Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Carboplatin Paclitaxel
Caricato da
Nida Auliya RahmahTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Carboplatin Paclitaxel
Caricato da
Nida Auliya RahmahCopyright:
Formati disponibili
BEVACIZUMAB (AVASTIN®), CARBOPLATIN & PACLITAXEL
for Cervical Cancer
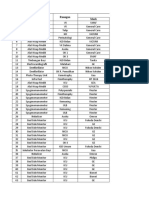
DRUG ADMINISTRATION SCHEDULE
Day Drug Dose Route Diluent & Rate
Sodium Chloride 0.9% 250/500ml Infusion Fast Running
Dexamethasone See Below*
Chlorphenamine 10mg Intravenous Slow bolus
Ranitidine 50mg Intravenous 50ml NaCl 0.9% over 20 mins
Slow bolus or 15 min infusion
Ondansetron* 8mg Oral/ IV
(patients over 65 years)
500ml NaCl 0.9% over 3hrs
Day 1 2
Paclitaxel 175mg/m IV Infusion (Use PVC Free Bag & Line) (start
infusion very slowly)
500/250ml 5% glucose over
Carboplatin AUC 5 or 6 IV Infusion
30 to 60 Minutes
Line should be flushed with 0.9% NaCl prior to administration of
Sodium Chloride 0.9%
bevacizumab
100mls 0.9% Sodium Chloride
Bevacizumab 15 mg/kg Infusion See below for rate
Check correct protocol is being use; there are three similar gynaecological cancers protocols with
different Bevacizumab doses.
● 7.5mg/kg is used for 1st line ovarian with carboplatin paclitaxel.
● 15mg/kg is used for cervical cancer with carboplatin paclitaxel.
DOSE FREQUENCY
Every 21 days for the first six cycles
BEVACIZUMAB RATE
Bevacizumab must be given in combination with chemotherapy every three weeks. Intravenous
infusion given over 90 minutes for initial dose; if tolerated next infusion can be given over 60 minutes;
can thereafter be given over 30 minutes. It can be given in 100ml Sodium Chloride provided the final
solution stays within the range of 1.4-16.5 mg/ml.
APPROVED INDICATIONS
The first line treatment of recurrent or metastatic cervical cancer in combination with chemotherapy
where all the following criteria are met:
1. Application made by and first cycle of systemic anti-cancer therapy to be prescribed by a
consultant specialist specifically trained and accredited in the use of systemic anti-cancer
therapy
2. Histologically confirmed carcinoma of the cervix
3. Indication for 1st line palliative chemotherapy
4. Primary stage IVB, recurrent, or persistent disease not amenable to curative treatment with
surgery and/or radiotherapy.
5. Given with Paclitaxel and either Cisplatin or Carboplatin
6. ECOG PS 0 or 1
7. No previous treatment with bevacizumab or other anti-VEGF therapy
Bevacizumab carboplatin paclitaxel for cervical CRP14-GY017 v1 4 Page 1 of 6
Issue Date:04/09/2018 Expiry Date: 04/09/2021
BEVACIZUMAB (AVASTIN®), CARBOPLATIN & PACLITAXEL
for Cervical Cancer
8. No contra-indication to the use of bevacizumab
9. Bevacizumab dose to be 15mg/kg every 3 weeks
Note: Bevacizumab is ONLY approved for use in combination with combination chemotherapy and
is not approved for use as a single agent maintenance therapy
Note: Bevacizumab should be discontinued for reasons of toxicity or disease progression,
whichever occurs first
EXCLUSION CRITERIA
Contraindicated in patients who have a history of hypersensitivity reaction to bevacizumab or other
recombinant human or humanized antibodies
Caution in patients with:
Untreated central nervous system metastases
Uncontrolled hypertension
History/ Risk factors for thromboembolic events e.g. history of arterial thromboembolic events
Significant cardiac risk factors for development of CHF (congestive heart failure)
Patients with baseline renal function less than 30ml/min (Creatinine Clearance)
PREMEDICATION
Anti-emetics are not required for Bevacizumab treatment. Take home medications as per
chemotherapy regimen.
Premedication of dexamethasone, ranitidine and chlorphenamine is given prior to Paclitaxel
infusion to reduce of risk of hypersensitivity reaction.
Dexamethasone can be given either as 20mg orally 12 and 6 hours prior to treatment or a
20mg IV bolus prior to treatment
Antiemetic cover with neurokinin 1 (NK1) receptor antagonists
ASCO 2017 antiemetic guidance recommends regimens containing carboplatin ≥ AUC4 should be
classified as high risk of CINV and patients offered a three-drug combination of a neurokinin 1 (NK1)
receptor antagonist, a serotonin (5-HT3) receptor antagonist and dexamethasone. Current practice in
NCA is to start with a two-drug regimen serotonin (5-HT3) receptor antagonist and dexamethasone
and add in a neurokinin 1 (NK1) receptor antagonist if CINV not adequately controlled. However, if
pre-assessment of patient identifies risk factors for CINV, units may wish to start with a 3-drug
combination.
RECOMMENDED TAKE HOME MEDICATION
Ondansetron 8mg twice daily for 2 to 3 days
Dexamethasone 4mg twice daily for 1 to 3 days and as above if oral pre-medication used
Metoclopramide 10mg three times daily as required
Suggested antiemetic regimen - may vary with local practice. See CINV policy for more details
INVESTIGATIONS / MONITORING REQUIRED
Pre-treatment:
Assessment of renal function, FBC, Cardiac history
Cardiac assessment incl. history and physical exam
Check renal function before commencing platinum. Use EDTA or Wright formulae to calculate GFR
Bevacizumab carboplatin paclitaxel for cervical CRP14-GY017 v1 4 Page 2 of 6
Issue Date:04/09/2018 Expiry Date: 04/09/2021
BEVACIZUMAB (AVASTIN®), CARBOPLATIN & PACLITAXEL
for Cervical Cancer
Prior to each cycle
FBC, U&Es, LFTs as required; GFR doubled checked using Wright formulae
Tumour markers as appropriate, e.g. where CEA is elevated this should be measured before each
cycle
Monitor blood pressure every cycle and more frequently in patients who develop hypertension
Proteinuria by dipstick analysis prior to treatment and before each dose. If protein present
undertake quantitative measurement of protein in urine and if greater than 2g > 24hrs delay of
bevacizumab.
ASSESMENT OF RESPONSE
Assessed radiologically after each cycle.
Metastatic: Tumour size and patient symptomatic response
REVIEW BY CLINICIAN
Review at each cycle as appropriate
NURSE / PHARMACIST LED REVIEW
Each cycle as applicable according to local protocols
ADMINISTRATION NOTES
BEVACIZUMAB
Hypertension is commonly observed, may be dose-related and should be managed with
antihypertensives, e.g. calcium channel blockers.
Units administering bevacizumab must have facilities available for the treatment of anaphylaxis
and resuscitation.
May not need to stop treatment for minor hypersensitivity e.g. reactions, flushing, localised rash.
Must be stopped for major reactions, e.g. hypotension, dyspnoea, angioedema or generalised
urticaria.
Paracetamol can be used to treat reactions.
Bevacizumab therapy should not be initiated for at least 28 – 60 days following major surgery or
until the surgical wound is fully healed. If elective surgery is planned, bevacizumab should be
withheld, and the long half-life considered.
PACLITAXEL
Paclitaxel must be administered via a non-PVC administration set and 0.2-micron filter.
May not need to stop treatment for minor hypersensitivity e.g. reactions, flushing, localised rash.
Must be stopped for major reactions, e.g. hypotension, dyspnoea, angioedema or generalised
urticaria.
If patient has hypersensitivity reaction, follow manufacturers re-challenge guidelines before
continuing with treatment.
Units administering Paclitaxel must have facilities available for the treatment of anaphylaxis and
resuscitation.
Blood pressure & pulse should be monitored regularly (e.g. every 30 minutes) during paclitaxel
infusion
Bevacizumab carboplatin paclitaxel for cervical CRP14-GY017 v1 4 Page 3 of 6
Issue Date:04/09/2018 Expiry Date: 04/09/2021
BEVACIZUMAB (AVASTIN®), CARBOPLATIN & PACLITAXEL
for Cervical Cancer
CARBOPLATIN
Patient needs Glomerular Filtration Rate (GFR) prior to commencement of treatment for
calculation of Carboplatin dosage. Subsequent measurement of GFR only needed if serum
creatinine changes by >20% from initial measurement.
May not need to stop treatment for minor hypersensitivity e.g. reactions, flushing, localised rash.
Must be stopped for major reactions, e.g. hypotension, dyspnoea, angioedema or generalised
urticaria.
EXTRAVASATION Follow NCA and Local Trust Guidelines
MAIN TOXICITIES
CARBOPLATIN AND PACLITAXEL
Risk of hypersensitivity and anaphylaxis, particularly on first and second cycle, start within a few
minutes of administration
Nausea and vomiting
Hypotension and bradycardia
Myelosuppression, particularly, thrombocytopenia, anaemia & neutropenia
Nephrotoxicity
Alopecia
Peripheral neuropathy
Otological impairment, especially at 8000 Hz
Myalgia
Back pain on administration
BEVACIZUMAB
Fatigue, hypertension, proteinuria, headache
Infusion-associated symptoms / acute hypersensitivity reactions (anaphylaxis, chills and fever,
nausea, vomiting, pain, rigors, headache, asthenia etc.)
Diarrhoea
Abdominal pain
Nausea and vomiting
Less Common Toxicities that may be severe or life-threatening include:
Arterial/venous thromboembolism
GI perforation, fistulas, wound dehiscence
Haemorrhage
Cardiac failure
Pneumonitis
DOSE MODIFICATIONS
Haematological toxicity:
Proceed on Day 1 If:
PLT ≥ 100 ANC ≥ 1.0
Delay 1 week on DAY 1 if:
PLT <100 ANC <1.0
Bevacizumab carboplatin paclitaxel for cervical CRP14-GY017 v1 4 Page 4 of 6
Issue Date:04/09/2018 Expiry Date: 04/09/2021
BEVACIZUMAB (AVASTIN®), CARBOPLATIN & PACLITAXEL
for Cervical Cancer
If Hb < 10 & patient symptomatic will need blood transfusion but may proceed with
chemotherapy as planned if performance status (PS) stable.
If pre-treatment U&Es & LFTs abnormal, delay treatment 1 week and discuss with Oncologist
as may need dose reduction.
Non-Haematological Toxicity:
If PS deteriorates to 3 or 4 and on assessment patient is more symptomatic withhold
treatment and discuss with Oncologist
Bevacizumab dose reduction for toxicity is not recommended, but dosing with bevacizumab should be
omitted or discontinued for the following adverse events: Uncontrollable hypertension, delayed
wound healing, surgery, grade 3 proteinuria (>3g in 24hrs ref. CTCv4).
When receiving in combination with chemotherapy, if a cycle of chemotherapy is delayed for any
reason, the bevacizumab dose should also be delayed until the patient is fit enough for chemotherapy
HYPERTENSION
Baseline blood pressure should be < 150/100mmHg.
If diastolic increase > 20mmHg above baseline or blood pressure rises to > 150/100mmHg,
antihypertensive therapy may be indicated. Treatment, and initial monitoring until stabilised, is
usually best managed via the patient’s GP.
If blood pressure > 180/110mmHg, it is advised that bevacizumab therapy is withheld until blood
pressure controlled.
PROTEINURIA
A suggested assessment of urine dipstick results is:
1+ or 2+ on dipstick Continue with bevacizumab (no additional evaluation required).
(0.3-2.9g/L)
May have dose of bevacizumab as scheduled but will need 24-hour urine to
measure 24-hour protein to be done a few days before next cycle due.
If 24-hour protein result < 2g, continue with bevacizumab with proteinuria
3+ on dipstick monitoring via 24-hour urine before each dose. If the 24-hour protein
(3-19g/L) level falls to <1g/24hr, return to dipstick analysis.
If ≥ 2g, withhold bevacizumab until repeat 24-hour urine collection shows
<2g protein. Then re-introduce bevacizumab, with continued proteinuria
monitoring via 24-hour urine.
4+ on dipstick Withhold bevacizumab. 24-hour urine required. Follow 24-hour urine
(≥20g/L) monitoring and guidance as for 3+ on dipstick.
RENAL IMPAIRMENT
There are no data for bevacizumab in patients with impaired renal function. However, dose
adjustments would not be expected to be required.
Carboplatin - If creatinine level increases by >20% from the result used to calculate GFR (or pre-
treatment baseline if EDTA performed) discuss with consultant and consider repeating EDTA.
Bevacizumab carboplatin paclitaxel for cervical CRP14-GY017 v1 4 Page 5 of 6
Issue Date:04/09/2018 Expiry Date: 04/09/2021
BEVACIZUMAB (AVASTIN®), CARBOPLATIN & PACLITAXEL
for Cervical Cancer
HEPATIC IMPAIRMENT
There are no data for bevacizumab in patients with impaired liver function. However, dose
adjustments would not be expected to be required.
Paclitaxel Dose reduction of 25% in patients with disturbed liver biochemistry. Contraindicated if
Bilirubin > x 2.5 ULN, Transaminases > x 2.5 ULN,
TREATMENT LOCATION
Can be given at Cancer Centre or Cancer Unit
REFERENCES
1. Kelly K et al. Randomized phase III trial of paclitaxel plus Carboplatin versus vinorelbine plus
cisplatin in the treatment of patients with advanced non-small-cell lung cancer: A southwest
oncology group trial. JCO 19(13): 3210-18, 2001.
2. Schiller JH et al. Comparison of four chemotherapy regimens for advanced non- small-cell lung
cancer. New Engl J Med 2002; 346:92-8.
3. Ozols RF et al. Phase III trial of carboplatin and paclitaxel compared with cisplatin and
paclitaxel in patients with optimally resected stage III ovarian cancer:
4. Kristensen et al; JCO 2011; 29 suppl; abstract LBA5006 (ICON 7)
5. Burger, R.A., Brady, M.F., Bookman, M.A., Fleming, G.F., Monk, B.J., Huang, H., Mannel, R.S.,
Homesley, H.D., Fowler, J., Greer, B.E. and Boente, M., 2011. Incorporation of bevacizumab in
the primary treatment of ovarian cancer. New England Journal of Medicine, 365(26), pp.2473-
2483.
Document Title: BEVACIZUMAB (AVASTIN®), CARBOPLATIN & PACLITAXEL for Cervical Cancer
Document No: CRP09 GY017 Current Version: 1.4
Chris Beck,
Reviewer: Date Approved: 04/09/2018
Cancer Alliance Pharmacist
Steve Williamson, Consultant
Approved by: Due for Review: 04/09/2021
Pharmacist, Northern Cancer Alliance
Summary of Changes 1.2 Document created, reviewed, formatted and approved.
1.3 Antiemetic advice updated
1.4 Updated against Chemocare parameters, updated CDF approval
Bevacizumab carboplatin paclitaxel for cervical CRP14-GY017 v1 4 Page 6 of 6
Issue Date:04/09/2018 Expiry Date: 04/09/2021
Potrebbero piacerti anche
- Taxotere Docetaxel 80 mg/4 ML Concentrate For Solution For InfusionDocumento52 pagineTaxotere Docetaxel 80 mg/4 ML Concentrate For Solution For InfusionArbiati Rahman100% (1)
- Is My Patient "Drug-Seeking"?: Matthew Hathaway Courtney Samanipour Amanda SeedsDocumento12 pagineIs My Patient "Drug-Seeking"?: Matthew Hathaway Courtney Samanipour Amanda Seedsapi-284053760Nessuna valutazione finora
- Chemotherapy and Biotherapy Hypersensitivity Reactions: Christine E. Coyle, RN, BSN, OCNDocumento55 pagineChemotherapy and Biotherapy Hypersensitivity Reactions: Christine E. Coyle, RN, BSN, OCNRakesh MishraNessuna valutazione finora
- Folfiri Beva Gi Col PDocumento12 pagineFolfiri Beva Gi Col Pvera docNessuna valutazione finora
- Oncology-Study of Cancer Cellular AbberationDocumento43 pagineOncology-Study of Cancer Cellular AbberationIrwan M. IskoberNessuna valutazione finora
- Principle of Chemotherapy Main PresentationDocumento84 paginePrinciple of Chemotherapy Main Presentationadekunle ajayiNessuna valutazione finora
- Chemotherapeutic DrugsDocumento4 pagineChemotherapeutic DrugsEditor IJTSRDNessuna valutazione finora
- Taxenes in Breast Cancer (Sharm)Documento76 pagineTaxenes in Breast Cancer (Sharm)safasayedNessuna valutazione finora
- Chemotherapy MedicinesDocumento2 pagineChemotherapy Medicinesr_mckenrick0% (1)
- Oncology LectureDocumento92 pagineOncology Lecturerustie26Nessuna valutazione finora
- Introduction To TransplantationDocumento3 pagineIntroduction To TransplantationGerardLumNessuna valutazione finora
- Introductory Pharmacology - Cancer ChemotherapyDocumento9 pagineIntroductory Pharmacology - Cancer ChemotherapyTyler Rosolowski100% (2)
- NCCN Guideline RC v3 2022Documento20 pagineNCCN Guideline RC v3 2022dony hendrawanNessuna valutazione finora
- DR Tommy - Cancer PainDocumento60 pagineDR Tommy - Cancer Painrisalbalu100% (1)
- D105 APBI Future - My Point of ViewDocumento70 pagineD105 APBI Future - My Point of ViewSoc. Portuguesa de Radioterapia OncologiaNessuna valutazione finora
- Alkylating AgentsDocumento53 pagineAlkylating AgentsDhanya KcNessuna valutazione finora
- Xodo Document - Periprocedural - Anticoagulation - GuidelineDocumento16 pagineXodo Document - Periprocedural - Anticoagulation - Guidelinebrigde_xNessuna valutazione finora
- Antineoplastic Agents 2011 Dental MARCH-1Documento41 pagineAntineoplastic Agents 2011 Dental MARCH-1BinayakSwainNessuna valutazione finora
- Lung Cancer Treatment Regimens (Part 1 of 4)Documento4 pagineLung Cancer Treatment Regimens (Part 1 of 4)Rubana Reaz TanaNessuna valutazione finora
- Cell Cycle ChemotherapyDocumento5 pagineCell Cycle ChemotherapyVictoria Alessandra BrownNessuna valutazione finora
- BC CancerDocumento42 pagineBC CancerIsal SparrowNessuna valutazione finora
- Concurrent ChemoRadiotherapyDocumento51 pagineConcurrent ChemoRadiotherapyJalal EltabibNessuna valutazione finora
- Overview of CancerDocumento31 pagineOverview of Cancersamarth kaulNessuna valutazione finora
- Antidote - Chart - 20141014 (Poison Control System) PDFDocumento5 pagineAntidote - Chart - 20141014 (Poison Control System) PDFMichael Freudiger100% (1)
- 2016 ASCO - ONS Chemo Standards PDFDocumento13 pagine2016 ASCO - ONS Chemo Standards PDFSindu SaiNessuna valutazione finora
- Antibiotic Class by CoverageDocumento3 pagineAntibiotic Class by Coverageayy1Nessuna valutazione finora
- Hematology Review 2021-2Documento142 pagineHematology Review 2021-2Maram AbdullahNessuna valutazione finora
- Molecular Diagnostics in Cancer Paper 1Documento15 pagineMolecular Diagnostics in Cancer Paper 1Marian ValdiviaNessuna valutazione finora
- Emetogenicity Tool Kit YaaaDocumento2 pagineEmetogenicity Tool Kit Yaaaandirio7486Nessuna valutazione finora
- Sample: Oncotype DX Breast Cancer AssayDocumento2 pagineSample: Oncotype DX Breast Cancer Assaybirhane gebreegziabiherNessuna valutazione finora
- Cancer ChemotherapyDocumento86 pagineCancer ChemotherapyFrancheska MicuNessuna valutazione finora
- Tumor MarkersDocumento9 pagineTumor MarkersDewi Puspita SariNessuna valutazione finora
- CELL OVERVIEW PREVENTION Notes 2015Documento7 pagineCELL OVERVIEW PREVENTION Notes 2015Alexander LukashenkoNessuna valutazione finora
- Drug Name Gemcitabine: Synonym (S) : Common Trade Name (S) : ClassificationDocumento8 pagineDrug Name Gemcitabine: Synonym (S) : Common Trade Name (S) : ClassificationOka Robi MuhammadNessuna valutazione finora
- If HP Cancer Guide br007 MriDocumento13 pagineIf HP Cancer Guide br007 Mrirusgal8992100% (1)
- Oxaliplatin Monograph 1dec2016Documento9 pagineOxaliplatin Monograph 1dec2016Nadial UzmahNessuna valutazione finora
- Medicine2 - Complications of Cancer Treatment 2007Documento76 pagineMedicine2 - Complications of Cancer Treatment 2007api-3762917Nessuna valutazione finora
- H. OncologyDocumento27 pagineH. OncologyGloryJaneNessuna valutazione finora
- What Is A Bone Marrow Transplant?Documento4 pagineWhat Is A Bone Marrow Transplant?Krisna AgustiniNessuna valutazione finora
- Pharm Chemo Drugs SauldDocumento6 paginePharm Chemo Drugs Sauldneal100% (1)
- Ovarian CancerDocumento7 pagineOvarian CancerAndi AliNessuna valutazione finora
- Thromboembolism & ThromboprophylaxisDocumento48 pagineThromboembolism & Thromboprophylaxisazida90Nessuna valutazione finora
- MS - Onco & HemaDocumento12 pagineMS - Onco & HemaLerry Claire LimosNessuna valutazione finora
- Cancer Genetics: Sreekutty S 2 MSC ZoologyDocumento34 pagineCancer Genetics: Sreekutty S 2 MSC ZoologyShamsudheen maharajasNessuna valutazione finora
- Selected Oncologic Emergencies: Sandra S. Ugras-ReyDocumento13 pagineSelected Oncologic Emergencies: Sandra S. Ugras-ReyJustene PeñamoraNessuna valutazione finora
- Chemotherapy: Chemotherapy, in Its Most General Sense, Refers To Treatment of Disease byDocumento42 pagineChemotherapy: Chemotherapy, in Its Most General Sense, Refers To Treatment of Disease byMalueth AnguiNessuna valutazione finora
- Benign and Malignant Lesion of Lower GIDocumento45 pagineBenign and Malignant Lesion of Lower GIAhmad Alzu3beNessuna valutazione finora
- Approach To The Adult With Unexplained Thrombocytopenia - UpToDateDocumento65 pagineApproach To The Adult With Unexplained Thrombocytopenia - UpToDateMagdy GabrNessuna valutazione finora
- 03-Anti-Cancer Drugs - FST PDFDocumento77 pagine03-Anti-Cancer Drugs - FST PDFRyan RachmawanNessuna valutazione finora
- Colon CancerDocumento7 pagineColon CancerKen Ancheta LagayadaNessuna valutazione finora
- Carboplatin MonographDocumento9 pagineCarboplatin Monographmerkuri100% (1)
- 3 - Clinical Pharmacology of ChemotherapyDocumento111 pagine3 - Clinical Pharmacology of ChemotherapyChinIsiangSocitoNessuna valutazione finora
- Management of High Grade Bladder Cancer & Carcinoma in SituDocumento26 pagineManagement of High Grade Bladder Cancer & Carcinoma in SituSakuntalaPalankiNessuna valutazione finora
- Classification of DrugsDocumento10 pagineClassification of DrugsSafura IjazNessuna valutazione finora
- Anticancer Drugs Anticancer Drugs: Tasneem Smerat Tasneem SmeratDocumento118 pagineAnticancer Drugs Anticancer Drugs: Tasneem Smerat Tasneem Smeratanwar jabari100% (1)
- Anti Cancer Drugs...Documento62 pagineAnti Cancer Drugs...KwirimeNessuna valutazione finora
- Penis Cancer, A Simple Guide To The Condition, Treatment And Related ConditionsDa EverandPenis Cancer, A Simple Guide To The Condition, Treatment And Related ConditionsNessuna valutazione finora
- Microemulsion Formulation For Topical Delivery of Miconazole NitrateDocumento8 pagineMicroemulsion Formulation For Topical Delivery of Miconazole NitrateNida Auliya RahmahNessuna valutazione finora
- Microemulsion Formulation For Topical Delivery of Miconazole NitrateDocumento8 pagineMicroemulsion Formulation For Topical Delivery of Miconazole NitrateNida Auliya RahmahNessuna valutazione finora
- Adrenaline and HypertensionDocumento160 pagineAdrenaline and HypertensionNida Auliya RahmahNessuna valutazione finora
- Enzymes Inhibitors From Plants An Alternate Approach To Treat DiabetesDocumento17 pagineEnzymes Inhibitors From Plants An Alternate Approach To Treat DiabetesNida Auliya RahmahNessuna valutazione finora
- Jurnal Madu PDFDocumento8 pagineJurnal Madu PDFNida Auliya RahmahNessuna valutazione finora
- Abstract Book SLVA2012Documento59 pagineAbstract Book SLVA2012Nida Auliya RahmahNessuna valutazione finora
- P65 Toxic Chems List B Cali PDFDocumento23 pagineP65 Toxic Chems List B Cali PDFnunyabeezwax1Nessuna valutazione finora
- Kualitas Bakterial Cabe GiligDocumento7 pagineKualitas Bakterial Cabe GiligNida Auliya RahmahNessuna valutazione finora
- (WWW - Wangsiteducation.com) UM UGM 2013 Dasar Kode 251 (Mark)Documento12 pagine(WWW - Wangsiteducation.com) UM UGM 2013 Dasar Kode 251 (Mark)N ParamithaNessuna valutazione finora
- Hand Hygiene Audit March 19Documento17 pagineHand Hygiene Audit March 19Sammie WainainaNessuna valutazione finora
- B. Inggris TongueDocumento2 pagineB. Inggris TongueP17211211007 NURUL HUDANessuna valutazione finora
- Verrucous CarcinomaDocumento12 pagineVerrucous Carcinomaanatomimanusia100% (1)
- Aetiology of Canine Infectious Respiratory Disease Complex and Prevalence of Its Pathogens in EuropeDocumento23 pagineAetiology of Canine Infectious Respiratory Disease Complex and Prevalence of Its Pathogens in EuropeNadia AbarcaNessuna valutazione finora
- Pleural Effusion: Etiology: Pleural Fluid Formation AbsorptionDocumento16 paginePleural Effusion: Etiology: Pleural Fluid Formation AbsorptionitsireneNessuna valutazione finora
- Laporan 10 Penyakit Terbesar Rawat Inap Bulan Januari 2022: Rawat Inap LT 1 Rawat Inap LT 2 Rawat Inap Perina-NiccuDocumento4 pagineLaporan 10 Penyakit Terbesar Rawat Inap Bulan Januari 2022: Rawat Inap LT 1 Rawat Inap LT 2 Rawat Inap Perina-NiccuAhmad MunifNessuna valutazione finora
- Daftar Kalibrasi Alat 2020Documento18 pagineDaftar Kalibrasi Alat 2020Budi SetyawanNessuna valutazione finora
- NAPZA Is The Abbreviation of DrugsDocumento24 pagineNAPZA Is The Abbreviation of DrugsFahmi ArdianNessuna valutazione finora
- E TIMA News Letter November 2016 2 Min - CompressedDocumento39 pagineE TIMA News Letter November 2016 2 Min - Compressedasidique5_292665351Nessuna valutazione finora
- Malnutrition in Older AdultsDocumento44 pagineMalnutrition in Older Adultsjohnjoe subaynoNessuna valutazione finora
- Alemnesh MandeshDocumento94 pagineAlemnesh MandeshDNessuna valutazione finora
- Investigations For Diseases of The Tongue A Review PDFDocumento6 pagineInvestigations For Diseases of The Tongue A Review PDFShantanu DixitNessuna valutazione finora
- SalesDocumento1 paginaSalesapi-77587316Nessuna valutazione finora
- Concept of PreventionDocumento48 pagineConcept of Preventionmahmoud100% (1)
- Pathophysiology of Pain in BiliodigestiDocumento19 paginePathophysiology of Pain in Biliodigestiprabowoaji12Nessuna valutazione finora
- Reducing Hospital Readmissions: by Jenny MinottDocumento12 pagineReducing Hospital Readmissions: by Jenny MinottRr.Tutik SRi HariyatiNessuna valutazione finora
- Drug StudyDocumento7 pagineDrug StudyHanna Clarisse PataoNessuna valutazione finora
- Comparison of Intravitreal Bevacizumab (Avastin) With Triamcinolone For Treatment of Diffused Diabetic Macular Edema: A Prospective Randomized StudyDocumento9 pagineComparison of Intravitreal Bevacizumab (Avastin) With Triamcinolone For Treatment of Diffused Diabetic Macular Edema: A Prospective Randomized StudyBaru Chandrasekhar RaoNessuna valutazione finora
- Cytomegalovirus (CMV) : R.Varidianto Yudo T., Dr.,MkesDocumento21 pagineCytomegalovirus (CMV) : R.Varidianto Yudo T., Dr.,MkesIndah WahyuningtyasNessuna valutazione finora
- PTB Case-StudyDocumento64 paginePTB Case-StudyBeverly DatuNessuna valutazione finora
- Referat Distosia Bahu ElfaDocumento16 pagineReferat Distosia Bahu ElfaElfa RiniNessuna valutazione finora
- Pfizer Drug R&D Pipeline As of July 31, 2007Documento19 paginePfizer Drug R&D Pipeline As of July 31, 2007anon-843904100% (1)
- 603ca5b18c1d9 PANE Written - Sample QuestionsDocumento11 pagine603ca5b18c1d9 PANE Written - Sample QuestionsFazal ShahNessuna valutazione finora
- Clinical Avian Medicine - 2 Volume Set PDFDocumento1.057 pagineClinical Avian Medicine - 2 Volume Set PDFSilvana Martinez100% (3)
- Chirorab Prescribing InformationDocumento2 pagineChirorab Prescribing Informationsr bNessuna valutazione finora
- DGN ExamDocumento5 pagineDGN ExamMaiga Ayub HusseinNessuna valutazione finora
- Hospital Direct Roller Slide SheetDocumento2 pagineHospital Direct Roller Slide SheetdantefuerteNessuna valutazione finora
- A Clinical Materia Medica by DR FringtonDocumento768 pagineA Clinical Materia Medica by DR FringtonAli AkbarNessuna valutazione finora
- SHD Form 4 T - NTPDocumento3 pagineSHD Form 4 T - NTPElle RochNessuna valutazione finora
- Lab 2 - Birth Spacing Policy in OmanDocumento39 pagineLab 2 - Birth Spacing Policy in OmanMeme 1234Nessuna valutazione finora