Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Three Axes in Sniffing Position
Caricato da
Rose Ann Tambanillo AlvarezTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Three Axes in Sniffing Position
Caricato da
Rose Ann Tambanillo AlvarezCopyright:
Formati disponibili
1964
CORRESPONDENCE
Anesthesiology
1999; 91:1964 –5
© 1999 American Society of Anesthesiologists, Inc.
Lippincott Williams & Wilkins, Inc.
The Three Axis Alignment Theory and the “Sniffing Position”:
Perpetuation of an Anatomic Myth?
To the Editor:—A review of the classic anesthesiology literature
reveals a common thread in the instructions for direct laryngos-
copy: To successfully visualize the larynx, one must align three
(oral, laryngeal, and pharyngeal) anatomic axes.1–7 Placing a patient
in the “sniffing position” is the accepted maneuver for aligning
these axes.
Recently, we evaluated a radiograph obtained during intubation in
the sniffing position, drew lines along the axes (fig. 1), and did not
observe this alignment. We then reviewed the literature to understand
the origin of this concept. The sniffing position has been credited to
Chevalier Jackson in 1913, although he did not use this terminology or
demonstrate alignment of the axes diagramatically. He simply sug-
gested that the patient be placed on a pillow in a natural position with
the head extended.8 He went on to suggest that, in fact, the pillow
might be removed, the thumbs placed on the forehead of the patient,
and the forehead vigorously forced downward and backward, causing
an anterior movement of the skull on the atlas and throwing the
Fig. 1. Intubation in sniffing position. LA 5 laryngeal axis; MA 5
cervical vertebrae forward.
mouth axis; PA 5 pharyngeal axis.
After this proposal by Jackson, numerous authors offered their
modifications of the technique. However, the first (only?) authors to
study the problem experimentally were Bannister and MacBeth,9 Stephen W. Borron, M.D., M.S.
whose frequently cited 1944 Lancet article graphically demon- Visiting Researcher
strates the alignment of the three axes by use of an added pillow Toxicological Intensive Care Unit
beneath the occiput, thus flexing the neck.9 The authors then INSERM U-26
propose that straightening the right angle formed by the axis of the Hôpital Fernand Widal
mouth and the pharyngolaryngeal axis requires extension of the University Paris VII
head on the atlantooccipital joint. They support their view with a Paris, France
series of drawings and radiographs. Although the authors’ drawings Frédéric Lapostolle, M.D.
illustrate plainly that the axes may be brought into complete align- Assistant Professor
ment, close examination of the radiographs shows that the drawing Department of Anesthesiology
did not coincide with the radiograph. Whereas the hard palate is Hôpital Avicenne, University Paris XIII
aligned with the larynx in the drawing, the angle of the larynx to the Paris, France
hard palate in the radiograph is roughly 36°. If one compares Claude Lapandry, M.D.
radiographs in the article, it becomes apparent that the laryngo- Assistant Professor
scope shown in one radiograph (patient in sniffing position) is not Department of Anesthesiology
in the mouth. Otherwise this patient would be missing all the upper Hôpital Avicenne, University Paris XIII
incisors. Perhaps this is what was referred to previously in the Paris, France
article as “cooking” a diagram. In spite of this, the “three-axes rule”
became reality.
It would appear to us that, although the sniffing position may References
provide the best laryngeal view, the explanation of the benefit of the
sniffing position based on alignment of the three axes is an error 1. Stoelting RK: Endotracheal intubation, Anesthesia. Edited by
perpetuated since 1944 that deserves reexamination. Miller RD. New York, Churchill Livingstone, 1986, pp 523–32
2. Finucane BT, Santora AH: Techniques of intubation, Airway Man-
Frédéric Adnet, M.D., Ph.D. agement. Edited by Finucane BT, Santora AH. St. Louis, Mosby, 1996,
Assistant Professor pp 161– 86
Department of Anesthesiology 3. Société Franĉaise d’Anesthésie et de Réanimation: Intubation dif-
Hôpital Avicenne, University Paris XIII ficile. Ann Fr Anesth Réanim 1996; 15:207–14
Paris, France 4. Benumof JL: Conventional (laryngosocpic) orotracheal and naso-
frederic.adnet@avc.ap-hop-paris.fr tracheal intubation (single-lumen tube), Airway Management, Princi-
Anesthesiology, V 91, No 6, Dec 1999
1965
CORRESPONDENCE
ples and Practices. Edited by Benumof JL. St Louis, Mosby, 1996, pp Management. Edited by Dailey RH, Simon B, Young GP, Stewart RD. St.
261–76 Louis, Mosby–Year Book, 1992, pp 73–91
5. Murrin KR: Causes of difficult intubation and intubation proce- 8. Jackson C: The technique of insertion of intratracheal insufflation
dure, Difficulties in Tracheal Intubation. Edited by Latto IP, Vaughan tubes. Surg Gynecol Obstet 1913; 17:507–9
RS. London, WB Saunders Company, 1997, pp 89 –106 9. Bannister FB, Macbeth RG: Direct laryngoscopy and tracheal
6. Schwartz DE, Wiener-Kronish JP: Management of difficult airway. intubation. Lancet 1944; ii:651– 4
Clin Chest Med 1991; 12:483–95
7. Scott J: Oral endotracheal intubation, The Airway: Emergency (Accepted for publication June 22, 1999.)
Anesthesiology
1999; 91:1965– 6
© 1999 American Society of Anesthesiologists, Inc.
Lippincott Williams & Wilkins, Inc.
Attempted Placement of a Thoracic Epidural Catheter via the
Caudal Route in a Newborn
To the Editor:—Inadvertent placement of an epidural catheter in the sure was seen after a test dose of 0.3 ml lidocaine, 1.5%, with epineph-
presacral area via the caudal route is described in a full-term infant rine (1:200,000). The epidural catheter was infused with 0.05% bupiv-
who underwent repair of tracheoesophageal fistula. acaine and fentanyl (1 mg/ml) at 1 ml/h. The patient was breathing
A 3.1-kg full-term boy infant with a prenatal diagnosis of tracheo- spontaneously and underwent ventilation at arrival to the intensive
esophageal fistula with esophageal atresia and left pulmonary agenesis care unit. Fentanyl was removed from the epidural infusion and the
presented at birth with respiratory distress. Routine monitors were analgesia was adequate. The patient was weaned from the ventilator
placed in the operating room, and after preoxygenation an awake and the trachea was extubated in the next 24 h. The epidural catheter
tracheal intubation was performed. Anesthesia was maintained with was removed on the fourth postoperative day.
isoflurane, oxygen, and air with the infant breathing spontaneously.
Chest and abdominal radiograms showed no vertebral anomalies. An
epidural catheter was inserted in the caudal space using a sterile
technique to facilitate perioperative pain management and early tra-
cheal extubation. An 18-gauge angiocatheter was placed in the caudal
space and a 20-gauge polyamide epidural catheter was advanced into
the epidural space via the angiocatheter. No cerebrospinal fluid or
blood was noted. The catheter was advanced with ease to the antici-
pated length for mid thoracic placement. No tachycardia, dysrhythmia,
or increase in blood pressure was recorded after a test dose of 0.3 ml
lidocaine, 1.5%, with epinephrine (1:200,000). An open gastrostomy
was then performed. A loading dose of 1.5 ml bupivacaine solution,
0.125%, was given via the epidural catheter. This was followed by a
continuous infusion of 0.05% bupivacaine and fentanyl (1 mg/ml) at 1
ml/h. The end-tidal concentration of isoflurane was kept constant
during the gastrostomy, and no changes in the patient’s blood pressure
and heart rate were noted. Routine epidurography with 0.5 ml contrast
(iohexol, 180 mg/ml) showed the catheter coiled in the presacral
space (fig. 1). The epidural infusion was discontinued.
The patient was then positioned for a right posterolateral thoracot-
omy. The fistula was ligated and divided, and the esophageal anasto-
mosis was performed without complication. The caudally placed cath-
eter was removed and replaced at the end of surgery. During a sterile
technique, an 18-gauge Crawford epidural needle was placed in the
caudal space. No blood or cerebrospinal fluid was noted. A 20-gauge
polyamide epidural catheter was easily advanced to a premeasured
distance from the caudal space to the mid thoracic area. An epiduro-
gram (0.5 ml iohexol, 180 mg/ml) confirmed the tip of the catheter at Fig. 1. Pelvic radiogram in the lateral view showing contrast
the mid thoracic level and absorption of the contrast from the presacral medium in the presacral space (arrow) and a coiled epidural
space (fig. 2). No tachycardia, dysrhythmia, or increase in blood pres- catheter.
Anesthesiology, V 91, No 6, Dec 1999
Potrebbero piacerti anche
- From Control of Airway and Breathing To Cardiopulmonary-Cerebral ResuscitationDocumento3 pagineFrom Control of Airway and Breathing To Cardiopulmonary-Cerebral ResuscitationCaesar Huseindy DaminggoNessuna valutazione finora
- HerniaDocumento3 pagineHerniaMonica Imelda Krist GultomNessuna valutazione finora
- Laryngoscopy - Its Past and Future: Canadian Anaesthetists? Society Journal June 2004Documento6 pagineLaryngoscopy - Its Past and Future: Canadian Anaesthetists? Society Journal June 2004razihaikalNessuna valutazione finora
- Recurrent Postoperative Laryngospasm ManagementDocumento2 pagineRecurrent Postoperative Laryngospasm Managementbalab2311Nessuna valutazione finora
- Anaesthetic Management of Pulmonary Hydatid CystDocumento6 pagineAnaesthetic Management of Pulmonary Hydatid CystPrabakaran ParameswaranNessuna valutazione finora
- 0310057x150430s103 PDFDocumento8 pagine0310057x150430s103 PDFAwker FurtNessuna valutazione finora
- Speaking ValveDocumento6 pagineSpeaking ValveJonssito Griffin Iglesias PerezNessuna valutazione finora
- 401-Article Text-778-1-10-20190128 PDFDocumento3 pagine401-Article Text-778-1-10-20190128 PDFCut Nanda FitriNessuna valutazione finora
- 2003 A Review of Surgical Treatment For Obstructive Sleep Apnoea Hypopnoea SyndromeDocumento6 pagine2003 A Review of Surgical Treatment For Obstructive Sleep Apnoea Hypopnoea SyndromeRabia MekamchaNessuna valutazione finora
- History of Anaesthesia Oropharyngeal and Nasopharyngeal Airways: I (1880-1995)Documento7 pagineHistory of Anaesthesia Oropharyngeal and Nasopharyngeal Airways: I (1880-1995)Lucille IlaganNessuna valutazione finora
- The History of Sleep Surgery: Kathleen Yaremchuk Laura Garcia-RodriguezDocumento5 pagineThe History of Sleep Surgery: Kathleen Yaremchuk Laura Garcia-RodriguezRehab BassamNessuna valutazione finora
- Ultrasound Findings of Appendico-Cecal Invagination: A Case Report and Literature ReviewDocumento6 pagineUltrasound Findings of Appendico-Cecal Invagination: A Case Report and Literature Reviewlailan maghfirahNessuna valutazione finora
- Sellick 1961Documento3 pagineSellick 1961BigbobNessuna valutazione finora
- Awake IntubationDocumento35 pagineAwake IntubationEbeneser SitepuNessuna valutazione finora
- 1 s2.0 S1875459713001161 MainDocumento4 pagine1 s2.0 S1875459713001161 Mainaieyha hamkaNessuna valutazione finora
- Utility of Lung UltrasoundDocumento3 pagineUtility of Lung UltrasoundMario Henrique Dutra de SouzaNessuna valutazione finora
- Anatomy Samplex 2Documento30 pagineAnatomy Samplex 2Jo Anne80% (10)
- 2008 Chest - The Blue ProtocolDocumento9 pagine2008 Chest - The Blue Protocoleduardo0% (1)
- PAPER (ENG) - Effect of A Tracheostomy Speaking Valve On Breathing-Swallowing InteractionDocumento7 paginePAPER (ENG) - Effect of A Tracheostomy Speaking Valve On Breathing-Swallowing InteractionAldo Hip NaranjoNessuna valutazione finora
- Nazari An 2018Documento16 pagineNazari An 2018Zakia DrajatNessuna valutazione finora
- Reconstruction of The Trachea: Experience in 100 ConsecutiveDocumento13 pagineReconstruction of The Trachea: Experience in 100 ConsecutiveNda MiraNessuna valutazione finora
- The British Journal O F SurgeryDocumento2 pagineThe British Journal O F SurgerySAILINGAREDDY MKNessuna valutazione finora
- 1099-0496 (200007) 30 1 1 Aid-Ppul1 3.0.co 2-qDocumento2 pagine1099-0496 (200007) 30 1 1 Aid-Ppul1 3.0.co 2-qLibre Joel IanNessuna valutazione finora
- Tippett-Siebens1991 Article UsingVentilatorsForSpeakingAndDocumento6 pagineTippett-Siebens1991 Article UsingVentilatorsForSpeakingAndRodrigo Navia ValenzuelaNessuna valutazione finora
- Heart MummorsDocumento2 pagineHeart MummorsHrabia DookuNessuna valutazione finora
- Corpus Alienum PneumothoraxDocumento3 pagineCorpus Alienum PneumothoraxPratita Jati PermatasariNessuna valutazione finora
- Respiratory Medicine Case Reports: Lauren A. Sharan, Thea P. Price, Boyd Hehn, David Manoff, Scott W. CowanDocumento4 pagineRespiratory Medicine Case Reports: Lauren A. Sharan, Thea P. Price, Boyd Hehn, David Manoff, Scott W. CowanJha BhoenkNessuna valutazione finora
- Pisa Nu 2009Documento6 paginePisa Nu 2009vinicius.alvarez3Nessuna valutazione finora
- Endoscopic Third VentriculostomyDocumento4 pagineEndoscopic Third VentriculostomyMohamed Farouk El-FaresyNessuna valutazione finora
- UNAS 2022 Juni (Ke-62) Larfar 1-23, Al-Im 1-4Documento51 pagineUNAS 2022 Juni (Ke-62) Larfar 1-23, Al-Im 1-4abubakar rizviNessuna valutazione finora
- Anal FistulasDocumento9 pagineAnal FistulasikeernawatiNessuna valutazione finora
- A Intubarion DownloadDocumento8 pagineA Intubarion DownloadDiegoNessuna valutazione finora
- Fibreoptic Intubation in Airway Management: A Review ArticleDocumento9 pagineFibreoptic Intubation in Airway Management: A Review ArticleFadilah SorayaNessuna valutazione finora
- Tissue-Preserving Techniques for Tonsillectomy and PharyngoplastyDocumento6 pagineTissue-Preserving Techniques for Tonsillectomy and Pharyngoplastylaljadeff12Nessuna valutazione finora
- Comparative Study Between Open Fistulectomy and Ligation of Intersphincteric Fistulas Tract (LIFT) Procedure For Uncomplicated Perianal FistulaDocumento7 pagineComparative Study Between Open Fistulectomy and Ligation of Intersphincteric Fistulas Tract (LIFT) Procedure For Uncomplicated Perianal FistulaInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- AAS Historia Primera UCI 2003Documento6 pagineAAS Historia Primera UCI 2003Diego Álvarez GrandaNessuna valutazione finora
- Gynecologic surgery techniques for general surgeonsDocumento13 pagineGynecologic surgery techniques for general surgeonsmauricio ricardoNessuna valutazione finora
- Respirology Case ReportsDocumento5 pagineRespirology Case Reportsশরীফ উল কবীরNessuna valutazione finora
- HidrosefalusDocumento10 pagineHidrosefalusNelly AstikaNessuna valutazione finora
- Bilateral Nasolabial Cyst MarcoviceanuDocumento4 pagineBilateral Nasolabial Cyst MarcoviceanubamsusiloNessuna valutazione finora
- The Erector Spinae Plane Block: A Review of Current EvidenceDocumento11 pagineThe Erector Spinae Plane Block: A Review of Current Evidencetnim.dsNessuna valutazione finora
- Oleson2014-Auricle Accupuncture NomenclatureDocumento15 pagineOleson2014-Auricle Accupuncture NomenclaturebillNessuna valutazione finora
- Barium Aspiration in An Infant: A Case Report and Review of ManagementDocumento4 pagineBarium Aspiration in An Infant: A Case Report and Review of Managementmedicina internaNessuna valutazione finora
- Life-Saving Esophageal Intubation in Neonate With Undiagnosed Tracheal Agenesis (A & A Case Reports, Vol. 9, Issue 1) (2017)Documento4 pagineLife-Saving Esophageal Intubation in Neonate With Undiagnosed Tracheal Agenesis (A & A Case Reports, Vol. 9, Issue 1) (2017)Mahdi WashahaNessuna valutazione finora
- Ambu BagDocumento10 pagineAmbu BagsaifudinNessuna valutazione finora
- 2010 Article 46Documento2 pagine2010 Article 46PaolaNessuna valutazione finora
- Infection Control Practices by The.46Documento1 paginaInfection Control Practices by The.46rosangelNessuna valutazione finora
- Influence of The Cuff Pressure On The Swallowing Reflex in Tracheostomized Intensive Care Unit PatientsDocumento6 pagineInfluence of The Cuff Pressure On The Swallowing Reflex in Tracheostomized Intensive Care Unit PatientscamiladelgadomNessuna valutazione finora
- Ecografia Pulmonar NeonatalDocumento12 pagineEcografia Pulmonar NeonatalJorge CastroNessuna valutazione finora
- Ecografia Pulmonar. Ficción o Realidad PDFDocumento9 pagineEcografia Pulmonar. Ficción o Realidad PDFAmilcar RomeroNessuna valutazione finora
- US Pulmón para Manejo de Atelectasias PerioperatoriasDocumento11 pagineUS Pulmón para Manejo de Atelectasias PerioperatoriasJURAGOMANessuna valutazione finora
- Extremities,: Abdomen Segment. ApparentDocumento5 pagineExtremities,: Abdomen Segment. ApparentSilvia RozaNessuna valutazione finora
- Archives 50 E2021119Documento3 pagineArchives 50 E2021119solxmar tmNessuna valutazione finora
- Congenital hiatal hernia repair in catDocumento7 pagineCongenital hiatal hernia repair in catBambang Wisnu LaksonoNessuna valutazione finora
- Atresia of The Foramina of Luschka and Magendie: The Dandy-Walker CystDocumento15 pagineAtresia of The Foramina of Luschka and Magendie: The Dandy-Walker CystAlexandra ChirvasituNessuna valutazione finora
- Physiology and histology of the Cubomedusæ including Dr. F.S. Conant's notes on the physiologyDa EverandPhysiology and histology of the Cubomedusæ including Dr. F.S. Conant's notes on the physiologyNessuna valutazione finora
- Penicillins and CephalosporinsDa EverandPenicillins and CephalosporinsRobert B. MorinNessuna valutazione finora
- The English Center Articulation AgreementDocumento9 pagineThe English Center Articulation AgreementJose CabreraNessuna valutazione finora
- Pakage PAU (Fruits)Documento70 paginePakage PAU (Fruits)Gary Bhullar57% (7)
- BSHM 23 ReviewerDocumento8 pagineBSHM 23 ReviewerTrixie Mae MuncadaNessuna valutazione finora
- Chapter 9 Lease DecisionsDocumento51 pagineChapter 9 Lease Decisionsceoji25% (4)
- Test Engleza 8Documento6 pagineTest Engleza 8Adriana SanduNessuna valutazione finora
- AP Research Survival Guide - RevisedDocumento58 pagineAP Research Survival Guide - RevisedBadrEddin IsmailNessuna valutazione finora
- AE3212 I 2 Static Stab 1 AcDocumento23 pagineAE3212 I 2 Static Stab 1 AcRadj90Nessuna valutazione finora
- Microscopes Open Up An Entire World That You Can't See With The Naked EyeDocumento4 pagineMicroscopes Open Up An Entire World That You Can't See With The Naked EyeLouie Jane EleccionNessuna valutazione finora
- Present Perfect.Documento1 paginaPresent Perfect.Leidy DiazNessuna valutazione finora
- Gild PitchDocumento19 pagineGild PitchtejabharathNessuna valutazione finora
- Ferain Et Al, 2016 - The Fatty Acid Profile of Rainbow Trout Liver Cells Modulates Their Tolerance To Methylmercury and CadmiumDocumento12 pagineFerain Et Al, 2016 - The Fatty Acid Profile of Rainbow Trout Liver Cells Modulates Their Tolerance To Methylmercury and Cadmiumarthur5927Nessuna valutazione finora
- Asset Valuation: Debt Investments: Analysis and Valuation: 1 2 N M 1 2 N MDocumento23 pagineAsset Valuation: Debt Investments: Analysis and Valuation: 1 2 N M 1 2 N MSirSmirkNessuna valutazione finora
- ACCA P1 Governance, Risk, and Ethics - Revision QuestionsDocumento2 pagineACCA P1 Governance, Risk, and Ethics - Revision QuestionsChan Tsu ChongNessuna valutazione finora
- Mod. 34 Classic Compact T06Documento4 pagineMod. 34 Classic Compact T06Jaime Li AliNessuna valutazione finora
- 30-99!90!1619-Rev.0-Method Statement For Pipeline WeldingDocumento21 pagine30-99!90!1619-Rev.0-Method Statement For Pipeline WeldingkilioNessuna valutazione finora
- Vortex: Opencl Compatible Risc-V Gpgpu: Fares Elsabbagh Blaise Tine Priyadarshini Roshan Ethan Lyons Euna KimDocumento7 pagineVortex: Opencl Compatible Risc-V Gpgpu: Fares Elsabbagh Blaise Tine Priyadarshini Roshan Ethan Lyons Euna KimhiraNessuna valutazione finora
- BA50BCODocumento6 pagineBA50BCOpedroarlindo-1Nessuna valutazione finora
- Compliance Risks and Controls: Speaker: Dott. Fabio AccardiDocumento14 pagineCompliance Risks and Controls: Speaker: Dott. Fabio AccardiJefferson WidodoNessuna valutazione finora
- Bron 2017Documento73 pagineBron 2017Anggia BungaNessuna valutazione finora
- New Microsoft Word DocumentDocumento1 paginaNew Microsoft Word Documentshubhangiw17Nessuna valutazione finora
- Chapter 27 Protists I. Evolution of EukaryotesDocumento7 pagineChapter 27 Protists I. Evolution of EukaryotesNadeem IqbalNessuna valutazione finora
- #1Documento7 pagine#1Ramírez OmarNessuna valutazione finora
- I. Specifikacija Opreme Sa Ugradnjom R.Br. Opis JM KomDocumento4 pagineI. Specifikacija Opreme Sa Ugradnjom R.Br. Opis JM KomAleksandar VidakovicNessuna valutazione finora
- Chapter - 2 Fish MongeryDocumento10 pagineChapter - 2 Fish MongeryKrishna ChaudharyNessuna valutazione finora
- Writing Lesson Plan LMDocumento6 pagineWriting Lesson Plan LMapi-457032696Nessuna valutazione finora
- FRP/HDPE septic tank specificationDocumento2 pagineFRP/HDPE septic tank specificationpeakfortuneNessuna valutazione finora
- Inventory of Vacant Units in Elan Miracle Sector-84 GurgaonDocumento2 pagineInventory of Vacant Units in Elan Miracle Sector-84 GurgaonBharat SadanaNessuna valutazione finora
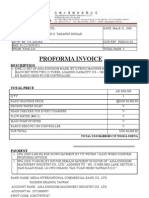
- Proforma Invoice: DescriptionDocumento3 pagineProforma Invoice: Descriptionanon-690278Nessuna valutazione finora
- Entrepreneurship: Ali Raza (Ph.D. Scholar, Near East University, North Cyprus, Mersin 10, Turkey)Documento35 pagineEntrepreneurship: Ali Raza (Ph.D. Scholar, Near East University, North Cyprus, Mersin 10, Turkey)Ameen KolachiNessuna valutazione finora