Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Vol90 No.11 2338 3744 PDF
Caricato da
SufyanTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Vol90 No.11 2338 3744 PDF
Caricato da
SufyanCopyright:
Formati disponibili
The Accuracy of Preoperative Templating
in Total Knee Arthroplasty
Aasis Unnanuntana MD*,
Marut Arunakul MD*, Amnauy Unnanuntana MD*
* Department of Orthopaedic Surgery, Siriraj Hospital, Mahidol University, Bangkok
Objective: Radiographic templates have been developed to assist with the preoperative planning process.
However, the clinical usefulness of preoperative templating in total knee replacement is still lacking. The
present study aims to evaluate the accuracy of preoperative templating in primary total knee replacement.
Material and Method: A retrospective study of 98 patients and 113 knees was carried out. Both the anteropos-
terior and lateral radiographic views were templated using the templates for DePuy Sigma PFC, fixed bearing
total knee system and the template size was documented for each patient pre-operatively. The operative
records were then reviewed to determine the size of the implant used during the operation.
Results: The overall accuracy between the preoperative template size and the final implant size was 50.4% for
the femoral component and 55.8% for the tibial component. The highest prediction for tibial assessment was
the anteroposterior view and the lateral intercondylar view for femoral assessment.
Conclusion: Approximately 50% of the patients had a preoperative template size that matched the actual
implant used. Many factors influence the final choice of the prosthesis used during total knee replacement;
therefore, the preoperative template size can only be used as a rough guide.
Keywords: Preoperative template, Size, Total knee replacement, Accuracy, Clinical usefulness, Radiographic
view
J Med Assoc Thai 2007; 90 (11): 2338-43
Full text. e-Journal: http://www.medassocthai.org/journal
Preoperative templating is considered an im- accuracy and reliability of preoperative templating in
portant part of preparation for total joint replacement. total knee replacements.
Generally, meticulous preoperative planning allows
the surgeon to perform the procedure precisely, avoid Material and Method
potential intraoperative complication, and achieve A retrospective review of the preoperative
good surgical results(1-3). It is well accepted that pre- radiographs, templates, plans and operative reports
operative templating is of paramount importance in of consecutive primary total knee replacements was
obtaining reproducible results in total hip replacement performed. All patients underwent surgery between
regarding restoration of hip biomechanics and limb January 2002 and January 2004 by a single surgeon
length equality(4-7). However, this step of preoperative (AmU). The preoperative diagnosis was end-stage
planning is not well emphasized in total knee replace- primary osteoarthritis in every patient, except for one
ments. Moreover, only few studies have evaluated the patient with secondary osteoarthritis due to gouty
clinical usefulness and predictability of preoperative arthritis. The exclusion criteria were patients who re-
templating techniques in total knee replacements(8,9). quired a complex surgical procedure such as extensive
Therefore, the present study aimed to evaluate the bone grafting and osteotomy in which the anatomy
could not be easily discerned, those with poor quality
Correspondence to : Unnanuntana A, Department of Ortho-
paedic Surgery, Faculty of Medicine, Siriraj Hospital, Mahidol
radiographs, and those with one or more missing
University, Bangkok 10700, Thailand. Phone: 0-2411-3191, radiographs. This left 113 knees in 98 patients for the
Fax: 0-2412-8172, E-mail: uaasis@yahoo.com present study. There were nine men and 89 women
2338 J Med Assoc Thai Vol. 90 No. 11 2007
with an average age of 68.7 years (range 46-87 years The preoperative radiographic template size
old). The mean deformity was varus 8 degrees (range, and the final prosthesis size were recorded for each
20 varus to 2 valgus), and the average range of patient. The accuracy of the preoperative templating
motion was 118 degrees of flexion with flexion con- technique on each view was reported as a percentage
tacture in 40 knees (range, 20 flexion contracture to and shown on a 95% Confidence Interval (95% CI).
10 of hyperextension). The Kappa Coefficient was used to provide the degree
The surgeon used the cemented, Sigma PFC, of agreement between the preoperative template
fixed bearing knee system in all patients (DePuy, values and the actual components used(12).
Warsaw, IN). Both preoperative and postoperative
radiographs consisted of an anteroposterior (AP) and Results
lateral view of the knee. These radiographs were For the femoral component size, the templated
obtained with a standard 100 cms distance from the size measuring from radiographic lateral intercondy-
tube to X-ray plate, which results in an average magni- lar view had the highest accuracy of 50.4% (57/113
fication of 20 + 6%(10,11). No magnification marker was knees) as shown in Table 1. This accuracy increased
used. The templating was performed by single author to over 90% (94.7% for lateral intercondylar view and
(AaU.) who had no prior knowledge of the implants 97.3% for anteroposterior view) of templated sizes
used in each patient. Four measurements were taken: within one size above or below those actually used
femoral anteroposterior and lateral view, tibial antero- (Table 2). For the tibial components, the highest pre-
posterior and lateral view(3). The measurement of diction of the final component size was measured from
femoral lateral view was subdivided into three tibia AP view with the accuracy of 55.8% (Table 1),
methods. All these measurements were compared with however, 96-97% were within 1 size larger or smaller as
the actual femoral and tibial components used, which shown in Table 2.
were collected from the operative records.
For the anteroposterior view of the femur, the
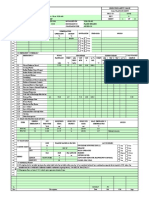
templating began by drawing a line that represented as Table 1. The accuracy of preoperative templating for
femoral and tibial components
a mechanical axis. The predicted femoral component
should be perpendicular to this line and covered both Radiographic view Exactly 95% CI
the medial and lateral condyles as much as possible, matched (%)
taking care not to overhang on each side. For the
lateral view, the template should be placed to maximize Femoral AP assessment 38.1 29.6-47.3
coverage of the distal femoral bone. With the anterior Lateral assessment
flange of the femoral component being flush with the Small femoral condyle 20.4 14.1-28.9
Intercondylar area 50.4 41.4-59.5
anterior femoral cortex, the center of the prosthesis
Large femoral condyle 12.4 7.5-19.7
pointed along the longitudinal axis of the femoral shaft, Tibial AP assessment 55.8 46.6-64.6
avoiding flexion or extension of the femoral compo- Tibial lateral assessment 46.9 38.0-56.1
nent. The authors subdivided the measurement on this
femoral lateral view by using different landmarks on
the posterior femoral cortex. The authors used the small
condyle that represents the lateral femoral condyle, Table 2. The accuracy of preoperative templating within 1
the large condyle that represents the medial femoral size (smaller or larger) for the femoral and tibial
condyle, and the intercondylar line that represents an components
area between the medial and lateral femoral condyle.
Radiographic view % matched 95% CI
For the anteroposterior view of the tibia, the within 1 size
authors placed the template on the tibial plateau with
the tibial stem parallel to the mechanical axis. The Femoral AP assessment 97.3 92.5-99.1
largest size, which covered the greatest amount of host Lateral assessment
bone without overhang on each side, was selected. Small femoral condyle 79.6 71.3-86.0
For the lateral view, the template was placed with the Intercondylar area 94.7 88.9-97.5
tibial stem parallel to the anterior tibial cortex and Large femoral condyle 50.4 41.4-59.5
Tibial AP assessment 96.5 91.3-98.6
adjusted so that the posterior slope best matched the
Tibial lateral assessment 97.3 92.5-99.1
patient’s own anatomy.
J Med Assoc Thai Vol. 90 No. 11 2007 2339
By using the Kappa Coefficient to indicate such as flexion contracture or rotational deformity
the degree of agreement(13), the lateral intercondylar has been identified as a possible source of error in
view of femur and AP view of the tibia gave the best preoperative templating. Heal and Blewitt found that
agreement for the femoral component (0.44) and tibial with the degree of knee flexion contracture increased,
component (0.46) respectively. Both values indicate the distance between the knee and x-ray plate increased
moderate levels of agreement above chance. as well. This resulted in a greater degree of magnifica-
tion on the radiographs(9). Moreover, the rotational
Discussion deformity of the knee can cause an error in sizing of
Preoperative templating has been advocated both the femoral and tibial component in AP and lateral
as a part of preoperative planning in total knee surgery. views as mentioned earlier.
The manufacturers provide various sets of templates Finally, the surgical technique has been shown
for multiple prosthetic designs. The aims of templating to affect the final implant size. Because the femoral
are to reconstruct the biomechanics of the knee joint, component size has an influence on the flexion gap,
predict the size of the optimal prosthetic component the surgical technique, which is based on balancing
size, and preemptively evaluate for any problem that the gap may lead to smaller sizes of the femoral compo-
the surgeon may encounter during the surgery. The nent than we anticipated based on anatomical sizing
principle of templating is to select the component that alone. An example of this situation is clearly seen in a
provides maximum bony containment and least removal recurvatum knee. After the standard distal femoral cut,
of the host bone while maintaining the correct mecha- a large extension space may result. In this situation, the
nical alignment(1,3). It has been widely accepted that surgeon may intentionally downsize the femoral com-
inappropriate size of the prosthesis can be a potential ponent in order to balance the relatively tight flexion
cause of postoperative problem and unfavorable out- gap. The present study tried to minimize this factor
come(14-17). Undersizing of the components may lead to by using the cases from only one surgeon in order to
iatrogenic fracture during the operation or postopera- reduce the influence of various surgical techniques.
tive instability due to imbalance of the flexion and The authors found that the lateral inter-
extension gap, whereas, oversizing of the femoral com- condylar view had the highest prediction of the final
ponents may lead to decreased postoperative flexion, femoral component used. To measure the distal femur,
patellofemoral maltracking, increased patellofemoral the femoral sizing guide (anterior reference) was used
forces and shear, and possibly pain compromising the in all cases. This femoral sizing guide measured the
end result(18-26). distal femur only in 1 dimension (antero-posterior
Aslam et al reported the reliability of pre- dimension (A/P)). Therefore, the size from lateral view
operative templating in 25 primary total knee arthro- of the radiograph mainly determined the overall size of
plasties. They found that the exact size of the prosthe- the femoral component. With this method, the femoral
sis was predicted for 49% of the femoral component component may be fit only on the A/P dimension but
and 67% of the tibial component(8). Heal and Blewitt overhang the bone at medial-lateral (M/L) interfaces.
studied the Kinemax total knee arthroplasty templates In this situation, the surgeon may make an intraopera-
and found only 57% accuracy with the preoperative tive adjustment by increasing or decreasing the femo-
templates(9). Similar to these earlier reports, the authors ral component size depending on the balance of the
found the overall accuracy of 50.4% for the femoral flexion and extension gap and to compensate for the
component and 55.8% for the tibial component with overhang. On the other hand, the authors used the
moderate agreement between preoperative templates medial-lateral dimension of the tibia to consider the
and the actual component used. appropriate intraoperative size because it was hard to
This low accuracy can be explained by several visualize the posterior tibial cortex. Therefore, the tibial
possibilities. Firstly, the rotation of the preoperative AP view had the highest prediction for the final im-
radiographs can obscure some important anatomic plant used.
landmarks and distort the actual bony configuration. Although, it is possible that the prosthetic
This could lead to an error in measurement of the pros- components utilized in the surgery will not be the best
thetic component size. Although the authors tried to fit for the patient’s own anatomy and leads to post-
exclude rotated radiographs, it was not always possible operative problems, the authors are not aware of any
to have the perfectly aligned radiographs available for obvious overhanging or usage of undersized compo-
surgery. Secondly, the patient’s preoperative deformity nents from the postoperative radiographs. In addition,
2340 J Med Assoc Thai Vol. 90 No. 11 2007
there were no intraoperative complications such as and facilitate the identification of specific cases that
fracture or mid-flexion instability. Recently, some manu- require special implants.
facturers have addressed the anatomical differences
between male and female, and introduced a new im- Acknowledgement
plant design, which the femoral component narrower We would like to give our appreciation to
in M/L dimension when compared to the traditional Dr. Stuart B. Goodman for reviewing this paper and
component of the same A/P dimension, to allow better providing us with suggestions.
fit with the patient’s bone and fewer intraoperative
adjustments(27-29). Because these new implant designs References
are not available all the time, careful preoperative 1. Crockarell JR Jr, Guyton JL. Arthroplasty of
templating may help the surgeon to have the appro- ankle and knee. In: Canale ST, editor. Campbell’s
priate sized implants brought to the operative room. operative orthopaedics. Philadelphia: Mosby;
The prediction of femoral and tibial compo- 2003: 265-70.
nent size within + 1 size was achieved in 97.3% and 2. Math KR. Imaging in evaluation of the knee.
96.5% of the femoral and tibial component respectively. In: Scott WN, Clarke HD, Cushner FD, editors.
With this high accuracy, it should theoretically reduce Insall and Scott surgery of the knee. Philadelphia:
the surgical time by allowing the nurse and surgical Churchill Livingstone; 2006: 145-8.
team to have the implants available in the operative 3. Rand JA. Preoperative planning and templating.
room. Della Valle et al showed that the time delay of In: Rand JA, editor. Total knee arthroplasty. New
bringing each of the two components in total hip York: Raven Press; 1993: 93-114.
arthroplasty from the implant room to the operating 4. Eggli S, Pisan M, Muller ME. The value of pre-
room is approximately 2 minutes. By having both com- operative planning for total hip arthroplasty. J
ponents available in the operating room, this could Bone Joint Surg Br 1998; 80: 382-90.
save about 400 minutes of operating room time for any 5. Della Valle AG, Padgett DE, Salvati EA. Preopera-
100 surgeries at one of the author’s institutions(30). tive planning for primary total hip arthroplasty. J
The major drawback of the present study is Am Acad Orthop Surg 2005; 13: 455-62.
its retrospective design and lack of the exact magni- 6. Maloney WJ, Keeney JA. Leg length discrepancy
fication of the preoperative radiographs. It is well after total hip arthroplasty. J Arthroplasty 2004;
known that magnification is directly proportional to 19: 108-10.
the distance between the knee and film; therefore, 7. Muller ME. Lessons of 30 years of total hip
increased magnification can be expected in obese arthroplasty. Clin Orthop Relat Res 1992; 12-21.
patients and conversely, less magnification in thin 8. Aslam N, Lo S, Nagarajah K, Pasapula C, Akmal M.
patients. Although a properly placed magnification Reliability of preoperative templating in total knee
marker may result in additional accuracy in templating, arthroplasty. Acta Orthop Belg 2004; 70: 560-4.
it is the authors’ experience that consistent use of a 9. Heal J, Blewitt N. Kinemax total knee arthroplasty:
magnification marker was not easily instituted in a high trial by template. J Arthroplasty 2002; 17: 90-4.
volume multispecialty university setting such as the 10. Clarke IC, Gruen T, Matos M, Amstutz HC.
authors’. Nevertheless, the authors recognize that Improved methods for quantitative radiographic
the use of magnification markers could potentially evaluation with particular reference to total-hip
improve accuracy in templating, and reappraisal of the arthroplasty. Clin Orthop Relat Res 1976; 121:
radiographic assessment, including the use of digital 83-91.
radiography with known magnification may improve 11. Knight JL, Atwater RD. Preoperative planning for
these results(31). total hip arthroplasty. Quantitating its utility and
In conclusion, the highest prediction of the precision. J Arthroplasty 1992; 7(Suppl):403-9.
final component size was achieved by preoperative 12. Fleiss JL. The measurement of interrater agreement.
templating on the lateral view of the femur and antero- In: Fleiss JL, editor. Statistical methods for rates
posterior view of the tibia with the accuracy of 50.4% and proportions. 2nd ed. New York: John Wiley &
and 55.8% respectively. However, this prediction can Sons; 1981: 212-36.
be improved to more than 90% accuracy by having 1 13. Landis JR, Koch GG. The measurement of observer
size smaller or larger available in the operative room. agreement for categorical data. Biometrics 1977;
Preoperative templating may optimize surgical time 33: 159-74.
J Med Assoc Thai Vol. 90 No. 11 2007 2341
14. Callaghan JJ, O’rourke MR, Saleh KJ. Why knees Hennington LJ. Effect of patella thickness on
fail: lessons learned. J Arthroplasty 2004; 19: 31-4. patella strain following total knee arthroplasty. J
15. Dennis DA. Evaluation of painful total knee Arthroplasty 1991; 6: 251-8.
arthroplasty. J Arthroplasty 2004; 19: 35-40. 25. Ryu J, Saito S, Yamamoto K, Sano S. Factors
16. Incavo SJ, Coughlin KM, Beynnon BD. Femoral influencing the postoperative range of motion in
component sizing in total knee arthroplasty: size total knee arthroplasty. Bull Hosp Jt Dis 1993; 53:
matched resection versus flexion space balanc- 35-40.
ing. J Arthroplasty 2004; 19: 493-7. 26. Scuderi GR, Insall JN, Scott NW. Patellofemoral
17. Laskin RS, Beksac B. Stiffness after total knee pain after total knee arthroplasty. J Am Acad Orthop
arthroplasty. J Arthroplasty 2004; 19: 41-6. Surg 1994; 2: 239-46.
18. Briard JL, Hungerford DS. Patellofemoral instabi- 27. Csintalan RP, Schulz MM, Woo J, McMahon PJ,
lity in total knee arthroplasty. J Arthroplasty 1989; Lee TQ. Gender differences in patellofemoral joint
4(Suppl): S87-97. biomechanics. Clin Orthop Relat Res 2002; 402:
19. Chiu KY, Ng TP, Tang WM, Yau WP. Review 260-9.
article: knee flexion after total knee arthroplasty. 28. Hitt K, Shurman JR, Greene K, McCarthy J, Moskal
J Orthop Surg (Hong Kong ) 2002; 10: 194-202. J, Hoeman T, et al. Anthropometric measurements
20. Koh JS, Yeo SJ, Lee BP, Lo NN, Seow KH, Tan SK. of the human knee: correlation to the sizing of
Influence of patellar thickness on results of total current knee arthroplasty systems. J Bone Joint
knee arthroplasty: does a residual bony patellar Surg Am 2003; 85(Suppl 4): 115-22.
thickness of < 12 mm lead to poorer clinical out- 29. Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez
come and increased complication rates? J Arthro- DE. Rotational landmarks and sizing of the distal
plasty 2002; 17: 56-61. femur in total knee arthroplasty. Clin Orthop Relat
21. Kurosaka M, Yoshiya S, Mizuno K, Yamamoto T. Res 1996; 331: 35-46.
Maximizing flexion after total knee arthroplasty: 30. Gonzalez Della Valle A, Slullitel G, Piccaluga F,
the need and the pitfalls. J Arthroplasty 2002; 17: Salvati EA. The precision and usefulness of
59-62. preoperative planning for cemented and hybrid
22. Papagelopoulos PJ, Sim FH. Limited range of primary total hip arthroplasty. J Arthroplasty 2005;
motion after total knee arthroplasty: etiology, 20: 51-8.
treatment, and prognosis. Orthopedics 1997; 20: 31. Viceconti M, Lattanzi R, Antonietti B, Paderni S,
1061-5. Olmi R, Sudanese A, et al. CT-based surgical
23. Rand JA. The patellofemoral joint in total knee planning software improves the accuracy of total
arthroplasty. J Bone Joint Surg Am 1994; 76: 612-20. hip replacement preoperative planning. Med Eng
24. Reuben JD, McDonald CL, Woodard PL, Phys 2003; 25: 371-7.
2342 J Med Assoc Thai Vol. 90 No. 11 2007
การศึกษาความแม่นยำของการวัดขนาดข้อเข่าเทียมจากภาพถ่ายรังสีกอ่ นการผ่าตัด
อาศิส อุนนะนันทน์, มารุต อรุณากูร, อำนวย อุนนะนันทน์
วัตถุประสงค์: ในการผ่าตัดเปลี่ยนข้อเทียมนั้นศัลยแพทย์มักจะต้องวัดขนาดของข้อเทียมจากภาพถ่ายรังสีเพื่อใช้เป็น
ขนาดอ้างอิงระหว่างผ่าตัดแต่เนื่องจากกการศึกษาถึงความถูกต้องแม่นยำของการวัดขนาดข้อเข่าเทียมยังมีไม่มากนัก
ดังนั้นการศึกษาครั้งนี้จึงมีวัตถุประสงค์เพื่อที่จะหาความถูกต้องแม่นยำของการวัดขนาดข้อเข่าเทียมจากภาพถ่ายรังสี
ก่อนการผ่าตัด
วัสดุและวิธกี าร: ผูศ้ กึ ษาได้รวบรวมภาพถ่ายรังสีของข้อเข่าเทียมก่อนการผ่าตัด ในผูป้ ว่ ยจำนวน 98 ราย (113 เข่า)
ภาพถ่ายรังสีประกอบด้วยภาพถ่ายรังสีในแนวตรง และแนวข้างของข้อเข่าทำมุมตั้งฉากซึ่งกันและกัน ผู้ศึกษาได้ทำ
การวัดและประเมินขนาดของข้อเข่าเทียมที่น่าจะเหมาะสมกับผู้ป่วยรายนั้น ๆ โดยใช้ภาพจำลอง ข้อเข่าเทียมขนาด
ต่าง ๆ ซึง่ ได้ทำมาเพือ่ ให้เหมาะสมกับขนาดขยายของข้อเข่าผูป้ ว่ ยในภาพถ่ายรังสีนน้ั ๆ ขนาดทีว่ ดั ได้ทง้ั จากภาพรังสี
ในแนวตรงและแนวข้างได้ถูกบันทึกไว้ และนำมาเปรียบเทียบกับขนาดที่ใช้จริงระหว่างการผ่าตัด
ผลการศึกษา: จากภาพถ่ายรังสีของข้อเข่าเทียมจำนวน 113เข่า ความถูกต้องแม่นยำโดยรวม มีคา่ ประมาณ 50.4%
สำหรับข้อเข่าเทียมส่วน femur และ 55.8% สำหรับข้อเข่าเทียม ส่วน tibia โดยผู้ศึกษาพบว่าภาพถ่ายรังสีแนวตรง
มี ค วามถู ก ต้ อ งแม่ น ยำมากที ่ ส ุ ด ในการคาดคะเนขนาดของข้ อ เข่ า เที ย มส่ ว น tibia และภาพถ่ า ยรั ง สี แ นวข้ า ง
มีความถูกต้องแม่นยำมากที่สุดในการคาดคะเนขนาดของข้อเข่าเทียมส่วน femur
สรุป: เนื่องจากมีหลายปัจจัยที่มีผลต่อศัลยแพทย์ในการเลือกขนาดของข้อเข่าเทียมระหว่างผ่าตัดสำหรับผู้ป่วย
แต่ละราย ดั้งนั้นการวัดขนาดของข้อเข่าเทียมก่อนการผ่าตัดจากภาพถ่ายรังสีจึงเป็นแค่การคาดคะเนขนาดของข้อเข่า
เทียมที่จะใช้จริงอย่างคร่าว ๆ เท่านั้นโดยมีค่าความแม่นยำประมาณ 50%
J Med Assoc Thai Vol. 90 No. 11 2007 2343
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5783)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Final PPT BpoDocumento21 pagineFinal PPT BpoPradeepNessuna valutazione finora
- Tenor Ax Voip Multipath/Gateway Switch: Product GuideDocumento131 pagineTenor Ax Voip Multipath/Gateway Switch: Product GuideEdgar A CanizalezNessuna valutazione finora
- OpenBoard AM335xDocumento2 pagineOpenBoard AM335xvedanttaNessuna valutazione finora
- Electrical Motor Test Analysis ReportDocumento21 pagineElectrical Motor Test Analysis ReportHaitham YoussefNessuna valutazione finora
- Autel Maxisys Citroen v4.10 Coverage TableDocumento58 pagineAutel Maxisys Citroen v4.10 Coverage TableBeto HoffmannNessuna valutazione finora
- Formal vs Informal Communication TypesDocumento13 pagineFormal vs Informal Communication TypesOmar GalalNessuna valutazione finora
- Study On The Conduction of Electricity On Salty WaterDocumento2 pagineStudy On The Conduction of Electricity On Salty WaterJordan Paul DejesusNessuna valutazione finora
- Userspace Drivers in LinuxDocumento4 pagineUserspace Drivers in LinuxJeffi Edward100% (1)
- Sintercast Vs HardfacingDocumento21 pagineSintercast Vs Hardfacinganrulo75% (4)
- QCAI476 LfiltersDocumento11 pagineQCAI476 LfilterscivodulNessuna valutazione finora
- Centrifugal Vs Reciprocating Compressor - Turbomachinery Magazine PDFDocumento2 pagineCentrifugal Vs Reciprocating Compressor - Turbomachinery Magazine PDFReyes SanchezNessuna valutazione finora
- The Swedish Guide 2019Documento139 pagineThe Swedish Guide 2019Bahram BandeshahNessuna valutazione finora
- Custom Storage ClassesDocumento2 pagineCustom Storage ClassesSameer KumthekarNessuna valutazione finora
- PW-3 Part Design For Ultrasonic Welding (Single PGS) HRDocumento8 paginePW-3 Part Design For Ultrasonic Welding (Single PGS) HRAlba R.Nessuna valutazione finora
- NPX Series - Npx-25: Data SheetDocumento2 pagineNPX Series - Npx-25: Data SheetCesar AdrianzenNessuna valutazione finora
- Software Engineering Course OverviewDocumento2 pagineSoftware Engineering Course OverviewRajatKumarNessuna valutazione finora
- Rickmeier - Gear Pump R25-16 PDFDocumento48 pagineRickmeier - Gear Pump R25-16 PDFAdam Kowalski60% (5)
- Doosan Retrofit ServiceDocumento99 pagineDoosan Retrofit Servicestopless_dalian685Nessuna valutazione finora
- Chrysler Neon 99 - Immobiliser SystemDocumento4 pagineChrysler Neon 99 - Immobiliser SystemeephantomNessuna valutazione finora
- AW-Automatic Cone WinderDocumento2 pagineAW-Automatic Cone WindertexveerNessuna valutazione finora
- Essbase Studio User's Guide 11.1.2.3Documento406 pagineEssbase Studio User's Guide 11.1.2.3suchaiNessuna valutazione finora
- Resistance in The Fluid System PDFDocumento21 pagineResistance in The Fluid System PDFDyo MandeNessuna valutazione finora
- Applied Ergonomics: Nora Balfe, Sarah Sharples, John R. WilsonDocumento13 pagineApplied Ergonomics: Nora Balfe, Sarah Sharples, John R. WilsonDian Palupi RestuputriNessuna valutazione finora
- Army C-sUAS Systems AssessmentDocumento4 pagineArmy C-sUAS Systems AssessmentArthur WongNessuna valutazione finora
- Analysis of Non-Salient Pole Synchronous Generator Using Phasor DiagramsDocumento19 pagineAnalysis of Non-Salient Pole Synchronous Generator Using Phasor DiagramsNavitha RodriguesNessuna valutazione finora
- PSV Calculation Sheet APIDocumento10 paginePSV Calculation Sheet APIionutlaur86100% (2)
- Balai Tanah MakassarDocumento2 pagineBalai Tanah MakassarAstrid VioletNessuna valutazione finora
- H.No:-1148, Sector:-6, Housing Board, Dharuhera (Rewari) Mobile No.: - 9812816143, 8708015205Documento2 pagineH.No:-1148, Sector:-6, Housing Board, Dharuhera (Rewari) Mobile No.: - 9812816143, 8708015205parveen tanwarNessuna valutazione finora
- Richard Bandler's Guide to Harnessing HypnosisDocumento3 pagineRichard Bandler's Guide to Harnessing HypnosisChristy Mayo0% (1)
- Oval DPR Overall For NGN ProjectDocumento4 pagineOval DPR Overall For NGN ProjectRashmi Ranjan MohantyNessuna valutazione finora