Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Role of Exercises and Drills in The Evaluation of PDF
Caricato da
M Candra MartalinggaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Role of Exercises and Drills in The Evaluation of PDF
Caricato da
M Candra MartalinggaCopyright:
Formati disponibili
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/6893957
Role of exercises and drills in the evaluation of public health in emergency
response
Article in Prehospital and disaster medicine: the official journal of the National Association of EMS Physicians and the World Association for Emergency and Disaster Medicine in
association with the Acute Care Foundation · June 2006
DOI: 10.1017/S1049023X00003642 · Source: PubMed
CITATIONS READS
43 691
4 authors:
Kristine Gebbie Joan Valas
Flinders University Adelphi University
270 PUBLICATIONS 3,085 CITATIONS 3 PUBLICATIONS 43 CITATIONS
SEE PROFILE SEE PROFILE
Jacqueline Merrill Stephen S. Morse
Columbia University Columbia University
66 PUBLICATIONS 959 CITATIONS 183 PUBLICATIONS 4,479 CITATIONS
SEE PROFILE SEE PROFILE
Some of the authors of this publication are also working on these related projects:
National Science Foundation - Mass Fatality management Project View project
Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Literature Reviews View project
All content following this page was uploaded by Stephen S. Morse on 22 May 2014.
The user has requested enhancement of the downloaded file.
ORIGINAL RESEARCH
Role of Exercises and Drills in the Evaluation
of Public Health in Emergency Response
Kristine M. Gebbie, DrPH, RN;1 Joan Valas, MS, RN;1 Jacqueline Merrill, MPH RN;1
Stephen Morse, PhD2
Abstract
1. Center for Health Policy, Columbia Introduction: Public health agencies have been participating in emergency
University School of Nursing, New York, preparedness exercises for many years. A poorly designed or executed exercise,
New York USA or an unevaluated or inadequately evaluated plan, may do more harm than
2. National Center for Disaster good if it leads to a false sense of security, and results in poor performance
Preparedness, Mailman School of Public during an actual emergency. At the time this project began, there were no
Health, Columbia University, New York, specific standards for the public health aspects of exercises and drills, and no
New York USA defined criteria for the evaluation of agency performance in public health.
Objective: The objective of this study was to develop defined criteria for the
Correspondence: evaluation of agency performance.
Joan Valas, MS, RN Method: A Delphi panel of 26 experts in the field participated in developing
Columbia University School of Nursing criteria to assist in the evaluation of emergency exercise performance, and
Center for Health Policy facilitate measuring improvement over time. Candidate criteria were based on
630 West 168th Street-Mail Code 6 the usual parts of an emergency plan and three other frameworks used else-
New York, NY 10032 USA where in public health or emergency response.
E-mail: jv16@columbia.edu Results: The response rate from the expert panel for Delphi Round I was
74%, and for Delphi Round II was 55%. This final menu included 46 public
Keywords: agency; criteria; emergency health-agency level criteria grouped into nine categories for use in evaluating
response; evaluation; event; exercises; drills; an emergency drill or exercise at the local public health level.
performance; public health; readiness; Conclusion: Use of the public health-specific criteria developed through this
standards process will allow for specific assessment and planning for measurable
improvement in a health agency over time.
Abbreviations:
CDC = Centers for Disease Control and Gebbie KM, Valas J, Merrill J, Morse S: Role of exercises and drills in the
Prevention evaluation of public health in emergency response. Prehosp Disast Med
DHS = (US) Department of Homeland 2006;21(3):173–182.
Security
FEMA = (US) Federal Emergency
Introduction
Management Agency
The roles of exercises and drills as a mechanisms for education, experience,
IAP = incident action plan
and evaluation of emergency response have increasingly become important
IC = incident command
for all response partners, including the public health system.1–3 The ability of
ICS = incident command system
the public health community to perform exercises, drills, and emergency sim-
JIC = jurisdiction-wide information center
ulations for both internal and external evaluation of plan effectiveness has
NACCHO = (US) National Association of
been improving, and includes greater involvement and more ties to other
County and City Health Officials
components of the response system. The objectives of the research are: (1) to
PIO = public information officer
clearly describe the levels of exercises and drills appropriate to levels of pre-
PPE = personal protective equipment
paredness, the purpose of the drill (management and leadership, operational
SOCO = single overriding communication
performance or systems performance), and the size of the agency and com-
objective
munity served; and (2) to develop a standardized set of criteria for use by local
UTL = universal task list
public health agencies or others to evaluate an agency’s response during a
drill, exercise, actual emergency event, or after-exercise evaluation are
Received: 22 June 2005
described in this report. In addition, a subsequent phase of the same project
Accepted: 19 July 2005
was undertaken to develop a standardized method for recording a drill or
Revised: 02 August 2005
exercise experience that can be used for the evaluation and documentation of
public health readiness.
Web publication: 21 June 2006
The emergency response readiness of the public health system increasing-
ly has been an important topic for research, development, and action in the
May – June 2006 http://pdm.medicine.wisc.edu Prehospital and Disaster Medicine
174 Role of Exercise and Drills
United States since 1996, with the events of 11 September One major challenge to this project was that public
2001 providing even more stimulus.4–6 This research health agencies already had been conducting or participat-
included: ing in exercises and drills, using a wide range of resources
1. the development of competencies in emergency pre- and working with US national, state, and local emergency
paredness for individual public health workers;2 preparedness organizations, the national network of
2. training for public health agency staff and their com- Academic Centers for Public Health Preparedness, and pri-
munity partners;4,7 vate consulting firms. This resulted in a lack of standardiza-
3. improved electronic and other communication tion that produced different vocabularies, expectations, and
capacities at all levels of public health practice;8,9 thus, different approaches in exercise assessment in the US.
4. federal guidance to state public health agencies (and The purpose of this study was to describe the levels of exer-
through state agencies to local public health agen- cises and drills appropriate to levels of preparedness and the
cies) on critical agency capacities needed for emer- purpose of these drills, and to develop a standardized set of
gency response;3 criteria for use by local public health agencies to evaluate an
5. strengthened planning for emergency response agency’s response during an exercise.
throughout the public health community;10 and
6. the creation of Project Public Health Ready, a system Methods
that certifies that a local public health agency has a To develop criteria using expert opinions, this Delphi study
staff competent in emergency response, a plan for was conducted at the Center of Health Policy at the
emergency response, and has tested its preparedness Columbia University School of Nursing. The study was
through exercises or drills.11 determined to be exempt from Institutional Research
Board approval on 02 January 2004.
Need for Exercises The first step in this study was to define the types and
Public health agencies have been participating in at least levels of exercises based on critical review of existing
some emergency preparedness exercises for many years, national standard language developed by the DHS.21 This
(e.g., the participation of local public health agencies in review resulted in a document that was circulated in the
emergency drills in the area surrounding nuclear power public health community for feedback and comment.
plants).12 Many jurisdictions have regular experiences with Subsequently, it was made available in its final form via the
emergencies caused by weather.6 However, a poorly designed project Website, and is summarized in Table 1.20
or executed exercise, or an unevaluated or inadequately The second step was to identify criteria for evaluating
evaluated plan, may do more harm than good if it leads to local public health emergency exercises. This was achieved
a false sense of security, resulting in poor performance dur- through a two-round Delphi survey utilizing a 26-member
ing an actual emergency. Also, the public may be put at risk expert panel to gain insight and consensus to the develop-
and confidence in the public health system undermined. ment of public health agency criteria for the evaluation of
The National Association of County and City Health emergency exercises. The experts for this panel were select-
Officials (NACCHO) has provided a useful tool, Bt ed based on experience and expertise from representative
Create, that guides an agency through the development of public health professional associations (boards of health,
a locally relevant exercise or drill.13 However, at the time local and state health officials), local and state public health
this project began, public health had not developed its own agencies, the Centers for Disease Control and Prevention
specific standards for the public health aspects of exercises (CDC), the DHS, and the Federal Emergency Management
and drills, and no defined criteria for the evaluation of Agency (FEMA). Special attention also was given to select-
agency performance existed. ing a panel that included representatives from each of the
Because exercises and drills are expected to provide a ten geographic regions of the country. The composition of
simulation of actual emergency experiences, the format for the panel is summarized in Table 2.
assessing response during a drill or exercise should be the
template for evaluation of an actual response.8,12 Evaluating Delphi Survey Round I
the degree to which the exercise and its results are used for Project staff reviewed an extensive range of materials from
ongoing organizational development also is crucial. There the DHS, the FEMA, the Centers for Public Health
currently are no published guidelines for assessing public Preparedness (funded by the CDC), and local public health
health emergency response. General guidelines developed departments. In developing the Round I Delphi instru-
by the US Department of Homeland Security (DHS) have ment, it was decided to present criteria for the evaluation
been developed, but are not specific for the public health of public health exercises in a manner consistent with and
agency role, both at the state and local levels.19 It is essen- understandable to those working in the broader emergency
tial that the evaluation of emergency response at the local management area. For that reason, the researchers chose to
level be consistent with expectations of emergency organize the document in categories identified by the
response at the state public health agency level, thus assur- major components of a public health agency emergency
ing that critical elements of response are developed in a management plan as described by NACCHO, which is a
consistent manner. Since this project began, several US format consistent with more general emergency plans.
organizations started initiatives that increase contribution However, because other ways of describing public health
from public health within the emergency response sector. performance or emergency response are in use, each of the
Prehospital and Disaster Medicine http://pdm.medicine.wisc.edu Vol. 21, No. 3
Gebbie, Valas, Merrill, et al 175
Type of Exercise Definition Examples
The starting points in a building block
approach to exercises. Primarily used
to familiarize agency and staff with Seminar Workshop
Discussion-Based Exercises existing plans and capabilities. Led by Tabletop
facilitators and presenters to keep Games
participants on track in meeting the
objectives of the exercise.
Used for the purpose of assessing and
validating emergency preparedness
polices, plans, and procedures. They
Drill
include drills, functional exercises, and
Operation-Based Exercises Functional Exercise
full-scale exercises. There is an actual
Full-Scale Exercise (FSE)
response and a mobilization of
personnel and apparatus over a
designated, extended period of time.
Gebbie © 2006 Prehospital and Disaster Medicine
Table 1—Summary of definitions
Expert Panel Respondents (n = 26) Range of Representation
State or Local Public Health Official/Practitioner 14 State and Local Public Health Agencies
DHS/FEMA Regions I, II, III, IV, V, VII, VII, IX, X
National Response Agencies Centers for Disease Control, FEMA, DHS
Association for State and Territorial Health Officials, National
Association of City and County Health Officials, National
Public Health Professional Organizations
Association of National Boards of Health, National
Environmental Health Association
Public Health Practice, Risk Communication, Disaster
Public Health Disaster Specialists/Academia
Management
Gebbie © 2006 Prehospital and Disaster Medicine
Table 2—Professions represented in the expert panel composition (DHS = Department of Homeland Security;
FEMA = Federal Emergency Management Agency; n = number)
plan components was also compared to components of potential criterion and respond whether it should be
three other frameworks: (1) components used by general retained, modified, or eliminated. Additionally, they were
emergency management;21–23 (2) Public Health in America’s asked to comment on the proposed criteria and suggest
essential services of public health;24 and (3) the focus plan- additional criteria. The Round I instrument was pilot-test-
ning areas of the CDC state emergency plan guidance in ed by four public health experts familiar with emergency
use at the time.25 The comparative framework was includ- response and emergency plan design, and slight adjustments
ed in Round I for the purpose of explaining and grouping in wording and format were made based on their feedback.
potential criteria the research team selected for considera- The survey was administered by mail and electronically
tion by the experts. (reflecting panelist preferences). Suggested modifications
For each category, the project team generated potential focused on adjusting the agency response times stipulated
criteria that could measure actions likely to be taken by in the potential criteria. Other suggested modifications
public health agencies during an emergency or a disaster. primarily were to clarify language. Reasons for proposing
For example, under the category “Initial Response rejection of criteria centered on redundant language, or
Command and Control” an initial draft criterion was: panelists’ knowledge of a particular health department’s
health department internal incident commander is identi- non-participation in a specific activity, related to a criteri-
fied immediately on notification that emergency manage- on. Only four criteria were not retained by the panel.
ment will be used in response to an incident. A total of 50
potential agency level criteria corresponding to 10 separate Delphi Survey Round II
categories were originally sent out. In Round I of the Based on the results of Round I, the Round II survey
Delphi survey, panel members were asked to read each instrument grouped 46 potential criteria into nine cate-
May – June 2006 http://pdm.medicine.wisc.edu Prehospital and Disaster Medicine
176 Role of Exercise and Drills
Gebbie © 2006 Prehospital and Disaster Medicine
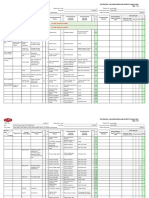
Figure 1—Exercise flow chart
gories: (1) initial response command and control; (2) com- respondents, resulting in 46 potential criteria. These 46 cri-
munication; (3) early recognition/surveillance and epi- teria served as the basis for Round II. In Round II, >80%
demiology; (4) sample testing; (5) evidence management; of respondents were in agreement with retaining all 46 cri-
(6) mass prophylaxis, immunization, and pharmaceutical teria presented. Eighty percent of respondents agreed with
stockpiles; (7) mass-patient care; (8) mass-fatality manage- retaining the potential criteria as written. The response rate
ment; and (9) environmental surety. All non-conflicting for Delphi Survey Round II was 74%.
editorial suggestions from Round I were included. Where In the last step of this research, the results of Round II
there were conflicting responses from the panel, changes were used as the basis for a final menu of criteria for use in
suggested by the majority of panelists were included. evaluating an emergency drill or exercise at the local public
Where there was no clear consensus, the research team health level. The research team selected the final criteria
decided on the best alternative for inclusion. The instru- based on the majority opinion of the response panel. For
ment also provided feedback to the expert panel consisting purpose of clarity, the team separated criteria that con-
of: (1) the individual panelist’s scores for each item in tained composite actions, so that each resulting criterion
Round I; and (2) the range of scores for each criterion in all had only one action verb and was stated in an observable
10 categories of plan response. format. This final document was circulated to the expert
In response to questions asked by panelists, the research panel for a final round of comments. The final set of crite-
team developed a flow chart (Figure 1) to illustrate where ria is shown in Table 3.
in the process of developing a drill or exercise one or more
criteria from the Round II menu of criteria could be select- Discussion
ed for use in exercise evaluation. The US Homeland Security Exercise Evaluation Program
The Round II survey was pilot tested again with four provides exercise evaluation guidelines for conducting and
public health experts, and minor adjustments were made observing exercise activities.21–23 Within that document,
before distribution. Again, the expert panelists were asked to the guidelines for public health lacked detail when this
review the criteria as they did in Round I. Round II also was project began. Once validated, use of the public health-spe-
administered by mail and e-mail. Suggested modifications cific criteria that were developed through this research
were based primarily on language clarification and disputed would allow for specific assessment and planning for mea-
response times. Criteria were rejected for similar reasons as surable improvement over time in a health agency. The
in Round I, and once again, few criteria were rejected. researchers plan to integrate these criteria into a format
that can be used by exercise observers to record the events
Results that take place in an exercise, and to use these observations
The response rate for Delphi Survey Round I was 74% and in an analysis of agency performance. Preliminary applica-
55% for Round II. Based on Round I responses, criteria tion in a limited number of exercises suggests that using
were eliminated, reused, or others were suggested by the structured criteria minimizes subjective interpretation.
Prehospital and Disaster Medicine http://pdm.medicine.wisc.edu Vol. 21, No. 3
Gebbie, Valas, Merrill, et al 177
I. Initial Response Command and Control
1. Health department internal incident commander is identified immediately on notification that emergency management will be
used in response to an incident.
2. All health department internal ICS positions (PIO, Liaison, Safety Officer, needed section chiefs) are identified and activated*
within 30 minutes regardless of time of day.
3. All initial, available, relevant information centralized to the agency’s ICS Planning Section using a situation board or
equivalent within 15 minutes.
4. Establish an IAP describing primary objectives and overall strategy to be accomplished by the health department in the first
24 hours within 30 minutes after the establishment of the department’s EOC.
5. Activate appropriate ICS General Staff Sections within 60 minutes of initial activation of internal incident commander.
6. Portions of state/local public health law/code relevant to the specific emergency retrieved and available to ICS Command
Staff.
7. Activate plan for operating/closing routine health department operations within 30 minutes of initial activation of internal
incident commander
II. Communication
1. Establish liaison with JIC within 15 minutes of notifying the incident commander that the JIC is operational.
2. Draft and approve public information for anticipated phases of response within two hours. Draft and approve public
information for anticipated phases of response within two hours of establishment of agency’s EOC.
3. Identify critical partners (e.g., other health jurisdictions, law enforcement, hospitals, etc.) and convey initial public health
information to them immediately upon approval of information and no later than one hour after approval of information by
agency JIC.
4. Establish a schedule to update partners regularly.
5. Test back-up communication procedures.
6. Identify a public health spokesperson appropriate to the emergency (e.g., Health Director, Epidemiologist).
7. SOCO developed, conveyed through ICS structure.
8. SOCO updated and distributed (e.g., posted to Situation Boards) as needed, but at least every four hours (maximum).
Gebbie © 2006 Prehospital and Disaster Medicine
Table 3—Menu of criteria for evaluation of local public health emergency drills and exercises (EOC = emergency
operations center; IAP = incident action plan; ICS = incident command system; JIC = jurisdiction-wide
information center; PIO = public information officer; SOCO = single overriding communications objective)
*activated = notified and in communication, not necessarily on-site continued
May – June 2006 http://pdm.medicine.wisc.edu Prehospital and Disaster Medicine
178 Role of Exercise and Drills
III. Early Recognition/Surveillance and Epidemology
1. Event/incident specific surveillance is established within 60 minutes of establishing the EOC.
2. Establish a preliminary case definition.
3. Adjustments to surveillance communicated as needed to and from the internal health public health IC.
4. Changes/enhancements in surveillance implemented within one hour of approval by the internal public health IC.
5. Epidemiology investigation plan including tools and forms completed within two hours of establishing the agency’s EOC.
6. Field Staff appropriately prepared and protected prior to deployment.
7. Establish time interval for updating epidemiology investigation plan based on reassessment of information.
IV. Sample Testing
1. Laboratory resources and requirements specific to agent/incident selected.
2. Specific protocols and procedures for collection of samples relevant to the specific emergency available within 60 minutes
of notification of incident by IC.
3. Ensure case investigators appropriately prepared and protected in PPE prior to deployment.
4. Field workers deployed to sites within 60 minutes of final IAP.
5. Samples properly packed and shipped/transported consistent with laboratory requirements.
Gebbie © 2006 Prehospital and Disaster Medicine
Table 3 (continued from page 177)—Menu of criteria for evaluation of local public health emergency drills and exer-
cises (EOC = emergency operations center; IAP = incident action plan; IC = incident command; PPE = personal
protective equipment) continued
When combined with narrative accounts from participants Recent publication of a Universal Task List (UTL) cov-
and observers, the criteria can contribute to the production ering actions to be taken by the various emergency
of a more detailed, robust “After Action Report”. More response sectors has raised questions about the use of the
importantly, because criteria reflect measures of tasks and criteria reported here. The UTL organizes tasks according
activities performed as part of an emergency response plan, to the four US Homeland Security Missions: Prevent,
they are likely to facilitate writing a more precise improve- Protect, Respond, and Recover. The criteria developed by
ment plan and be easily adapted for use in updating emer- this research can provide the metrics by which successful
gency response plans. completion of tasks may be measured. The UTL tasks in
Prehospital and Disaster Medicine http://pdm.medicine.wisc.edu Vol. 21, No. 3
Gebbie, Valas, Merrill, et al 179
V. Evidence Management
1. Evidentiary requirements confirmed with relevant agencies through jurisdiction-wide National Incident Management System
partners, prior to collection of personal or environmental samples.
2. Coordinated arrangements for maintaining chain of evidence in place prior to collection of any samples/specimens.
VI. Mass Prophylaxis and Immunization and Pharmaceutical Stockpiles
1. Generic mass dispensing strategy adapted to specific event within 60 minutes of notification.
2. Dispensing sites are staffed with adequate and appropriately staffed personnel for mass dispensing (including volunteer
surge staff) prior planned to site opening time.
3. Needed “just in time” training including use of PPE identified and requested at least two hours prior to planned opening of
sites.
4. System in place to restock supplies throughout duration of site operation.
5. System in place to rotate or relieve staff during site operation.
6. All needed record keeping supplies prepared and delivered for opening mass dispensing sites prepared and delivered to
site coordinators by opening of site(s).
VII. Mass-Patient Care
1. Generic mass care strategy adapted to specific event within 60 minutes of notification.
2. Mass care sites are staffed with adequate and appropriately staffed personnel (including volunteer surge staff) prior to
opening.
3. Needed “just in time” training including use of PPE identified and requested at least two hours prior to planned opening of
sites.
4. System in place to restock supplies throughout duration of site operation.
5. System in place to rotate or relieve staff during site operation.
6. All needed record keeping supplies prepared and delivered for opening mass dispensing sites prepared and delivered to
site coordinators by opening of site(s).
VIII. Mass-Fatality Management
1. If needed, identify suitable facility prior to dispatch of pick-up vehicles.
2. Develop plan for transport bodies, including routes and expected timeframes prior to dispatch of pick-up vehicles.
IX. Environmental Surety
1. Develop/adapt strategy for control of environment rendered hazardous by this event within 30 minutes of site identification.
2. Identify specific characteristics of affected areas and report to incident commander within 30 minutes of arrival on site.
3. Establish PPE criteria for staff.
Gebbie © 2006 Prehospital and Disaster Medicine
Table 3 (continued from page 178)—Menu of criteria for evaluation of local public health emergency drills and
exercises (PPE = personal protective equipment)
May – June 2006 http://pdm.medicine.wisc.edu Prehospital and Disaster Medicine
180 Role of Exercise and Drills
Function Universal Task List Item Local Public Health Criteria
VI. Mass Prophylaxis & Immunization and
Pharmaceutical Stockpiles
1. Generic mass dispensing strategy adapted to specific
event within 60 minutes of notification.
2. Dispensing sites are staffed with adequate and
appropriately staffed personnel for mass dispensing
(including volunteer surge staff) prior to planned site
opening time.
#1.1.1.2 Develop plans, procedures,
and protocols to implement 3. Needed “just in time” training, including use of PPE
national pharmaceutical stockpile identifed and requested at least two hours prior to
operations planned opening of sites.
4. System in place to restock supplies throughout
duration of site operation.
5. System in place to rotate or relieve staff during site
operation.
6. All needed record keeping supplies prepared and
delivered for opening mass dispensing sites prepared
and delivered to site coordinator by opening of site(s).
IV. Sample Testing
1. Laboratory resources and requirements specific to
agent/incident selected.
2. Specific protocols and procedures for collection of
samples relevant to the specific emergency available
Misson: Protection within 60 minutes of notification of incident by IC.
#1.1.2 Develop laboratory plans,
(Pro.C.1.) procedures, and protocols
3. Ensure case investigators appropriately prepared and
protected in PPE prior to deployment.
4. Field workers deployed to sites within 60 minutes of
final IAP.
5. Samples properly packed and shipped/transported
consistent with laboratory requirements.
III. Early Recognition/Surveillance and Epidemiology
1. Event/incident specific surveillance is established
within 60 minutes of establishing the EOC.
2. Establish a preliminary case definition.
3. Adjustments to surveillance communicated as needed
to and from the internal health public health IC.
4. Changes/enhancements in surveillance implemented
#1.1.3 Develop plans and within one hour of approval by the internal public
procedures for disease outbreak health IC.
5. Epidemiology investigation plan including tools and
forms completed within 2 hours of establishing the
agency’s EOC.
6. Field Staff appropriately prepared and protected prior
to deployment.
7. Establish time interval for updating epidemiology
investigation plan based on reassessment of
information.
Gebbie © 2006 Prehospital and Disaster Medicine
Table 4—Relationship of universal task list items to exercise evaluation criteria (EOC = emergency operations
center; IAP = incident action plan; IC = incident command; PPE = personal protective equipment) continued
Prehospital and Disaster Medicine http://pdm.medicine.wisc.edu Vol. 21, No. 3
Gebbie, Valas, Merrill, et al 181
Function Universal Task List Item Local Public Health Criteria
VII. Mass Patient Care
1. Generic mass care strategy adapted to specific event
within 60 minutes of notification.
2. Mass care sites are staffed with adequate and
#1.1 Develop plans, procedures, appropriate personnel (including volunteer surge staff)
and protocols for the immediate prior to opening.
provision of mass care services 3. Needed “just in time” training including use of PPE
Misson:Response to shelters for disaster victims to identified and requested at least two hours prior to
(Res.C.3) include shelter, feeding, basic planned opening of sites.
first aid, bulk distribution of
needed items, and other related
4. System in place to restock supplies throughout duration
services
of site operation.
5. System in place to rotate or relieve staff during site
operation.
6. All needed patient record keeping supplies prepared
and delivered for opening mass care sites prepared and
delivered to site cooordinator by opening of site(s).
Gebbie © 2006 Prehospital and Disaster Medicine
Table 4 (continued from page 180)—Relationship of universal task list items to exercise evaluation criteria
(PPE = personal protective equipment)
two mission areas for which the public health criteria may The research team notes that limitations of this research may
be used for measurement are listed in Table 4. be attributed to the 74% response rate from the expert panel.
With any Delphi research approach, there is one per-
spective on the topic of interest. The researchers made Conclusion
every effort to acheive inclusion of those with an interest in Public health agencies must be able to measure perfor-
emergency response in the local public health level, with- mance and identify areas for improvement. This can be
out regard to known perspective on the question of criteria. done through ongoing training and emergency response
The range of responses to the first round indicates that this exercising, and through the use of response exercises that
was accomplished. It is impossible to fully interpret the include plans for evaluation. The criteria developed
lower response rate to the second round. The non-respon- through this research are essential for those purposes.
dents did not represent any one constituency or interest Preparedness and response are dynamic processes, as
group, and the researchers’ observation is that this round threats change and weaknesses are identified. Capacity is
coincided with a busy time of grant renewals and other continuously built through planning, exercising, evaluating,
demands for time from the experts involved with this study. and improving.
References
1. Cope JR: Workforce Competencies for emergency preparedness NACCHO 8. Simmons SC, Murphy TA, Blanarovich A, et al: Telehealth technologies and
Exchange 2003;1(2):1–2. applications for terrorism response: A report of the 2002 coastal North
2. Centers for Disease Control and Prevention. Bioterrorism & emergency readi- Carolina domestic preparedness training exercise. J Am Inform Assoc
ness: competencies for all public health workers. Available at http://www.nurs- 2003;10(2):166–176.
ing.hs.columbia.edu/institute-centers/chphsr/btcomps.html. Accessed 14 June 9. Centers for Disease Control and Prevention. Health alert network. Available
2005. at http://www.phppo.cdc.gov/han/Index.asp2001. Accessed 14 June 2005.
3. Centers for Disease Control and Prevention. Capacity inventory. Available at 10. New York City Office of Emergency Management. Keeping New York pre-
http://www.phppo.cdc.gov/od/inventory/index.asp. Accessed 14 June 2005. pared: An overview of the New York City Office of Emergency
4. Allan S: The challenges of local preparedness for bioterrorism and other Management. http://nyc.gov/htm/oem/pdf/oem_briefing_document.pdf.
emergencies. NACCHO Exchange 2002;1(1):1–5. Accessed 14 June 2005.
5. Firshien J: Public health preparedness for disaster: Perspective from 11. National Association of County and City Health Officials: Project Public
Washington, D.C. J Urban Health 2002;79(1):6–7. Health Ready. Available at http://www.naccho.org/topics/emergency/pphr.cfm.
6. Barbera JA, MacIntyre AG: The reality of the modern bioterrorism response. Accessed 14 June 2005.
In: The Lancet Supplement Vol. 360. Available at http://thelancet.com. 12. Ford JK, Schmidt AM: Emergency response training: Strategies for enhancing
Accessed 14 June 2005. real world performance. Journal of Hazardous Material 2000;75(2–3):195–215.
7. Morse A: Bioterrorism Preparedness for Local Health Departments. 13. National Association of County and City Health Officials. Bt Create: A cus-
J Community Health Nurs 2002;19(4):203–211. tomizable bioterrorism tabletop exercise builder. Available at http://www.nac-
cho.org/prod141.cfm. Accessed 14 June 2005.
14. Gebbie KM, Merrill JA, Hwang I, et al: Identifying individual competency
in emerging areas of practice: An applied approach. Qual Health Res
2002;12(7):990–999.
May – June 2006 http://pdm.medicine.wisc.edu Prehospital and Disaster Medicine
182 Role of Exercise and Drills
15. Turnock BJ: Roadmap for public health workforce preparedness. J Public 21. US Department of Homeland Security, Office for Domestic Preparedness:
Health Manag Pract 2003;9(6):471–480. Homeland security exercise and evaluation program—Volume I: Overview
16. Kerby DS, Brand MW, Johnson DL, Ghouri FS: Self-assessment in the and doctrine. Available at http://www.ojp.usdoj.gov/odp/docs/HSEEPv1.pdf.
measurement of public health workforce preparedness for bioterrorism or Accessed 14 June 2005.
other public health disasters. Public Health Rep 2005;120(2):186–191. 22. US Department of Homeland Security, Office for Domestic Preparedness:
17. Qureshi KA, Gershon RR, Merrill JA, et al: Effectiveness of an emergency Homeland Security Exercise and Evaluation Program—Volume II: Exercise
preparedness training program for public health nurses in New York City. Evaluation and Improvement. Available at http://www.ojp.usdoj.gov/odp/
Fam Community Health 2004;27(3):242–249. docs/HSEEPv1.pdf. Accessed 14 June 2005.
18. Columbia University School of Nursing, Center for Health Policy: Clinical 23. US Department of Homeland Security, Office for Domestic Preparedness:
competencies during initial assessment and management of emergency Homeland security exercise and evaluation program—Volume III: Exercise
events. Available at http://www.cumc.columbia.edu/dept/nursing/institutes- program management and exercise planning process. Available at
centers/chphsr/clinician-comps.pdf. Accessed 14 June 2005. http://www.ojp.usdoj.gov/odp/docs/HSEEPv3.pdf. Accessed 14 June 2005.
19. US Department of Homeland Security, Federal Emergency Management 24. Public Health Functions Steering Committee: Public health in American
Agency: State and local guide (SLG) 101: Guide of all-hazards emergency essential public health services. Available at http://www.health.gov/phfunc-
operations planning. Available at http://www.fema.gov.pdf/rrr/slf101.pdf. tions/public.htm. Accessed 14 June 2005.
Accessed 14 June 2005. 25. Centers for Disease Control and Prevention: Continuation guidance for
20. Columbia University School of Nursing Center for Health Policy: Defining cooperative agreement on public health preparedness and response for
emergency exercises: A working guide to the terminology. Available at bioterrorism—Budget year five. Available at http://www.bt.cdc.gov/plan-
http://www.cumc.columbia.edu/dept/nursing/institutes-centers/chphsr/def- ning/continuationguidance/index.asp. Accessed 14 June 2005.
exer.pdf. Accessed 14 June 2005.
Prehospital and Disaster Medicine http://pdm.medicine.wisc.edu Vol. 21, No. 3
View publication stats
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- I. About Graphs: What Is A Graph?Documento29 pagineI. About Graphs: What Is A Graph?Mae DinDinNessuna valutazione finora
- CHAPTER 1-ResearchDocumento3 pagineCHAPTER 1-ResearchLyn Valles100% (3)
- Personal Data: Curriculum VitaeDocumento4 paginePersonal Data: Curriculum VitaemeronNessuna valutazione finora
- Manual Testing Interview Question FreshersDocumento8 pagineManual Testing Interview Question Freshersbeghinbose0% (1)
- CPM - 100: Principles of Project ManagementDocumento75 pagineCPM - 100: Principles of Project ManagementDocuments ManNessuna valutazione finora
- Data Gathering Procedure - MaryAnnDoldolDocumento4 pagineData Gathering Procedure - MaryAnnDoldolmary ann doldolNessuna valutazione finora
- Mathematics 1 Oneside PDFDocumento106 pagineMathematics 1 Oneside PDFYuxdar ContellNessuna valutazione finora
- Thesis I Manual - 2021Documento26 pagineThesis I Manual - 2021Pragati KashyapNessuna valutazione finora
- HSC Chemistry 7.0 User's Guide: Mass Balancing and Data ReconciliationDocumento50 pagineHSC Chemistry 7.0 User's Guide: Mass Balancing and Data ReconciliationJoshua JohnsonNessuna valutazione finora
- Models and Methods For Evaluation: Ron OwstonDocumento14 pagineModels and Methods For Evaluation: Ron OwstonAMAAL ALORININessuna valutazione finora
- BEO1106 Business Statistics Assignment Part III AnswerSheetDocumento4 pagineBEO1106 Business Statistics Assignment Part III AnswerSheetXavier GohNessuna valutazione finora
- Od Proposal - SMLDocumento32 pagineOd Proposal - SMLSheila May LantoNessuna valutazione finora
- Pca IcaDocumento34 paginePca Icasachin121083Nessuna valutazione finora
- Abhishek Shukla Project Reporton (Power Purchase)Documento57 pagineAbhishek Shukla Project Reporton (Power Purchase)beast singhNessuna valutazione finora
- Chapter 04Documento44 pagineChapter 04hassan10012Nessuna valutazione finora
- AC1985658267Documento12 pagineAC1985658267Chuchu TayeNessuna valutazione finora
- Application of Infrared Thermography Technique in Uilding Finish EvaluationDocumento9 pagineApplication of Infrared Thermography Technique in Uilding Finish EvaluationNicolas De NadaiNessuna valutazione finora
- Effects of ISO 9001 On Efficiency of Firms A Conceptual FrameworkDocumento4 pagineEffects of ISO 9001 On Efficiency of Firms A Conceptual FrameworkInternational Journal of Innovative Science and Research Technology100% (1)
- TIVA Part I - Pharmacokinetic Principles and Methods of Delivery PDFDocumento56 pagineTIVA Part I - Pharmacokinetic Principles and Methods of Delivery PDFMaria José RecheNessuna valutazione finora
- Vacuuming and Dishwasher Task AnalysisDocumento4 pagineVacuuming and Dishwasher Task AnalysisElizabeth Curtin100% (1)
- Rafika 1601240742 Academic WritingDocumento4 pagineRafika 1601240742 Academic WritingRafika FairuzNessuna valutazione finora
- ChallengesAuditingJune2006 PDFDocumento16 pagineChallengesAuditingJune2006 PDFFachrurroziNessuna valutazione finora
- Pbi-Multi-Day-Planner Week 2 2 1Documento5 paginePbi-Multi-Day-Planner Week 2 2 1api-436249293Nessuna valutazione finora
- CD6 Prototype PFMEADocumento4 pagineCD6 Prototype PFMEAmpedraza-1Nessuna valutazione finora
- Time-Space Modeling of Journey-Time Exposure To Traffic-Related Air Pollution Using GISDocumento16 pagineTime-Space Modeling of Journey-Time Exposure To Traffic-Related Air Pollution Using GISNur Risa AprilyantiNessuna valutazione finora
- Malhotra 05Documento26 pagineMalhotra 05Abhishek JainNessuna valutazione finora
- SYNOPSIS-A Comparative Study of NPA of Urban Co-Op BanksDocumento7 pagineSYNOPSIS-A Comparative Study of NPA of Urban Co-Op BanksJitendra UdawantNessuna valutazione finora
- Dressmaking B Chapter1 4 DoneDocumento41 pagineDressmaking B Chapter1 4 Donemalupet nataeNessuna valutazione finora
- MBA 5004 - Assessment Guide-3Documento13 pagineMBA 5004 - Assessment Guide-3vzu53350Nessuna valutazione finora
- Ambuja ReportDocumento97 pagineAmbuja Reportpinkydholakia33% (3)