Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Calcium Homeostasis INFOO
Caricato da
Mika Sophia GonzagaCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Calcium Homeostasis INFOO
Caricato da
Mika Sophia GonzagaCopyright:
Formati disponibili
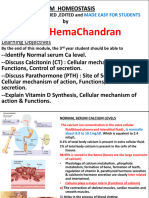
Hormonal Control of Blood Calcium Levels -decrease the blood calcium level when it
rises above the normal (releases Ca from bone)
- Blood levels of calcium are regulated by the
In this process it opposes the effects of the
parathyroid hormone, which acts on the bones,
parathyroid hormone, which acts to increase
kidneys, and intestines to keep levels constant.
the blood level of calcium.
Key Points:
:by regulate phosphate metabolism, it lowers
• The parathyroid hormone (PTH), the blood phosphorus level when it rises above
secreted by the parathyroid glands normal.
(belonging to the endocrine system) is
hypoparathyroidism: deficiency of parathyroid
responsible for regulating blood calcium
hormone
levels; it is released whenever blood
calcium levels are low. hyperparathyroidism: an abnormal increase in
parathyroid gland activity
PTH increases blood calcium levels by
stimulating osteoclasts, which break calcitriol: the active metabolite (substance
down bone to release calcium into the necessary for metabolic processes) 1,25-
blood stream. dihydroxycholecalciferol of vitamin D3 that is
involved in the absorption of calcium.
PTH increases blood calcium levels by
increasing the amount of calcium : functions
resorbed by the kidneys before it can be
-promoting absorption of dietary calcium
excreted in the urine.
from the gastrointestinal tract (digestive system
tract)
PTH increases blood calcium levels by
triggering the formation of calcitriol, - increasing renal tubular reabsorption of
which increases absorption of dietary calcium, reducing the loss of calcium in the
calcium through the intestines. urine.
Calcitonin, a hormone produced by the - stimulate release of calcium from
thyroid, acts in opposition to PTH by osteoblasts causing them to release RANKL
inhibiting osteoclasts, stimulating (Receptor Activator of Nuclear factor-Kappa B
osteoblasts, and increasing excretion of Ligand found on the extracellular surface of
calcium into the urine by the kidneys. their plasma membrane) which activates
osteoclasts
Vocab: osteoclast: a large multinuclear (many nucleus)
cell associated with bone resorption
osteoblast: a mononucleate (single nucleus) cell
that secretes the matrix for bone mineralization :bone resorption – osteoclasts remove bone
(during initial bone formation and later bone tissue by removing the mineral matrix of the
remodeling [if necessary]) bone (courtesy of osteoblast) and dissolving the
collagen part of the bone
: at the later part of bone formation, the
osteoblast is surrounded by the growing bone -the bone is broken down to
matrix and as the material calcifies, the cell is source calcium and transfer it to the blood.
trapped and forms into an osteocyte (bone cell) -happens when there is low
parathyroid hormone: a polypeptide (chain of amount of calcium in the blood
amino acids caused by dehydration; function
dependent on one’s distinct chemical structure)
hormone that is released by the parathyroid
glands (endocrine system) and is involved in
raising the levels of calcium ions in the blood.
:aka parathormone or parathyrin
calcitonin: a hormone that is mainly secreted by
parafollicular cells (C cells) of the thyroid gland
that regulates calcium and phosphate
metabolism
:by regulate calcium,
DA BEEF LEZGO! In the intestines:
Core Idea: Regulation of blood calcium is - PTH increases dietary calcium (calcium from
important for generating muscle contractions food) absorption
and quick nerve impulses.
-Effects are indirect.
- If calcium levels get too high, membrane
- PTH triggers the formation of calcitriol, an
permeability to sodium (Na+) decreases and
active form of vitamin D3, which acts on the
membranes become less responsive.
intestines to increase absorption of dietary
- If calcium levels get too low, membrane calcium (calcium from food). PTH release is
permeability to sodium (Na+) increases and inhibited (prevented) by rising blood calcium
convulsions or muscle spasms may result. levels.
- Blood calcium levels are regulated by In the kidneys:
parathyroid hormone (PTH), which is produced
-PTH acts directly on the kidneys to increase
by the parathyroid glands.
calcium re-absorption.
* It is released in response to low blood
* Kidneys regulate how much calcium
calcium levels.
must be eliminated.
*PTH increases calcium levels by
* Kidneys turn vitamin D3 into an
targeting the skeleton, kidneys and intestine.
active metabolite (calcitriol), which helps
increase renal calcium resorption (metabolic
process) and phosphate excretion.
In the skeleton (main homeostasis for calcium
occurs)(the whole process including PTH and - The hormone calcitonin, which is produced by
calcitonin, osteoblast deposition of ca and the parafollicular (or C) cells of the thyroid, has
osteoclast resorption of ca is called ossification) the opposite effect on blood calcium levels as
PTH. Calcitonin decreases blood calcium levels
When blood calcium levels are high!
by inhibiting osteoclasts, stimulating
- PTH promote osteoblast formation (cells which osteoblasts, and stimulating calcium excretion
mineralize bone thru extracellular matrix) to by the kidneys.
deposit the calcium from the blood into the
bone.
-PTH discourages osteoclast formation which
are cells that cause bone reabsorption,
decreasing the amount of calcium level to be
absorbed from the bone to transfer into the
blood.
When blood calcium levels are low!
- Calcitonin is a hormone produced by the
parafollicular (or C) cells is released from the
thyroid gland and reverses the effect of PTH on
blood calcium levels!
-Calcitonin signals osteoclast formation, which
are cells that cause bone reabsorption,
increasing the amount of calcium level to be
absorbed from the bone to transfer into the
blood.
-Calcitonin then discourages osteoblast
formation, decreasing the bone calcium levels
of the body just until the bone calcium levels
become normal once again.
Potrebbero piacerti anche
- Life And Death Of A Parathyroid Gland Cell (Calcium Man)Da EverandLife And Death Of A Parathyroid Gland Cell (Calcium Man)Nessuna valutazione finora
- Control Blood of Calcium LevelsDocumento2 pagineControl Blood of Calcium Levelswoman in stemNessuna valutazione finora
- Parathyroid Gland, Functions, Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandParathyroid Gland, Functions, Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- MK Biokimia - Metabolisme MineralDocumento84 pagineMK Biokimia - Metabolisme MineralmusimsemiNessuna valutazione finora
- A Simple Guide to Hyperparathyroidism, Treatment and Related DiseasesDa EverandA Simple Guide to Hyperparathyroidism, Treatment and Related DiseasesNessuna valutazione finora
- Calcium HomeostasisDocumento10 pagineCalcium Homeostasiszsf8m52ky4Nessuna valutazione finora
- Parathyroid Gland: Clinical Chemistry - 3Documento16 pagineParathyroid Gland: Clinical Chemistry - 3Mary Rose BarrigaNessuna valutazione finora
- Calcium Metabolism 1Documento24 pagineCalcium Metabolism 1Shimmering MoonNessuna valutazione finora
- Share Market Report 6Documento13 pagineShare Market Report 6Nithish DevadigaNessuna valutazione finora
- Hormon Parathyroid: Dr. Nanang Miftah F, SPPDDocumento13 pagineHormon Parathyroid: Dr. Nanang Miftah F, SPPDFitri Nur DiniNessuna valutazione finora
- Calcium Regulation in MetabolismDocumento2 pagineCalcium Regulation in MetabolismveerdoriNessuna valutazione finora
- Parathormone, CalcitoninDocumento14 pagineParathormone, CalcitoninIbrahimNessuna valutazione finora
- Calcium Haemostasis: By: Vasavi.NDocumento26 pagineCalcium Haemostasis: By: Vasavi.NmahalakshmiNessuna valutazione finora
- Calcium Salts Calcitonin and CA RegulatorsDocumento40 pagineCalcium Salts Calcitonin and CA RegulatorsSudhakar LakavathNessuna valutazione finora
- Calcium Homeostasis: Normal Plasma LevelsDocumento5 pagineCalcium Homeostasis: Normal Plasma LevelsE MeerNessuna valutazione finora
- Parathyroid: Calcium and Vitamin DDocumento135 pagineParathyroid: Calcium and Vitamin DPhysiology by Dr RaghuveerNessuna valutazione finora
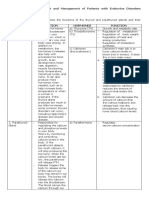
- Assessment and Management of Patients With Endocrine DisordersDocumento8 pagineAssessment and Management of Patients With Endocrine DisordersaliNessuna valutazione finora
- Parathyroid Hormone and Calcium Regulation: By: Abebe TDocumento29 pagineParathyroid Hormone and Calcium Regulation: By: Abebe TLidiya TeshomeNessuna valutazione finora
- ParathyroidDocumento2 pagineParathyroiddhaineyNessuna valutazione finora
- Biochem 11Documento5 pagineBiochem 11Abdullah RaufNessuna valutazione finora
- Lect 9 Parathyroid Gland-1Documento30 pagineLect 9 Parathyroid Gland-1warda farooqNessuna valutazione finora
- Hormonal Control of Calcium and Phosphate MetabolismDocumento50 pagineHormonal Control of Calcium and Phosphate MetabolismhamidNessuna valutazione finora
- Calcium Homeostasis: Bone Blood Ca++ KidneyDocumento12 pagineCalcium Homeostasis: Bone Blood Ca++ KidneyGiselleCamilliaNessuna valutazione finora
- Calcium Homeostasis: General PhysiologyDocumento6 pagineCalcium Homeostasis: General PhysiologyE MeerNessuna valutazione finora
- 27 - Hypo and Hypernatremia - and Hypo and Hyperkalieama PDFDocumento48 pagine27 - Hypo and Hypernatremia - and Hypo and Hyperkalieama PDFEITHAR OmarNessuna valutazione finora
- Calcium Homeostasis: Bone Blood Ca++ KidneyDocumento12 pagineCalcium Homeostasis: Bone Blood Ca++ KidneyArnab SahaNessuna valutazione finora
- Calcium Homeostasis: Bone Blood Ca++ KidneyDocumento12 pagineCalcium Homeostasis: Bone Blood Ca++ KidneyOmSilence2651Nessuna valutazione finora
- Calcium MetabolismDocumento19 pagineCalcium MetabolismShabariNath R NairNessuna valutazione finora
- Homeostatic Function of Thyroid and Parathyroid Gland & Calcium HomeostasisDocumento15 pagineHomeostatic Function of Thyroid and Parathyroid Gland & Calcium HomeostasisGEETA MOHANNessuna valutazione finora
- HypocalcemiaDocumento4 pagineHypocalcemiaJezreel BonaNessuna valutazione finora
- Calcium Homeostasis: V.Yuvaraj ROLL NO.: 150 First Year MbbsDocumento22 pagineCalcium Homeostasis: V.Yuvaraj ROLL NO.: 150 First Year MbbsYuvarajNessuna valutazione finora
- Calcium Homeostasis: Bone Blood Ca++ KidneyDocumento12 pagineCalcium Homeostasis: Bone Blood Ca++ KidneyZhin ChinNessuna valutazione finora
- General Instructions: - The Search Should Contain The FollowingsDocumento15 pagineGeneral Instructions: - The Search Should Contain The FollowingsDr-AHmad Fasfous AL-QaisiNessuna valutazione finora
- PTH RegulationDocumento16 paginePTH RegulationJetGoliath 26Nessuna valutazione finora
- Parathyroid Gland: Dr. Mustafa Abdalgadir Khandgawi Ibrahim 2016Documento24 pagineParathyroid Gland: Dr. Mustafa Abdalgadir Khandgawi Ibrahim 2016Mustafa KhandgawiNessuna valutazione finora
- Lecture 15 Parathyroid Gland Anatomy and FunctionDocumento3 pagineLecture 15 Parathyroid Gland Anatomy and FunctionbomabenediNessuna valutazione finora
- HypercalcemiaDocumento2 pagineHypercalcemiaJulieNessuna valutazione finora
- Schenck 2007Documento16 pagineSchenck 2007Luisa Fernanda Rojas DiazNessuna valutazione finora
- Calcium HomeostasisDocumento37 pagineCalcium Homeostasispolog.jm610Nessuna valutazione finora
- Mineral Metabolism.Documento26 pagineMineral Metabolism.Shivanand MaliNessuna valutazione finora
- Study Guide For Calcium and Phosphate MetabolismDocumento74 pagineStudy Guide For Calcium and Phosphate MetabolismMohammad MamunuzzamanNessuna valutazione finora
- Parathyroid Hormone: Shahab Ullah Khan Ayub Medical CollegeDocumento28 pagineParathyroid Hormone: Shahab Ullah Khan Ayub Medical CollegeDr KhanNessuna valutazione finora
- Calcium and Phosphorus HomeostasisDocumento3 pagineCalcium and Phosphorus Homeostasisshakila786Nessuna valutazione finora
- Parathyroid HormoneDocumento12 pagineParathyroid HormoneSagar SharmaNessuna valutazione finora
- Calcium HomeostasisDocumento38 pagineCalcium Homeostasiskelvinmaina9993Nessuna valutazione finora
- Parathyroid Hormone, HyperparathyroidismDocumento39 pagineParathyroid Hormone, HyperparathyroidismAris josuaNessuna valutazione finora
- Drugs Affecting Calcium BalanceDocumento63 pagineDrugs Affecting Calcium BalanceRd Chandane100% (1)
- HypoparathyroidismDocumento2 pagineHypoparathyroidismLorelyn Santos CorpuzNessuna valutazione finora
- Calcium MetabolismDocumento29 pagineCalcium MetabolismsnehaNessuna valutazione finora
- Regulation of Calcium Parathyroid, Vitamin D & CalcitoninDocumento29 pagineRegulation of Calcium Parathyroid, Vitamin D & CalcitoninJessica StewartNessuna valutazione finora
- 5 Parathyroid GlandDocumento24 pagine5 Parathyroid GlandReem 10Nessuna valutazione finora
- Parathyroid HormoneDocumento12 pagineParathyroid HormoneJamesNessuna valutazione finora
- Hormonal Control of Calcium Homeostasis Chapter 9Documento8 pagineHormonal Control of Calcium Homeostasis Chapter 9Roua SafwatNessuna valutazione finora
- Calcium Metabolism: DR - Ammar Jawad MBCHB, MPHDocumento54 pagineCalcium Metabolism: DR - Ammar Jawad MBCHB, MPHMurali ManiNessuna valutazione finora
- Hypercalcemia (F&e)Documento3 pagineHypercalcemia (F&e)Sarah Grace CajucomNessuna valutazione finora
- Parathyroid Hormone PDFDocumento120 pagineParathyroid Hormone PDFLaura TapiaNessuna valutazione finora
- PP 6 CalciumDocumento28 paginePP 6 Calciumnurina_drNessuna valutazione finora
- Disorders of CA+ MetabolismDocumento41 pagineDisorders of CA+ MetabolismSuliman GarallehNessuna valutazione finora
- Hypercalcemia in Dogs Emergent Care Diagnostics and TreatmentsDocumento8 pagineHypercalcemia in Dogs Emergent Care Diagnostics and Treatmentstarilubis277Nessuna valutazione finora
- Calcium Metabolism: Presented by Ch. Likhita 1 Year P.GDocumento113 pagineCalcium Metabolism: Presented by Ch. Likhita 1 Year P.GLikhita ChNessuna valutazione finora
- Theo FactsDocumento2 pagineTheo FactsMika Sophia GonzagaNessuna valutazione finora
- Technique and Style in Painting: Humanities 100Documento51 pagineTechnique and Style in Painting: Humanities 100Mika Sophia GonzagaNessuna valutazione finora
- Nucleotide - Monomer of Nucleic AcidsDocumento2 pagineNucleotide - Monomer of Nucleic AcidsMika Sophia GonzagaNessuna valutazione finora
- Blubber Boy's Anaphy Report FinalDocumento2 pagineBlubber Boy's Anaphy Report FinalMika Sophia GonzagaNessuna valutazione finora
- Name: Mika Sophia G. Gonzaga Section: Bsn-1B ScoreDocumento1 paginaName: Mika Sophia G. Gonzaga Section: Bsn-1B ScoreMika Sophia GonzagaNessuna valutazione finora
- Quantitative ExerciseDocumento11 pagineQuantitative ExerciseMika Sophia GonzagaNessuna valutazione finora
- Practical ResearchDocumento31 paginePractical ResearchMika Sophia GonzagaNessuna valutazione finora
- RPH Notes For ReportingDocumento10 pagineRPH Notes For ReportingMika Sophia Gonzaga100% (1)
- Chapter 12,13Documento2 pagineChapter 12,13Mamoona KambohNessuna valutazione finora
- Cellular Respiration DefinitionDocumento9 pagineCellular Respiration Definitionmaria genioNessuna valutazione finora
- DLP MitosisDocumento6 pagineDLP MitosisAlleen Joy Solivio100% (2)
- 2 Prebiotics and Probiotics - Modifying and Mining The Microbiota PDFDocumento6 pagine2 Prebiotics and Probiotics - Modifying and Mining The Microbiota PDFvanessaNessuna valutazione finora
- Science 8 - BiodiversityDocumento26 pagineScience 8 - BiodiversityJean Marie Macadaeg Ordinario100% (1)
- mRNA Vaccines A New Era in VaccinologyDocumento19 paginemRNA Vaccines A New Era in Vaccinologyedysson1Nessuna valutazione finora
- Directorate of Distance Education: Sri Venkateswara University:: TirupatiDocumento15 pagineDirectorate of Distance Education: Sri Venkateswara University:: TirupatiRajNessuna valutazione finora
- M.Sc. Microbiology (Part-II) (For Dept. of Microbioloy, SPPU) - 28092021Documento12 pagineM.Sc. Microbiology (Part-II) (For Dept. of Microbioloy, SPPU) - 28092021Dolly ChhajedNessuna valutazione finora
- Musculoskeletal Anatomy and PhysiologyDocumento26 pagineMusculoskeletal Anatomy and PhysiologyAmy92% (13)
- Diabetic NephropathyDocumento41 pagineDiabetic NephropathyBen IntosiusNessuna valutazione finora
- Endocrine System-Worksheet MTIDocumento4 pagineEndocrine System-Worksheet MTIKolynNessuna valutazione finora
- Leukosit: - Leukopoiesis Proses Pembentukan Leukosit - Sel Seri LeukositDocumento44 pagineLeukosit: - Leukopoiesis Proses Pembentukan Leukosit - Sel Seri LeukositAyu RahayuNessuna valutazione finora
- Neurobiology of Cancer Interactions Between Nervous, Endocrine and Immune Systems As A Base For Monitoring and Modulating The Tumorigenesis by The BrainDocumento15 pagineNeurobiology of Cancer Interactions Between Nervous, Endocrine and Immune Systems As A Base For Monitoring and Modulating The Tumorigenesis by The BrainSaurabh Gayali100% (2)
- Sangre de GradoDocumento7 pagineSangre de GradoChristian Trujillo CollantesNessuna valutazione finora
- Science 9 W1-W4Documento21 pagineScience 9 W1-W4Jennifer Lacadue Masoa - LumantasNessuna valutazione finora
- Mic 1 - Microbiology and Parasitology (Lecture) Assignment No. 1: Introduction To MicrobiologyDocumento2 pagineMic 1 - Microbiology and Parasitology (Lecture) Assignment No. 1: Introduction To MicrobiologyRica AngelesNessuna valutazione finora
- Vegetative PropagationDocumento23 pagineVegetative PropagationAaron DizonNessuna valutazione finora
- Anatomy and Physiology of GITDocumento4 pagineAnatomy and Physiology of GITyassyrnNessuna valutazione finora
- Malamed Local Anesthesia - 1Documento100 pagineMalamed Local Anesthesia - 1Ines delacroix33% (3)
- Origin of MetazoaDocumento4 pagineOrigin of MetazoaAmod KumarNessuna valutazione finora
- Activated Sludge Troubleshooting ChartDocumento1 paginaActivated Sludge Troubleshooting ChartIslandHighlander100% (2)
- Guilbert Et Al., 2012Documento17 pagineGuilbert Et Al., 2012Alfredo PerettiNessuna valutazione finora
- BTBC209IU Biochemistry 1: International UniversityDocumento33 pagineBTBC209IU Biochemistry 1: International UniversityLinhNguyeNessuna valutazione finora
- MBoC5e - CHPT - 13 Intracellular Vesicular TrafficDocumento111 pagineMBoC5e - CHPT - 13 Intracellular Vesicular TrafficAnnisaazharNessuna valutazione finora
- Akasg Biology Investigatory Project 12Documento14 pagineAkasg Biology Investigatory Project 12kanishkaran67% (3)
- Virulence: Factors in Escherichia Coli Urinary Tract InfectionDocumento49 pagineVirulence: Factors in Escherichia Coli Urinary Tract Infectionfajar nugrahaNessuna valutazione finora
- Ans 201 Anatomy and Physiology of Farm AnimalsDocumento33 pagineAns 201 Anatomy and Physiology of Farm AnimalsAdewaleNessuna valutazione finora
- Assignment No. 01: Human Digestive System and Respiratory SystemDocumento3 pagineAssignment No. 01: Human Digestive System and Respiratory SystemZIA UR REHMANNessuna valutazione finora
- Nirlife Critical Care ProductsDocumento4 pagineNirlife Critical Care ProductsManpreet Sachdeva100% (1)
- What Professor Armand Marie Leroi Doesn't KnowDocumento1 paginaWhat Professor Armand Marie Leroi Doesn't Know'Messianic' DylanologistNessuna valutazione finora
- ICH Quality Guidelines: An Implementation GuideDa EverandICH Quality Guidelines: An Implementation GuideAndrew TeasdaleNessuna valutazione finora
- The Nature of Drugs Vol. 1: History, Pharmacology, and Social ImpactDa EverandThe Nature of Drugs Vol. 1: History, Pharmacology, and Social ImpactValutazione: 5 su 5 stelle5/5 (5)
- Periodic Tales: A Cultural History of the Elements, from Arsenic to ZincDa EverandPeriodic Tales: A Cultural History of the Elements, from Arsenic to ZincValutazione: 3.5 su 5 stelle3.5/5 (137)
- The Regenerative Grower's Guide to Garden Amendments: Using Locally Sourced Materials to Make Mineral and Biological Extracts and FermentsDa EverandThe Regenerative Grower's Guide to Garden Amendments: Using Locally Sourced Materials to Make Mineral and Biological Extracts and FermentsValutazione: 5 su 5 stelle5/5 (3)
- The Production of Volatile Oils and Perfumery Plants in the United StatesDa EverandThe Production of Volatile Oils and Perfumery Plants in the United StatesNessuna valutazione finora
- Chemistry for Breakfast: The Amazing Science of Everyday LifeDa EverandChemistry for Breakfast: The Amazing Science of Everyday LifeValutazione: 4.5 su 5 stelle4.5/5 (14)
- AP® Chemistry Crash Course, For the 2020 Exam, Book + Online: Get a Higher Score in Less TimeDa EverandAP® Chemistry Crash Course, For the 2020 Exam, Book + Online: Get a Higher Score in Less TimeValutazione: 5 su 5 stelle5/5 (1)
- It's Elemental: The Hidden Chemistry in EverythingDa EverandIt's Elemental: The Hidden Chemistry in EverythingValutazione: 4 su 5 stelle4/5 (10)
- Taste: Surprising Stories and Science About Why Food Tastes GoodDa EverandTaste: Surprising Stories and Science About Why Food Tastes GoodValutazione: 3 su 5 stelle3/5 (20)
- Lead with Your Heart: Lessons from a Life with HorsesDa EverandLead with Your Heart: Lessons from a Life with HorsesValutazione: 4 su 5 stelle4/5 (8)
- Monkeys, Myths, and Molecules: Separating Fact from Fiction, and the Science of Everyday LifeDa EverandMonkeys, Myths, and Molecules: Separating Fact from Fiction, and the Science of Everyday LifeValutazione: 4 su 5 stelle4/5 (1)
- Guidelines for Defining Process Safety Competency RequirementsDa EverandGuidelines for Defining Process Safety Competency RequirementsValutazione: 3 su 5 stelle3/5 (1)
- Chemistry for Breakfast: The Amazing Science of Everyday LifeDa EverandChemistry for Breakfast: The Amazing Science of Everyday LifeValutazione: 4.5 su 5 stelle4.5/5 (90)
- Is That a Fact?: Frauds, Quacks, and the Real Science of Everyday LifeDa EverandIs That a Fact?: Frauds, Quacks, and the Real Science of Everyday LifeValutazione: 5 su 5 stelle5/5 (4)
- Tribology: Friction and Wear of Engineering MaterialsDa EverandTribology: Friction and Wear of Engineering MaterialsValutazione: 5 su 5 stelle5/5 (1)
- Project Solomon: The True Story of a Lonely Horse Who Found a Home--and Became a HeroDa EverandProject Solomon: The True Story of a Lonely Horse Who Found a Home--and Became a HeroValutazione: 5 su 5 stelle5/5 (9)
- AP Chemistry Flashcards, Fourth Edition: Up-to-Date Review and PracticeDa EverandAP Chemistry Flashcards, Fourth Edition: Up-to-Date Review and PracticeNessuna valutazione finora
- Handbook of Formulating Dermal Applications: A Definitive Practical GuideDa EverandHandbook of Formulating Dermal Applications: A Definitive Practical GuideNessuna valutazione finora
- Essential Chemistry for Formulators of Semisolid and Liquid DosagesDa EverandEssential Chemistry for Formulators of Semisolid and Liquid DosagesValutazione: 5 su 5 stelle5/5 (2)
- Organic Chemistry for Schools: Advanced Level and Senior High SchoolDa EverandOrganic Chemistry for Schools: Advanced Level and Senior High SchoolNessuna valutazione finora
- Formulating, Packaging, and Marketing of Natural Cosmetic ProductsDa EverandFormulating, Packaging, and Marketing of Natural Cosmetic ProductsNessuna valutazione finora
- The Nature of Drugs Vol. 1: History, Pharmacology, and Social ImpactDa EverandThe Nature of Drugs Vol. 1: History, Pharmacology, and Social ImpactValutazione: 5 su 5 stelle5/5 (1)