheries
up in knots over this—and sometimes
not get any further. The diaphragms Left ventricle
should lie at the level of the sixth ribs
anteriorly. The right hemidiaphragm Cardio-phrenic angle
is usually higher than the left because
the liver pushes it up.
Costophrenic angle
● Good penetration? You should just
be able to see the lower thoracic Fig 1 Normal chest x ray film
vertebral bodies through the heart.
● Is the patient rotated? The spinous
processes of the thoracic vertebrae written on the film it is safe to You can summarise all the above infor-
should be midway between the assume it is PA. PA films are better, mation in a simple opening phrase:
medial ends of the clavicles. particularly because the heart is not “This is a frontal chest radiograph of a
● Most chest x ray films are taken as magnified as on an AP film, young male patient. The patient has taken
posterior anterior (PA)—that is, the making it easier to comment on the a good inspiration and is not rotated; the
x rays shoot through from the back heart size. Tip: You can avoid the film is well penetrated.”
of the patient to the x ray plate in whole PA/AP debate by describing While you are saying this keep looking
front of the patient. If the patient is all chest x ray films “frontal”—that at the film.
too sick to stand up for this, an is, you are looking at the patient ● First look at the mediastinal
anterior posterior (AP) film will be straight on. contours—run your eye down the left
done—that is, the x rays shoot ● Finally, some examiners like you to side of the patient and then up the
through from front to back. An call x ray films radiographs; strictly right.
anterior posterior film will always speaking you can’t actually see the ● The trachea should be central. The
be labelled as AP, so if nothing is x rays themselves. aortic arch is the first structure on
316 STUDENT BMJ VOLUME 8 SEPTEMBER 2000
Education
the left, followed by the left L
pulmonary artery; notice how you
can trace the pulmonary artery
branches fanning out through the
lung (see fig 1).
● Two thirds of the heart lies on the left
side of the chest, with one third on
the right. The heart should take up
no more than half of the thoracic
cavity. The left border of the heart is
made up by the left atrium and left
ventricle.
● The right border is made up by the
right atrium alone (the right ventricle
sits anteriorly and therefore does not
have a border on the PA chest x ray
film—a question that examiners love
to ask. Above the right heart border
lies the edge of the superior vena
cava.
● The pulmonary arteries and main
bronchi arise at the left and right
hila. Enlarged lymph nodes can
also occur here, as can primary
tumours. These make the hilum
seem bulky—note the normal size of
the hila on this film. Fig 2 Sclerotic—white metastasis in the right seventh rib
● Now look at the lungs. Apart from
the pulmonary vessels (arteries and
veins), they should be black may be disease of the air spaces or By the time you have gone through
(because they are full of air). Scan interstitium. Don’t forget to look the above, showing that you are looking
both lungs, starting at the apices for a pneumothorax—in which case at the film in a logical fashion, the
and working down, comparing left you would see the sharp line of the examiner should guide you towards the
with right at the same level, just as edge of the lung. abnormality.
you would when listening to the ● Make sure you can see the surface of You may be shown a lateral chest
chest with your stethoscope. The the hemidiaphragms curving x ray (see fig 3), usually to confirm a
lungs extend behind the heart, so downwards, and that the diagnosis you have made on the PA
look here too. Force your eye to costophrenic and cardiophrenic film. Therefore don’t panic when the
look at the periphery of the lungs— angles are not blunted—suggesting an lateral goes up because it means you’ve
you should not see many lung effusion. Check there is no free air probably made the diagnosis. There are
markings here; if you do then there under the hemidiaphragm. only two spaces to look at on the later-
● Finally look at the soft tissues and al film.
bones. Are both breast shadows The heart lies antero-inferiorly. Look
A present? Is there a rib fracture? This at the area anterior and superior to the
would make you look even harder heart. This should be black, because it
for a pneumothorax. Are the bones contains aerated lung. Similarly the area
destroyed or sclerotic? (see fig 2) posterior to the heart should be black
You can summarise your findings as you right down to the hemidiaphragms. The
are looking: “The trachea is central, the blackness in these two areas should be
mediastinum is not displaced. The medi- equivalent; therefore you can compare
astinal contours and hila seem normal. one with the other. If the area anterior
The lungs seem clear, with no pneumo- and superior to the heart is opacified,
thorax. There is no free air under the suspect disease in the anterior medi-
diaphragm. The bones and soft tissues astinum or upper lobes. If the area pos-
seem normal.” terior to the heart is opacified suspect
If you have not seen any abnormality by collapse or consolidation in the lower
this point, say so—“I have not yet identified lobes.
an abnormality so I will now look through
my review areas”—and then look at the Elizabeth Dick specialist registrar in radiology North
“review areas”—places where you can Thames Deanery
easily miss disease. These are:
Acknowledgements: I would like to thank Dr Anju Sahdev,
apices, periphery of the lungs, under Dr Brian Holloway, and Dr Robert Dick for contributing
and behind the hemidiaphragms some of the films shown. Many thanks to Dr Diana
(don’t forget the lungs will extend Fairclough, Dr Robert Dick, and Dr Alex Leff for their help-
Fig 3 Lateral chest x ray (normal) here), and behind the heart. ful comments reviewing these articles.
STUDENT BMJ VOLUME 8 SEPTEMBER 2000 317
Education
Chest x rays made easy
In the second of a five part series, Elizabeth Dick begins to look at chest abnormalities, starting with the
mediastinum and heart
The basics of looking at a chest x ray (recap):
● First look at the mediastinal contours—run
your eye down the left side of the patient
and then up the right.
● The trachea should be central. The aortic
arch is the first structure on the left,
followed by the left pulmonary artery;
notice how you can trace the pulmonary
artery branches fanning out through the
lung (see figure 1).
● Two thirds of the heart lies on the left side
of the chest, with one third on the right.
The heart should take up no more than
half of the thoracic cavity. The left border
of the heart is made up by the left atrium
and left ventricle.
● The right border is made up by the right
atrium alone. Above the right heart border
lies the edge of the superior vena cava.
● The pulmonary arteries and main bronchi
arise at the left and right hila. Enlarged
lymph nodes can also occur here, as can
primary tumours. These make the hilum
seem bulky—note the normal size of the Trachea
hila on this film.
● Now look at the lungs. Apart from the
pulmonary vessels (arteries and veins),
they should be black (because they are full Superior vena cava
of air). Scan both lungs, starting at the Aortic arch
apices and working down, comparing left
with right at the same level, just as you Right hilum and Left hilum
would when listening to the chest with right main bronchus Pulmonary artery
your stethoscope. The lungs extend behind branches fan out
the heart, so look here too. Force your eye 1/3
Left atrium
to look at the periphery of the lungs—you
Right atrium 2/3
should not see many lung markings here; Lung peripheries
if you do then there may be disease of the Left ventricle
air spaces or interstitium. Don’t forget to
look for a pneumothorax.
● Make sure you can see the surface of the Cardio-phrenic angle
hemidiaphragms curving downwards, and
that the costophrenic and cardiophrenic
angles are not blunted—suggesting an
Costophrenic angle
effusion. Check there is no free air under Fig 1 Normal chest x ray film
the hemidiaphragm.
● Finally, look at the soft tissues and bones. Presenting the film
Are both breast shadows present? Is there You can summarise your findings in a few sentences: “The trachea is central, the
a rib fracture? This would make you look mediastinum is not displaced. The mediastinal contours and hila seem normal. The lungs
even harder for a pneumothorax. Are the seem clear, with no pneumothorax. There is no free air under the diaphragm. The bones
bones destroyed or sclerotic? and soft tissues seem normal.”
358 STUDENT BMJ VOLUME 8 OCTOBER 2000 studentbmj.com
Education
Fig 2 Right-sided pleural effusion pushing mediastinum 4
to the left
Fig 5 Left ventricular failure, see text for details
The trachea and mediastinum Similarly, a left sided tension pneu-
are deviated mothorax will push the mediastinum to
The trachea can be pulled or pushed, the right, as air builds up in the left
almost always by one of three processes pleural space and cannot be released
(two that push, one that pulls). A right (fig 3).
Fig 3 Left tension pneumothorax pushing mediastinum to sided pleural effusion will push the tra- On the other hand, if there is collapse
the right (lung edge arrowed) chea and mediastinum to the left (fig 2). on the left this will pull the trachea and
mediastinum to the left side (fig 4). Most
other processes (consolidation, non-
tension pneumothorax, etc) have little
effect on the mediastinum. If you see the
mediastinum is shifted then you need to
think of these three things and look for
them (see future article).
An enlarged heart
The most common reason for the heart to
be enlarged is congestive cardiac failure,
so look for signs of left ventricular failure
on the rest of the film (fig 5). These are:
1 Upper lobe blood diversion. The
pulmonary veins running from the
upper lobes seem more prominent than
those running from the lower lobes.
2 Kerley B lines. These are tiny horizontal
lines from the pleural edge and are
typical of fluid overload with fluid
collecting in the interstitial space.
3 “Bat’s wing” haziness around the hila.
4 Alveolar shadowing. In very severe
pulmonary oedema fluid collects not
only in the interstitial space but in the air
spaces or alveoli. You can recognise this
by seeing hazy shadowing throughout
the lungs, and possibly air bronchograms
Fig 4 Left lower lobe collapse (arrow) with shift of the mediastinum to the left (see future article).
STUDENT BMJ VOLUME 8 OCTOBER 2000 studentbmj.com 359
Education
There are only a few occasions when
there may be the appearance of left ven-
tricular failure (LVF) but a normal sized
heart—in an acute myocardial infarct (sud-
den onset of LVF), or lymphangitis carci-
nomatosa may mimic the appearances of
LVF and be accompanied by a normal
sized heart.
Fig 7 Left hilar carcinoma (arrow)
Fig 6 Primary pulmonary hypertension, both right and
especially left pulmonary arteries are enlarged (arrowed)
Enlarged hila
This could be due to an abnormality in any
of the three structures which lie at the
hilum.
● The pulmonary artery—for example,
pulmonary artery hypertension,
secondary to mitral valve disease;
chronic pulmonary emboli; or
primary pulmonary hypertension
(fig 6).
● The main bronchus—carcinoma
arising in the proximal bronchus
(fig 7).
● Enlarged lymph nodes—caused by
infection, such as tuberculosis—spread
from a primary lung tumour;
lymphoma; or sarcoidosis (fig 8).
Next month: we will look at lung
abnormalities.
Elizabeth Dick, specialist registrar in radiology,
North Thames Deanery
See Web Extra at
studentbmj.com for our
web-based x ray quiz
Fig 8 Bilateral hilar lymphadenopathy (arrowed) due to sarcoidosis
360 STUDENT BMJ VOLUME 8 OCTOBER 2000 studentbmj.com
Education
Chest x rays made easy
In the third of a five part series, Elizabeth Dick looks at abnormalities of the lung fields
The basics of looking at a chest x ray (recap):
● First look at the mediastinal contours—run
your eye down the left side of the patient L
and then up the right.
● The trachea should be central. The aortic
arch is the first structure on the left,
followed by the left pulmonary artery;
notice how you can trace the pulmonary
artery branches fanning out through the
lung (see figure 1).
● Two thirds of the heart lies on the left side
of the chest, with one third on the right.
The heart should take up no more than
half of the thoracic cavity. The left border
of the heart is made up by the left atrium
and left ventricle.
● The right border is made up by the right
atrium alone. Above the right heart border
lies the edge of the superior vena cava.
● The pulmonary arteries and main bronchi
arise at the left and right hila. Enlarged
lymph nodes can also occur here, as can
primary tumours. These make the hilum
seem bulky—note the normal size of the
hila on this film.
● Now look at the lungs. Apart from the
pulmonary vessels (arteries and veins), they
should be black (because they are full of
air). Scan both lungs, starting at the apices
and working down, comparing left with
right at the same level, just as you would
when listening to the chest with your
stethoscope. The lungs extend behind the
heart, so look here too. Force your eye to
look at the periphery of the lungs—you
should not see many lung markings here; if
you do then there may be disease of the air
spaces or interstitium. Don’t forget to look
for a pneumothorax.
● Make sure you can see the surface of the Fig 1 Right pneumothorax. The right side of the lung is blacker, and the lung edge is seen (arrow). There is no
hemidiaphragms curving downwards, and mediastinal shift and therefore no tension
that the costophrenic and cardiophrenic
angles are not blunted—suggesting an ● One half of the lung may seem when air can enter the pleural space
effusion. Check there is no free air under blacker—that is, more radiolucent— (via a hole in the lung surface or the
the hemidiaphragm. than the other, which will be more chest wall) but, because of a ball-valve
● Finally, look at the soft tissues and bones. radio-opaque or whiter. In particular, effect, air cannot leave by the same
Are both breast shadows present? Is there the area beyond the collapsed lung route. So more and more air
a rib fracture? This would make you look will be very radiolucent because there accumulates in the pleural space.
even harder for a pneumothorax. Are the are no pulmonary vessel markings. This pushes the mediastinum over to
bones destroyed or sclerotic?
● You should be able to identify the the opposite (normal) side and
edge of the collapsed lung (see eventually compresses the normal
fig 1). lung so that less inspiration occurs
Pneumothorax on the normal side, with compression
It is important to view around the periph- Having identified a pneumothorax you on the heart and decreased venous
ery of the lungs to look for a pneumotho- need to look for several more associated return until finally the patient arrests
rax (air in the pleural space with associated abnormalities: (see fig 2). Always look for this and
collapsed lung). It is very easy to miss ● Most importantly—this is a pass or fail say: “There is no shift of the
a pneumothorax. Watch out for the observation—is there evidence of a mediastinum and therefore no
following signs: tension pneumothorax? This occurs tension pneumothorax” or “There is
408 STUDENT BMJ VOLUME 8 NOVEMBER 2000 studentbmj.com
Education
shift of the mediastinum away from
the side of the pneumothorax L
indicating a (right/left) tension
pneumothorax. This is a medical
emergency which I would treat
immediately by inserting a large bore
cannula into the (right/left) pleural
space.”
● The cause of the pneumothorax may
be apparent—for example, fracture of
the ribs.
● There may be associated surgical
emphysema—that is, air in the soft
tissues—and air in the mediastinum
(see fig 3).
There is extra shadowing in
the lungs
It may be difficult to work out what is caus-
ing extra shadowing in the lungs, especial-
ly near the mediastinum where normal
structures may overlay the extra shadow-
ing. It is useful to look at the periphery of
the lungs because normally the outermost
edge of the lungs should be fairly black
with a few tapering blood vessels. If you do
see more shadowing in the periphery then
there may be either interstitial or air space
disease. As examiners often show films
with one of these two types of shadowing,
understanding the difference between
these two is worth while because it will help
you to interpret what you see and lead you
to the correct differential diagnosis.
The lung is made up of bronchi, which
branch, at the end of which are alveoli. The
interstitial space (or potential space) sur-
rounds the alveoli. The whole of the lung Fig 2 Left tension pneumothorax with shift of the mediastinum to the right. The lung edge is arrowed
from bronchi to alveoli is the air space—
L that is, it normally contains air. But the
air spaces can fill up—with fluid (such as in
severe pulmonary oedema), with pus (as
in infection), with blood (as in rare diseases
such as Goodpasture’s syndrome, associ-
ated with renal failure), or with tumour
cells (alveolar carcinoma).
Fluid and pus are more common than
the second two. When the air spaces fill up,
the alveoli fill first, with the bronchi being
relatively spared. Therefore the bronchi,
which are still air filled, stand out against
the alveoli, which are filled with pus or
fluid. This is called an air bronchogram
and is simply a sign that there is air space
disease. Consolidation is another term for
air space shadowing (see figs 4 and 5). If
there is air space disease then you need to
work out which part of the lungs it is affect-
ing. A quick way is to use the word “zone”
to describe which part of the lung is affect-
ed. Say something like “There is shadow-
ing in the air spaces of the right mid and
lower zone.” You can then take your time
Fig 3 Surgical emphysema (arrow) and pneumomediastinum (arrowhead) to work out which lobe is affected. You can
STUDENT BMJ VOLUME 8 NOVEMBER 2000 studentbmj.com 409
Education
find out more about lobar anatomy in the
L later section on collapse and consolidation.
Let’s turn to the interstitial space. This
surrounds bronchi, vessels, and groups of
alveoli. When there is disease in the
interstitium it manifests itself by reticulo-
nodular shadowing (criss cross lines or
tiny nodules or both). The main two
processes affecting the interstitium are
accumulation of fluid (occurring in pul-
monary oedema or in lymphangitis carci-
nomatosa) and inflammation leading to
fibrosis (occurring in industrial lung dis-
ease, inflammatory arthritides such as
rheumatoid arthritis, inflammation of
unknown cause such as cryptogenic fibros-
ing alveolitis and sarcoidosis). If you see
criss cross lines or tiny nodules or both say:
“There is reticulo-nodular shadowing with-
in the lower zones.” (See figure 6.)
Use the table to work out whether the
extra shadowing you can see is air space or
interstitial.
Next month: we will look at collapse,
consolidation, and pleural effusions.
Fig 4 Left and right lower lobe air space shadowing in an ITU patient I would like to thank Dr Anju Sahdev,
Dr Brian Holloway, and Dr Robert Dick
for contributing some of the films which
L are illustrated.
Elizabeth Dick, specialist registrar in radiology,
North Thames Deanery
Fig 6 Recticular-nodular shadowing caused by lung fibrosis (circled). Note how the heart has lost its normal smooth
outline and seems “shaggy”
Features of air space and interstitial lung disease
Air space disease Interstitial lung disease
Zones Any Any
Fig 5 Right middle and lower zone consolidation/air
Appearances Confluent shadowing Linear/reticular/nodular
Air bronchograms shadowing
space shadowing. Note air bronchogram (arrow).
There is no loss of volume, which is a key feature of
Causes Fluid (pulmonary oedema, Fluid (pulmonary oedema/ consolidation
(differential adult respiratory distress lymphangitis
diagnoses) syndrome) carcinomatosa)
Pus (infection/consolidation) Inflammation leading to Erratum: see p407.
fibrosis (industrial lung
Blood disease, inflammatory
(Goodpasture’s syndrome) arthritides, inflammation of See Web Extra at
unknown cause, sarcoid) studentbmj.com for our
Tumour cells
(alveolar cell carcinoma) web-based x ray quiz
410 STUDENT BMJ VOLUME 8 NOVEMBER 2000 studentbmj.com
Education
Chest x rays made easy
In the fourth of a five part series, Elizabeth Dick compares collapse and consolidation of the lung and
looks at pleural effusions
The basics of looking at a chest x ray (recap): Normal Frontal view Lateral view
R L
● First look at the mediastinal contours—run Upper Upper
your eye down the left side of the patient lobe lobe
Upper
and then up the right. lobe Post Ant Post Ant
● The trachea should be central. The aortic Horizontal
Oblique fissure Oblique
arch is the first structure on the left, fissure fissure
Horizontal Middle
followed by the left pulmonary artery; fissure Vertebrae lobe
notice how you can trace the pulmonary Lower Lower
artery branches fanning out through the lobe lobe
lung. R Lung L Lung
● Two thirds of the heart lies on the left side
of the chest, with one third on the right. Fig 1 Where the lobes of the lung normally lie
The heart should take up no more than
half of the thoracic cavity. The left border
of the heart is made up by the left atrium Abnormality: lobar collapse
and left ventricle. Collapse of a lobe is caused by proximal
● The right border is made up by the right obstruction—for example, by a neoplasm,
atrium alone. Above the right heart border mucus plug, such as in a postoperative
lies the edge of the superior vena cava. patient, or foreign body, such as in a child.
● The pulmonary arteries and main bronchi Always mention that you are looking for
arise at the left and right hila. Enlarged the cause of the collapse.
lymph nodes can also occur here, as can When the lobe is not aerated it will lose
primary tumours. much of its volume and collapse to a pre-
● Now look at the lungs. Apart from the dictable location depending on whether
pulmonary vessels (arteries and veins), they it is an upper, middle, or lower lobe.
should be black (because they are full of Figure 1 shows the normal site of the
air). Scan both lungs, starting at the apices
lobes of the lung; figures 2 to 5 and their Fig 2 Right upper lobe collapse. Increased shadowing in
and working down, comparing left with
accompanying line diagrams show where the right upper zone with a clear linear border of the
right at the same level, just as you would
when listening to the chest with your
the lobes collapse to. The collapsed lobe horizontal fissure which has been pulled up (arrowhead).
stethoscope. The lungs extend behind the itself can be very difficult to see—there Note the remaining right lung is blacker than the opposite
heart, so look here too. Force your eye to may simply be a little extra shadowing on side. In addition the hilum is pulled up. There is a mass
look at the periphery of the lungs—you the film. A collapsed lobe is a cause of vol- arising from the right hilum (arrow); this is the obstructing
should not see many lung markings here; if ume loss; the other cause is a pneumoth- bronchial carcinoma which is causing the collapse
you do then there may be disease of the air orax. The signs that should alert you to
spaces or interstitium. Don’t forget to look a collapse are due to the loss of lung R Upper lobe collapse Frontal view
for a pneumothorax. volume:
● Make sure you can see the surface of the ● The mediastinum may be shifted Collapsed R
hemidiaphragms curving downwards, and upper lobe
towards the side of collapse
that the costophrenic and cardiophrenic ● The hilum is pulled up or down from Horizontal fissure
pulled up
angles are not blunted—suggesting an where it normally lies
effusion. Check there is no free air under Residual R middle
● The horizontal fissure will also be and lower lobe
the hemidiaphragm. Look for
pulled up (in a right upper lobe expands to compensate proximal
so R side blacker than
● Lateral films: if the area anterior or collapse) or down (right lower lobe L side
obstruction
eg a carcinona
superior to the heart is opacified, suspect
collapse)
disease in the anterior mediastinum or
● The remaining (non-collapsed) lung
upper lobes respectively. If the area
on the side of the collapse has to seem blacker with fewer lung
posterior to the heart is opacified suspect
collapse or consolidation in the lower
expand to fill the hemithorax, thus markings than the opposite normal
lobes. “spreading” its contained vessels; side
therefore the abnormal side will ● The proximal obstruction may be
444 STUDENT BMJ VOLUME 8 DECEMBER 2000 studentbmj.com
Education
L L L
Fig 4a Antero-posterior chest radiograph. Right middle Fig 5a Antero-posterior chest radiograph. Left lower lobe
lobe collapse. The right middle lobe lies adjacent to the collapse. The lower lobes collapse posteriorly and
right heart border, so the right heart outline is lost. inferiorly so that the contour of the hemidiaphragm is
lost. The collapsed left lower lobe may form a “sail”
Fig 3a Antero-posterior chest radiograph, left upper lobe shape behind the heart border on the Antero-posterior
collapse
P A film (arrow)
P A P A
Fig 3b Lateral. Left upper lobe collapse. Increased Fig 4b Lateral, same patient. The right middle lobe
shadowing in the left upper and mid zone with a blurred collapses anteriorly in a wedge shape over the heart. The
lower border. The left heart border is also lost, because upper border of the wedge is the horizontal fissure
the lung collapses adjacent to it. On the lateral view the (arrowhead), the lower border is the oblique fissure
upper lobe can be seen to have collapsed anteriorly and (arrow) Fig 5b On the lateral film there is extra shadowing
lies anterior to the oblique fissure (arrow) posteriorly over the vertebrae due to the collapsed lobe
R Middle lobe collapse (arrow)
L Upper lobe collapse Frontal view Lateral view
Frontal view Lateral view L Lower lobe collapse
Upper zone Upper lobe
veil-like collapses Frontal view Lateral view
shadowing anteriorly L Hilum
with no Horizontal pulled
and fissure
clear superiorly down
lower R Middle
border lobe
Oblique R Middle lobe
lies against heart Oblique
Hilum fissure fissure
border making it
pulled up indistinct L Lower lobe
L Lower lobe collapses
shadowing behind posteriorly
heart with loss of clarity of and inferiorly
medial hemi-diaphragm
visible—for example, a large serous fluid, blood, or pus (fig 7).
carcinoma arising from the right Complete collapse of one lung with the
upper lobe. mediastinum shifting over the the abnor- the two most common, and it can be
mal side can also cause a “white out” on difficult to distinguish between them—of
Abnormality: confluent the abnormal side (fig 8). Finally, after a course, they can coexist.
opacification of the hemithorax pneumonectomy the mediastinum shifts The key features of an effusion are:
There are four main causes of confluent to the empty hemithorax and the resid- ● If the patient is erect there should be
opacification of a hemithorax—consoli- ual pleural space fills with fluid and a fluid level and meniscus visible
dation (fig 6) (that is, material within the fibrotic material leaving the patient with ● If the effusion is large the
air-spaces—see November studentBMJ) a complete “white out” on the side that mediastinum will be shifted to the
and pleural effusion—that is, material has been operated on (fig 9). opposite side. Compare this with
within the pleural space, which could be Consolidation and pleural effusion are pure consolidation in which there is
STUDENT BMJ VOLUME 8 DECEMBER 2000 studentbmj.com 445
Education
L L
Fig 7 Right pleural effusion. There is opacification of the
lower right hemithorax with a fluid level, and the
mediastinum is pushed to the left side
Fig 6a Left lower lobe consolidation. There is opacification of the left lower zone with loss of the hemidiaphragm,
indicating the consolidation abuts the diaphragm—that is, is within the lower lobe. A key feature is that there is no loss
of volume. There is no mediastinal shift and no fluid level Fig 8 Complete collapse of the right lung. A proximal
right main bronchus carcinoma has obstructed the distal
collapse of the lung is accompanied right bronchus and caused complete collapse of the right
P A by a pleural effusion the loss of lung with the trachea and mediastinum pulled to the right
volume (caused by the collapse) may side by the loss of volume on the right. There is also a
be balanced out by the increase in rightsided pleural effusion, best seen superiorly. However,
volume of the hemithorax (caused by the loss of volume due to the right lung collapse is
the effusion) and therefore it may greater than the increase in rightsided volume due to the
seem as if the volume of the pleural effusion so that overall the mediastinum is pulled
hemithorax overall is equivalent to over to the right
the opposite side.
As we discussed in November the key
feature of consolidation is an air bron-
chogram. In infective causes of consolida-
tion the process may affect a lobe (lobar
pneumonia in a distribution according the
normal anatomy shown in fig 1) or spread
in a more patchy distribution (broncho-
pneumonia). Now test yourself with our
web quiz at studentbmj.com.
Fig 6b On the lateral film, air bronchograms can be seen Next month: we will look at lung nod-
within the consolidation which occupies the posterior ules and masses.
lower hemithorax—that is, the normal anatomical site of I would like to thank Dr Anju Sahdev, Fig 9 Left pneumonectomy. The left lung contained a
the left lower lobe Dr Brian Holloway, and Dr Robert Dick carcinoid tumour and was removed. There is left sided
for contributing some of the films which loss of volume with shift of the mediastinum and chest
no change in volume of the are illustrated. wall (ribs) and left hemidiaphragm towards the “empty”
hemithorax and therefore no left hemithorax. The residual space in the left hemithorax
mediastinal shift. There is one caveat Elizabeth Dick, specialist registrar in radiology, North
fills with fluid and fibrotic tissue a few weeks after
to bear in mind, which is that if Thames Deanery pneumonectomy
446 STUDENT BMJ VOLUME 8 DECEMBER 2000 studentbmj.com
Education
Chest x rays made easy
In the final part of the series, Elizabeth Dick looks at lung nodules and masses.
The basics of looking at a chest x ray (recap):
● First look at the mediastinal contours—run L
your eye down the left side of the patient
and then up the right.
● The trachea should be central. The aortic
arch is the first structure on the left,
followed by the left pulmonary artery;
notice how you can trace the pulmonary
artery branches fanning out through the
lung (see figure 1).
● Two thirds of the heart lies on the left side
of the chest, with one third on the right.
The heart should take up no more than
half of the thoracic cavity. The left border
of the heart is made up by the left atrium
and left ventricle.
● The right border is made up by the right
atrium alone. Above the right heart border
lies the edge of the superior vena cava.
● The pulmonary arteries and main bronchi
arise at the left and right hila. Enlarged
lymph nodes can also occur here, as can
primary tumours. These make the hilum
seem bulky—note the normal size of the
hila on this film.
● Now look at the lungs. Apart from the
pulmonary vessels (arteries and veins), they
should be black (because they are full of Fig 1 Miliary tuberculosis. There are multiple small discrete nodules throughout both lungs
air). Scan both lungs, starting at the apices
and working down, comparing left with
right at the same level, just as you would Abnormality: multiple discrete (up to 5 mm) or large. The differential
when listening to the chest with your
nodules in the lungs diagnosis is shown in box 1 and some
stethoscope. The lungs extend behind the
Discrete nodules do not have a reticular of them are illustrated in figures 1, 2,
heart, so look here too. Force your eye to
look at the periphery of the lungs—you
or linear component. They can be small and 3.
should not see many lung markings here; if
you do then there may be disease of the air Box 1– Differential diagnosis of small and large lung nodules
spaces or interstitium. Don’t forget to look
for a pneumothorax. Small nodules (<5 mm)
● Make sure you can see the surface of the ● Miliary tuberculosis (so called because they look like tiny seeds “milia”), due to
hemidiaphragms curving downwards, and haematogenous spread
that the costophrenic and cardiophrenic ● Sarcoid (which can also cause reticulo-nodular shadowing)
angles are not blunted—suggesting an ● Metastases (although they are usually bigger)
effusion. Check there is no free air under ● Pneumoconiosis⎯for example, due to inhaling coal dust. This is rare nowadays
the hemidiaphragm. ● Chickenpox pneumonia
● Finally, look at the soft tissues and bones. Larger nodules/masses (>5 mm)
Are both breast shadows present? Is there ● Common: Metastases (especially breast, testis, gastrointestinal tract, kidney, and
a rib fracture? This would make you look thyroid)
even harder for a pneumothorax. Are the ● Rare: Inflammatory nodules⎯for example, due to vasculitis of rheumatoid
bones destroyed or sclerotic? arthritis or Wegener’s granulomatosis
10 STUDENT BMJ VOLUME 9 FEBRUARY 2001 studentbmj.com
Education
L L
2 1
Fig 4 Previous primary tuberculosis. Both the peripheral
lung nodule (Ghon focus, arrow 1) and the hilar lymph
nodes (arrow 2), which have been infected with
tuberculosis, have calcified.
Fig 2 Multiple miliary lung metastases (arrowed). These were caused by a thyroid carcinoma
L
Fig 5 Secondary tuberculosis. Some consolidation in the
right upper lobe with a cavity (arrowed), typical of
secondary tuberculosis
Abnormality: single nodule or mass
in the lung
The two main causes of a single mass
in the lung are: infection⎯for example,
tuberculosis and neoplasm⎯for
example, primary bronchial tumour or
single metastasis. In both cavitation may
occur.
Other causes of single or multiple mass-
es in the lung are rare. Only mention them
if pressed by an examiner. They include
hydatid cyst and pulmonary arteriovenous
malformation.
Tuberculosis (TB)
Turberculosis has various manifestations
in the lung. In primary tuberculosis there
Fig 3 Multiple small calcified lung nodules (arrowed), most are less than 5mm in diameter. These are caused by previous is a peripheral lung mass (Ghon focus)
chickenpox pneumonia which has calcified. The patient is usually asymptomatic with enlarged hilar lymph nodes (fig 4).
STUDENT BMJ VOLUME 9 FEBRUARY 2001 studentbmj.com 11
Education
Consolidation can also occur. In secondary
L tuberculosis there is patchy consolidation
especially in the upper lobes (fig 5). This
can cavitate. Other manifestations include
pleural effusions and miliary tuberculosis.
Mediastinal lymphadenopathy does not
occur in secondary TB.
Other infections can cavitate, including
pneumonias due to Staphylococcus, Klebsiel-
la, and Cryptococcus. Pneumocystis carinii, as
the name suggests, can form cysts which
are airfilled and have a similar appearance
on an x ray film to cavities (fig 6).
Lung carcinomas can also cavitate, squa-
mous cell carcinomas are the typical his-
tological subtype to do so (fig. 7).
Box 2 – Primary lung carcinoma—
features to look for
● Any site (from central to peripheral
lung)
● May cavitate
Fig 6 Pneumocystis carinii pneumonia in a patient with AIDs. PCP has varied appearances. Here there is an air space
● Spiculated, irregular outline
shadowing in the lower zones plus a cyst in the right upper zone (arrow)
● Distal consolidation or collapse
● Pleural effusion
● Hilar lymphadenopathy
L ● Local bony destruction
● Multiple bony metastases
Apart from cavitation, other features
of lung carcinomas are listed in box 2:
they can occur in the periphery of the
lung or centrally (in or near the medi-
astinum). The outline of the tumour may
be spiculated. Look for associated pleur-
al effusion or hilar lymphadenopathy.
Proximal tumours can cause distal con-
solidation or collapse. Local rib destruc-
tion or multiple bony metastases can also
occur so look for these.
I would like to thank Dr Anju Sahdev,
Dr Brian Holloway, and Dr Robert Dick
for contributing some of the films which
are illustrated.
Elizabeth Dick, specialist registrar in radiology,
North Thames Deanery
See Web Extra at
studentbmj.com for our
web-based x ray quiz
Fig 7 Cavitating right hilar carcinoma (arrow)
12 STUDENT BMJ VOLUME 9 FEBRUARY 2001 studentbmj.com
Potrebbero piacerti anche
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsDa EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsNessuna valutazione finora
- CardiologyDocumento6 pagineCardiologyFrancis FransNessuna valutazione finora
- Valvular Heart Disease 2Documento46 pagineValvular Heart Disease 2Topea BogdanNessuna valutazione finora
- Heart MurmurDocumento7 pagineHeart MurmurChuu Suen TayNessuna valutazione finora
- Fetal ArrhythmiasDocumento18 pagineFetal ArrhythmiasKarin Stefanny Muñoz CastilloNessuna valutazione finora
- Paediatric Radiology QuizDocumento11 paginePaediatric Radiology QuizManju ManjunathNessuna valutazione finora
- Chest Radiology For DummiesDocumento6 pagineChest Radiology For DummiesTom MallinsonNessuna valutazione finora
- Pediatrics ECG by DR Ali Bel KheirDocumento9 paginePediatrics ECG by DR Ali Bel KheirFerasNessuna valutazione finora
- Respiratory Examination - DR - Hammouri's Style: Rahaf Wardeh Internal Medicine 2016-2017Documento5 pagineRespiratory Examination - DR - Hammouri's Style: Rahaf Wardeh Internal Medicine 2016-2017asdddNessuna valutazione finora
- PANCE Prep Pearls Valvular Disease PDFDocumento4 paginePANCE Prep Pearls Valvular Disease PDFkatNessuna valutazione finora
- Cardiovascular ExaminationDocumento13 pagineCardiovascular ExaminationBitu JaaNessuna valutazione finora
- Chest X Rays Made EasyDocumento3 pagineChest X Rays Made EasyHaluk AlibazogluNessuna valutazione finora
- Family Medicine 33: 28-Year-Old Female With Dizziness: Learning ObjectivesDocumento6 pagineFamily Medicine 33: 28-Year-Old Female With Dizziness: Learning ObjectivesAndrea Kristin OrigenesNessuna valutazione finora
- Valvular Heart Disease: Presented by DR Mirjana Milutinovic Professor, SJSMDocumento69 pagineValvular Heart Disease: Presented by DR Mirjana Milutinovic Professor, SJSMAbanoub AwadallaNessuna valutazione finora
- Adult Congenital Heart Disease Board ReviewDocumento79 pagineAdult Congenital Heart Disease Board ReviewKhajornsak Som-UnNessuna valutazione finora
- Assessment of The Chest and LungsDocumento46 pagineAssessment of The Chest and LungsSumathi GopinathNessuna valutazione finora
- Paeds Handbook Class2021 1568487638Documento30 paginePaeds Handbook Class2021 1568487638kafosidNessuna valutazione finora
- Paeds ECG InterpretationDocumento28 paginePaeds ECG InterpretationMuhammad Moazzam GulzarNessuna valutazione finora
- Cardiology A. Woo PDFDocumento52 pagineCardiology A. Woo PDFiuliNessuna valutazione finora
- GI Exam (RCT)Documento6 pagineGI Exam (RCT)kenners100% (11)
- Patient History TemplateDocumento2 paginePatient History TemplateDr Shazana NazrinNessuna valutazione finora
- Approach To TruamaDocumento29 pagineApproach To TruamaIbsa ShumaNessuna valutazione finora
- History Taking: DR - Ahmed Gaber Ass. Prof of Neurology Ain Shams UniversityDocumento81 pagineHistory Taking: DR - Ahmed Gaber Ass. Prof of Neurology Ain Shams UniversityKhaled OssamaNessuna valutazione finora
- EKGDocumento31 pagineEKGJay JiangNessuna valutazione finora
- Medicine1 Grand PE ScriptDocumento10 pagineMedicine1 Grand PE ScriptCarmeline Santi BeronillaNessuna valutazione finora
- Thyroid Exam OSCEDocumento4 pagineThyroid Exam OSCEJon Mark LimNessuna valutazione finora
- Chest X-Ray Interpretation A Structured Approach Radiology OSCEDocumento1 paginaChest X-Ray Interpretation A Structured Approach Radiology OSCEValentina SepúlvedaNessuna valutazione finora
- CXR Lecture DR Lenora FernandezDocumento70 pagineCXR Lecture DR Lenora Fernandezapi-19431894100% (1)
- AnesthesiaDocumento24 pagineAnesthesiaakufahabaNessuna valutazione finora
- Gemp3 Paediatric Clinical Examination SkillsDocumento13 pagineGemp3 Paediatric Clinical Examination SkillsAnna-Tammy HumanNessuna valutazione finora
- Echo Facts IndexDocumento3 pagineEcho Facts Indexs336336anl100% (1)
- Problem-based Approach to Gastroenterology and HepatologyDa EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNessuna valutazione finora
- Intern Survival Guide (UIC)Documento51 pagineIntern Survival Guide (UIC)medstick100% (1)
- Radiological Chest SignsDocumento15 pagineRadiological Chest SignsEzekiel ArtetaNessuna valutazione finora
- ABA OSCE ReviewDocumento25 pagineABA OSCE ReviewJohn Smith100% (1)
- Congenital Heart DiseaseDocumento74 pagineCongenital Heart DiseaseKeith LajotNessuna valutazione finora
- Word AssociationDocumento27 pagineWord AssociationMilan Kolovrat100% (1)
- Chest X - Rays in Pediatric CardiologyDocumento8 pagineChest X - Rays in Pediatric CardiologyAimhigh_PPMNessuna valutazione finora
- Pediatric Cardiology LectureDocumento87 paginePediatric Cardiology LectureMena HashemNessuna valutazione finora
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsDa EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsNessuna valutazione finora
- Adult Congenital Heart Disease Board ReviewDocumento76 pagineAdult Congenital Heart Disease Board ReviewOQAB13Nessuna valutazione finora
- CardiologyDocumento52 pagineCardiologyDexzal100% (2)
- Coronary Artery DiseaseDocumento3 pagineCoronary Artery DiseaseRitz CelsoNessuna valutazione finora
- Neonatal Examination: 2016 EditionDocumento18 pagineNeonatal Examination: 2016 EditionDoha100% (1)
- Pediatric Diagnosis PedDocumento153 paginePediatric Diagnosis PedIceNessuna valutazione finora
- Stroke - Final ReportDocumento16 pagineStroke - Final ReportgolokipokNessuna valutazione finora
- CardiacDocumento10 pagineCardiacMarcus Reynolds100% (1)
- Surgery Tips and ResourcesDocumento2 pagineSurgery Tips and ResourcesAbeebs SalahouNessuna valutazione finora
- Bloom SyndromeDocumento2 pagineBloom SyndromeDrMubashir ShaikhNessuna valutazione finora
- Alert Medical Series: Emergency Medicine Alert IIIDa EverandAlert Medical Series: Emergency Medicine Alert IIINessuna valutazione finora
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsDa EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNessuna valutazione finora
- Torsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandTorsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Pediatric Cardiology and Pulmonology: A Practically Painless ReviewDa EverandPediatric Cardiology and Pulmonology: A Practically Painless ReviewNessuna valutazione finora
- Anesthesia for Congenital Heart DiseaseDa EverandAnesthesia for Congenital Heart DiseaseStephen A. StayerNessuna valutazione finora
- Community-Acquired Pneumonia: Strategies for ManagementDa EverandCommunity-Acquired Pneumonia: Strategies for ManagementAntoni TorresValutazione: 4.5 su 5 stelle4.5/5 (2)
- 2020 Lecture Radiography of Tibia and Fibula and Knee - 2 Per PageDocumento38 pagine2020 Lecture Radiography of Tibia and Fibula and Knee - 2 Per PagejaimejmNessuna valutazione finora
- The Abdomen Part 1Documento13 pagineThe Abdomen Part 1jaimejmNessuna valutazione finora
- Physical Principles of MRS Lab Manual 2020Documento27 paginePhysical Principles of MRS Lab Manual 2020jaimejmNessuna valutazione finora
- Shaderware Installation-1Documento1 paginaShaderware Installation-1jaimejmNessuna valutazione finora
- Surface Anatomy and Spinal LevelsDocumento2 pagineSurface Anatomy and Spinal LevelsjaimejmNessuna valutazione finora
- Protocol GeneralRadiologyUltrasoundDocumento2 pagineProtocol GeneralRadiologyUltrasoundjaimejmNessuna valutazione finora
- 9848 2018 Week 10 Clinical - Introduction 2018Documento19 pagine9848 2018 Week 10 Clinical - Introduction 2018jaimejmNessuna valutazione finora
- 9848 2018 Week 6 - Professionalism and Patient Centred CareDocumento37 pagine9848 2018 Week 6 - Professionalism and Patient Centred CarejaimejmNessuna valutazione finora
- Alcott Littlewomen PDFDocumento414 pagineAlcott Littlewomen PDFjaimejmNessuna valutazione finora
- Asrt12 Bstpracdigradwhp Final PDFDocumento27 pagineAsrt12 Bstpracdigradwhp Final PDFJun F. LaudeNessuna valutazione finora
- 9848 2018 Week 10 Clinical - Introduction 2018Documento19 pagine9848 2018 Week 10 Clinical - Introduction 2018jaimejmNessuna valutazione finora
- Food30010 Tut 2Documento4 pagineFood30010 Tut 2jaimejmNessuna valutazione finora
- 9848 2018 Week 1 - TerminologyDocumento54 pagine9848 2018 Week 1 - TerminologyjaimejmNessuna valutazione finora
- Anat20006 2016-L6.3Documento23 pagineAnat20006 2016-L6.3jaimejmNessuna valutazione finora
- Roses Are Red, Violets Are Blue, Without Your Lungs Your Blood Would Be, Too.Documento249 pagineRoses Are Red, Violets Are Blue, Without Your Lungs Your Blood Would Be, Too.MabesNessuna valutazione finora
- A Rare Case of Vanishing Lung SyndromeDocumento3 pagineA Rare Case of Vanishing Lung SyndromeMUH. RAKIB YUNUSNessuna valutazione finora
- CH 13 Respiratory-SystemDocumento88 pagineCH 13 Respiratory-SystemAntonio Calleja II100% (1)
- AIDA+MEDICAL+STATEMENT+v2 2+june+2019Documento2 pagineAIDA+MEDICAL+STATEMENT+v2 2+june+2019AB OutNessuna valutazione finora
- Respiratory Medicine 151 200Documento31 pagineRespiratory Medicine 151 200Ahmed Kh. Abu Warda100% (2)
- Dental Treatment of Medical Compromised PatientsDocumento50 pagineDental Treatment of Medical Compromised PatientssrinivasNessuna valutazione finora
- NBM18Q&ADocumento11 pagineNBM18Q&AIlse Pol TRuizNessuna valutazione finora
- Prequalification April 2021Documento113 paginePrequalification April 2021RajkumarNessuna valutazione finora
- Science Class 5 NotesDocumento27 pagineScience Class 5 NotesHarshil PatelNessuna valutazione finora
- Physical Examination TemplateDocumento9 paginePhysical Examination Templatedhuha_minozNessuna valutazione finora
- Nursing InterventionsDocumento2 pagineNursing InterventionsJanine Paola CabangilNessuna valutazione finora
- Basic Rowing PhysiologyDocumento17 pagineBasic Rowing Physiologyarab14Nessuna valutazione finora
- Essentials of Microbiology For Dental StudentsDocumento71 pagineEssentials of Microbiology For Dental StudentsRadu FuseaNessuna valutazione finora
- CopdDocumento74 pagineCopdSardor AnorboevNessuna valutazione finora
- Genral Science Notes For Grade SeventhDocumento52 pagineGenral Science Notes For Grade SeventhZohaib AhmadNessuna valutazione finora
- AQG2ndEd 6 12vanadiumDocumento9 pagineAQG2ndEd 6 12vanadiumAlaa SaadNessuna valutazione finora
- The Respiratory SystemDocumento8 pagineThe Respiratory SystemDavid DanielNessuna valutazione finora
- Breathing and Exchange of GasesDocumento8 pagineBreathing and Exchange of GasessuryababaNessuna valutazione finora
- Sputum AnalysisDocumento12 pagineSputum AnalysisAdriana GarciaNessuna valutazione finora
- Acute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesDocumento17 pagineAcute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesCandice ChengNessuna valutazione finora
- Science Form 3 Yearly Lesson PlanDocumento16 pagineScience Form 3 Yearly Lesson PlanAbdul Rahman NarawiNessuna valutazione finora
- Basic Respiratory WebquestDocumento8 pagineBasic Respiratory WebquestWidjaya HS TeacherNessuna valutazione finora
- Group 8: Patient Case History of Present IllnessDocumento4 pagineGroup 8: Patient Case History of Present IllnessShara AboNessuna valutazione finora
- Biology GlossaryDocumento6 pagineBiology GlossarySayam JhaveriNessuna valutazione finora
- ArdsDocumento9 pagineArdsNoel Anthony BadajosNessuna valutazione finora
- Respiratory AssessmentDocumento8 pagineRespiratory AssessmentScott HalNessuna valutazione finora
- Bio4 5Documento11 pagineBio4 5ミーチェルNessuna valutazione finora
- Process ApproachDocumento11 pagineProcess ApproachRaymond Sales EsteriaNessuna valutazione finora
- (Donna Frownfelter PT DPT MA CCS RRT FCCP, ElDocumento827 pagine(Donna Frownfelter PT DPT MA CCS RRT FCCP, ElJeffery Samuel89% (9)
- Concept MapDocumento9 pagineConcept Mapapi-608044542Nessuna valutazione finora