Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Cytotoxic
Caricato da
Miguel Cuevas DolotCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Cytotoxic
Caricato da
Miguel Cuevas DolotCopyright:
Formati disponibili
CYTOTOXIC CHEMOTHERAPY 2014 -2015
Dr. Lim ONCOLOGY
4 types: Platinum analog
1. conventional chemotherapy – doxorubicin, paclitaxel, docetaxel For colon CA
2. Targeted agents – herceptin, bevacizumab, avastin
3. Hormonal therapies – tamoxifen S/E: prominently neurotoxic – most notorious
4. Biologic therapies – interferons, inteleukins
*it will not come out on the exam
2. ANTITUMOR ANTIBIOTICS AND TOPOISOMERASE INHIBITORS
Review: Cell cycle
DNA replication occurs during S phase MOA: They bind to DNA directly and can frequently undergo electron
There are 5 phases (G0, G1, G2, S, M) transfer reactions to generate free radicals in close proximity to DNA
The importance of cell cycle is that, different chemo drugs targets damage in the form of single strand breaks or cross links.
specific phases. They modify enzymes that regulate the capacity of DNA to unwind to
allow normal replication or transcriprion
CHEMOTHERAPEUTIC AGENTS USED FOR CANCER
Topoisomearse I – creates a single strand breaks that then rejoin
A. Phase non specific – agents which can act in any phase of the cell cycle following the passage of the other DNA strand through the break
B. Phase specific – agents which require the cell to be at a particular cell cycle
phase to cause greatest effect Toposiomerase II – creates a double strand breaks through which
*dose and side effects of the drugs will not be included in the exam, just another segment of DNA duplex passes before rejoining.
memorize the drugs under each classification DNA damage can occur in any cell cycle but cells tend to arrest In S Phase
(phase specific)
DIRECT DNA INTERACTING AGENTS
a. Doxorubicin
Formation of covalent DNA adducts: Alter DNA structure, replication and topoisomerase II
Powrerful vesicant with necrosis of tissue apparent 4-7 days after
1. ALKYLATING AGENTS (CELL CYCLE PHASE NON SPECIFIC) extravasation, should be administeresd into a rapidly flowing IV line
(NSS)
Metabolized in the liver (careful with liver problems)
MOA: they break down either spontaneously or after normal organ or
tumor cell metabolism to reactive intermediate that covalently modify
S/E: acute cardiotoxicity, atrial and ventricular dysrhythmias
bases in DNA, this leads to cross linkage of DNA strands or appearance of
breaks in DNA as a result of repair efforts.
If >550 mg/m2 – causes chronic cardiotoxicity (cardiomyopathy)
S/E: alopecia, myelosuppression(bone marrow suppression), gonadal
b. Etoposide
dysfunction(sterility), mucositis, pulmonary fibrosis
Prominent G2 phase arrest (phase specific)
Major toxicity: “second” neoplasm-leukemia
Binds directly to topoisomerase II and DNA in a reversible ternary
a. Cyclophosphamide (non phase specific) complex
Metabolized by 4-hydroxy-cyclophosphamide(active form) which Given slowly, if it is too fast, can cause hypotension
decomposes into an alkylating species as well as chloroacetaldehyde
and acrolein. S/E: acute leukemia – “second” malignancy
Acrolein – causes chemical cystitis, if severe, cystitis can be treated by
MESNA and Hydration.
b. Ifosphamide (non phase specific)
Cyclophosphamide analog also activated in the liver slowly
Requires coadministration of mesna to prevent bladder injury INDIRECT EFFECTORS OF DNA FUNCTION
(cystitis)
1. ANTIMETABOLITES
S/E: CNS-confusion, somnolence, psychosis
MOA: cause DNA damage indirectly, by mis-incorporation into DNA,
Treatment: Mesna, hydration abnormal timing or progression through DNA synthesis or altered
function of pyrimidine and purine biosynthetic enzymes
c. Cisplatin Acts on S Phase (phase specific)
MOA: efficient bifunctional interactor with DNA forming DNA forming
cross links or breakage a. Methotrexate
Requires administration of adequate hydration forced dieresis with Inhibits dihydrofolate reductase which regenerates reduced folates
furosemide and mannitol to prevent kidney damage from the oxidized folates. Without reduced folates, cells die a
Monitor creatinine level “thymine-less death”.
Cleared by the kidney
C/I :patients with kidney problems High dose of methotrexate with leukovorin is used for osteosarcoma
S/E: neurotoxicity, hearing loss, intensely emetogenic, myelosuppression, Renal toxicity is augmented by renal dysfunction and drugs like
hypomagnesemia which can lead to hypocalcemia, Reynauds salicylates, probenecid, NSAIDs.
phenomenon (chronic vascular toxicity) Sequestered in 3rd space(ascitis, effusion) collections causing
prolonged myelosuppression
d. Carboplatin Can cause crystals in real tubules, so to prevent this, give sodium
Less nephro-, oto- and neurotoxicity bicarbonate to alakalinize the urine
S/E: myelosuppression is more frequent
e. Oxiplatin
Et factum est ut amicis transcribit durum simul in unum!
Medicine vade
Page 1 of 3 yours truly, lj
CYTOTOXIC CHEMOTHERAPY 2014 -2015
Dr. Lim ONCOLOGY
b. Pemetrexed c. Lapatinib
Inhibits several enzymes including: No action in cell cycle, sa EGF receptors lang siya
(These are enzymes used in purine and pyrimidine synthesis) Used in Breast CA
Thymidilate synthase
Dihydrofolate reductase
Glycinamide ribonucleotide formyltransferase
Used in Lung CA and mesothelioma PROTEOSOME INHIBITOR “MIB”
a. Bortezomib
Inhibitor of the proteosome
c. 5-Fluouracil (5FU) Has activity in multiple myeloma and certain lymphomas
Metabolized in cells to 5’FdUMP which inhibits thymidilate
synthetase S/E: neuropathy, orthostatic hypotension, w/ or w/o hyponatremia,
reversible thrombocytopenia
2. ANTIMITOTIC AGENTS
M phase(phase specific)
HORMONAL AGENTS
a. Vincristine 1. Tamoxifen
Binds to tubulin dimer with the result that microtubules are 10 fold greater antitumor activity in breast CA whose tumors express
disaggregated. estrogen receptors.
Blocks M phase
Causes peripheral neurotoxicity in the form of glove and stocking S/E: thromboembolic phenomena, endometrial CA (matagal ang gamit)
neuropathy
b. Vinblastine 2. Aromatase
Similar to vincristine but more myelotoxic with more frequent Family of enzymes that catalyze the formation of estrogen in various
thrombocytopenia, mucositis, stomatitis. tissues including ovary, and peripheral adipose tissue and some tumor
cells
c. TAXANES 2 types of aromatase inhibitors:
Blocks S phase a. Irreversible – steroid analogues such as exemestane
Stabilize microtubules against depolymerization b. reversible – such as anastrozole, letrozole
Microtubules function abnormally and are not able to undergo the
normal dynamic changes of microtubule structure and function
3. Anastrozole
c.1 paclitaxel Superior to tamoxifen in the adjuvant treatment of breast CA in
Requires use of Cremophor-containing vehicle that can cause postmenopausal patients with estrogen receptor positive tumors.
hypersensitivity reactions-premedicate with dexamethasone and *if premenopausal ang patient use tamoxifen
diphenhydramine
S/E: increase risk in osteoporosis (monitor bone mineral density)
S/E: hypersensitivity reactions(patient turning violet), LHRH (leutenizing hormone releasing hormone) agonist
myelosuppression, neurotoxicity, cardiac rhythm disturbances Prostate CA – treated with androgen deprivation
Diethylstilbestrol (DES) – acting as an estrogen at the level of the
hypothalamus to downregulate LH.
c.2 docetaxel
Requires polysorbate as a vehicle Treatment:
Cause fluid retention in addition to hypersensitivity reactions 1. Orchiectomy – equally effective as moderate-dose DES inducing
Give steroids and diuretics to prevent fluid retention a response of 80% (best treatment) of previously untreated
patients with prostate CA but w/o the prominent cardiovascular
S/E: myelosuppression and neuropathy side effects of DES
*1st option orchiectomy, 2nd option leuprolide
2. Leuprolide and goserelin (LHRH agonist) – Tonic stimulation of
the LHRH receptor with the loss of its normal pulsatile activation
resulting in decreased output of LH in the anterior pituitary.
TYROSINE KINASE INHIBITORS “TINIB” *primary hormonal manipulation in prostate cancer, one can choose
Acts on EGF receptors orchiectomy or leuprolide, but not both.
a. Imatinib
Targets ATP binding site of the p210 protein tyrosine kinase that is
ANDROGEN RECEPTOR BLOCKER
formed as a result in chromosome 9,22 translocation producing CML
1. flutamide/ bicalutamide
*EGF antagonists – gefitinib, erlotinib, lapatinib Uncertain additional benefit in extending overall response duration.
b. Gefitinib and erlotinib
Used in lung CA (small cell)
EGF antagonist that act at the ATP binding site of EGF receptor
tyrosine kinase
Et factum est ut amicis transcribit durum simul in unum!
Medicine vade
Page 2 of 3 yours truly, lj
CYTOTOXIC CHEMOTHERAPY 2014 -2015
Dr. Lim ONCOLOGY
CLASSIFICATIONS OF DRUGS 6. Tyrosine kinase inhibitors
1. Alkylators “TINIBS”
Cyclophosphamide Imatinib
Mechlorethamine Gefitinib
Chorambucil Erlotinib
Melphalan Dasatinib
Carmustine (BCNU) Sorafenib
Lomustine (CCNU) Sunitinib
Ifosphamide
Procarbazine
Dacarbizine (DTIC) 7. Protease inhibitors
Temozolimide Bortezomib
Altretamine (formerly hexamethylmelamine)
Cisplatin
Carboplatin 8. Histone deacetylase inhibitors
Oxaliplatin Vorinostat
Romidepsin
2. Antitumor antibiotics and topoisomerase poisons
Bleomycin 9. mTor inhibitors
Actinomycin D Temsirolimus
Etoposide Everolimus’
Topotetan
Irinotecan
Doxorubicin and Daunorubicin 10. Miscellaneous
Idarubicin Arsenic trioxide
Epirubicin
Mitoxantrone
3. Antimetabolites
Deoxycoformycin
6-mercaptopurine
Azathioprine
2-chlorodeoxyadeosine
Hydroxyurea
Methotrexate
5 FU(5 fluouracil)
Capecitabine
Cytosine arabinoside
Azacytidine
Gemcitabine
Fludarabine phosphate
Asparaginase
Premetexed
4. Antimitotic agents
Vincristine
Vinblastine
Vinorelbine
Paclitaxel
Docetaxel
Estramustine phosphate
Nab-pacliatxel
Ixabepilone
5. Molecularly targeted agents
A. Retinoids
o Tretinoin
o Bexarotene
B. targeted toxins
o Denileukin diftitox
Et factum est ut amicis transcribit durum simul in unum!
Medicine vade
Page 3 of 3 yours truly, lj
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Mind Maps PDFDocumento208 pagineMind Maps PDFAnonymous 9uu04elNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- English Reading Kit Level 1: Pupil's Assessment ManualDocumento15 pagineEnglish Reading Kit Level 1: Pupil's Assessment ManualGretylle Quicoy100% (1)
- Low Intermediate Korean Vocabulary and GrammarDocumento10 pagineLow Intermediate Korean Vocabulary and GrammarTuong Van Nguyen100% (3)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Active Listening HANDOUT PDFDocumento26 pagineActive Listening HANDOUT PDFMiguel Cuevas DolotNessuna valutazione finora
- A Book of Beasts PDFDocumento32 pagineA Book of Beasts PDFbrad drac100% (2)
- Fouts Federal LawsuitDocumento28 pagineFouts Federal LawsuitWXYZ-TV DetroitNessuna valutazione finora
- Anesthesia Pocket Cards 7 18 18Documento6 pagineAnesthesia Pocket Cards 7 18 18Miguel Cuevas DolotNessuna valutazione finora
- History Taking ExaminationDocumento7 pagineHistory Taking ExaminationIndunil AnuruddhikaNessuna valutazione finora
- Castigliano's 2nd TheoremDocumento29 pagineCastigliano's 2nd TheoremMiddle East100% (4)
- Community-Acquired Pneumonia - CPG 2016Documento26 pagineCommunity-Acquired Pneumonia - CPG 2016Jamie SebastianNessuna valutazione finora
- Click Here For Download: (PDF) HerDocumento2 pagineClick Here For Download: (PDF) HerJerahm Flancia0% (1)
- The Saving Cross of The Suffering Christ: Benjamin R. WilsonDocumento228 pagineThe Saving Cross of The Suffering Christ: Benjamin R. WilsonTri YaniNessuna valutazione finora
- InvestMemo TemplateDocumento6 pagineInvestMemo TemplatealiranagNessuna valutazione finora
- Effectiveness of Transdermal MagnesiumDocumento2 pagineEffectiveness of Transdermal MagnesiumMiguel Cuevas Dolot100% (1)
- Covid 19 CPR 7 RulesDocumento21 pagineCovid 19 CPR 7 RulesMiguel Cuevas DolotNessuna valutazione finora
- How Can Patients Visitors Help - May18Documento2 pagineHow Can Patients Visitors Help - May18Miguel Cuevas DolotNessuna valutazione finora
- PSB 368Documento6 paginePSB 368Miguel Cuevas DolotNessuna valutazione finora
- Covid 19 CPR 7 RulesDocumento21 pagineCovid 19 CPR 7 RulesMiguel Cuevas DolotNessuna valutazione finora
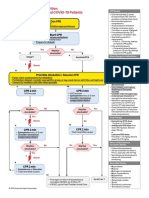
- ACLS Cardiac Arrest Algorithm For Suspected or Confirmed COVID-19 PatientsDocumento1 paginaACLS Cardiac Arrest Algorithm For Suspected or Confirmed COVID-19 PatientsMariuxi Tatiana ChocoNessuna valutazione finora
- (MED) COVID-19 Trans V. 2.0Documento6 pagine(MED) COVID-19 Trans V. 2.0Isabel VinasNessuna valutazione finora
- Covid 19 PDFDocumento18 pagineCovid 19 PDFMiguel Cuevas DolotNessuna valutazione finora
- Physical Examination in ENT: Ussana Promyothin, MDDocumento60 paginePhysical Examination in ENT: Ussana Promyothin, MDMiguel Cuevas DolotNessuna valutazione finora
- Clinical Examination of The Ear, Nose and Throat: Dave Pothier ST Mary's 2003Documento30 pagineClinical Examination of The Ear, Nose and Throat: Dave Pothier ST Mary's 2003Ekambaram TrmNessuna valutazione finora
- Physical Examination in ENT: Ussana Promyothin, MDDocumento60 paginePhysical Examination in ENT: Ussana Promyothin, MDMiguel Cuevas DolotNessuna valutazione finora
- Physical Assessment: Ear, Nose, Mouth, and ThroatDocumento59 paginePhysical Assessment: Ear, Nose, Mouth, and ThroatMiguel Cuevas DolotNessuna valutazione finora
- Vertigo Gail Ishiyama 1 13 10Documento40 pagineVertigo Gail Ishiyama 1 13 10Myname Rama LienNessuna valutazione finora
- Pedia Tickler Update 2017Documento2 paginePedia Tickler Update 2017Tani BokNessuna valutazione finora
- Cook Book (Filipino) 13 PDFDocumento23 pagineCook Book (Filipino) 13 PDFAdina AnghelNessuna valutazione finora
- Drug IndexDocumento2 pagineDrug IndexMiguel Cuevas DolotNessuna valutazione finora
- Nocturnals Physiology 2018Documento14 pagineNocturnals Physiology 2018Miguel Cuevas DolotNessuna valutazione finora
- Benign Paroxysmal Positional Vertigo: Waseem WatadDocumento37 pagineBenign Paroxysmal Positional Vertigo: Waseem WatadnoviNessuna valutazione finora
- A Case-Control Study of The Association of Diet and Obesity With Gout in Taiwan PDFDocumento12 pagineA Case-Control Study of The Association of Diet and Obesity With Gout in Taiwan PDFMiguel Cuevas DolotNessuna valutazione finora
- A Case-Control Study of The Association of Diet and Obesity With Gout in Taiwan PDFDocumento12 pagineA Case-Control Study of The Association of Diet and Obesity With Gout in Taiwan PDFMiguel Cuevas DolotNessuna valutazione finora
- Clinical AbstractDocumento4 pagineClinical AbstractMiguel Cuevas DolotNessuna valutazione finora
- TCVS - Cardiac Surgery Part 2 Dr. de AsisDocumento8 pagineTCVS - Cardiac Surgery Part 2 Dr. de AsisMiguel Cuevas DolotNessuna valutazione finora
- Neurologic ExamDocumento1 paginaNeurologic ExamMiguel Cuevas DolotNessuna valutazione finora
- HEMAreviewDocumento3 pagineHEMAreviewMiguel Cuevas DolotNessuna valutazione finora
- Kerosene PDFDocumento31 pagineKerosene PDFRudyMLanaNessuna valutazione finora
- SunEdison Pancho Perez Complaint As FiledDocumento47 pagineSunEdison Pancho Perez Complaint As FiledLizHoffmanNessuna valutazione finora
- 1.3 Digital Communication and AnalogueDocumento6 pagine1.3 Digital Communication and AnaloguenvjnjNessuna valutazione finora
- Iver Brevik, Olesya Gorbunova and Diego Saez-Gomez - Casimir Effects Near The Big Rip Singularity in Viscous CosmologyDocumento7 pagineIver Brevik, Olesya Gorbunova and Diego Saez-Gomez - Casimir Effects Near The Big Rip Singularity in Viscous CosmologyDex30KMNessuna valutazione finora
- Knut - Fleur de LisDocumento10 pagineKnut - Fleur de LisoierulNessuna valutazione finora
- Yield of Concrete - tcm45-341215 PDFDocumento3 pagineYield of Concrete - tcm45-341215 PDFBijaya RaulaNessuna valutazione finora
- Info Cad Engb FestoDocumento14 pagineInfo Cad Engb FestoBayu RahmansyahNessuna valutazione finora
- Oral Communication in Context Quarter 2: Week 1 Module in Communicative Strategies 1Documento10 pagineOral Communication in Context Quarter 2: Week 1 Module in Communicative Strategies 1Agatha Sigrid GonzalesNessuna valutazione finora
- Speakout Language BankDocumento7 pagineSpeakout Language BankСаша БулуєвNessuna valutazione finora
- The Trials of The Rizal Bill (Gist)Documento2 pagineThe Trials of The Rizal Bill (Gist)CJ IbaleNessuna valutazione finora
- Correct Translation of 2-16Documento19 pagineCorrect Translation of 2-16muhammad_zubair708110Nessuna valutazione finora
- مذكرة التأسيس الرائعة لغة انجليزية للمبتدئين?Documento21 pagineمذكرة التأسيس الرائعة لغة انجليزية للمبتدئين?Manar SwaidanNessuna valutazione finora
- Second Unit Test 2022: Radha Madhav Public School BareillyDocumento4 pagineSecond Unit Test 2022: Radha Madhav Public School BareillyRaghav AgarwalNessuna valutazione finora
- Description of Medical Specialties Residents With High Levels of Workplace Harassment Psychological Terror in A Reference HospitalDocumento16 pagineDescription of Medical Specialties Residents With High Levels of Workplace Harassment Psychological Terror in A Reference HospitalVictor EnriquezNessuna valutazione finora
- Sales Purchases Returns Day BookDocumento8 pagineSales Purchases Returns Day BookAung Zaw HtweNessuna valutazione finora
- Akhbar Al Fuqaha Narration - Non Raful Yadayn From Ibn Umar - Reply To Zubair Ali ZaiDocumento15 pagineAkhbar Al Fuqaha Narration - Non Raful Yadayn From Ibn Umar - Reply To Zubair Ali ZaiAbdullah YusufNessuna valutazione finora
- Sec 25 HmaDocumento3 pagineSec 25 HmaMukul BajajNessuna valutazione finora
- Physical Education 10 WEEK 2Documento10 paginePhysical Education 10 WEEK 2Israel MarquezNessuna valutazione finora
- History RizalDocumento6 pagineHistory RizalIrvin LevieNessuna valutazione finora
- An Aging Game Simulation Activity For Al PDFDocumento13 pagineAn Aging Game Simulation Activity For Al PDFramzan aliNessuna valutazione finora
- Shipping Operation Diagram: 120' (EVERY 30')Documento10 pagineShipping Operation Diagram: 120' (EVERY 30')Hafid AriNessuna valutazione finora
- Merger of Bank of Karad Ltd. (BOK) With Bank of India (BOI)Documento17 pagineMerger of Bank of Karad Ltd. (BOK) With Bank of India (BOI)Alexander DeckerNessuna valutazione finora