Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Obstetrics & Gynaecology 2019-2008 Regular+Supplementary Group Wise Question Papers WBUHS
Caricato da
Aditya BarmanTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Obstetrics & Gynaecology 2019-2008 Regular+Supplementary Group Wise Question Papers WBUHS
Caricato da
Aditya BarmanCopyright:
Formati disponibili
Obstetrics & Gynecology Group Wise Question
⚕⚕⚕⚕⚕⚕⚕⚕⚕⚕⚕⚕⚕⚕⚕⚕⚕⚕⚕⚕
medgag.com present
2019 TO 2008 GROUP WISE
QUESTIONS PAPERS OF WBUHS &
Recent Marks Distributions
3RD PROFESSIONAL MBBS PART II
Version 2.0
OBSTETRICS &
GYNAECOLOGY
By- DR. ASHIS RONG
Like and follow MEDGAG Facebook Page by scanning this QR code
or touching the Group Logo
www.medgag.com By- Dr. Ashis Rong
Obstetrics & Gynecology Group Wise Question
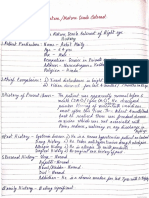
Recent Marks Distributions of WBUHS
❤ Obstetrics & GynaecOlOGy
A. Theory examination 80 marks (2 paper1st paper 40 marks + 2nd paper 40 marks)
Paper I Obstetrics & Social Obstetrics
Paper II Gynaecology, FW & Demography
Questions in Both Papers:
1) Group-A 1 = 10 Marks
Long Question (Basic & Allied)
2) Group-B 1 out of 2 = 10 Marks
Long Question- clinical problem
3) Group-C 2 out of 4 = 2 x 5 =10 Marks
Short Notes
4) Group-D 2 out of 4 = 2 x 5 =10 Marks
Brief answer type
Total = 40 Marks
B. Practical Examination = 50 Marks [30+20]
1. One long case = 30
2. One Short case = 20
C. Oral Examination = 30 Marks
1. Instrument, Operation (only outline) and steps of minor operations =5
2. 6 Specimen = 5
3. X-Ray (only in Gynecology Table) & USG films (Only reading) = 5
4. Problems and recent advances = 5
5. Delivery Notes = 5
6. Obstetrics manoeuvres = 5
D. Internal Assessment = 40 Marks (theory 20 + practical 20)
TOTAL 200 MARKS IN OBSTETRICS & GYNAECOLOGY
www.medgag.com By- Dr. Ashis Rong
Obstetrics & Gynecology Group Wise Question
Obstetrics (PaPer – I)
Group – A
1. What are the varieties of twin pregnancy? What are the antenatal complications of twin pregnancy? How
do you manage a case twin pregnancy after the first baby is delivered vaginally? 2+3+5 (2019 regular; P-
1)
2. What do you mean by gestational diabetes mellitus (GDM)? How do you screen GDM? What are the
complications of diabetes mellitus on pregnancy? Enumerate the major birth defect in infants? 2+2+3+3
(2019 supplementary; P-1)
3. A lady comes with history of 8 months amenorrhoea, on examination fundal height was found to be of 24
week size – What are the possibilities? Give an outline of diagnosis and management of intra-uterine
Foetal Death (IUFD). 2+4+4 (2018 regular; P-1)
4. A primigravida at 36 weeks of gestation with vaginal bleeding attend hospital emergency. What are the
different causes of bleeding in late pregnancy? How will you diagnose the causes and manage such a case?
2+4+4 (2018 supplementary; P-1)
5. How do you diagnose pre-eclampsia? What are its complications? 5+5 (2017 regular; P-1)
6. Briefly describe the diagnosis of twin pregnancy? What are the maternal complication in twine pregnancy?
How would you conduct labour after the delivery of the first baby in twin? (2017 supplementary; P-1)
7. Define intra-uterine fetal death (IUFD). What are its causes? How do you diagnose such a case? 1+4+5
(2016 regular; P-1)
8. Define pre-term labour. Enumerate its cause. How will you manage a case of preterm labour at 33 weeks
of gestation? 2+3+5 (2016 supplementary; P-1)
9. What are the varieties of twin pregnancy? Enumerate the maternal and fetal complications of twin
pregnancy. How would you diagnose twin pregnancy? 2+4+4 (2015 regular; P-1)
10. What are the causes of anaemia in pregnancy? Discuss the complication of anaemia in pregnancy. Briefly
outline its management. 3+4+3 (2015 supplementary; P-1)
11. A primigravida at 34 weeks of gestation with vaginal bleeding attends hospital emergency. Enumerate
the possible causes. How will you diagnose it? What will be the management of such case? 2+4+4 (2014
regular; P-1)
12. What are the indications for induction of labour? What are the different methods of induction? Write
briefly its complication. 3+3+4 (2014 supplementary; P-1)
13. Enumerate the causes of bleeding per vagina in early months of Pregnancy. Discuss the diagnosis of molar
pregnancy and its management. 2+4+4 (2013 regular; P-1)
14. Define antenatal care. Discuss the benefits of the antenatal care and outline the standard antenatal care
methods 2+4+4 (2013 supplementary; P-1)
15. A primigravida of 36 weeks of gestation was admitted with convulsions and a blood pressure of 160/110
mm of Hg. What is your provisional diagnosis? How will you manage this case? 2+3+5 (2012 regular; P-
1)
16. Define ectopic pregnancy. What are the clinical features of unruptured tubal ectopic pregnancy? Discuss
briefly the different modalities of treatment of unruptured tubal pregnancy. 2+3+5 (2012 supplementary; P-
1)
17. A multi gravida carrying 32 weeks of gestation comes to O&G Emergency with the c/o painful bleeding
per vagina. Mention the diagnosis and outline the management in short. 4+6 (2011 regular; P-1)
18. Enumerate the causes of bleeding per vagina in early month of pregnancy. Discuss the diagnosis and
management of threatened abortion. 3+3+4 (2011 supplementary; P-1)
19. A primigravida is admitted at 34 weeks pregnancy with bleeding per vagina. How will you investigate and
manage such a case? 4+6 (2010 regular; P-1)
20. A primigravida at 34 weeks of gestation is brought to hospital with convention and hypertension - Discuss
the management of such a case. 10 (2010 supplementary; P-1)
21. A primigravida had assisted delivery with outlet forceps. She started severe vaginal bleeding four hours
after child birth. Enumerate the causes of this bleeding. How will you manage such a patient?v2+8 (2009
regular; P-1)
22. A 26 years old primigravida carrying twins has just delivered baby. Write in brief your subsequent
management till the second baby is born. What are the post-partum complications of twin pregnancy? 7+3
(2009 supplementary; P-1)
www.medgag.com By- Dr. Ashis Rong 1
Obstetrics & Gynecology Group Wise Question
23. Define Pre-eclampsia. What are the diagnostic criteria? What are immediate and remote complications?
Outline a protocol of management of Eclampsia with Magnesium Sulphate. 2+2+3+3 (2008 regular; P-1)
24. Describe the symptoms and sign of iron deficiency anaemia. How do you investigate such a case? What
are the complication of severe anaemia in pregnancy? 2+4+4 (2008 supplementary; P-1)
Group – B
1. Define maternal mortality ratio. What are the factors that control MMR? How can it be reduced? 2+3+5
(2019 regular; P-1)
2. A 24 year old lady at 34 weeks of pregnancy has a blood pressure of 150/100 mm of Hg. What are the
possible causes? How do you manage such a case? 3+7 (2019 supplementary; P-1)
3. Define PPH. What are the causes of PPH? How do you manage a case of atonic PPH immediately after
vaginal delivery? 2+3+5 (2018 regular; P-1)
4. What is Eclampsia? Outline the management of Eclampsia. What are the complication of Eclampsia?
2+5+3 (2018 supplementary; P-1)
5. Define abortion. Give its classification. How do you differentiate between threatened abortion and
inevitable abortion? Briefly outline the management of missed abortion. 2+2+3+3 (2017 regular; P-1)
6. How do you diagnose tubal ectopic pregnancy? Outline the management of tubal ectopic pregnancy. 5+5
(2017 supplementary; P-1)
7. A primigravida, 28 years, presents with vaginal bleeding at 34 weeks of gestation. What are its causes?
How will you investigate such a case? Outline its management. 2+3+5 (2016 regular; P-1)
8. Define post-partum hemorrhage (PPH). What are the causes of primary PPH? Discuss the management of
third stage hemorrhage. 2+3+5 (2016 supplementary; P-1)
9. What are the causes of bleeding per vagina in the first trimester of pregnancy? Discuss the diagnosis of
hydatidiform mole. Write in short its management. 2+4+4 (2015 regular; P-1)
10. A 24 year old primigravida attends hospital emergency with history of amenorrhoea for 34 weeks with
headache and swelling of feet. What is the likely diagnosis? How would you proceed to manage the case?
What are the complication associated with this condition? 2+4+4 (2015 supplementary; P-1)
11. Define normal labour. What are the different stages of labour? How will you monitor the progress of
labour? What precautions are taken during delivery of head in vertex position? 2+2+4+2 (2014 regular; P-
1)
12. Define PPH. How would you classify PPH? How would you manage a case of atonic PPH? 2+3+5 (2014
supplementary; P-1)
13. Discuss the diagnosis & complications of twin pregnancy. Enumerate briefly the management of twin
pregnancy in labour. 3+3+4 (2013 regular; P-1)
14. Define anaemia in pregnancy. Enumerate the causes and complication of anaemia in pregnancy. Discuss
its management in a lady with 32 weeks of pregnancy. 2+2+2+4 (2013 supplementary; P-1)
15. Define intrauterine foetal death. Enumerate the causes of intrauterine foetal death. Outline it’s
management. 2+3+5 (2012 regular; P-1)
16. A women is having profuse vaginal bleeding shortly after delivery of placenta her fourth childbirth. On
examination her uterus feels flabby. What is your diagnosis? What are the common causes of bleeding
shortly after childbirth? How will you manage this case? How such bleeding can be prevented? 2+3+2+3
(2012 supplementary; P-1)
17. Define Recurrent Abortion. Outline the investigations in such a case. 2+8 (2011 regular; P-1)
18. Discuss the diagnosis and management of a case of Rh-immunisation from 1st trimester of pregnancy till
delivery. 5+5 (2011 supplementary; P-1)
19. A multigravida is admitted at 32 weeks pregnancy with a haemoglobin value of-4 gm%. Discuss
investigation and management of such a ease. 3+7 (2010 regular; P-1)
20. What are the causes of intrauterine foetal death (IUFD). Discuss the diagnosis and management of such.
4+3+3 (2010 supplementary; P-1)
21. A primigravida aged 30 years attends your clinic at 32 weeks of gestation with breech presentation. How
will you manage the case till birth of the baby? What injury may occur to the mother and the baby during
vaginal breech delivery? 5+5 (2009 regular; P-1)
22. How will you diagnose intrauterine foetal death? Outline the management of such a case in a diabetic
primigravida carrying 36 weeks of pregnancy. 5+5 (2009 supplementary; P-1)
23. Define habitual abortion. How will you investigate a patient with history of habitual abortion? Briefly
outline the treatment of cervical incompetence in pregnancy. 2+5+3 (2008 regular; P-1)
www.medgag.com By- Dr. Ashis Rong 2
Obstetrics & Gynecology Group Wise Question
24. Define intra-uterine growth restriction I.U.G.R. what are the factors that contribute to I.U.G.HR.? How
toy can diagnosis such a case and confirm it? 2+3+5 (2008 supplementary; P-1)
Group – C
1. Missed abortion. (2019 regular; P-1)
2. Causes of obstructed labour. (2019 regular; P-1)
3. Battledore placenta. (2019 regular; P-1)
4. Uses of oxytocin in obstetrics. (2019 regular; P-1)
5. Deep transvers arrest. (2019 supplementary; P-1)
6. Episiotomy. (2019 supplementary; P-1)
7. Oligohydramnios. (2019 supplemen(2019 supplementary; P-1)tary; P-1)
8. Velamentous insertion of cord.
9. Plane of pelvic dimension. (2018 regular; P-1)
10. Medical management of ectopic pregnancy. (2018 regular; P-1)
11. MgSO4 (Magnesium Sulphate) therapy in eclampsia. (2018 regular; P-1)
12. Apgar score. (2018 regular; P-1)
13. Puerperal pyrexia. (2018 supplementary; P-1)
14. Retained placenta. (2018 supplementary; P-1)
15. Haematological changes of pregnancy. (2018 supplementary; P-1)
16. Bishop’s score. (2018 supplementary; P-1)
17. Non-stress test. (2017 regular; P-1)
18. Amniotic fluid. (2017 regular; P-1)
19. Puerperal sepsis. (2017 regular; P-1)
20. Neonatal resuscitation at birth. (2017 regular; P-1)
21. Lower uterine segment. (2017 supplementary; P-1)
22. Cord prolapse. (2017 supplementary; P-1)
23. Hyperemesis gravidarum. (2017 supplementary; P-1)
24. Placenta membranacea. (2017 supplementary; P-1)
25. Use of Misoprostol in Obstetrics. (2016 regular; P-1)
26. Placenta succenturiate. (2016 regular; P-1)
27. Routine examination of newborn at birth. (2016 regular; P-1)
28. Vulval haematoma. (2016 regular; P-1)
29. Diagnosis of missed abortion. (2016 supplementary; P-1)
30. External cephalic version. (2016 supplementary; P-1)
31. Velamentous insertion of cord. (2016 supplementary; P-1)
32. Exclusive breastfeeding. (2016 supplementary; P-1)
33. Haematological changes in pregnancy. (2015 regular; P-1)
34. Battledore placenta. (2015 regular; P-1)
35. Complications in Intra-uterine fetal death. (2015 regular; P-1)
36. Benefits of breast feeding. (2015 regular; P-1)
37. Puerperal pyrexia. (2015 supplementary; P-1)
38. Hyperemesis gravidarum. (2015 supplementary; P-1)
39. Hydrops fetalis. (2015 supplementary; P-1)
40. Complication of preterm baby. (2015 supplementary; P-1)
41. Retained placenta. (2014 regular; P-1)
42. Long Uterine Segment. (2014 regular; P-1)
43. Apgar Score. (2014 regular; P-1)
44. Vulva hematoma. (2014 regular; P-1)
45. Importance of USG in obstetrics. (2014 supplementary; P-1)
46. Morbidly adherent placenta. (2014 supplementary; P-1)
47. Follow-up in Molar pregnancy. (2014 supplementary; P-1)
48. Importance of Ischial spine in obstetrics. (2014 supplementary; P-1)
49. Obstetric outlet. (2013 regular; P-1)
50. Partogram. (2013 regular; P-1)
51. Cord prolapse. (2013 regular; P-1)
52. Presenting part. (2013 supplementary; P-1)
www.medgag.com By- Dr. Ashis Rong 3
Obstetrics & Gynecology Group Wise Question
53. Amniotic fluid. (2013 supplementary; P-1)
54. Missed abortion. (2013 supplementary; P-1)
55. Perinatal transmission of HIV. (2013 supplementary; P-1)
56. External Cephalic Version. (2012 regular; P-1)
57. Retained Placenta. (2012 regular; P-1)
58. Maternal Complications of multifetal pregnancy. (2012 regular; P-1)
59. Cardiovascular changes in normal pregnancy. (2012 regular; P-1)
60. Prophylaxis against the isoimmunisation. (2012 supplementary; P-1)
61. Management of premature rupture of membrane. (2012 supplementary; P-1)
62. Management of the iron deficiency anaemia in pregnancy. (2012 supplementary; P-1)
63. Bishop's Score. (2011 regular; P-1)
64. Physiological Anaemia of Pregnancy. (2011 regular; P-1)
65. Induction of Labour. (2011 regular; P-1)
66. Role of ultrasound in early pregnancy. (2011 supplementary; P-1)
67. Deep transverse Arrest in Labour. (2011 supplementary; P-1)
68. Partogram. (2011 supplementary; P-1)
69. Screening for Down’s syndrome in pregnancy. (2010 regular; P-1)
70. Non-stress test. (2010 regular; P-1)
71. Polyhydramnios. (2010 regular; P-1)
72. Active management of 3rd stage of labour. (2010 supplementary; P-1)
73. Complications of monochorionic twins. (2010 supplementary; P-1)
74. Complete perineal tear. (2010 supplementary; P-1)
75. Face presentation. (2009 regular; P-1)
76. Daily foetal movement count beyond 36 weeks of pregnancy. (2009 regular; P-1)
77. Partogram. (2009 regular; P-1)
78. Obstetrics outlet of pelvis. (2009 supplementary; P-1)
79. Artificial rupture of membranes. (2009 supplementary; P-1)
80. Acute puerperal mastitis. (2009 supplementary; P-1)
81. Lower Uterine Segment. (2008 regular; P-1)
82. Vulval Haematoma. (2008 regular; P-1)
83. Non-Stress test. (2008 regular; P-1)
84. Bishop’s score. (2008 supplementary; P-1)
85. Deep transverse arrest. (2008 supplementary; P-1)
86. HELLP syndrome. (2008 supplementary; P-1)
Group – D
1. All cases of placenta previa do not require caesarean delivery – Justify. (2019 regular; P-1)
2. Thalassemia screening should be done in the first antenatal visit – Comment. (2019 regular; P-1)
3. Cord blood test in Rh-negative mother is necessary – Justify. (2019 regular; P-1)
4. Follow up of a case of H. Mole is essential – Justify. (2019 regular; P-1)
5. Active management of third stage of labour is mandatory – Justify (2019 supplementary; P-1)
6. Through assessment is needed before induction of labour – Comment (2019 supplementary; P-1)
7. Routine examination of urine during pregnancy is essential – Justify (2019 supplementary; P-1)
8. Fetal anomaly scan should be done in the first half of pregnancy – Comment (2019 supplementary; P-1)
9. Once caesarean section in not always caesarean section – Justify (2018 regular; P-1)
10. Routine ultrasonography USG examination in second trimester 18-20 weeks, to all pregnant mother is
mandatory – Justify (2018 regular; P-1)
11. Supplementation of folic acid is necessary in all pregnancy – Justify (2018 regular; P-1)
12. All labours should be monitored by partograph – Comment (2018 regular; P-1)
13. Inspection of placenta after delivery is mandatory – Justify (2018 supplementary; P-1)
14. Exclusive breastfeeding is beneficial for mother also – Justify (2018 supplementary; P-1)
15. Caesarean section should be done liberally in breech presentation – Justify (2018 supplementary; P-1)
16. Low forceps delivery is still justified – Comment (2018 supplementary; P-1)
17. Active management of third stage of labour should be routinely practised – justify (2017 regular; P-1)
18. Injection Betamethasone should be given to all women with pre-term labour – justify (2017 regular; P-1)
www.medgag.com By- Dr. Ashis Rong 4
Obstetrics & Gynecology Group Wise Question
19. Follow up is necessary after evacuation of Hydatidiform mole – comment (2017 regular; P-1)
20. All antenatal mothers should be screened for diabetes mellitus – justify (2017 regular; P-1)
21. Maternal mortality is mostly avoidable – Justify (2017 supplementary; P-1)
22. Anti-D immunoglobulin can prevent Rh-iso-immunization – Comment (2017 supplementary; P-1)
23. Iron supplementary is necessary in pregnancy – Justify (2017 supplementary; P-1)
24. Eclampsia is a preventable disease – Comment (2017 supplementary; P-1)
25. Early diagnosis of ectopic pregnancy prevents surgical intervention – Justify (2016 regular; P-1)
26. Oral iron supplementation during pregnancy is necessary – Comment (2016 regular; P-1)
27. Perinatal mortality and morbidity is higher in breech delivery – Comment (2016 regular; P-1)
28. All post – caesarean section mothers do not require caesarean section as a mode of Termination of
subsequent pregnancy. (2016 regular; P-1)
29. Ventouse delivery is safer in comparison to forcep delivery – Comment (2016 supplementary; P-1)
30. Use of ultrasonography is essential during pregnancy – Comment (2016 supplementary; P-1)
31. Routine screening for HIV in Antenatal mothers is very important – Justify (2016 supplementary; P-1)
32. Magnesium sulphate is a drug of choice in the treatment of eclampsia – Comment (2016 supplementary; P-
1)
33. Iron therapy is essential during pregnancy – Justify (2015 regular; P-1)
34. Partograph is a suitable method to monitor labour – Comment (2015 regular; P-1)
35. Active management of third stage of labour should be done in all cases – Justify (2015 regular; P-1)
36. Eclampsia is preventable to a large extent – Comment (2015 regular; P-1)
37. Tubal pregnancy does not always need surgical intervention – Justify (2015 supplementary; P-1)
38. Prompt and adequate provision of blood reduce maternal mortality – Justify (2015 supplementary; P-1)
39. Betamethasone should be given to all pregnant women with threatened preterm labour – Comment (2015
supplementary; P-1)
40. Inspection of placenta after delivery is mandatory – Justify (2015 supplementary; P-1)
41. Maternal mortality is mostly preventable – Justify (2014 regular; P-1)
42. All pregnant women should undergo routine ultrasound in 2nd trimester (18-12) week – Justify (2014
regular; P-1)
43. Screening for HIV infection should be done on all pregnant women – Justify (2014 regular; P-1)
44. External cephalic version still has got a place in the management of breech presentation – Comment (2014
regular; P-1)
45. MVA (Manual Vacuum Aspiration) is preferable over other methods of termination of pregnancy in early
first trimester – Justify (2014 supplementary; P-1)
46. Ventouse is preferable over obstetric forceps – Comment (2014 supplementary; P-1)
47. All post caesarean pregnancy at term do not required caesarean section to terminate the pregnancy –
Comment (2014 supplementary; P-1)
48. Treatment of anaemia in pregnancy reduces maternal mortality – Justify (2014 supplementary; P-1)
49. All post caesarean section Pregnancy cases may not be delivered by caesarean section again – Give reasons.
(2013 regular; P-1)
50. Magnesium sulphate is the drug of choice in the treatment of Eclampsia – Justify (2013 regular; P-1)
51. Active management of third stage of labour should be done in all cases – Justify (2013 regular; P-1)
52. Prophylactic Iron therapy should be given to all pregnant women – Justify (2013 regular; P-1)
53. All vaginal breech delivery should be conducted by trained birth attendants – Comment (2013
supplementary; P-1)
54. Eclampsia is a preventable disease – Comment (2013 supplementary; P-1)
55. Ectopic pregnancy may also be managed medically – Comment (2013 supplementary; P-1)
56. Not all cases of vaginal delivery need episiotomy – Comment (2013 supplementary; P-1)
57. All cases of placenta praevia should be delivered by caesarean section – Comment (2012 regular; P-1)
58. Forceps is losing its place to ventouse us a method of instrumental delivery – Comment (2012 regular; P-
1)
59. Routine ultrasonography in all asymptomatic low risk pregnant women is not recommended – Justify (2012
regular; P-1)
60. Vaginal delivery in breech presentation is more dangerous than in vertex presentation – Justify (2012
regular; P-1)
61. Emergency obstetric care (EmOC) is one of the most effective strategies for preventing maternal death –
Explain how? (2012 supplementary; P-1)
www.medgag.com By- Dr. Ashis Rong 5
Obstetrics & Gynecology Group Wise Question
62. Breast milk is the best food for a newborn – Justify (2012 supplementary; P-1)
63. Partograph has reduced perinatal mortality and maternal morbidity considerably – Justify (2012
supplementary; P-1)
64. Routine screening for foetal congenital malformation is a must even in low risk young primigravida –
Commend (2012 supplementary; P-1)
65. How antenatal care can reduce maternal mortality in our country. (2011 regular; P-1)
66. HIV testing should be done in all pregnant woman – Justify (2011 regular; P-1)
67. Episiotomy reduces many of the gynaecological disorder – Clarify it (2011 regular; P-1)
68. Pre-eclampsia is not preventable always whereas Eclampsia is always preventable – Justify (2011 regular;
P-1)
69. Vaginal delivery of breech presentation increases perinatal morbidity and mortality – How and when?
(2011 supplementary; P-1)
70. Breast feeding reduces neonatal and infant morbidity and mortality – Discuss in short (2011 supplementary;
P-1)
71. Vaginal birth is possible in post caesarean pregnancy – When and how? (2011 supplementary; P-1)
72. All pregnant women should be given iron and folic acid – Comment (2010 regular; P-1)
73. All pregnant women should undergo ultrasound in second trimester – Justify (2010 regular; P-1)
74. All women should be advised about early breast feeding – Why?(2010 regular; P-1)
75. injection betamethasone should be given to all women with preterm labour – Justify (2010 regular; P-1)
76. Prophylactic forceps delivery is beneficial in post-caesarean vaginal delivery – Justify (2010 supplementary;
P-1)
77. Ergometrine should not be given to prevent postpartum hemorrhage in a woman with heart disease – Give
reasons (2010 supplementary; P-1)
78. All pregnant women should undergo haemoglobin estimation and blood group testing – Justify (2010
supplementary; P-1)
79. Manual removal of placenta should be done under general anaesthesia – Give reasons (2010 supplementary;
P-1)
80. All pregnant women should be offered screwing for HIV infection in early pregnancy – Justify (2009
regular; P-1)
81. Magnesium sulphate is the drug of choice in the treatment of eclampsia – Justify (2009 regular; P-1)
82. Active management of third stage of labour should be done in all cases – Justify (2009 regular; P-1)
83. Maternal mortality is mostly avoidable – Comment (2009 regular; P-1)
84. All cases of post caesarean pregnancy at term should be delivered by caesarean section – Comment (2009
supplementary; P-1)
85. Height of fundus of gravid uterus may not always corroborate with the period of amenorrhea – Give reason
(2009 supplementary; P-1)
86. Anti–D prophylaxis is a must in a Rh-negative foetus in situations of likely foeto-maternal haemorrhage
– Justify (2009 supplementary; P-1)
87. Ultrasonography should be done during antenatal investigation of all pregnant women – Comment (2009
supplementary; P-1)
88. Prenatal counselling is a must – Justify (2008 regular; P-1)
89. External Cephalic Version has got a place in management of breech presentation – Critically evaluate (2008
regular; P-1)
90. Misoprostol has almost replaced other drugs for pregnancy termination (MTP) – Comment (2008 regular;
P-1)
91. Twin pregnancy is a high risk pregnancy – Justify (2008 regular; P-1)
92. Once a caesarean section dose not mean always a caesarean section – Comment (2008 supplementary; P-1)
93. Most of the maternal death are preventable – Justify (2008 supplementary; P-1)
94. Management of cases of eclampsia needs special set up – Justify (2008 supplementary; P-1)
95. Follow up of all Hydatidiform mole patient should be done – Justify (2008 supplementary; P-1)
www.medgag.com By- Dr. Ashis Rong 6
Obstetrics & Gynecology Group Wise Question
GynaecoloGy (PaPer – II)
Group – A
1. Define post – menopausal bleeding. What are its causes? How do you manage such a case? 2+3+5 (2019
regular; P-2)
2. Define Primary amenorrhoea. How do you proceed to investigate a case of primary amenorrhoea? 2+8
(2019 supplementary; P-2)
3. What are the common cause of lower abdominal lump in women of reproductive age group? How will you
differentiate clinically between ovarian and uterine lump? Enumerate the common epithelial ovarian
tumours. 3+4+3 (2018 regular; P-2)
4. Define menorrhagia. Enumerate the causes of Menorrhagia. Discuss the management of 35 years aged
lady, complains of heavy flow and USG showing a large uterine fibroid of 9x9 cm., present on the anterior
wall of body of uterus. 2+3+5 (2018 supplementary; P-2)
5. Define ovulation. What are the symptoms and signs of ovulation? How would you investigate the female
factors in a case of infertility? 1+4+5 (2017 regular; P-2)
6. A patient with 16 weeks pregnancy uterine size lump attends OPD. What are the possible causes of that
lump? How would you manage a 42 years old patient with uterine fibroid? What are the degenerative
changes of fibroid? 2+5+3 (2017 supplementary; P-2)
7. Define metrorrhagia. What are its causes? How would you proceed to manage a patient aged 45 years
having metrorrhagia? 1+3+6 (2016 regular; P-2)
8. Briefly describe the supports of uterus. What are the causes of genito-urinary prolapse? How would you
assess the degree of the prolapse? 4+3+3 (2016 supplementary; P-2)
9. Define post-menopausal bleeding. What are the causes of post-menopausal bleeding? Give an outline of
its management. 1+4+5 (2015 regular; P-2)
10. Define infertility. Discuss in brief the cause of primary infertility in the female. Outline the investigation
in the female partner. Give a short account of one ovulation inducing drug. 1+4+4+1 (2015 supplementary;
P-2)
11. What are the different types of genito-urinary fistula? What are its cause? How will you diagnose a case
of V.V.F.? 2+4+4 (2014 regular; P-2)
12. Define menopause. What are the clinical problems associated with menopause? How are those problems
addressed? 2+3+5 (2014 supplementary; P-2)
13. What are the causes of menorrhagia. Discuss the management of uterine fibroid. 4 + 6 (2013 regular; P-2)
14. What is amenorrhoea? What are the types of Amenorrhoea? Discuss the management of P.C.O.D. 1+3+6
(2013 supplementary; P-2)
15. Discuss the supports of uterus. Enumerate the etiological factors for Pelvic organ Prolapse. Outline the
management of procidentia in a post menopausal lady. 4+3+3 (2012 regular; P-2)
16. A 45 years old woman presented with irregular vaginal bleeding for one year duration. Discuss the
differential diagnosis. Discuss management of early stage cervical cancer. 4+6 (2012 supplementary; P-2)
17. Define Menorrhagia. What are its causes? How would you manage a case of Menorrhagia due to fibroid
uterus? 2+2+6 (2011 regular; P-2)
18. Mention the causes of primary amenorrhea. Mention modern day tools for diagnostic evaluation of a case
of primary amenorrhea. 4+6 (2011 supplementary; P-2)
19. Enumerate causes of menorrhagia in a forty year old women. Discuss management of such a case with
fibroids. 3+7 (2010 regular; P-2)
20. Enumerate the causes of postmenopausal bleeding per vagina. Describe the management of carcinoma
endometrium in a 60 years women. 3+7 (2010 supplementary; P-2)
21. Name the cervical premalignant lesions. How do you screen these lesions? Describe the FIGO staging of
carcinoma of cervix. 2+3+5 (2009 regular; P-2)
22. Classify benign ovarian tumors. What are the clinical features of malignancy in a patient with ovarian
tumour? What is stage 1 ovarian malignancy according to FIGO? 5+2+3 (2009 supplementary; P-2)
23. Define post menopausal bleeding. What are the causes? How you will arrive at a diagnosis in a case of
post menopausal bleeding? l+4+5 (2008 regular; P-2)
24. Define infertility. What are indirect of presumptive evidences of ovulation and how they are inferred? What
are the direct and conclusive evidence of ovulation? 2+4+4 (2008 supplementary; P-2)
www.medgag.com By- Dr. Ashis Rong 7
Obstetrics & Gynecology Group Wise Question
Group – B
1. What are the types of genito-urinary fistula? How do you diagnose VVF? Enumerate the causes of VVF.
3+4+3 (2019 regular; P-2)
2. What is abnormal uterine bleeding? Enumerate its causes. How do you investigate such a case in a 40 years
old leady? 2+3+5 (2019 supplementary; P-2)
3. A women aged 35 years came to OPD with the complain of something coming down per vagina. What are
different diagnosis and distinguishing features of these condition? Discuss the different treatment options
available for second degree vagino-uterine prolapse? 2+4+4 (2018 regular; P-2)
4. Define infertility. Enumerate the ovarian causes of infertility. What are the evidence of ovulation? Name
some drugs used for induction of ovulation. 1+4+3+2 (2018 supplementary; P-2)
5. What are the causes of post-menopausal bleeding? How would you proceed to investigate such a case? 4+6
(2017 regular; P-2)
6. What are the causes of abnormal vaginal discharge? Briefly mention the clinical features of candida
vaginitis? How would you differentiate it from trichomonas vaginalis? 3+4+3 (2017 supplementary; P-2)
7. Enumerate two common varieties of benign epithelial tumours of ovary. Discuss the diagnosis and
management of benign ovarian tumour. 1+4+5 (2016 regular; P-2)
8. Enumerate the common site of endometriosis. What are the symptoms of pelvic endometriosis? Briefly
discuss the medical management of pelvic endometriosis. 2+4+4 (2016 supplementary; P-2)
9. A 15 year old girl complains of amenorrhoea with periodic pain in lower abdomen. How would you proceed
to diagnose the case? What will be the management of such a case? 5+5 (2015 regular; P-2)
10. Define menorrhagia. What are its causes? Discuss the management of such a case associated with a large
firm hypogastric mass. 1+4+5 (2015 supplementary; P-2)
11. What is dysmenorrhoea? How will you differentiate between primary and secondary dysmenorrhoea? How
will you treat a case of primary dysmenorrhoea? +4+5 (2014 regular; P-2)
12. A lady, 40 years of age, presents with a lower abdominal lump. Enumerate the possible causes. How would
you investigate such a case? 5+5 (2014 supplementary; P-2)
13. What are the causes of Infertility in female partner. Discuss the methods of detection of ovulation & how
to induce ovulation. 2 +4 +4 (2013 regular; P-2)
14. What is Cervical Intraepithelial Neoplasm? How to diagnose premalignant lesion of cervix? Discuss the
management of CIN 2+4+4 (2013 supplementary; P-2)
15. A 45 years old lady with a lower abdominal lump complains of pelvic pain. Who are the possible causes?
Briefly outline the management of such a case. 3+7 (2012 regular; P-2)
16. Enumerate the common site of endometriosis. What are the clinical features of pelvic endometriosis?
Briefly discuss the medical management of pelvic endometriosis. 2+2+6 (2012 supplementary; P-2)
17. Define secondary infertility. What are the causes of secondary infertility? Outline the investigation of such
a case. 2+4+4 (2011 regular; P-2)
18. Define in Endometriosis. Mention the common site of endometriosis. Outline the treatment options
available for pelvic endometriosis. 2+2+5 (2011 supplementary; P-2)
19. Discuss investigation of a couple with primary infertility. Describe drugs used for ovulation induction. 5+5
(2010 regular; P-2)
20. Write briefly the causes of genital prolapse. Discuss the management of a case of uterine prolapse with
cystocele and rectocele in a 35 years old woman. 4+6 (2010 supplementary; P-2)
21. What are the types of urinary incontinence? A primipara aged 22 years who had forceps delivery following
prolonged delivery, complains of continuous leakage of urine par vaginal, which started about 7 days after
childbirth. Mention the likely cause and your methods to diagnosis of the condition. 5+1+4 (2009 regular;
P-2)
22. How will you proceed to investigate and treat a case of abnormal uterine bleeding in parous women age
38 years? 5+5 (2009 supplementary; P-2)
23. Define secondary amenorrhoea. What are the pathological causes of secondary amenorrhoea? Mention the
investigations necessary for diagnosis of PCOS. 1+4+5 (2008 regular; P-2)
24. A 14 year old girl attended G&O emergency with the complain of primary amenorrhoea, lower abdominal
pain, acute retention of urine and a lower abdominal mass. What is the probable diagnosis? How will you
investigate the case and treat her? 2+5+3 (2008 supplementary; P-2)
www.medgag.com By- Dr. Ashis Rong 8
Obstetrics & Gynecology Group Wise Question
Group – C
1. Lymphatic drainage of vulva. (2019 regular; P-2)
2. Vaginal candidiasis. (2019 regular; P-2)
3. Supports of the Uterus. (2019 regular; P-2)
4. Inversion of uterus. (2019 regular; P-2)
5. Puberty menorrhagia. (2019 supplementary; P-2)
6. Imperforate hymen. (2019 supplementary; P-2)
7. FIGO staging od carcinoma of cervix. (2019 supplementary; P-2)
8. Contraindications of intra-uterine devices. (2019 supplementary; P-2)
9. Puberty menorrhagia. (2018 regular; P-2)
10. Complication of ovarian tumour. (2018 regular; P-2)
11. definition and causes of secondary amenorrhoea. (2018 regular; P-2)
12. tubal factors of infertility. (2018 regular; P-2)
13. Hormonal treatment of pelvic endometriosis. (2018 supplementary; P-2)
14. Emergency contraception. (2018 supplementary; P-2)
15. Symptoms and signs of carcinoma cervix. (2018 supplementary; P-2)
16. Family planning methods suitable for breast feeding women. (2018 supplementary; P-2)
17. Perineal body. (2017 regular; P-2)
18. Dermoid cyst of ovary. (2017 regular; P-2)
19. Progesterone-only pill. (2017 regular; P-2)
20. Normal semen report. (2017 regular; P-2)
21. Lymphatic drainage of cervix. (2017 supplementary; P-2)
22. Contraindication of OCP. (2017 supplementary; P-2)
23. Primary dysmenorrhoea. (2017 supplementary; P-2)
24. Puberty menorrhoea. (2017 supplementary; P-2)
25. Causes of secondary dysmenorrhoea. (2016 regular; P-2)
26. PAP smear from cervix. (2016 regular; P-2)
27. Different methods of tubectomy. (2016 regular; P-2)
28. Gartner’s duct cyst. (2016 regular; P-2)
29. Candida vaginitis. (2016 supplementary; P-2)
30. Lymphatic drainage of vulva. (2016 supplementary; P-2)
31. Contraindications of intrauterine devices. (2016 supplementary; P-2)
32. Three swab test. (2016 supplementary; P-2)
33. Vaginal trichomoniasis. (2015 regular; P-2)
34. Uterine polyp. (2015 regular; P-2)
35. Lymphatic drainage of uterine cervix. (2015 regular; P-2)
36. Tubercular endometritis. (2015 regular; P-2)
37. Dermoid cyst of the ovary. (2015 supplementary; P-2)
38. Contra-indication of intrauterine device. (2015 supplementary; P-2)
39. Pelvic part of ureter. (2015 supplementary; P-2)
40. Bacterial vaginosis. (2015 supplementary; P-2)
41. Support of the pelvic organs. (2014 regular; P-2)
42. Mucinous cystadenoma. (2014 regular; P-2)
43. Contraindications of OCP. (2014 regular; P-2)
44. Causes of primary amenorrhoea. (2014 regular; P-2)
45. Metrorrhagia. (2014 supplementary; P-2)
46. Stress urinary incontinence. (2014 supplementary; P-2)
47. Granulosa Cell tumour. (2014 supplementary; P-2)
48. Findings of normal semen analysis. (2014 supplementary; P-2)
49. Cervical erosion. (2013 regular; P-2)
50. Dermoid cyst of ovary. (2013 regular; P-2)
51. Cryptomenorrhea. (2013 regular; P-2)
52. Tubal patency. (2013 supplementary; P-2)
53. Hormonal control of physiology of menstruation. (2013 supplementary; P-2)
54. Emergency Contraception. (2013 supplementary; P-2)
www.medgag.com By- Dr. Ashis Rong 9
Obstetrics & Gynecology Group Wise Question
55. Trichomonal Vaginitis. (2012 regular; P-2)
56. Submucous myoma. (2012 regular; P-2)
57. Progesterone only Pill (POP). (2012 regular; P-2)
58. Puberty menorrhagia. (2012 supplementary; P-2)
59. Bacterial vaginosis. (2012 supplementary; P-2)
60. LNG-IUS (Levonorgestrel containing IUS). (2012 supplementary; P-2)
61. Imperforate Hymen. (2011 regular; P-2)
62. Emergency Commotion. (2011 regular; P-2)
63. Ovarian curses of Secondary Amenorrhoea. (2011 regular; P-2)
64. Laparoscopic female sterilization - advantages and disadvantages. (2011 supplementary; P-2)
65. Diagnosis of malignant ovarian tumors. (2011 supplementary; P-2)
66. Turner's syndrome. (2011 supplementary; P-2)
67. Cervical erosion. (2010 regular; P-2)
68. Methods of 1st trimester MTP. (2010 regular; P-2)
69. Post coital contraceptive. (2010 regular; P-2)
70. Methods of 2nd trimester MTP. (2010 supplementary; P-2)
71. Test of ovulation. (2010 supplementary; P-2)
72. Investigations of a case of vesicovaginal fistula. (2010 supplementary; P-2)
73. Pelvic part of ureter. (2009 regular; P-2)
74. Dermoid cyst of ovary. (2009 regular; P-2)
75. Complications of intra uterine contraceptive device. (2009 regular; P-2)
76. Gartner duct cyst. (2009 supplementary; P-2)
77. Normal semenogram (WHO). (2009 supplementary; P-2)
78. Emergency contraception. (2009 supplementary; P-2)
79. Lymphatic drainage of cervix. (2008 regular; P-2)
80. LNG -IUS. (2008 regular; P-2)
81. Solid tumours of ovary. (2008 regular; P-2)
82. Lymphatic drainage of Vulva. (2008 supplementary; P-2)
83. Medical management of ectopic pregnancy. (2008 supplementary; P-2)
84. CA–125. (2008 supplementary; P-2)
Group – D
1. Ovarian malignancy is a silent killer – Comment. (2019 regular; P-2)
2. Colposc0pe is an important tool for a gynaecologist – Justify. (2019 regular; P-2)
3. All cases of abnormal uterine bleeding (AUB) do not require surgical management – Comment. (2019
regular; P-2)
4. Laparoscopy gives more diagnostic informations than hystero-salpingography – Comment. (2019 regular;
P-2)
5. Tumour marker have important prognostic value in ovarian malignancy – Justify (2019 supplementary; P-
2)
6. Women should undergo cervical PAP smear test – Justify (2019 supplementary; P-2)
7. Weight reduction is the first line treatment in obese PCOS – Comment (2019 supplementary; P-2)
8. Retrograde menstruation is not the only causes of pelvic endometriosis – Comment (2019 supplementary;
P-2)
9. Carcinoma cervix is a preventable malignancy – Justify (2018 regular; P-2)
10. Post-menopausal bleeding per vagina should always be investigate – Justify (2018 regular; P-2)
11. Different types of menstrual abnormalities may be associated with leiomyomas – Comment (2018
regular; P-2)
12. Three swab test differentiates the different urinary fistulas – Comment (2018 regular; P-2)
13. Diagnostic Laparoscopy has advantages over hysterosalpingography for evaluation of tubal factor in an
infertile women – Justify (2018 supplementary; P-2)
14. Husband’s semen analysis is the first investigation while evaluating an infertile couple – Justify (2018
supplementary; P-2)
15. There are many non-contraceptive benefits of oral contraceptive – Comment (2018 supplementary; P-2)
16. Neoadjuvant chemotherapy in malignant ovarian tumour – Discuss (2018 supplementary; P-2)
www.medgag.com By- Dr. Ashis Rong 10
Obstetrics & Gynecology Group Wise Question
17. Ovarian malignancy is often diagnosed late – Comment (2017 regular; P-2)
18. Upper reproductive tract infection is a sequalae of lower reproductive tract infection – Comment (2017
regular; P-2)
19. Use of injectable contraception’s or IUCD are important contraceptives for our country – Justify (2017
regular; P-2)
20. Laparoscopy is mandatory for evaluation of female infertility – Justify (2017 regular; P-2)
21. Cervical cancer is a preventable disease – Justify (2017 supplementary; P-2)
22. Mullerian duct anomaly is often associated with urinary tract abnormality – Comment (2017
supplementary; P-2)
23. Life style modification is important to treat PCOD – Justify (2017 supplementary; P-2)
24. Medical therapy is preferred over surgical treatment in menorrhagia – Comment (2017 supplementary; P-
2)
25. Husband’s semen analysis is the first investigation to evaluate a case of infertility – Justify (2016 regular;
P-2)
26. Surgical treatment for genital prolapse is decided after considering age and reproductive wishes of the
patient – Comment (2016 regular; P-2)
27. Dysfunctional uterine bleeding is a diagnosis of exclusion – Justify (2016 regular; P-2)
28. Syndromic approach is effective for managing reproductive tract infection – Justify (2016 regular; P-2)
29. Body weight reduction is an important part of management of PCOS – Comment (2016 supplementary; P-
2)
30. Post menopausal vaginal bleeding should be properly investigated – Justify (2016 supplementary; P-2)
31. GnRH analogue is an important tool in the management of uterine fibroid – Comment (2016
supplementary; P-2)
32. Ovarian malignancy carried a poorer prognosis than other genital malignancy in female – Comment
(2016 supplementary; P-2)
33. Healthy ovaries should be preserved in hysterectomy done for benign diseases in women aged less than
45 years – Comment (2015 regular; P-2)
34. Oral contraceptive pills have non-contraceptive benefits – Comment (2015 regular; P-2)
35. Laparoscopy is more informative than HSG in evaluation of female infertility – Justify (2015 regular; P-2)
36. Diagnosis of ovarian cancer is usually delayed – Justify (2015 regular; P-2)
37. Cervical cancer is a preventable disease – Comment (2015 supplementary; P-2)
38. Progestin only pill (POP) is recommended for lactating mother – Justify (2015 supplementary; P-2)
39. Repeated vaginal delivery increases the chance of genital prolapse – Comment (2015 supplementary; P-2)
40. Medical therapy is preferred over surgical therapy in the management of DUH cases – Comment (2015
supplementary; P-2)
41. Laparoscopy is essential in gynaecological practice – Comment (2014 regular; P-2)
42. Male partner should be investigated first to evaluate an infertility couple – Justify (2014 regular; P-2)
43. Vaginal bleeding in post-menopausal women should always be investigate – Justify (2014 regular; P-2)
44. There is no appropriate method for screening carcinoma of ovary – Comment (2014 regular; P-2)
45. IUCD is not contraceptive of choice in a newly married woman – Justify (2014 supplementary; P-2)
46. Something coming down per vagina does not necessarily mean- it is a case of genital prolapsed –
Comment (2014 supplementary; P-2)
47. Combined oral contraceptive pills have more benefits than risks – Comment (2014 supplementary; P-2)
48. Medical therapy is preferred over surgical therapy in the management of DUB cases – Comment (2014
supplementary; P-2)
49. Non-contraceptive use of male condoms – Discuss (2013 regular; P-2)
50. Role of Laparoscopy in diagnosis & management of Endometriosis (2013 regular; P-2)
51. Methods of choice of second trimester M.T.P. Justify the methods (2013 regular; P-2)
52. Tumour Marker has great prognostic value in ovarian malignancy – Justify (2013 regular; P-2)
53. Polycystic ovarian syndrome is an endocrine and metabolic disorder – Justify (2013 supplementary; P-2)
54. Trichomonal vaginitis is sexually transmitted disease – Justify (2013 supplementary; P-2)
55. Pregnancy can be avoidable even following unprotected intercourse – Justify (2013 supplementary; P-2)
56. Ovarian conservation during Hysterectomy has both advantages – Discuss (2013 supplementary; P-2)
57. Cervical Screening can effectively reduce Cancer Cervix – Justify (2012 regular; P-2)
58. The scope of laparoscopic surgery is enhancing – Comment (2012 regular; P-2)
www.medgag.com By- Dr. Ashis Rong 11
Obstetrics & Gynecology Group Wise Question
59. Combined oral Contraceptive is the best Contraceptive option for newly married couple – Justify (2012
regular; P-2)
60. Age of the patient should be considered before undertaking hysterectomy for benign conditions. (2012
regular; P-2)
61. Dysfunctional uterine bleeding is a diagnosis by exclusion – Justify (2012 supplementary; P-2)
62. HRT should be used selectively – Justify (2012 supplementary; P-2)
63. Laparoscopy is preferable to Hysterosalpingography in investigation of female infertility – Comment
(2012 supplementary; P-2)
64. No scalpel vasectomy should gradually replace tubectomy as a method of permanent contraception –
Comment (2012 supplementary; P-2)
65. Any case of post-menopausal bleeding should be carefully investigated – Justify (2011 regular; P-2)
66. Indications of ‘Dilatation Curettage’ operation should not be neglected – Mention the discuss the
indication. (2011 regular; P-2)
67. Analyse the importance of Diagnostic Laparoscopy. (2011 regular; P-2)
68. Hysterectomy is not always necessary to treat DUH – clinically evaluate(2011 supplementary; P-2)
69. Laparoscopy is an important investigation for infertility - Justify (2011 supplementary; P-2)
70. Hormone replacement therapy in a post menopausal women – Mention advantages as well as
disadvantages (2011 supplementary; P-2)
71. All married women should undergo PAP smear examination – Justify (2010 regular; P-2)
72. Good counselling can increase contraceptive acceptance – How? (2010 regular; P-2)
73. All women with bilateral tubal block on hysterosalpingography should undergo diagnostic laparoscopy –
Justify (2010 regular; P-2)
74. Prolapse of uterus is preventable – How? (2010 regular; P-2)
75. Laparoscopic ligation is the best method of ligation – Clinically evaluate (2010 supplementary; P-2)
76. All women of reproductive age should undergo pap smear – Comment (2010 supplementary; P-2)
77. Emergency contraception should be widely available – Justify (2010 supplementary; P-2)
78. All adolescent girls should be given HPV vaccine – Justify (2010 supplementary; P-2)
79. Hormone replacement therapy should be advised in all post menopausal women – critically evaluate
(2009 regular; P-2)
80. Laparoscopy is a better procedure than hystero-salpingography in evaluation of infertility – Justify (2009
regular; P-2)
81. Method of your choice for second trimester medical termination of presume (MTP) – Justify your choice
(2009 regular; P-2)
82. Chemotherapy is the mainstay of treatment in chorio-carcinoma of uterus – Justify (2009 regular; P-2)
83. All cases of female infertility should have laparoscopy – Justify (2009 supplementary; P-2)
84. Polycystic ovarian syndrome is a diagnostic riddle – Comment (2009 supplementary; P-2)
85. Complete perineal tear is due to mismanaged second stage of labour – Comment (2009 supplementary; P-
2)
86. As a sterilisation procedure, the ideal site for partial salpingectomy is not ampulla – Comment (2009
supplementary; P-2)
87. Justify the place of H.S.G. in the workup protocol of infertility (2008 regular; P-2)
88. Early diagnosis of ovarian cancer is still not possible – Give reasons (2008 regular; P-2)
89. Male partner should be investigated first in a case of infertility – Give reasons (2008 regular; P-2)
90. Selection of cases must be meticulous before prescribing HRT – Justify (2008 regular; P-2)
91. Genito-Urinary prolapse is a sequelae of multiparity – Comment (2008 supplementary; P-2)
92. Gynaecological Malignancy – Screening may or may not be helpful – Comment (2008 supplementary; P-
2)
93. Chronic pelvic pain needs proper evaluation – Comment (2008 supplementary; P-2)
94. Ovaries need to be preserved during Hysterectomy in patient below 45 years – Justify (2008
supplementary; P-2)
NOTES:…………………………………………………………………………………………………………
…………………………………………………………………………………………………………………...
…………………………………………………………………………………………………………………..
…………………………………………………………………………………………………………………..
…………………………………………………………………………………………………………………...
…………………………………………….....THANK YOU…..………………….……………………………
www.medgag.com By- Dr. Ashis Rong 12
Potrebbero piacerti anche
- PROLOG: Gynecologic Oncology and Critical Care, Eighth Edition (Assessment & Critique)Da EverandPROLOG: Gynecologic Oncology and Critical Care, Eighth Edition (Assessment & Critique)Nessuna valutazione finora
- Comprehensive Handbook Obstetrics & Gynecology 3rd EdDa EverandComprehensive Handbook Obstetrics & Gynecology 3rd EdValutazione: 5 su 5 stelle5/5 (1)
- PROLOG: Obstetrics, Eighth Edition (Assessment & Critique)Da EverandPROLOG: Obstetrics, Eighth Edition (Assessment & Critique)Valutazione: 5 su 5 stelle5/5 (2)
- PROLOG: Patient Management in OfficeDa EverandPROLOG: Patient Management in OfficeValutazione: 5 su 5 stelle5/5 (4)
- The Unofficial Guide to Obstetrics and Gynaecology: Core O&G Curriculum Covered: 300 Multiple Choice Questions with Detailed Explanations and Key Subject SummariesDa EverandThe Unofficial Guide to Obstetrics and Gynaecology: Core O&G Curriculum Covered: 300 Multiple Choice Questions with Detailed Explanations and Key Subject SummariesValutazione: 1.5 su 5 stelle1.5/5 (3)
- Obstetrics and Gynecology Question PapersDocumento22 pagineObstetrics and Gynecology Question Papersprinceej84% (19)
- Obstetrics and Gynecology Question PapersDocumento22 pagineObstetrics and Gynecology Question Papersprinceej84% (19)
- Wits Obstetrics 2008Documento134 pagineWits Obstetrics 2008Muvenn Kannan100% (1)
- MCQ For PG Entrance Obstetrics and Gynaecology PDFDocumento2 pagineMCQ For PG Entrance Obstetrics and Gynaecology PDFdraymanonline.com100% (1)
- PROLOG: Patient Management in the Office, Eighth EditionDa EverandPROLOG: Patient Management in the Office, Eighth EditionNessuna valutazione finora
- Obstetrics and Gynecology Review QuestionsDocumento11 pagineObstetrics and Gynecology Review QuestionsnoblefxNessuna valutazione finora
- Essay Q's Obs and Gyn 2Documento2 pagineEssay Q's Obs and Gyn 2whoosh200886% (7)
- Obstetric-Gynecology MCQsDocumento297 pagineObstetric-Gynecology MCQsDr Ishtiaq Ahmad88% (125)
- 38-Obstetrics & GynecologyDocumento11 pagine38-Obstetrics & GynecologyIbrahimFikry0% (1)
- WHO Labor Care Guide Slides LCGDocumento23 pagineWHO Labor Care Guide Slides LCGAnonymous efqPXILEQJ50% (2)
- Obstetrics and Gynecology NOTESDocumento73 pagineObstetrics and Gynecology NOTESAwais Awais100% (6)
- Gyn MCQs PRIMEsDocumento40 pagineGyn MCQs PRIMEssk100% (2)
- RCOG Green Top Notes 1Documento48 pagineRCOG Green Top Notes 1Anonymous LnLvsb100% (1)
- OngmcqsDocumento26 pagineOngmcqsMoody Summour67% (3)
- Mnemonics in Materia Medica by H. B. Parmar: Read Online and Download EbookDocumento6 pagineMnemonics in Materia Medica by H. B. Parmar: Read Online and Download EbookAditya Barman33% (3)
- The Red Book, 2022-23Documento189 pagineThe Red Book, 2022-23Gringo Chan67% (3)
- Obstetrics & Gynaecology 2019-2008 Regular-Supplementary Group Wise Question Papers WBUHS PDFDocumento14 pagineObstetrics & Gynaecology 2019-2008 Regular-Supplementary Group Wise Question Papers WBUHS PDFAditya BarmanNessuna valutazione finora
- Gynaecology & Obstetrics Sorted Questions 8 SemesterDocumento4 pagineGynaecology & Obstetrics Sorted Questions 8 SemesterSaikat MondalNessuna valutazione finora
- Dewhurst's Textbook of Obstetrics & GynaecologyDa EverandDewhurst's Textbook of Obstetrics & GynaecologyChristoph LeesValutazione: 2 su 5 stelle2/5 (1)
- Instruction Manual in Obstetrics: Volume OneDa EverandInstruction Manual in Obstetrics: Volume OneNessuna valutazione finora
- Medical School Companion Obstetrics and Gynecology Practice Question BookDa EverandMedical School Companion Obstetrics and Gynecology Practice Question BookNessuna valutazione finora
- Nursing the NeonateDa EverandNursing the NeonateMaggie MeeksNessuna valutazione finora
- OBS & GYN MCQsDocumento10 pagineOBS & GYN MCQsmaximNessuna valutazione finora
- Obs QNDocumento15 pagineObs QNAnurag AnupamNessuna valutazione finora
- Emqs ObsDocumento33 pagineEmqs Obsbakkiaha100% (1)
- MCQ - On Obstetrics and Gynaecology PART 2Documento78 pagineMCQ - On Obstetrics and Gynaecology PART 2Kripa Susan100% (3)
- Obstetric SBAs MCQDocumento5 pagineObstetric SBAs MCQCofeelovesIronman Javier100% (1)
- Obstetrics and GynacologyDocumento14 pagineObstetrics and GynacologykalkidanNessuna valutazione finora
- ObstetricsDocumento23 pagineObstetricsSundar MuneesNessuna valutazione finora
- ObG AIIMSDocumento18 pagineObG AIIMSvk100% (1)
- Obs and Gynae Data Interpretation Past PaperDocumento21 pagineObs and Gynae Data Interpretation Past PaperShaheera Shamsudin100% (2)
- OB MustKnowsDocumento90 pagineOB MustKnowsHarlyn MagsinoNessuna valutazione finora
- Mqs For Mrcog Part 2Documento174 pagineMqs For Mrcog Part 2Poppy HazarikaNessuna valutazione finora
- Obstetrics Mcqs PDFDocumento2 pagineObstetrics Mcqs PDFJennifer47% (17)
- Websites & Books MRCOG Part 2Documento2 pagineWebsites & Books MRCOG Part 2kousiksethNessuna valutazione finora
- Obstetrics and Gynecology Module 4Documento7 pagineObstetrics and Gynecology Module 4hevinpatel100% (1)
- C. Anovulation: C. Dysfunctional Uterine BleedingDocumento18 pagineC. Anovulation: C. Dysfunctional Uterine BleedingJan Mikhail Frasco100% (1)
- Normal Abnormal LabourDocumento63 pagineNormal Abnormal LabourFelicianna Ashwinie StanleyNessuna valutazione finora
- Revision in Obstetrics&Gynecology Revision in Obstetrics&GynecologyDocumento136 pagineRevision in Obstetrics&Gynecology Revision in Obstetrics&GynecologySiam Weng Loong100% (4)
- Obstetrics and Gynecology Question Papers - Vol IIDocumento19 pagineObstetrics and Gynecology Question Papers - Vol IIprinceejNessuna valutazione finora
- O&G OSCE by MaddyDocumento287 pagineO&G OSCE by MaddyNariska Cooper100% (1)
- MCQ GynecologyDocumento25 pagineMCQ GynecologyAli Alhaddi80% (5)
- Obstetrics and Gynecology Mock ReviewDocumento14 pagineObstetrics and Gynecology Mock ReviewokurimkuriNessuna valutazione finora
- Clinical Obstetrics and GynaecologyDocumento215 pagineClinical Obstetrics and GynaecologyrizkyocktaNessuna valutazione finora
- Obg Extra EdgeDocumento201 pagineObg Extra EdgeabhishekbmcNessuna valutazione finora
- Obg MCQSDocumento11 pagineObg MCQSShriyansh ChaharNessuna valutazione finora
- MrcogDocumento26 pagineMrcogShafiqueMuhammad100% (1)
- Ospe 2Documento31 pagineOspe 2Med StudentNessuna valutazione finora
- Trial of ScarDocumento12 pagineTrial of Scarnyangara50% (2)
- TOG Articles List 2103-2016Documento4 pagineTOG Articles List 2103-2016FA Khan0% (1)
- Obs & Gyne OSCE CasesDocumento58 pagineObs & Gyne OSCE CasesMegan BolduanNessuna valutazione finora
- Mrcog Part 1Documento26 pagineMrcog Part 1JenkRisk100% (2)
- University of Gondar College of Medicine and Health ScienceDocumento100 pagineUniversity of Gondar College of Medicine and Health ScienceCHALIE MEQUNessuna valutazione finora
- Cases in ObgDocumento41 pagineCases in ObgShriyansh Chahar0% (1)
- The West Bengal University of Health SciencesDocumento21 pagineThe West Bengal University of Health SciencesAditya BarmanNessuna valutazione finora
- Gimsh 9TH SemDocumento4 pagineGimsh 9TH SemAditya BarmanNessuna valutazione finora
- @#&X-Rays Best Shaswata DaDocumento19 pagine@#&X-Rays Best Shaswata DaAditya BarmanNessuna valutazione finora
- Specimen SX (KPC)Documento6 pagineSpecimen SX (KPC)Aditya BarmanNessuna valutazione finora
- @problem Cards (SX)Documento3 pagine@problem Cards (SX)Aditya BarmanNessuna valutazione finora
- MCK 9th Sem (Offline) 2020 PapersDocumento4 pagineMCK 9th Sem (Offline) 2020 PapersAditya BarmanNessuna valutazione finora
- @ophthalmology Long CasesDocumento12 pagine@ophthalmology Long CasesAditya BarmanNessuna valutazione finora
- Eye Short Cases KPCMCH @subiseshDocumento10 pagineEye Short Cases KPCMCH @subiseshAditya BarmanNessuna valutazione finora
- Medicine 2019-2008 Regular-Supplementary Group Wise Question Papers WBUHS-1 PDFDocumento24 pagineMedicine 2019-2008 Regular-Supplementary Group Wise Question Papers WBUHS-1 PDFAditya Barman100% (1)
- Long Cs (Malda) PDFDocumento9 pagineLong Cs (Malda) PDFAditya BarmanNessuna valutazione finora
- Paediatrics 2019-2008 Regular-Supplementary Question Papers (Chapter Wise) - 1 PDFDocumento10 paginePaediatrics 2019-2008 Regular-Supplementary Question Papers (Chapter Wise) - 1 PDFAditya BarmanNessuna valutazione finora
- PostnatalDocumento36 paginePostnatalAditya BarmanNessuna valutazione finora
- SURGERY 2019-2008 Regular-Supplementary Chapter Wise Question Papers WBUHS-1 PDFDocumento17 pagineSURGERY 2019-2008 Regular-Supplementary Chapter Wise Question Papers WBUHS-1 PDFAditya Barman100% (1)
- Must Know in Eye PDFDocumento14 pagineMust Know in Eye PDFAditya BarmanNessuna valutazione finora
- Ophthalmology HistoryDocumento9 pagineOphthalmology HistorySalman FarsiNessuna valutazione finora
- Antenatal Care (Gen - Survey)Documento16 pagineAntenatal Care (Gen - Survey)Aditya BarmanNessuna valutazione finora
- OrthoDocumento23 pagineOrthoAditya BarmanNessuna valutazione finora
- The Cardiovascular SystemDocumento43 pagineThe Cardiovascular Systemtravis efraimNessuna valutazione finora
- Acoustic NeuromaDocumento19 pagineAcoustic NeuromaIshNessuna valutazione finora
- Surgery Report & RatingsDocumento25 pagineSurgery Report & RatingsWXYZ-TV Channel 7 DetroitNessuna valutazione finora
- Upper Respiratory Tract Infection (Farter Bu'RaraDocumento58 pagineUpper Respiratory Tract Infection (Farter Bu'RaraFajrul Fhalaq BasoNessuna valutazione finora
- Red Tide: Causative AgentDocumento2 pagineRed Tide: Causative Agentchristian quiaoitNessuna valutazione finora
- Makerere AR 67th Graduation Day2 22ndfeb2017Documento40 pagineMakerere AR 67th Graduation Day2 22ndfeb2017The Independent Magazine100% (2)
- Perioperative Nursing Concept PDFDocumento21 paginePerioperative Nursing Concept PDFMari Fe100% (1)
- 2021 - BMC - The - Japanese - Clinical - Practice - Guidelines - For - Management SepsisDocumento144 pagine2021 - BMC - The - Japanese - Clinical - Practice - Guidelines - For - Management SepsisSara MendesNessuna valutazione finora
- History Taking Form in Gynecology Obstetrics - CompressDocumento8 pagineHistory Taking Form in Gynecology Obstetrics - CompresskeightNessuna valutazione finora
- Identification of Risk Factors and Seroprevalence For Septicemia Epizootica (SE) Endemic Case of Buffaloes in Aceh Barat, AcehDocumento5 pagineIdentification of Risk Factors and Seroprevalence For Septicemia Epizootica (SE) Endemic Case of Buffaloes in Aceh Barat, AcehSri PrihandaniNessuna valutazione finora
- 4.A.3.3 Ramos v. CA (1999 and 2002)Documento4 pagine4.A.3.3 Ramos v. CA (1999 and 2002)Soraya Salubo Laut100% (1)
- StaphylococcusDocumento28 pagineStaphylococcusAliyah SajaNessuna valutazione finora
- Digestive Questionnaire (Medical)Documento1 paginaDigestive Questionnaire (Medical)Mexico EnglishNessuna valutazione finora
- Stroke Hemoragic: Sebagai Salah Satu Tugas Mata Kuliah TIK Akademi Keperawatan (Akper) SawerigadingDocumento10 pagineStroke Hemoragic: Sebagai Salah Satu Tugas Mata Kuliah TIK Akademi Keperawatan (Akper) SawerigadingMade Serly KrisdayantiNessuna valutazione finora
- CV DR Ari Sami Hussain NadhimDocumento5 pagineCV DR Ari Sami Hussain NadhimAri SamiNessuna valutazione finora
- A Case Study of Perimenopause With KsheerabastiDocumento3 pagineA Case Study of Perimenopause With KsheerabastiEditor IJTSRDNessuna valutazione finora
- Polyphenols, and Physical PerformanceDocumento7 paginePolyphenols, and Physical PerformancezoliteamlavylitesNessuna valutazione finora
- Pre & Post Operative TracheostomyDocumento2 paginePre & Post Operative TracheostomyHantu Kak Limah100% (2)
- Pricelist 13 Juli 2020Documento21 paginePricelist 13 Juli 2020Achmad Sya'idNessuna valutazione finora
- MOCKBOARD Exam I QUISTION ONLYDocumento14 pagineMOCKBOARD Exam I QUISTION ONLYRegine EncinadaNessuna valutazione finora
- Medgears: We Have Been Pioneers at Manufacturing, Exporting and Wholesaling A Wide Assortment of High-QualityDocumento24 pagineMedgears: We Have Been Pioneers at Manufacturing, Exporting and Wholesaling A Wide Assortment of High-QualitySubhasis MallikNessuna valutazione finora
- KetamineDocumento27 pagineKetaminesamfarmer3330% (2)
- DRUGS Initial StockDocumento163 pagineDRUGS Initial StockdeasyNessuna valutazione finora
- Forward IMRT Breast PDFDocumento54 pagineForward IMRT Breast PDFmitza05100% (1)
- Poliomyelitis Proposal PDFDocumento8 paginePoliomyelitis Proposal PDFRbab haiNessuna valutazione finora
- ThesisDocumento111 pagineThesisVictor AkinseyeNessuna valutazione finora
- Knee ReplacementnhschoicesDocumento4 pagineKnee ReplacementnhschoicesCotard DelusionNessuna valutazione finora
- Im Case Study 04Documento49 pagineIm Case Study 04Shaine BalverdeNessuna valutazione finora
- Elman Book FlyerDocumento2 pagineElman Book FlyerCarolina CruzNessuna valutazione finora