Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Clinical Impact of A Multiplex Gastrointestinal PCR Panel in Patients With Acute
Caricato da
Carlos Elías Mendoza LopezTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Clinical Impact of A Multiplex Gastrointestinal PCR Panel in Patients With Acute
Caricato da
Carlos Elías Mendoza LopezCopyright:
Formati disponibili
Clinical impact of a Multiplex Gastrointestinal PCR Panel in Patients with Acute
Gastroenteritis
Robert J. Cybulski Jr.*1, Allen C. Bateman*#1, Lori Bourassa1, Andrew Bryan1, Barb Beail1,
Jason Matsumoto2, Brad T. Cookson1,3 and Ferric C. Fang1,2,3,4
1. Department of Laboratory Medicine, University of Washington, Seattle, USA
2. Harborview Medical Center Clinical Microbiology Laboratory, Seattle, USA
3. Department of Microbiology, University of Washington, Seattle, USA
4. University of Washington School of Medicine, Seattle, USA
*These authors contributed equally to the work
#
Current address: Communicable Disease Division, Wisconsin State Laboratory of Hygiene,
Madison, USA
Corresponding author
Prof. Ferric C. Fang
University of Washington School of Medicine
1959 NE Pacific St., Box 357735
Seattle, Washington 98195-7735 USA
Tel: 206-221-6770
Fax: 206-616-1575
email: fcfang@uw.edu
© The Author(s) 2018. Published by Oxford University Press for the Infectious Diseases Society of
America. All rights reserved. For permissions, e-mail: journals.permissions@oup.com.
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
Summary of the article main points
A multiplex PCR panel facilitated the more rapid institution of appropriate antimicrobial therapy
in patients with acute gastroenteritis compared to traditional diagnostic methods.
Short Title
Clinical Impact of GI Multiplex PCR
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
Abstract
Background. Molecular syndromic diagnostic panels can enhance pathogen identification in the
approximately 2-4 billion episodes of acute gastroenteritis that occur annually worldwide.
However, the clinical utility of these panels has not been established.
Methods. We conducted a prospective, multi-center study to investigate the impact of the
BioFire FilmArray Gastrointestinal PCR panel on clinical diagnosis and decision-making and
compared the clinical acuity of patients with positive results obtained exclusively with the
FilmArray with those detected by conventional stool culture. A total of 1,887 consecutive fecal
specimens were tested in parallel by FilmArray and stool culture. Laboratory and medical
records were reviewed to determine rates of detection, turnaround times, clinical features and the
nature and timing of clinical decisions.
Results. FilmArray detected pathogens in 35.3% of specimens, compared to 6.0% for culture.
Median time from collection to result was 18h for FilmArray and 47h for culture. Median time
from collection to initiation of antimicrobial therapy was 22h for FilmArray and 72h for
culture. Patients diagnosed by FilmArray were more likely to receive targeted rather than
empirical therapy, compared to those diagnosed by culture (p=0.0148). Positive STEC results
were reported 47h faster with FilmArray and facilitated discontinuation of empirical
antimicrobials. Patients diagnosed exclusively by FilmArray had clinical characteristics similar
to those identified by culture.
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
Conclusions. FilmArray markedly improved clinical sensitivity in patients with acute diarrhea,
identified cases with clinical acuity comparable to those identified by culture, and enabled
clinicians to make more timely and targeted therapeutic decisions.
Keywords: acute gastroenteritis; multiplex PCR panel; syndromic testing; culture-
independent diagnostic test
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
BACKGROUND
Accurate and timely diagnosis of acute gastroenteritis is an unmet clinical and public health need
[1, 2], as diarrhea remains a leading cause of morbidity and mortality worldwide [3, 4].
Approximately 80% of acute gastroenteritis cases are presently unattributed [4], partly due to
insensitive and pathogen-specific diagnostic tests [1, 5, 6]. Multiplex nucleic acid amplification
testing provides rapid turnaround time and allow clinicians to test on the basis of clinical
syndromes [7-9], recognizing the overlapping clinical presentations of various gastrointestinal
infections [10]. Many pathogens identified by multiplex panels respond to antimicrobial therapy
[11-20], offering potential benefit from timely results that enable targeted therapy and the
detection of Shiga-like toxin producing E. coli (STEC) for which antibiotics are contraindicated
[21, 22]. Multiplex testing improves laboratory workflow [23] and can enhance infection control
by increasing outbreak detection [24] and guiding contact precaution decisions [25].
Questions remain regarding the costs and benefits of multiplex panels. Increasing reliance upon
molecular assays may increase public health awareness of disease incidence, but fewer cultured
isolates may be available for outbreak investigations [26, 27]. Benefits realized from multiplex
syndromic testing may vary among patient populations [28-31]. It is also debated whether
additional cases of infectious gastroenteritis diagnosed by multiplex PCR warrant antimicrobial
treatment, and the clinical impact of multiplex panels is uncertain in the absence of coordinated
stewardship efforts [32, 33].
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
We undertook a nine-month, prospective, multi-center study with parallel testing of stool
specimens by the BioFire FilmArray Gastrointestinal PCR panel and conventional methods.
The objectives were to determine whether the additional patients detected by multiplex PCR
have comparable clinical features to those diagnosed with conventional methods and to measure
the impact of more rapid diagnosis on clinical decision-making and therapy.
METHODS
Study design, Population and Procedures
Parallel testing of stool specimens by FilmArray and conventional methods was performed
from Jan 1 to Sept 30, 2017. A historical control group comprised of patients with positive stool
cultures tested at the same laboratories from Jan 1 to Sept 30, 2016 was also analyzed. Eligible
subjects included newly-admitted (<3d) inpatients and outpatients from 17 outpatient clinics in
the greater Seattle, Washington metropolitan area served by the clinical laboratories of the
University of Washington and Harborview Medical Centers, ranging in age from 0 to 91 years.
Samples positive by FilmArray for C. difficile only were not included in the study due to the
preexisting availability of a standalone molecular assay for C. difficile (GeneXpert, Sunnyside,
CA); however, all C. difficile results were reported to clinicians.
Immediately prior to the study period, conventional stool culture was replaced as an orderable
test by the FilmArray panel. Clinicians were informed of the change in testing methodology by
in-person presentations and an institution-wide memorandum from the Medical Directors.
Specimens were submitted in Cary-Blair transport medium or as fresh stool transferred into
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
Cary-Blair medium within 2h and tested by FilmArray on receipt. Specimens received from
11pm-7am were tested the following morning and results released as soon as available. For study
purposes, cultures continued to be performed in parallel. Stool was plated onto agar media
(Remel Inc, Hardy Diagnostics) including Blood, MacConkey, MacConkey-Sorbitol,
Salmonella-Shigella Selective, Cefsulodin-Irgasan-Novobiocin and Campylobacter Selective
agars. As Aeromonas spp. are not detected by the FilmArray panel, Aeromonas isolated in
culture was reported separately. Thiosulfate-Citrate-Bile Salt-Sucrose agar for enhanced
recovery of Vibrio spp. was added from Jun-Sep. Selenite broth enrichment for 24h prior to
plating onto Salmonella-Shigella Selective agar was performed at the University of Washington
but not Harborview Medical Center. Campylobacter Selective agar was incubated under
microaerophilic conditions at 42C for 3d, whereas other plates were incubated at 37C in
ambient air for 2d. Inoculation into Gram-negative broth (Hardy Diagnostics) for 16-24h
enrichment was conducted prior to performing the Immunocard STAT! EHEC Shiga toxin
immunoassay (Meridian Biosciences, Inc.). Additional conventional tests included ova and
parasite examination, Cryptosporidium/Cyclospora testing by modified acid-fast smear, Giardia
ProSpecT stool antigen testing (Remel Inc), and a laboratory-developed viral gastroenteritis
multiplex PCR panel. Clinicians were not prevented from ordering these tests when FilmArray
was ordered. Results were reported in the laboratory information system with the exception of
STEC results, which were called to clinicians per laboratory protocol.
Chart Review and Data Analysis
Record numbers were obtained from the laboratory information system (LIS) for patients testing
positive by culture from Jan-Sept 2016 or by any method from Jan-Sept 2017 for chart review.
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
For the 2017 cohort, 14 patients lacking documentation of clinical findings were excluded,
although their test results were included in the analysis of clinical sensitivity and time-to-
diagnosis.
Electronic chart review was performed by 4 doctoral-level clinical microbiologists and overseen
by the corresponding author, who is a physician and ID specialist. Ten charts were reviewed by
all 4 reviewers for initial training and standardization, with charts subsequently reviewed by
individual reviewers. Collected information included clinical signs and symptoms of
gastroenteritis (fever, nausea, vomiting, diarrhea, abdominal pain, tenesmus, hematochezia,
duration of symptoms, mucus, nature of stool, elevated WBC) and antimicrobial treatment. Time
of sample collection, arrival in the laboratory, and result reporting were obtained from the LIS.
Antibiotics were estimated to be prescribed at 5pm on the day on which they were ordered.
Empirical antimicrobial therapy was defined as therapy initiated prior to the release of results.
Targeted therapy was defined on the basis of documentation that the primary clinician received a
result and then prescribed an agent with predicted activity against the microbe detected.
Statistical Analysis
Clinical sensitivity was defined as the ability to detect a pathogen when the pathogen is present
in a clinical specimen, as determined by a composite gold standard combining the results of
conventional and molecular assays. To compare the clinical variables of distinct patient
populations, t-tests, Mann-Whitney tests, or Fisher's exact tests were performed, as appropriate.
Linear regression was performed to compare trends in targeted versus empirical initiation of
antimicrobial therapy. A p-value <0.05 was considered significant. Adjustments for multiple
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
comparisons used a post-hoc Bonferroni's correction method. GraphPad Prism Version 7.0a for
Mac OS X was used for statistical analyses.
Ethics Statement
Regulatory approval was provided by the University of Washington’s Institutional Review Board
(IRB #52540).
RESULTS
FilmArray GI Panel Performance
A total of 1,887 patient specimens were tested in parallel by FilmArray and conventional stool
culture between Jan 1 and Sept 30, 2017 (Figure 1, Supplemental Table 1). FilmArray
detected one or more pathogen in 669 (35.3%) specimens, compared to 113 (6.0%) detected by
culture. For conventionally cultured bacterial pathogens, 155 (8.2%) were positive by
FilmArray, representing a 37% increase compared to culture (p=0.0078). FilmArray detected
significantly more STEC (p=0.0002), Plesiomonas shigelloides (p=0.0142) and Yersinia
enterocolitica (p=0.0414) than culture. Conventionally cultured pathogens most frequently
detected by FilmArray in the absence of culture positivity were Campylobacter spp. (n=68, 18
additional), Shigella/Enteroinvasive E. coli (EIEC) (n=43, 15 additional), and STEC (n=21, 18
additional). FilmArray cannot distinguish Shigella and EIEC, and EIEC is not cultivable by
standard clinical microbiology culture techniques. The most common FilmArray targets not
identifiable by culture were C. difficile (n=234, 25.5% of specimens tested), Enteropathogenic E.
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
coli (n=154, 8.2%), and Enteroaggregative E. coli (n=112, 5.9%). Pediatric patients (ages 0-17y)
represented 5.5% of the total tested population with a positivity rate (33.7%) not significantly
different from the overall population and comparable pathogen-specific detection rates aside
from a higher (p=0.0001) rate of rotavirus detection (n=6, 5.31% of total tested). Comparison of
culture results from 2016 and 2017 indicated similar detection rates (Supplemental Table 2).
Fourteen specimens negative by FilmArray had positive cultures. Twelve of these were
organisms not on the FilmArray panel (8 Aeromonas spp., 3 Campylobacter hyointestinalis and
1 Helicobacter pullorum). Salmonella enterica (non-Typhi) and Campylobacter jejuni were each
recovered from a single culture when the FilmArray was negative. The Salmonella isolate was a
single colony, indicating a low organism burden. The Campylobacter isolate was part of a mixed
infection in which Giardia and Norovirus were detected by FilmArray, and 1+ Campylobacter
grew in culture. FilmArray reportedly fails to detect Campylobacter jejuni ssp. doylei [9] and
possibly some strains of C. coli [34].
Clinicians’ simultaneous ordering of FilmArray and tests such as O&P examination, modified
acid-fast smear, Giardia antigen testing, and a laboratory-developed viral multiplex PCR panel
enabled a limited comparison (Figure 2). FilmArray led to increased detection of Entamoeba
histolytica and Giardia lamblia (n=23, 1.4% of specimens tested) when compared to O&P
examination of the same specimen (n=6, 0.3%). FilmArray also detected viral or parasitic
pathogens in 137 cases in which additional diagnostic tests were not ordered.
10
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
FilmArray increased detection of coinfections (Supplemental Figure 1). Multiple positive
targets were detected in 184 stool specimens (27.5% of all positive specimens, 9.8% overall).
Thirty-eight involved only cultivable pathogens; 4 of 38 of these coinfections were detected by
culture. The remaining 115 coinfections included FilmArray targets unrecoverable by culture,
with conventional testing methods detected in 4 of 115.
Turnaround Time and Impact on Clinical Decision-Making
FilmArray testing in Jan-Sept 2017 had a median turnaround time (collection to first report) of
18h, which was significantly (p<0.0001) shorter than the 47h median turnaround time for culture
in Jan-Sept 2016 (Table 1) or conventional testing methods performed in parallel
(Supplemental Table 3). The estimated median time from collection to antibiotic initiation was
26h in 2017 compared to 72h in 2016 (p < 0.0001). In 2017, 64 of 272 (23.5%) antimicrobial
prescriptions were initiated empirically at the time of encounter. This proportion is lower
(p=0.0148) than the 20 of 50 (40.0%) cases of empirical therapy in 2016 (Figure 3). The use of
FilmArray resulted in a significant (r2 = 0.65, p = 0.009 by linear regression) trend toward
targeted rather than empirical therapy over the course of the study period (Figure 4).
FilmArray identified 21 STEC infections, with 4 identified as E. coli O157:H7. Stool culture
and Shiga-like toxin immunoassay identified 3 STEC/O157:H7 infections. The median
turnaround-time for all FilmArray results was 18h, making the assay significantly faster than
stool culture and immunoassay for reporting positive (60.0h, p = 0.0006) and negative (75.0h,
p<0.0001) results. Nine of 21 patients with STEC-positive results were empirically prescribed
antimicrobials, with discontinuation of empirical therapy occurring in 8 of 9 cases after STEC
11
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
was reported. The median time from the release of results to clinician-directed discontinuation of
therapy was 8h (range 0.5–25h).
Clinical Features of Patients
Clinical features of 2017 patients detected by FilmArray or culture are presented in Table 2.
Those with discordant results (FilmArray-positive/culture-negative) reported a longer duration
of symptoms at the time of presentation than those with concordant results (FilmArray-
positive/culture-positive). Otherwise, patients exhibited similar clinical features. The 2017
patients with conventionally cultured pathogens detected by FilmArray (concordant and
discordant combined) were compared with uncultivable pathogens detected exclusively by
FilmArray (Table 3). Patients with conventionally cultured pathogens presented more
frequently with chills and received antibiotics at a higher rate. The aggregate population of
patients infected with conventional pathogens Campylobacter, Salmonella and/or Shigella was
compared to those infected with the diarrheagenic E. coli species EPEC, EAEC and ETEC that
were not recoverable by culture (Supplemental Table 4). Patients with Campylobacter,
Salmonella and/or Shigella were more likely to report chills, have measurable fever and receive
antibiotic therapy. Patients with diarrheagenic E. coli infections reported a longer duration of
symptoms at presentation. As expected, 2016 and 2017 culture-positive patients showed no
significant differences (Supplemental Table 5).
The clinical features of pediatric patients (ages 0-17y) were not significantly different from those
of adults (Supplemental Table 6). Patients with mixed infections had a higher rate of
international travel within 30d than those testing positive for a single pathogen (Supplemental
12
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
Table 7). Finally, organism-specific comparisons were performed to assess the clinical features
of patients infected with Campylobacter spp., Salmonella spp. or Shigella/EIEC with concordant
or discordant results (Supplemental Table 8). For Campylobacter spp., concordant cases
followed general trends observed for the entire concordant population, with a slight non-
significant trend toward greater symptom severity. Shigella patients with concordant results were
more likely to be male and had a shorter duration of symptoms at presentation. No significant
differences were observed in patients with Salmonella.
DISCUSSION
Multiplex syndromic panels are more sensitive than conventional methods, although questions
remain regarding clinical utility and cost-effectiveness [7, 28-31]. To address these concerns, we
undertook a nine-month prospective multi-center study involving parallel testing of stool
specimens by the BioFire FilmArray GI Panel and conventional diagnostics. Consistent with
previous reports [8, 9, 35-37], FilmArray demonstrated greater clinical sensitivity than stool
culture (Figure 1, Supplemental Table 1), identifying over three times as many pathogens as
conventional assays, including 41% more among targets common to both methods (Figure 2).
The majority of FilmArray targets not identifiable by conventional culture were diarrheagenic
E. coli (STEC, EPEC, EAEC and ETEC), long recognized as important causes of acute
gastroenteritis [9, 38].
FilmArray provided more rapid turnaround time compared to alternative conventional methods
(Table 1 and Supplemental Table 3). Patients with an infectious cause of acute gastroenteritis
detected by FilmArray were more likely (p=0.0148) to receive targeted rather than empirical
13
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
therapy when compared to those detected by culture (Figure 3), suggesting that the reduced
turnaround time of FilmArray encouraged more targeted antimicrobial therapy. This effect on
prescribing decisions became more pronounced over the course of the study (Figure 4), further
suggesting that clinicians adjusted their practice as they became accustomed to the availability of
rapid results. Diagnostics-directed therapy is a central goal of diagnostic stewardship and
contrasts with earlier studies in which multiplex syndromic panels only impacted clinical
practice in the context of a coordinated stewardship effort [32, 33]. Reduced time-to-treatment
and an impact on antibiotic prescribing were also specifically observed in STEC infections.
Negative results allowed initiation of antimicrobial therapy without concern for the induction of
hemolytic-uremic syndrome [21, 22]. Positive STEC results led to the discontinuation of
antimicrobials in 8 of 9 cases when therapy had been initiated empirically, with a median time-
to-discontinuation of 8h following reporting of results, further demonstrating that FilmArray
results affected clinical decision-making.
Patients infected with conventionally cultured pathogens identified by both FilmArray and stool
culture (concordant) tended to have greater symptom severity than those positive for those same
organisms by FilmArray only (discordant), although these trends were not significant with the
exception of a longer duration of symptoms among discordant patients (Table 2). These
observations are consistent with the higher organism burden required for culture positivity and
the relationship between organism burden and disease severity. However, neither antimicrobial
prescription rates nor duration of therapy differed significantly between these groups, suggesting
that clinicians placed equal significance on culture and molecular results.
14
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
Patients diagnosed with pathogens detectable only by FilmArray exhibited similar clinical
characteristics to those diagnosed with conventionally cultured pathogens (concordant plus
discordant) (Table 3). More than 60% of these patients received antimicrobial therapy when
diagnosed with bacterial and/or parasite pathogens, suggesting that these diagnoses were viewed
by clinicians as clinically relevant. A specific subset comparison was performed between those
patients diagnosed with pathogens considered to be prominent causes of acute bacterial
gastroenteritis (Campylobacter, Salmonella and Shigella) and those diagnosed with a
diarrheagenic E. coli species (EPEC, EAEC and/or ETEC) (Supplemental Table 4). The results
indicate that conventionally cultured pathogens may be more highly associated with certain signs
of inflammation, but the diarrheagenic E. coli pathogens should not be neglected due to their
potential to cause protracted illness. Together, these comparisons show that the additional cases
identified by FilmArray are clinically comparable to those identified by stool culture. Along
with the potential for rapid testing to encourage targeted rather than empirical therapy (Figure
4), these observations argue against the selective reporting of FilmArray results, which could
lead to both the overtreatment of patients lacking identifiable pathogens and the undertreatment
of patients with unreported treatable pathogens such as diarrheagenic E. coli.
For Campylobacter spp., concordant patients were slightly but not significantly more
symptomatic than discordant patients (Supplemental Table 8). Concordant Shigella cases also
exhibited a non-significant trend toward increased severity, more recent symptom onset and an
association with male gender. An ongoing outbreak of Shigella infections among MSM in
several metropolitan areas including Seattle underscores the utility of highly sensitive molecular
assays for case detection and outbreak investigation [24]. For Salmonella infections, concordant
15
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
patients tended to exhibit symptoms of gastroenteritis and present in an outpatient setting,
whereas discordant patients were more likely to require hospitalization.
FilmArray allowed increased recognition of coinfections. The ability of FilmArray to detect
coinfections has been noted previously [35], but there is uncertainty regarding the clinical
interpretation and relevance of these cases. Detection of multiple potential pathogens may
influence case management [39] and is not unusual in returning travelers who may have been
exposed to contaminated food or water [40]. Patients with coinfections were generally younger
and evenly gender-distributed, and more likely to have recent international travel (Supplemental
Table 7). We also observed mixed infection scenarios among MSM patients with Shigella. In
contrast to earlier studies in children [41], we did not observe greater severity of illness in
patients with coinfections. The detection of mixed bacterial and/or parasitic infections generally
led to initiation of appropriate combination therapy (not shown).
A unique strength of the present study is the prospective parallel testing of a large patient cohort
by both multiplex PCR and culture in real-time, accompanied by a comprehensive review of
their clinical characteristics. Limitations of the study include the insufficient size of certain
subgroups to draw definitive conclusions regarding small observed differences. Also,
retrospective review of medical records is subject to confounding factors and biases. The study
was limited to two hospitals within a single healthcare system, although the academic medical
center, the county hospital and the 17 community clinics they support collectively represent a
broad and representative metropolitan demographic that includes both healthy immunocompetent
individuals and patients with various forms of immunocompromise and chronic illness.
16
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
In summary, a nine-month, prospective, multi-center study found that the BioFire FilmArray
gastrointestinal panel markedly improves the sensitivity of laboratory diagnosis in patients with
acute diarrhea and allows clinicians to make more timely and targeted therapeutic decisions. The
additional cases detected by FilmArray are comparable in clinical presentation and acuity to
those diagnosed by conventional culture, indicating that the syndromic panel identifies clinically
relevant infections. Previously identified by clinicians as an unmet need in infectious disease
diagnostics [1, 3], syndromic testing represents a significant advance in the laboratory diagnosis
of patients with acute gastroenteritis [42].
17
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
NOTES
Acknowledgments. The authors thank Tom Smith, Sarah Jensen and Brett Norquist for their
assistance with the execution of this study.
Financial support. Test kits and instruments were provided by BioFire Diagnostics, a
bioMérieux Company.
Conflicts of Interest: Dr. Fang reports grants, personal fees and non-financial support from
BioFire, during the conduct of the study; grants, personal fees and non-financial support from
Cepheid, grants and non-financial support from ELITech, non-financial support from Luminex,
personal fees from IDSA, outside the submitted work.
18
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
REFERENCES
1. Hennessy TW, Marcus R, Deneen V, et al. Survey of physician diagnostic practices for patients
with acute diarrhea: clinical and public health implications. Clin Infect Dis 2004; 38 Suppl 3:
S203-11.
2. Blaschke AJ, Hersh AL, Beekmann SE, Ince D, Polgreen PM, Hanson KE. Unmet diagnostic
needs in infectious disease. Diagn Microbiol Infect Dis 2015; 81(1): 57-9.
3. Kosek M, Bern C, Guerrant RL. The global burden of diarrhoeal disease, as estimated from
studies published between 1992 and 2000. Bull World Health Organ 2003; 81(3): 197-204.
4. Scallan E, Griffin PM, Angulo FJ, Tauxe RV, Hoekstra RM. Foodborne illness acquired in the
United States--unspecified agents. Emerg Infect Dis 2011; 17(1): 16-22.
5. Stockmann C, Rogatcheva M, Harrel B, et al. How well does physician selection of microbiologic
tests identify Clostridium difficile and other pathogens in paediatric diarrhoea? Insights using
multiplex PCR-based detection. Clin Microbiol Infect 2015; 21(2): 179 e9-15.
6. Bruijnesteijn van Coppenraet LE, Dullaert-de Boer M, Ruijs GJ, et al. Case-control comparison
of bacterial and protozoan microorganisms associated with gastroenteritis: application of
molecular detection. Clin Microbiol Infect 2015; 21(6): 592 e9-19.
7. McAuliffe GN, Anderson TP, Stevens M, et al. Systematic application of multiplex PCR
enhances the detection of bacteria, parasites, and viruses in stool samples. J Infect 2013; 67(2):
122-9.
8. Khare R, Espy MJ, Cebelinski E, et al. Comparative evaluation of two commercial multiplex
panels for detection of gastrointestinal pathogens by use of clinical stool specimens. J Clin
Microbiol 2014; 52(10): 3667-73.
9. Buss SN, Leber A, Chapin K, et al. Multicenter evaluation of the BioFire FilmArray
gastrointestinal panel for etiologic diagnosis of infectious gastroenteritis. J Clin Microbiol 2015;
53(3): 915-25.
10. Mattila L. Clinical features and duration of traveler's diarrhea in relation to its etiology. Clin
Infect Dis 1994; 19(4): 728-34.
11. Thoren A, Wolde-Mariam T, Stintzing G, Wadstrom T, Habte D. Antibiotics in the treatment of
gastroenteritis caused by enteropathogenic Escherichia coli. J Infect Dis 1980; 141(1): 27-31.
12. Butler T, Lolekha S, Rasidi C, et al. Treatment of acute bacterial diarrhea: a multicenter
international trial comparing placebo with fleroxacin given as a single dose or once daily for 3
days. Am J Med 1993; 94(3A): 187S-94S.
13. Mattila L, Peltola H, Siitonen A, Kyronseppa H, Simula I, Kataja M. Short-term treatment of
traveler's diarrhea with norfloxacin: a double-blind, placebo-controlled study during two seasons.
Clin Infect Dis 1993; 17(4): 779-82.
14. Hoge CW, Shlim DR, Ghimire M, et al. Placebo-controlled trial of co-trimoxazole for
Cyclospora infections among travellers and foreign residents in Nepal. Lancet 1995; 345(8951):
691-3.
15. Glandt M, Adachi JA, Mathewson JJ, et al. Enteroaggregative Escherichia coli as a cause of
traveler's diarrhea: clinical response to ciprofloxacin. Clin Infect Dis 1999; 29(2): 335-8.
16. Rossignol JF, Ayoub A, Ayers MS. Treatment of diarrhea caused by Giardia intestinalis and
Entamoeba histolytica or E. dispar: a randomized, double-blind, placebo-controlled study of
nitazoxanide. J Infect Dis 2001; 184(3): 381-4.
17. Rossignol JF, Ayoub A, Ayers MS. Treatment of diarrhea caused by Cryptosporidium parvum: a
prospective randomized, double-blind, placebo-controlled study of Nitazoxanide. J Infect Dis
2001; 184(1): 103-6.
18. Zheng H, Sun Y, Lin S, Mao Z, Jiang B. Yersinia enterocolitica infection in diarrheal patients.
Eur J Clin Microbiol Infect Dis 2008; 27(8): 741-52.
19. Nelson RL, Kelsey P, Leeman H, et al. Antibiotic treatment for Clostridium difficile-associated
diarrhea in adults. Cochrane Database Syst Rev 2011; (9): CD004610.
19
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
20. DuPont HL. Persistent Diarrhea: A Clinical Review. JAMA 2016; 315(24): 2712-23.
21. Wong CS, Jelacic S, Habeeb RL, Watkins SL, Tarr PI. The risk of the hemolytic-uremic
syndrome after antibiotic treatment of Escherichia coli O157:H7 infections. N Engl J Med 2000;
342(26): 1930-6.
22. Freedman SB, Xie J, Neufeld MS, et al. Shiga Toxin-Producing Escherichia coli Infection,
Antibiotics, and Risk of Developing Hemolytic Uremic Syndrome: A Meta-analysis. Clin Infect
Dis 2016; 62(10): 1251-8.
23. Halligan E, Edgeworth J, Bisnauthsing K, et al. Multiplex molecular testing for management of
infectious gastroenteritis in a hospital setting: a comparative diagnostic and clinical utility study.
Clin Microbiol Infect 2014; 20(8): O460-7.
24. Prakash VP, LeBlanc L, Alexander-Scott NE, et al. Use of a culture-independent gastrointestinal
multiplex PCR panel during a Shigellosis outbreak: considerations for clinical laboratories and
public health. J Clin Microbiol 2015; 53(3): 1048-9.
25. Rand KH, Tremblay EE, Hoidal M, Fisher LB, Grau KR, Karst SM. Multiplex gastrointestinal
pathogen panels: implications for infection control. Diagn Microbiol Infect Dis 2015; 82(2): 154-
7.
26. Shea S, Kubota KA, Maguire H, et al. Clinical Microbiology Laboratories' Adoption of Culture-
Independent Diagnostic Tests Is a Threat to Foodborne-Disease Surveillance in the United States.
J Clin Microbiol 2017; 55(1): 10-9.
27. Imdad A, Retzer F, Thomas LS, et al. Impact of Culture-Independent Diagnostic Testing on
Recovery of Enteric Bacterial Infections. Clin Infect Dis 2017.
28. Goldenberg SD, Bacelar M, Brazier P, Bisnauthsing K, Edgeworth JD. A cost benefit analysis of
the Luminex xTAG Gastrointestinal Pathogen Panel for detection of infectious gastroenteritis in
hospitalised patients. J Infect 2015; 70(5): 504-11.
29. McMillen T, Lee YJ, Kamboj M, Babady NE. Limited diagnostic value of a multiplexed
gastrointestinal pathogen panel for the detection of adenovirus infection in an oncology patient
population. J Clin Virol 2017; 94: 37-41.
30. Beal SG, Tremblay EE, Toffel S, Velez L, Rand KH. A Gastrointestinal PCR Panel Improves
Clinical Management and Lowers Health Care Costs. J Clin Microbiol 2018; 56(1).
31. Hitchcock MM, Gomez CA, Banaei N. Low Yield of FilmArray GI Panel in Hospitalized
Patients with Diarrhea: An Opportunity for Diagnostic Stewardship Intervention. J Clin Microbiol
2017.
32. Timbrook TT, Morton JB, McConeghy KW, Caffrey AR, Mylonakis E, LaPlante KL. The Effect
of Molecular Rapid Diagnostic Testing on Clinical Outcomes in Bloodstream Infections: A
Systematic Review and Meta-analysis. Clin Infect Dis 2017; 64(1): 15-23.
33. Banerjee R, Teng CB, Cunningham SA, et al. Randomized Trial of Rapid Multiplex Polymerase
Chain Reaction-Based Blood Culture Identification and Susceptibility Testing. Clin Infect Dis
2015; 61(7): 1071-80.
34. 510(k) Summary For FilmArray Gastrointestinal (GI) Panel Kit. Available at:
https://www.accessdata.fda.gov/cdrh_docs/pdf14/K140407.pdf.
35. Spina A, Kerr KG, Cormican M, et al. Spectrum of enteropathogens detected by the FilmArray
GI Panel in a multicentre study of community-acquired gastroenteritis. Clin Microbiol Infect
2015; 21(8): 719-28.
36. Piralla A, Lunghi G, Ardissino G, et al. FilmArray GI panel performance for the diagnosis of
acute gastroenteritis or hemorragic diarrhea. BMC Microbiol 2017; 17(1): 111.
37. Murphy CN, Fowler RC, Iwen PC, Fey PD. Evaluation of the BioFire FilmArray(R)
GastrointestinalPanel in a Midwestern Academic Hospital. Eur J Clin Microbiol Infect Dis 2017;
36(4): 747-54.
38. Chao AW, Bhatti M, DuPont HL, Nataro JP, Carlin LG, Okhuysen PC. Clinical features and
molecular epidemiology of diarrheagenic Escherichia coli pathotypes identified by fecal
20
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
gastrointestinal multiplex nucleic acid amplification in patients with cancer and diarrhea. Diagn
Microbiol Infect Dis 2017; 89(3): 235-40.
39. Pawlowski SW, Warren CA, Guerrant R. Diagnosis and treatment of acute or persistent diarrhea.
Gastroenterology 2009; 136(6): 1874-86.
40. Antikainen J, Kantele A, Pakkanen SH, et al. A quantitative polymerase chain reaction assay for
rapid detection of 9 pathogens directly from stools of travelers with diarrhea. Clin Gastroenterol
Hepatol 2013; 11(10): 1300-7 e3.
41. Valentini D, Vittucci AC, Grandin A, et al. Coinfection in acute gastroenteritis predicts a more
severe clinical course in children. Eur J Clin Microbiol Infect Dis 2013; 32(7): 909-15.
42. Fang FC, Patel R. 2017 Infectious Diseases Society of America Infectious Diarrhea Guidelines: A
View From the Clinical Laboratory. Clin Infect Dis 2017; 65(12): 1974-6.
21
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
FIGURE LEGENDS
FIGURE 1. Improved clinical sensitivity and range of pathogens detected by FilmArray
compared to traditional stool culture. Classic enteric bacterial pathogens detected by
conventional stool culture (A) depicted as a subset of the total detection of enteric pathogens by
FilmArray (B).
FIGURE 2. Improved clinical sensitivity of FilmArray compared to conventional stool
testing methods. Results displayed are the aggregate total (n) for all pathogens detected by a
particular conventional method, compared with the number of same organisms detected by
FilmArray.
FIGURE 3. Rapid and targeted antimicrobial therapy after FilmArray implementation.
Results for stool culture in 2016 (A) and FilmArray in 2017 (B) summarize the time-to-result
(hours) and the physician’s decision to treat empirically or based upon testing results (targeted).
Figure 4. Increase in targeted rather than empirical therapy over time after FilmArray
implementation. Results displayed indicate the total number (n) of cases where antimicrobials
were prescribed based upon test results (targeted) versus prescribed prior to having test results
(empirical), measured on a monthly basis following implementation of the FilmArray.
22
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
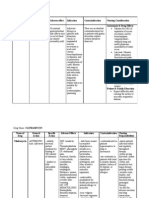
TABLE 1. Comparison of FilmArray and Stool Culture Turnaround Times and Impact
on Clinical Decisions
2016 Culture 2017 FilmArray p
Cases Reviewed, n 83 496 n/a
Median Time Collection to First
47.0 18.0 <0.0001
Report (h)
Patients with bacteria/parasite
83 420 n/a
identified, n
Eligible patients prescribed
50 (60.3) 272 (63.8) ns
antimicrobials, n (%)
Empirical antimicrobial
20 (40.0) 64 (23.5) 0.0148
prescription, n (%)
Median Time Collection to
72.0 26.0 <0.0001
Antimicrobial (h)
Note. Categorical values analyzed for statistical significance by Chi squared test. Comparison of
medians performed with Mann-Whitney test.
Abbreviations. n/a; not applicable; n.s., not significant
23
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
TABLE 2. Clinical Features of Patients Diagnosed with Classic Enteric Bacterial Pathogens
by FilmArray
Concordant Discordant
p
Results Results
Patients, n 98 68
Age, years
Mean (range) 40.3 (1-91) 39.6 (1-82) n.s.
Median (range) 34.0 (1-91) 36.0 (1-82) n.s.
Percent Female 35.60% 53.60% n.s.
Ordering location, n (%)
Outpatient 80 (79) 55 (80%) n.s.
ED 17 (17) 9 (13%)
Inpatient 4 (4) 5 (7%)
Mean # of symptoms per patient (range) 3.8 (0-8) 3.4 (0-8) n.s.
Patients with Headache, n (%) 9 (9) 5 (7) n.s.
Patients with Abdominal pain, n (%) 73 (75) 49 (72) n.s.
Patients with Tenesmus, n (%) 2 (2) 1 (2) n.s.
Patients with Nausea, n (%) 42 (43) 30 (44) n.s.
Patients with Vomiting, n (%) 19 (19) 14 (21) n.s.
Patients with Diarrhea, n (%) 96 (98) 62 (91) n.s.
Patients with Watery Diarrhea, n (%) 53 (54) 36 (53) n.s.
Patients with Blood in Stool, n (%) 22 (22) 8 (12) n.s.
Patients with Chills, n (%) 28 (29) 14 (21) n.s.
Patients with Fatigue, n (%) 27 (28) 13 (19) n.s.
Patients with Fever, n (%) 17/97 (18) 10/65 (15) n.s.
Patients with Leukocytosis, n (%) 20/48 (42) 5/30 (17) n.s.
Patients with Fecal Leukocytes, n (%) 5/12 (42) 1/9 (11) n.s.
Median duration of symptoms at presentation, days (range) 7 (1-90) 8.5 (1-240) <0.0001
Patients with international travel history, n (%) 33 (34) 31 (46) n.s.
Patients with bacteria/parasite receiving antibiotic, n (%) 79 (81) 47 (68) n.s.
Patients receiving empirical antibiotic therapy, n (%) 27 (34) 10 (21) n.s.
Median duration of antibiotics, days (range) 4.5 (1-10) 5 (1-28) n.s.
Patients hospitalized, n (%) 12 (12) 8 (12) n.s.
Cases with apparent resolution of symptoms, n (%) 88 (90) 62 (91) n.s.
Note. Categorical values analyzed for statistical significance by Chi squared test. Comparison of
means performed by t test. Comparison of medians performed with Mann-Whitney test.
Adjustment for multiple comparisons made through Bonferroni’s method.
Abbreviations. n.s., not significant
24
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
TABLE 3. Comparison of Clinical Features for Patients Diagnosed by FilmArray for
Cultivable and Non-Cultivable Enteric Pathogens
Conventionally FilmArray™
Cultured Exclusive p
Pathogens Pathogens
Patients, n 166 305
Age (years)
mean 40.0 (1-91) 40.7 (0-87) n.s.
median 36.0 (1-91) 39.5 (0-87) n.s.
Percent female 41.8% 44.6% n.s.
Ordering location, n (%)
Outpatient 135 (82) 263 (83) n.s.
ED 26 (16) 37 (12)
Inpatient 9 (2) 16 (5)
Mean number of symptoms per patient (range) 3.6 (0-8) 3.2 (0-8) n.s.
Patients with Headache, n (%) 14 (8) 16 (5) n.s.
Patients with Abdominal pain, n (%) 122 (73) 208 (68) n.s.
Patients with Tenesmus, n (%) 3 (2) 7 (2) n.s.
Patients with Nausea, n (%) 72 (43) 117 (38) n.s.
Patients with Vomiting, n (%) 33 (20) 63 (21) n.s.
Patients with Diarrhea, n (%) 158 (95) 282 (93) n.s.
Patients with Watery Diarrhea, n (%) 89 (54) 144 (47) n.s.
Patients with Blood in Stool, n (%) 30 (18) 35 (12) n.s.
Patients with Chills, n (%) 42 (25) 35 (12) 0.0001
Patients with Fatigue, n (%) 40 (24) 62 (20) n.s.
Patients with Fever, n (%) 27/162 (17) 25/292 (9) n.s.
Patients with Leukocytosis, n (%) 25/78 (32) 27/144 (19) n.s.
Patients with Fecal Leukocytes, n (%) 6/21 (29) 11/30 (37) n.s.
Median duration of symptoms at presentation, days (range) 7 (1-240) 7 (1-365) n.s.
Patients with international travel history, n (%) 64 (39) 119 (39) n.s.
Patients with bacteria/parasite receiving antibiotic, n (%) 126/166 (76) 145/240 (60) 0.0011
Patients receiving empirical antibiotic therapy, n (%) 37 (22) 38 (19) n.s.
Median duration of antibiotics, days (range) 5 (1-28) 5 (1-28) n.s.
Patients hospitalized, n (%) 20 (12) 47 (15) n.s.
Cases with apparent resolution of symptoms, n (%) 150 (90) 253 (83) n.s.
Note. Categorical values analyzed for statistical significance by Chi squared test. Comparison of
means performed by t test. Comparison of medians performed with Mann-Whitney test.
Adjustment for multiple comparisons made through Bonferroni’s method.
Abbreviations. n.s., not significant
25
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
Figure 1.
26
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
Figure 2.
27
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
Figure 3.
28
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
Figure 4.
29
Downloaded from https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciy357/4985150
by Kaohsiung Medical University Library user
on 26 April 2018
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Drug StudyDocumento3 pagineDrug StudyJohn AlcantaraNessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Bases Da Fisiopatologia Da Diarreia (The Pathophysiology of Diarrhea)Documento18 pagineBases Da Fisiopatologia Da Diarreia (The Pathophysiology of Diarrhea)MujiartiNessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Introduction To Sample QuestionsDocumento24 pagineIntroduction To Sample QuestionsmtassyNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (894)
- IMNCI Management of Childhood Illness Chart Booklet WHO 2018Documento54 pagineIMNCI Management of Childhood Illness Chart Booklet WHO 2018IgweNessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- DiahrreaDocumento49 pagineDiahrreaRushdiAldeiriNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- CASE STUDY Escherichia ColiDocumento6 pagineCASE STUDY Escherichia ColiEunice AndradeNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Protecting Children from Cholera in KanyamaDocumento8 pagineProtecting Children from Cholera in KanyamaJameson KaundaNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- 7 Gastroenteritis Nursing Care PlansDocumento9 pagine7 Gastroenteritis Nursing Care PlansEricsonMitraNessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- New Commercial Acceptability of Fresh MilkDocumento33 pagineNew Commercial Acceptability of Fresh MilkEdward Kenneth DragasNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- Communicable DiseasesDocumento12 pagineCommunicable Diseasesjustinejeon6Nessuna valutazione finora
- Group 3 - Week 8 (Nur192)Documento29 pagineGroup 3 - Week 8 (Nur192)Cristine JanolinoNessuna valutazione finora
- Hygiene Promotion Training For Community Mobilisers - Course OutlineDocumento60 pagineHygiene Promotion Training For Community Mobilisers - Course OutlineLaura Tomasa83% (6)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Understanding Nutritional Needs for Ulcerative ColitisDocumento7 pagineUnderstanding Nutritional Needs for Ulcerative ColitisJessica GlitterNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- 05 N269 31604Documento23 pagine05 N269 31604Antony John Britto100% (2)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Sustainable Development Goal 6Documento5 pagineSustainable Development Goal 6Aesthete WishesNessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Standard Guideline 2010 PDFDocumento479 pagineStandard Guideline 2010 PDFLuvita Fitri KarinaNessuna valutazione finora
- Global Health Priorities and ProgramsDocumento22 pagineGlobal Health Priorities and ProgramsNalu ChangNessuna valutazione finora
- Community Health Nursing Roles and ResponsibilitiesDocumento7 pagineCommunity Health Nursing Roles and ResponsibilitiesIsabel Bibat DavidNessuna valutazione finora
- What Are Foodborne IllnessesDocumento2 pagineWhat Are Foodborne IllnessesDavid Lara RodriguezNessuna valutazione finora
- The Pre-Travel Consultation: An OverviewDocumento4 pagineThe Pre-Travel Consultation: An OverviewintanNessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Chakor DraftDocumento12 pagineChakor Draftkhalidiqbal101Nessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- Mininfra-Water and Sanitation Strategic PlanDocumento90 pagineMininfra-Water and Sanitation Strategic PlanEustache NIJEJENessuna valutazione finora
- Stool Analysis: What Is The Stool or Feces?Documento28 pagineStool Analysis: What Is The Stool or Feces?Annisa SafiraNessuna valutazione finora
- GastrointestinalDocumento16 pagineGastrointestinalCelestial, Maybelle MarieNessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- MalnutritionDocumento34 pagineMalnutritionWidoWati RinNieNessuna valutazione finora
- Pediatric Gastroenteritis Workup - Laboratory Studies, Imaging Studies, Other TestsDocumento4 paginePediatric Gastroenteritis Workup - Laboratory Studies, Imaging Studies, Other TestsJL CalvinNessuna valutazione finora
- Rabbit Diseases: Disease Cause Symptoms Prevention TreatmentDocumento3 pagineRabbit Diseases: Disease Cause Symptoms Prevention TreatmentAkinwumiNessuna valutazione finora
- Drug Study Paracetamol Ambroxol Ascorbic Acid CefuroximeDocumento6 pagineDrug Study Paracetamol Ambroxol Ascorbic Acid CefuroximeJaymark LambinoNessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Pro-Ctcae EnglishDocumento18 paginePro-Ctcae EnglishyouldenaNessuna valutazione finora
- Introduction To The CARE Design, Monitoring and Evaluation StandardsDocumento73 pagineIntroduction To The CARE Design, Monitoring and Evaluation StandardsDejan ŠešlijaNessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)