Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Arthroscopic Drilling For The Treatment of Osteochondral Lesions of The Talus
Caricato da
Anonymous kdBDppigETitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Arthroscopic Drilling For The Treatment of Osteochondral Lesions of The Talus
Caricato da
Anonymous kdBDppigECopyright:
Formati disponibili
Arthroscopic Drilling for the Treatment of
Osteochondral Lesions of the Talus*
BY TSUKASA KUMAI, M.D., PH.D.†, YOSHINORI TAKAKURA, M.D., PH.D.†,
ICHIRO HIGASHIYAMA, M.D.†, AND SUSUMU TAMAI, M.D., PH.D.†, NARA, JAPAN
Investigation performed at Nara Medical University, Nara
Abstract operative immobilization; thus, the procedure is less
Background: An osteochondral lesion of the talus invasive than other types of operative treatment for the
is a relatively rare disorder of the ankle. While a num- condition and it allows early resumption of daily activ-
ber of treatment options have been reported, it appears ities and sports. On the basis of the results in this study,
to be difficult to manage all lesions with a single ap- we believe that the procedure is effective and useful in
proach. We evaluated the indications for and the results young patients, especially those who have not yet had
of arthroscopic drilling for the treatment of an os- closure of the epiphyseal plate. A specific indication
teochondral lesion of the talus. for the procedure is an early lesion with only mild
Methods: Eighteen ankles (seventeen patients) with osteosclerosis of the surrounding talar bone, continuity
a symptomatic osteochondral lesion of the talus were of the cartilaginous surface, and stability of the os-
examined. The ages of the patients ranged from ten to teochondral fragment.
seventy-eight years (mean, 28.0 years) at the time of the
operation, and the patients were followed postopera- An osteochondral lesion of the talus appears to be
tively for two to 9.5 years (mean, 4.6 years). After the a relatively rare disorder and, although many patients
continuity of the cartilage overlying the lesion and the have a history of trauma, the etiology remains largely
stability of the lesion had been confirmed, arthroscopic unknown1,4,15. The principles of treatment of this con-
drilling was performed with use of a Kirschner wire that dition have been well established since the description
was 1.0 to 1.2 millimeters in diameter. A cast was not by Berndt and Harty4 in 1959, and a number of treat-
applied postoperatively, and full weight-bearing was al- ment methods have been reported1-4,6,8-10,12-14,16. Berndt and
lowed six weeks after the procedure. Harty classified the lesions into four stages. Stage I in-
Results: The clinical result was good for thirteen dicates a small area of compression of subchondral
ankles and fair for five; all ankles had improvement. bone; stage II, a partially detached osteochondral frag-
Twelve of the thirteen ankles that were in patients who ment; stage III, a completely detached osteochondral
were less than thirty years old had a good result. In fragment that remains in the talar crater; and stage IV,
contrast, only one of the five ankles in patients who a displaced osteochondral fragment. Treatment is most
were fifty years old or more had a good result. Thus, commonly based on this radiographic classification
the clinical results tended to be better for younger system. Subsequent studies4,6,14 have supported this ap-
patients. Improvement was seen radiographically in fif- proach, which involves a trial of nonoperative treatment
teen ankles. However, the three ankles in patients who for stage-I and II and medial stage-III lesions and oper-
were more than sixty years old were found to have no ative treatment for lateral stage-III lesions and stage-IV
improvement on radiographic examination. Analysis of lesions. We have evaluated the treatment of osteochon-
the group of patients who had a history of trauma dral lesions of the talus in many patients, and currently
revealed that the mean interval between the injury and we do not believe that a single approach can be applied
the operation was 6.3 months for the three ankles that to all lesions; instead, an appropriate treatment must be
had a good radiographic result and 11.3 months for selected from the various alternatives for each patient.
the six that had a fair result. Thus, the radiographic Of these alternatives, arthroscopic drilling is simple, is
results tended to be better when the interval between less invasive than other types of operative treatment,
the injury and the operation was shorter. and necessitates a short duration of hospitalization; thus,
Conclusions: Arthroscopic drilling for the treat- it is considered to be highly advantageous, especially for
ment of medial osteochondral lesions of the talus does students and athletes. In this study, we evaluated the
not require osteotomy of the medial malleolus or post- specific indications for and the results of this procedure.
Materials and Methods
*No benefits in any form have been received or will be received
from a commercial party related directly or indirectly to the subject
Seventeen (six male and eleven female) patients with
of this article. No funds were received in support of this study. eighteen affected ankles were evaluated (Table I). Their
†Department of Orthopaedic Surgery, Nara Medical University, ages ranged from ten to seventy-eight years (mean, 28.0
840 Shijyo-cho, Kashihara, Nara 634-8522, Japan.
years) at the time of the operation, and they were fol-
Copyright 1999 by The Journal of Bone and Joint Surgery, Incorporated lowed postoperatively for two to 9.5 years (mean, 4.6
VOL. 81-A, NO. 9, SEPTEMBER 1999 1229
1230 TSUKASA KUMAI, YOSHINORI TAKAKURA, ICHIRO HIGASHIYAMA, AND SUSUMU TAMAI
TABLE I
PATIENT DEMOGRAPHICS AND RESULTS
Gender, History of Duration of Site of Duration of Clinical Radiographic
Case Age at Op. Trauma Symptoms* Lesion Stage4 Follow-up Result Result
(yrs.) (mos.) (mos.)
1 M, 15 Yes 1 Medial II 114 Good Good
2 M, 27 Yes 4 Medial II 100 Good Good
3 F, 13 No 13 Medial II 84 Good Fair
4 F, 50 No 39 Medial II 66 Fair Fair
5 F, 62 No 62 Medial II 64 Fair Poor
6 F, 66 No 38 Medial II 64 Fair Poor
7 F, 10 No 27 Medial II 60 Good Good
12 No 51 Medial II 36 Good Fair
8 F, 78 Yes NA Medial II 60 Fair Poor
9 F, 13 No 26 Medial II 48 Good Fair
10 M, 13 Yes 12 Medial II 42 Good Fair
11 F, 22 No 15 Medial II 42 Good Fair
12 M, 50 Yes 1.5 Medial II 41 Good Fair
13 M, 16 Yes 14 Medial II 40 Good Good
14 F, 13 Yes 18 Medial II 36 Good Fair
15 F, 15 Yes 6 Medial II 36 Good Fair
16 M, 13 Yes 6 Medial II 30 Good Fair
17 F, 16 Yes 24 Medial II 24 Fair Fair
*NA = not available.
years). Ten patients (ten ankles) had a clear history of large unstable fragment, the fragment was reduced and
trauma, and seven patients (eight ankles) did not. Of fixed with bone pegs in an open operation. Seventeen
the patients who had a history of trauma, nine had an patients (the study group) were managed with arthro-
inversion injury; three (Cases 1, 13, and 14) of the nine scopic drilling; twenty-eight, with excision of the frag-
had been injured during sports activity. The remain- ment; and twenty-seven, with reduction and fixation.
ing patient (Case 8) was seen a long time after the injury, Continuity of the cartilaginous surface and stability of
and she did not remember the details. the osteochondral fragment, confirmed by arthroscopic
The preoperative symptom of the condition was probing, were regarded as essential indications for ar-
usually pain in the ankle joint during or after exercise. throscopic drilling.
In addition, mild swelling was observed in many pa-
tients. The site of the lesion was medial in all ankles. Operative Procedure
According to the radiographic classification system of After induction of spinal or general anesthesia, the
Berndt and Harty4, all of the lesions were stage II. Pre- patient is placed in the supine position with the cal-
operative computed tomography scans were made to caneal region slightly protruding from the end of the
obtain information about the osseous lesion in fourteen operating table to allow free plantar flexion and dorsi-
ankles, and magnetic resonance imaging was performed flexion of the ankle. Although there are reports7,11 of
to evaluate the condition of the bone surrounding the skeletal traction being used to widen the joint space, we
lesion in thirteen ankles. do not use that technique because the joint space is
The seventeen patients were among a group of relatively wide in patients who have this disease, most
seventy-two patients with an osteochondral lesion of of whom are young, and because the lesions are so small
the talus for whom we considered operative treatment that skilled manual manipulation is needed for drilling.
with one of three operative procedures: excision of the A medial portal adjacent to the anterior tibial tendon
osteochondral fragment and curettage, reduction and is used, and a 2.7-millimeter-diameter arthroscope is in-
fixation of the osteochondral fragment with bone pegs, serted. As the lesions are frequently located in the me-
and arthroscopic drilling. As the stability of the lesion dial aspect of the talar dome, they are examined with
cannot be determined on the basis of plain radiographs the ankle joint in plantar flexion. If the junction between
alone, arthroscopic viewing and probing are essential. the lesion and the normal area cannot be determined
Diagnostic arthroscopy was first performed in all pa- with arthroscopic viewing alone, probing of the carti-
tients; when intact cartilage over the lesion and a stable laginous surface is helpful because the cartilaginous sur-
fragment were detected with probing, arthroscopic drill- face of the lesion is often softened; when this is the case,
ing was carried out. When a small unstable fragment the tip of the probe dips into the cartilage in the region
was detected arthroscopically, excision of the fragment of the lesion. In addition, the cartilaginous surface is
and curettage was performed. In patients who had a observed with regard to its continuity and signs of de-
THE JOURNAL OF BONE AND JOINT SURGERY
ARTHROSCOPIC DRILLING FOR THE TREATMENT OF OSTEOCHONDRAL LESIONS OF THE TALUS 1231
The arthroscope is immobilized, and a Kirschner
wire, 1.0 to 1.2 millimeters in diameter, is inserted from
about three centimeters proximal to the tip of the me-
dial malleolus and is directed across the medial mal-
leolus into the lesion through the intact cartilage. The
size of the Kirschner wire was selected mainly on
the basis of the size of the injured region. The position
of the Kirschner wire is confirmed with arthroscopy,
and the wire is drilled into the lesion (percutaneous
transmalleolar drilling) (Fig. 1). Under arthroscopy, the
Kirschner wire is withdrawn to the articular surface at
the distal end of the tibia, and drilling is performed at
a few other sites after slightly changing the angle of
plantar flexion or dorsiflexion of the ankle joint. Drill-
ing is continued until healthy bleeding from the bone
marrow or leakage of fat droplets is confirmed. Next,
the angle of insertion of the Kirschner wire is changed,
and the same procedure is repeated. The drilling is
performed at several sites, including areas around the
lesion. The operation is completed by irrigating the ar-
ticular space.
After the operation, no cast is applied and the oper-
ative site is gently compressed by an elastic dressing.
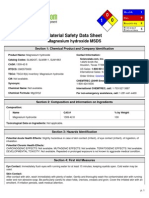
FIG. 1 Plantar flexion and dorsiflexion of the ankle are allowed
Illustration of percutaneous transmalleolar drilling. A Kirschner from the day after the operation, gradual partial weight-
wire, 1.0 to 1.2 millimeters in diameter, is inserted from about three bearing with use of a crutch is initiated at five weeks,
centimeters proximal to the tip of the medial malleolus and is
directed across the medial malleolus into the lesion through the and full weight-bearing is permitted at about six weeks
intact cartilage. Drilling is continued until healthy bleeding from the after the operation. Sports activities are not permitted
bone marrow or leakage of fat droplets is confirmed. for at least two months.
generation, such as fibrillation. The mobility of the os- Results
teochondral fragment in relation to the bone surround- The clinical evaluation was performed according to
ing the lesion and the extent of the lesion are assessed the criteria of Berndt and Harty4. A patient who had
with a probe. occasional symptoms but no disabling pain was consid-
FIG. 2
Graph showing the relationship between the age at the time of the operation and the clinical result. Twelve of the thirteen ankles that had
a good result were in patients who were less than thirty years old.
VOL. 81-A, NO. 9, SEPTEMBER 1999
1232 TSUKASA KUMAI, YOSHINORI TAKAKURA, ICHIRO HIGASHIYAMA, AND SUSUMU TAMAI
FIG. 3
Graph showing the relationship between the age at the time of the operation and the radiographic result. Three of the four ankles that had
a good result were in patients who were less than twenty years old, and all three ankles with a poor result were in patients who were more than
sixty years old.
ered to have a good result. A patient who had a decrease clinical results tended to be better for younger patients
in symptoms but still had some disabling pain was con- (Fig. 2). Ten of the eleven ankles in patients who were
sidered to have a fair result. The result was considered less than twenty years old had a good result.
to be poor if the symptoms had not decreased. The
clinical result was good for thirteen ankles and fair for
five; all ankles had a decrease in the symptoms (Table
I). All thirteen ankles with a good result had recovered
a full range of motion no later than two weeks after the
operation, and the swelling around the ankle had also
decreased. Pain did not recur after walking with full
weight-bearing. The five ankles that were rated as fair
also regained an almost full range of motion two weeks
after the operation. However, four of these five ankles
gradually became slightly swollen again after walking
with weight-bearing was resumed. The five ankles that
were rated as fair were painful after the patients walked
a long distance. Two (Cases 5 and 6) of the five ankles
were painful when the patients went up and down stairs,
and another ankle (Case 17) was slightly painful after
recreational sports. Seven patients (seven ankles) had
engaged in sports as recreational activities before the
operation, and all of them had resumed sports activity
at the time of the evaluation.
Of the ten ankles that had a history of trauma, eight
had a good result and two had a fair result. In con-
trast, of the eight ankles that did not have a history of
trauma, five had a good result and three had a fair
result. Thus, the clinical results tended to be worse for the
ankles that did not have a history of trauma. Of the thir-
teen ankles that were in patients who were less than
thirty years old at the time of the operation, twelve had
FIG. 4-A
a good result. In contrast, only one of the five ankles that
Figs. 4-A, 4-B, and 4-C: Case 7, a ten-year-old girl.
were in patients who were fifty years old or more had Fig. 4-A: Plain radiograph, made at the initial examination, show-
a good result; the other four had a fair result. Thus, the ing irregularity on the medial side of the talar dome (arrow).
THE JOURNAL OF BONE AND JOINT SURGERY
ARTHROSCOPIC DRILLING FOR THE TREATMENT OF OSTEOCHONDRAL LESIONS OF THE TALUS 1233
atively satisfactory9,10,12-14,16. We have encountered more
than 100 osteochondral lesions of the talus. The size
and stability of the lesion, the continuity of the cartilag-
inous surface, and the condition of the talar bone sur-
rounding the lesion have varied among patients, and
it appears to be inappropriate to treat all lesions with
a single approach. In fact, we choose among three op-
tions — excision of the osteochondral fragment, reduc-
tion and fixation of the osteochondral fragment, and
arthroscopic drilling — according to the condition of
the individual lesion, and we have obtained relatively
good results with each procedure. For this reason, care-
ful selection of the type of treatment is important, and
various imaging modalities must be used effectively
to evaluate the condition of the lesion accurately13,15-17.
Computed tomography scans and magnetic resonance
imaging are particularly useful for assessing the fea-
tures of the lesion. Magnetic resonance imaging also
provides information about the condition of the talar
bone surrounding the lesion17. As a discrepancy between
FIG. 4-B
the radiographic staging system of Berndt and Harty4
Arthroscopy showed that, although there was roughness of the
cartilaginous surface (arrows), its continuity was preserved. Mild and the arthroscopic appearance has been reported16,
softening of the cartilage was detected by probing. direct arthroscopic viewing and probing are also im-
portant for selection of the best treatment method.
The radiographic result was considered to be good We perform excision of the osteochondral fragment and
when complete osseous union or ossification was ob- curettage in patients in whom the osteochondral frag-
served, fair when osseous union or ossification was ment is small and completely detached from the talar
incomplete but improved compared with the preopera-
tive finding, and poor when no changes were observed.
The ankles with a fair radiographic result showed some
tendency toward ossification compared with the pre-
operative finding; mainly, the radiolucent zone distal to
the osteochondral fragment tended to disappear. The
radiographic result was good for four ankles, fair for
eleven, and poor for three (Table I). Of the ten ankles
that had a history of trauma, three, six, and one had a
good, fair, and poor result, respectively. In contrast, of
the eight ankles that did not have a history of trauma,
one, five, and two were rated as good, fair, and poor,
respectively. Radiographic results tended to be worse
for patients who did not have a history of trauma.
Three of the four ankles in which complete osseous
union or ossification was observed were in patients
who were less than twenty years old (Figs. 3 through
4-C), and all three of the ankles in which there were
no radiographic changes compared with the preopera-
tive status were in patients who were more than sixty
years old. Analysis of the group that had a history of
trauma showed that the mean interval between the
injury and the operation was 6.3 months for the three
ankles that had a good radiographic result and 11.3
months for the six that had a fair radiographic result.
Discussion
Various operative techniques for the treatment of FIG. 4-C
osteochondral lesions of the talus have been reported, Plain radiograph made one year after arthroscopic drilling. Heal-
and the results of each type of treatment have been rel- ing is complete.
VOL. 81-A, NO. 9, SEPTEMBER 1999
1234 TSUKASA KUMAI, YOSHINORI TAKAKURA, ICHIRO HIGASHIYAMA, AND SUSUMU TAMAI
bone. We also carry out open reduction and fixation of of the medial malleolus or of the dome of the talus.
large unstable osteochondral fragments, which allows There have been recent reports on the use of retro-
direct observation of the condition of the lesion and grade transtalar drilling that does not injure normal car-
the talar bone as well as the most accurate morpholog- tilage8. Recently, we also have been using retrograde
ical repair of the articular surface. However, when the transtalar drilling, but we have managed only a small
lesion is located on the posteromedial side, osteotomy number of patients and the duration of postoperative
of the medial malleolus may be required to expose follow-up is short. This procedure may become more
the lesion. Moreover, immobilization in a cast and non- popular in the near future.
weight-bearing are needed for approximately five and In the present study, the clinical and radiographic
ten weeks, respectively, and some bone atrophy is in- results tended to be better for patients who had a history
evitable10,12,13. Removal of the internal fixation is also of trauma. This may be due to the fact that, when there
necessary after bone union. In contrast, arthroscopic is no history of trauma, there is a long duration of symp-
drilling does not require osteotomy of the medial mal- toms with a resultant poor situation for remodeling be-
leolus or postoperative immobilization in a cast, so the cause of the sclerotic changes surrounding the lesion.
procedure is less invasive and allows early resumption Patients who did have a history of trauma but a longer
of daily activities and sports2,8,10,13-16. period between the injury and the operation also had
The consistency of the results of this procedure must less radiographic improvement. Many patients who
still be evaluated, but fairly good results can be obtained were managed long after the injury had sclerotic talar
if the patients are selected carefully. We performed this bone surrounding the lesion; this sclerosis is represented
procedure in patients in whom the continuity of the as an osteosclerotic image on radiographs and as a rel-
cartilaginous surface and the stability of the lesion had atively wide low-intensity area on T1-weighted mag-
been confirmed arthroscopically. Angermann and Jen- netic resonance images. Therefore, such patients may
sen2 believed that, if the overlying articular cartilage have extensive avascularity in the region of the lesion.
appears intact, then drilling into the lesion through the Destruction of the sclerotic bone must be ensured at the
cartilage is adequate treatment. However, on the basis time of the operation to induce reestablishment of the
of the results of the present study, this procedure ap- blood flow. The effects of drilling from above the osteo-
pears to be ineffective in middle-aged and older individ- chondral fragment alone may be limited in such patients.
uals who have a reduced ability to regenerate bone. Our results suggest that arthroscopic drilling, which
Particularly, when a patient has a subchondral bone is less invasive than other operative treatments and
cyst, filling in of bone is unlikely to be induced by, and can be performed with short hospitalization, should be
no radiographic improvement is expected from, drilling considered first for young patients who have an osteo-
from the articular surface alone, even if the continuity chondral lesion of the talus. A specific indication for this
of the cartilaginous surface is maintained. Although procedure is an early osteochondral lesion with only
no patient who had a subchondral cyst was included in mild osteosclerosis of the surrounding talar bone, conti-
this series, we previously performed drilling in an el- nuity of the cartilaginous surface, and stability of the
derly woman who had intact cartilage overlying a sub- osteochondral fragment.
chondral cyst. Filling in of bone was not observed after In conclusion, arthroscopic drilling for patients who
the operation, and the patient did not have a good result. are less than thirty years old has a major advantage
In contrast, this procedure is markedly effective and compared with the traditional osteotomy of the medial
useful in young patients, especially those who have not malleolus, as it allows early mobilization and return to
yet had closure of the epiphyseal plate5. With modern the preinjury status. An early stable osteochondral le-
techniques (arthroscopy and fluoroscopy), we can drill sion in a young patient should be considered an absolute
into the bone without crossing normal cartilage, either indication for the procedure.
References
1. Alexander, A. H., and Lichtman, D. M.: Operative treatment of transchondral talar-dome fractures (osteochondritis dissecans). Long-
term follow-up. J. Bone and Joint Surg., 62-A: 646-652, June 1980.
2. Angermann, P., and Jensen, P.: Osteochondritis dissecans of the talus: long-term results of operative treatment. Foot and Ankle, 10:
161-163, 1989.
3. Bauer, M.; Jonsson, K.; and Lindén, B.: Osteochondritis dissecans of the ankle. A 20-year follow-up study. J. Bone and Joint Surg.,
69-B(1): 93-96, 1987.
4. Berndt, A. L., and Harty, M.: Transchondral fractures (osteochondritis dissecans) of the talus. J. Bone and Joint Surg., 41-A: 988-1020,
Sept. 1959.
5. Bradley, J., and Dandy, D. J.: Results of drilling osteochondritis dissecans before skeletal maturity. J. Bone and Joint Surg., 71-B(4):
642-644, 1989.
6. Canale, S. T., and Belding, R. H.: Osteochondral lesions of the talus. J. Bone and Joint Surg., 62-A: 97-102, Jan. 1980.
7. Ferkel, R. D., and Fischer, S. P.: Progress in ankle arthroscopy. Clin. Orthop., 240: 210-220, 1989.
8. Ferkel, R. D.: Osteochondral lesions of the talus. In Arthroscopic Surgery: the Foot and Ankle, pp. 145-170. Edited by T. L. Whipple. Phil-
adelphia, Lippincott-Raven, 1996.
THE JOURNAL OF BONE AND JOINT SURGERY
ARTHROSCOPIC DRILLING FOR THE TREATMENT OF OSTEOCHONDRAL LESIONS OF THE TALUS 1235
9. Flick, A. B., and Gould, N.: Osteochondritis dissecans of the talus (transchondral fractures of the talus): review of the literature and new
operative approach for medial dome lesions. Foot and Ankle, 5: 165-185, 1985.
10. Frank, A.; Cohen, P.; Beaufils, P.; and Lamare, J.: Arthroscopic treatment of osteochondral lesions of the talar dome. Arthroscopy, 5:
57-61, 1989.
11. Guhl, J. F.: New concepts (distraction) in ankle arthroscopy. Arthroscopy, 4: 160-167, 1988.
12. O’Farrell, T. A., and Costello, B. G.: Osteochondritis dissecans of the talus. The late results of surgical treatment. J. Bone and Joint Surg.,
64-B(4): 494-497, 1982.
13. Parisien, J. S.: Arthroscopic treatment of osteochondral lesions of the talus. Am. J. Sports Med., 14: 211-217, 1986.
14. Pritsch, M.; Horoshovski, H.; and Farine, I.: Arthroscopic treatment of osteochondral lesions of the talus. J. Bone and Joint Surg., 68-A:
862-865, July 1986.
15. Shea, M. P., and Manoli, A., II: Osteochondral lesions of the talar dome. Foot and Ankle, 14: 48-55, 1993.
16. Van Buecken, K.; Barrack, R. L.; Alexander, A. H.; and Ertl, J. P.: Arthroscopic treatment of transchondral talar dome fractures. Am. J.
Sports Med., 17: 350-356, 1989.
17. Yulish, B. S.; Mulopulos, G. P.; Goodfellow, D. B.; Bryan, P. J.; Modic, M. T.; and Dollinger, B. M.: MR imaging of osteochondral lesions
of the talus. J. Comput. Assist. Tomog., 11: 296-301, 1987.
VOL. 81-A, NO. 9, SEPTEMBER 1999
Potrebbero piacerti anche
- A Case-Based Guide To Clinical Endocrinology (October 23, 2015) - (1493920588) - (Springer)Documento434 pagineA Case-Based Guide To Clinical Endocrinology (October 23, 2015) - (1493920588) - (Springer)AbdulraHman KhalEd100% (2)
- Young FrankensteinDocumento109 pagineYoung FrankensteinColleen Hawks-Pierce83% (6)
- Psychiatric Case History NotesDocumento8 paginePsychiatric Case History NotesTysle100% (1)
- Microsoft Word Document جديدDocumento3 pagineMicrosoft Word Document جديدHisham EssamNessuna valutazione finora
- Long-Term Stability Alter Orthodontic Treatment - Nonextraction With Prolonged RetentionDocumento7 pagineLong-Term Stability Alter Orthodontic Treatment - Nonextraction With Prolonged RetentionRenan VeigaNessuna valutazione finora
- Pelet 2006 Bankart repair for recurrent anterior glenohumeral instability- Results at twenty-nine years’ follow-upDocumento5 paginePelet 2006 Bankart repair for recurrent anterior glenohumeral instability- Results at twenty-nine years’ follow-uptheorthopaedistNessuna valutazione finora
- J Joms 2008 01 046Documento10 pagineJ Joms 2008 01 046Delta JackNessuna valutazione finora
- Articulo 2Documento4 pagineArticulo 2TOMAS DAVID CHICA LLAMASNessuna valutazione finora
- Radial Nerve PalsyDocumento4 pagineRadial Nerve PalsyRamziNessuna valutazione finora
- To Evaluate The Functional Outcome of Volar Plating in Distal End Radius FracturesDocumento11 pagineTo Evaluate The Functional Outcome of Volar Plating in Distal End Radius FracturesIJAR JOURNALNessuna valutazione finora
- Low-Dose External Beam Radiotherapy As A Postoperative Treatment For Patients With Diffuse Pigmented Villonodular Synovitis of The KneeDocumento6 pagineLow-Dose External Beam Radiotherapy As A Postoperative Treatment For Patients With Diffuse Pigmented Villonodular Synovitis of The Kneekrishivpatel27Nessuna valutazione finora
- The Role of Cervical Headgear and Lower Utility Arch in The Control of The Vertical DimensionDocumento10 pagineThe Role of Cervical Headgear and Lower Utility Arch in The Control of The Vertical Dimensionnadia Tovar GarciaNessuna valutazione finora
- Shan 2018Documento4 pagineShan 2018pancholin_9Nessuna valutazione finora
- Ulnar Stiloid K - R - N - N e - Lik Etti - I Distal Radius K - R - Klar - N - N de - Erlendirilmesinde Yeni Bir Indeks (#191560) - 169235Documento5 pagineUlnar Stiloid K - R - N - N e - Lik Etti - I Distal Radius K - R - Klar - N - N de - Erlendirilmesinde Yeni Bir Indeks (#191560) - 169235Christopher Freddy Bermeo RiveraNessuna valutazione finora
- Operative Treatment of Terrible Triad of TheDocumento8 pagineOperative Treatment of Terrible Triad of TheAndrea OsborneNessuna valutazione finora
- Head Gear Effect - PancherzDocumento11 pagineHead Gear Effect - PancherzSrishti SyalNessuna valutazione finora
- Paper PublicationDocumento10 paginePaper PublicationabhijeethjainNessuna valutazione finora
- A Clinical Study On Ankylosis of The Temporomandibular Joint PARA ODONTO 1 2007-1Documento7 pagineA Clinical Study On Ankylosis of The Temporomandibular Joint PARA ODONTO 1 2007-1Sitta Itu NanaNessuna valutazione finora
- Abstracts: Kurz Implants, Precision Instruments, Ventilation TubesDocumento32 pagineAbstracts: Kurz Implants, Precision Instruments, Ventilation TubesMarcos PauloNessuna valutazione finora
- Closed Intra - Articular Fractures of The Distal End of Humerus Surgically Treated by Trans - Olecranon Approach Using The Chevron OsteotomyDocumento4 pagineClosed Intra - Articular Fractures of The Distal End of Humerus Surgically Treated by Trans - Olecranon Approach Using The Chevron OsteotomyIJAR JOURNALNessuna valutazione finora
- Treatment of Old Unreduced Posterior Dislocation of ElbowDocumento4 pagineTreatment of Old Unreduced Posterior Dislocation of Elbowwenny hildaNessuna valutazione finora
- Nailing and Plating As Fixation of Humeral Shaft FracturesDocumento6 pagineNailing and Plating As Fixation of Humeral Shaft FracturesIJAR JOURNALNessuna valutazione finora
- Editorial: Orbital "Blowout" Fractures: Time For A New ParadigmDocumento3 pagineEditorial: Orbital "Blowout" Fractures: Time For A New ParadigmMaria MiripNessuna valutazione finora
- Dental Arch Widths and Mandibular Base Width in Class III MalocclusionsDocumento6 pagineDental Arch Widths and Mandibular Base Width in Class III MalocclusionsShiva PrasadNessuna valutazione finora
- Distinguishing Benign Notochordal Cell Tumors From Vertebral ChordomaDocumento9 pagineDistinguishing Benign Notochordal Cell Tumors From Vertebral ChordomaOM JHANessuna valutazione finora
- Tamai Zone 1 Fingertip Amputation: Reconstruction Using A Digital Artery Flap Compared With Microsurgical ReplantationDocumento7 pagineTamai Zone 1 Fingertip Amputation: Reconstruction Using A Digital Artery Flap Compared With Microsurgical ReplantationFeliciaDewiNessuna valutazione finora
- Class II Malocclusion Treatment With The Herbst Appliance in Patients After The Growth PeakDocumento8 pagineClass II Malocclusion Treatment With The Herbst Appliance in Patients After The Growth PeakHelenaNessuna valutazione finora
- Jurnal Ortho 12Documento4 pagineJurnal Ortho 12Santika IndahsariNessuna valutazione finora
- Cranifaringioma 1Documento13 pagineCranifaringioma 1Oka Iramda SaputraNessuna valutazione finora
- Cephalometric changes with open bite bionatorDocumento8 pagineCephalometric changes with open bite bionatorLiceth Herrera MartinezNessuna valutazione finora
- IJAJR 2018 Long Term Functional Outcomes of The Terrible Triad of The ElbowDocumento6 pagineIJAJR 2018 Long Term Functional Outcomes of The Terrible Triad of The ElbowAndrea OsborneNessuna valutazione finora
- Investigation of Free-Flap Transfer Reconstruction in Elderly Patients and Oral Intake FunctionDocumento3 pagineInvestigation of Free-Flap Transfer Reconstruction in Elderly Patients and Oral Intake Functioncusom34Nessuna valutazione finora
- Parker 1995Documento12 pagineParker 1995Juliana ÁlvarezNessuna valutazione finora
- Magnetic BBDocumento7 pagineMagnetic BBVicente ContrerasNessuna valutazione finora
- Delir 2013Documento7 pagineDelir 2013Karam EidNessuna valutazione finora
- Conunterclock WiseDocumento5 pagineConunterclock WiseEduardo HernándezNessuna valutazione finora
- 2009 - Bosch Osteotomy Vs Scarf in Hallux ValgusDocumento10 pagine2009 - Bosch Osteotomy Vs Scarf in Hallux ValgusMiguel Angel Palacios FloresNessuna valutazione finora
- Long-Term Benefits of Early Treatment for Pseudo Class III MalocclusionDocumento8 pagineLong-Term Benefits of Early Treatment for Pseudo Class III MalocclusionManena RivoltaNessuna valutazione finora
- Injury: Jérôme Pierrart, Thierry Bégué, Pierre Mansat, GeecDocumento5 pagineInjury: Jérôme Pierrart, Thierry Bégué, Pierre Mansat, GeecJair FigueroaNessuna valutazione finora
- Freitas 2017Documento17 pagineFreitas 2017Anupama Jessica HenryNessuna valutazione finora
- Clinicoradiological and Functional Outcomes of Lisfranc Injuries Managed by Different Treatment Modalities in A Tertiary Care CentreDocumento7 pagineClinicoradiological and Functional Outcomes of Lisfranc Injuries Managed by Different Treatment Modalities in A Tertiary Care CentreIJAR JOURNALNessuna valutazione finora
- Hand OITE - 2012 2013 2014Documento209 pagineHand OITE - 2012 2013 2014Sadiq AliNessuna valutazione finora
- A Long Term Follow Up Study of Total Meniscectomy.30Documento5 pagineA Long Term Follow Up Study of Total Meniscectomy.30Anshal GuptaNessuna valutazione finora
- Congenital Postero-Medial Bowing of The Tibia and Fibula: Is Early Surgery Worthwhile?Documento8 pagineCongenital Postero-Medial Bowing of The Tibia and Fibula: Is Early Surgery Worthwhile?Kaustubh KeskarNessuna valutazione finora
- A Comparative Study of Management of Closed & Comminuted Distal TibialFractures With Intramedullary Inter Locking Nail Vs MIPODocumento8 pagineA Comparative Study of Management of Closed & Comminuted Distal TibialFractures With Intramedullary Inter Locking Nail Vs MIPOInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- AJODO-2013 Hodges 143 5 665Documento10 pagineAJODO-2013 Hodges 143 5 665player osamaNessuna valutazione finora
- Sipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A ProsDocumento9 pagineSipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A Prossteven saputraNessuna valutazione finora
- Diafiza Femurala Intramedular NailingDocumento4 pagineDiafiza Femurala Intramedular NailingAnuta GiurgiNessuna valutazione finora
- 2013artpolsi ActaBiomedicaDocumento7 pagine2013artpolsi ActaBiomedicaAli MoustafaNessuna valutazione finora
- Journal Homepage: - : Manuscript HistoryDocumento8 pagineJournal Homepage: - : Manuscript HistoryIJAR JOURNALNessuna valutazione finora
- A Bent Needle Tip During Irrigation For Enchondroma of The Distal Phalanx: A New Curettage ToolDocumento9 pagineA Bent Needle Tip During Irrigation For Enchondroma of The Distal Phalanx: A New Curettage ToolusmandumassarNessuna valutazione finora
- Schimming, Eckelt e Kittner (1999) The Value of Coronal Computer Tomograms in Fractures of The Mandibular Condylar ProcessDocumento8 pagineSchimming, Eckelt e Kittner (1999) The Value of Coronal Computer Tomograms in Fractures of The Mandibular Condylar ProcessSamádhi FugitaNessuna valutazione finora
- Iwanaga 2017Documento5 pagineIwanaga 2017zj7n2rhtb4Nessuna valutazione finora
- 10 1016@j Jcms 2020 09 007Documento6 pagine10 1016@j Jcms 2020 09 007Sathyla Lander SelomNessuna valutazione finora
- Sarcoma SacroDocumento10 pagineSarcoma SacroManuelGonzalezGaitanoNessuna valutazione finora
- Comparative evaluation of TADs vs Class III elasticsDocumento9 pagineComparative evaluation of TADs vs Class III elasticsSantiago VarelaNessuna valutazione finora
- Evaluation of The Utility of Cephalometric Parameters Part 1Documento5 pagineEvaluation of The Utility of Cephalometric Parameters Part 1Alejandra LorancaNessuna valutazione finora
- Sauve KapandjiDocumento3 pagineSauve KapandjiZieky YoansyahNessuna valutazione finora
- Nicholl 1995Documento5 pagineNicholl 1995intanlisaiNessuna valutazione finora
- 1992 Proestakis, Soderholm, Bratthall, Etc. Gingivectomy Versus Flap Surgery, The Effect of The Treatment of Infrabony DefectsDocumento13 pagine1992 Proestakis, Soderholm, Bratthall, Etc. Gingivectomy Versus Flap Surgery, The Effect of The Treatment of Infrabony DefectsAlejandro morenoNessuna valutazione finora
- Ocr 12416Documento7 pagineOcr 12416khaled mohammadNessuna valutazione finora
- Expansion RapidaDocumento11 pagineExpansion RapidaNayely MiguelNessuna valutazione finora
- Laparoscopic Gastrectomy for Cancer: Standard Techniques and Clinical EvidencesDa EverandLaparoscopic Gastrectomy for Cancer: Standard Techniques and Clinical EvidencesSeigo KitanoNessuna valutazione finora
- Evidenced-Based Approach to Soft Tissue ApproximationDocumento4 pagineEvidenced-Based Approach to Soft Tissue ApproximationAnonymous kdBDppigENessuna valutazione finora
- Bouché2012 Chapter ChronicCompartmentSyndromeOfLe PDFDocumento6 pagineBouché2012 Chapter ChronicCompartmentSyndromeOfLe PDFAnonymous kdBDppigENessuna valutazione finora
- Revision: Scar TechniquesDocumento4 pagineRevision: Scar TechniquesAnonymous kdBDppigENessuna valutazione finora
- Evaluation of Outcomes in Patients Following Surgical Treatment of Chronic Exertional Compartment Syndrome in The LegDocumento9 pagineEvaluation of Outcomes in Patients Following Surgical Treatment of Chronic Exertional Compartment Syndrome in The LegAnonymous kdBDppigENessuna valutazione finora
- Skin Local: PlastiesDocumento14 pagineSkin Local: PlastiesAnonymous kdBDppigENessuna valutazione finora
- TOI-) ND: Closi-) ReDocumento8 pagineTOI-) ND: Closi-) ReAnonymous kdBDppigENessuna valutazione finora
- Swanson: Flexible Hinge Toe ImplantDocumento14 pagineSwanson: Flexible Hinge Toe ImplantAnonymous kdBDppigENessuna valutazione finora
- Ptantar Anatomy: Tfie Skin Private SurgicalDocumento9 paginePtantar Anatomy: Tfie Skin Private SurgicalAnonymous kdBDppigENessuna valutazione finora
- Internal Fixation Podiatric: SurgeryDocumento7 pagineInternal Fixation Podiatric: SurgeryAnonymous kdBDppigENessuna valutazione finora
- Fundamental skin closure techniquesDocumento4 pagineFundamental skin closure techniquesAnonymous kdBDppigENessuna valutazione finora
- Locking Plate Techniques For Fracture Stability: Jay D. Ryan, DPMDocumento5 pagineLocking Plate Techniques For Fracture Stability: Jay D. Ryan, DPMAnonymous kdBDppigENessuna valutazione finora
- Talar Fractures: The Injury, The Management, and The AftermathDocumento17 pagineTalar Fractures: The Injury, The Management, and The AftermathAnonymous kdBDppigENessuna valutazione finora
- Closed Reduction and Internal Fixation of Lisfranc Fracture DislocationsDocumento8 pagineClosed Reduction and Internal Fixation of Lisfranc Fracture DislocationsAnonymous kdBDppigENessuna valutazione finora
- Intrinsicmuscleflapsfor Coverageofsmalldefectsin Thefoot: Grace Chuang CraigDocumento14 pagineIntrinsicmuscleflapsfor Coverageofsmalldefectsin Thefoot: Grace Chuang CraigAnonymous kdBDppigENessuna valutazione finora
- Swanson: Flexible Hinge Toe ImplantDocumento14 pagineSwanson: Flexible Hinge Toe ImplantAnonymous kdBDppigENessuna valutazione finora
- Open 4-Compartment Fasciotomy For Chronic Exertional Compartment Syndrome of The LegDocumento11 pagineOpen 4-Compartment Fasciotomy For Chronic Exertional Compartment Syndrome of The LegAnonymous kdBDppigENessuna valutazione finora
- Stress Modulation of Fracture Fixation Implants: Review ArticleDocumento9 pagineStress Modulation of Fracture Fixation Implants: Review ArticleAnonymous kdBDppigENessuna valutazione finora
- Multidirectional Instability of The Ankle: Surgical ReconstructionDocumento7 pagineMultidirectional Instability of The Ankle: Surgical ReconstructionAnonymous kdBDppigENessuna valutazione finora
- Core Decompression Ankle Pain ReliefDocumento9 pagineCore Decompression Ankle Pain ReliefAnonymous kdBDppigENessuna valutazione finora
- Percutaneous Osteotomies in Pediatric Deformity Correction: Nickolas Nahm,, Louise Reid Boyce NicholsDocumento16 paginePercutaneous Osteotomies in Pediatric Deformity Correction: Nickolas Nahm,, Louise Reid Boyce NicholsAnonymous kdBDppigENessuna valutazione finora
- Minimally Invasive Treatment of Displaced Intra-Articular Calcaneal FracturesDocumento14 pagineMinimally Invasive Treatment of Displaced Intra-Articular Calcaneal FracturesAnonymous kdBDppigENessuna valutazione finora
- Bone Marrow Stimulation and Biological Adjuncts For Treatment of Osteochondral Lesions of The TalusDocumento12 pagineBone Marrow Stimulation and Biological Adjuncts For Treatment of Osteochondral Lesions of The TalusAnonymous kdBDppigENessuna valutazione finora
- Unknown PDFDocumento6 pagineUnknown PDFAnonymous kdBDppigENessuna valutazione finora
- Swanson: Flexible Hinge Toe ImplantDocumento14 pagineSwanson: Flexible Hinge Toe ImplantAnonymous kdBDppigENessuna valutazione finora
- Pathophysiology of Tendinopathy: Michael Girdwood, Sean Docking, Ebonie Rio, and Jill CookDocumento22 paginePathophysiology of Tendinopathy: Michael Girdwood, Sean Docking, Ebonie Rio, and Jill CookAnonymous kdBDppigENessuna valutazione finora
- Wound: CtosureDocumento8 pagineWound: CtosureAnonymous kdBDppigENessuna valutazione finora
- ICD-10 PodiatryDocumento25 pagineICD-10 PodiatryAnonymous kdBDppigENessuna valutazione finora
- Swanson: Flexible Hinge Toe ImplantDocumento14 pagineSwanson: Flexible Hinge Toe ImplantAnonymous kdBDppigENessuna valutazione finora
- Skin: Unique Anatomy: The IowerDocumento3 pagineSkin: Unique Anatomy: The IowerAnonymous kdBDppigENessuna valutazione finora
- Swanson: Flexible Hinge Toe ImplantDocumento14 pagineSwanson: Flexible Hinge Toe ImplantAnonymous kdBDppigENessuna valutazione finora
- MM M Hall of Femme Ebook 62463Documento15 pagineMM M Hall of Femme Ebook 62463Tayaba Naim KhanNessuna valutazione finora
- Reasoning BookDocumento38 pagineReasoning BookAshish Sharma100% (1)
- Pathology of JointsDocumento13 paginePathology of JointswobblegobbleNessuna valutazione finora
- Acute otitis media in adults: An overviewDocumento15 pagineAcute otitis media in adults: An overviewchristineNessuna valutazione finora
- ACHALASIADocumento31 pagineACHALASIAkhan jeetNessuna valutazione finora
- IMSS Nursing Knowledge ExamDocumento11 pagineIMSS Nursing Knowledge ExamScribdTranslationsNessuna valutazione finora
- Hospital Job DescriptionsDocumento48 pagineHospital Job DescriptionsLoresita Amoranto Rebong RNNessuna valutazione finora
- Zingiber Officinale MonographDocumento5 pagineZingiber Officinale Monographc_j_bhattNessuna valutazione finora
- 53 Vol. 6 Issue 7 IJPSR 2015 RA 4953Documento9 pagine53 Vol. 6 Issue 7 IJPSR 2015 RA 4953Dina AyupnNessuna valutazione finora
- Classi Fications of Adverse Drug Reactions: 1. EidosDocumento6 pagineClassi Fications of Adverse Drug Reactions: 1. Eidosdolemite4Nessuna valutazione finora
- AcetaminophenDocumento2 pagineAcetaminophenKimskiusNessuna valutazione finora
- Iqvia Institute General Use of Medicines 2024 For WebDocumento60 pagineIqvia Institute General Use of Medicines 2024 For Webaguiar.jessicapNessuna valutazione finora
- Herb II-5-Herbs That Tonify Qi & BloodDocumento51 pagineHerb II-5-Herbs That Tonify Qi & BloodEdison halimNessuna valutazione finora
- Aims and Applications: Aims: The Three Aims of Pharmacoepidemiology AreDocumento10 pagineAims and Applications: Aims: The Three Aims of Pharmacoepidemiology Aregowtham0% (1)
- It PDFDocumento385 pagineIt PDFCosmina UngurNessuna valutazione finora
- Treatment Head LiceDocumento26 pagineTreatment Head LiceCherry Amor Betita MadronaNessuna valutazione finora
- 3 Azarpour Et Al. JNBR 4 (1) 2015 PDFDocumento9 pagine3 Azarpour Et Al. JNBR 4 (1) 2015 PDFKamailNessuna valutazione finora
- Msds MgOHDocumento5 pagineMsds MgOHCahyaGeriyanaNessuna valutazione finora
- Overdentures Improve Chewing Efficiency and Bone SupportDocumento8 pagineOverdentures Improve Chewing Efficiency and Bone SupportMezo SalahNessuna valutazione finora
- Anemia: Differential DiagnosisDocumento7 pagineAnemia: Differential DiagnosisZaman MigozaradNessuna valutazione finora
- Teen Pregnancy Rates in BoliviaDocumento2 pagineTeen Pregnancy Rates in BoliviaVanessa Sandoval Aguilera100% (1)
- Replacing ESR with Plasma ViscosityDocumento6 pagineReplacing ESR with Plasma ViscosityRyan ChenNessuna valutazione finora
- Types of Casts and Their IndicationsDocumento3 pagineTypes of Casts and Their IndicationsPhylum ChordataNessuna valutazione finora
- Emergency Welfare FormDocumento2 pagineEmergency Welfare FormKristopher HarperNessuna valutazione finora
- 20 Uses of Vicks VaporubDocumento3 pagine20 Uses of Vicks VaporubDrBertram ForerNessuna valutazione finora
- INNOVATIVE CARE LINEDocumento4 pagineINNOVATIVE CARE LINEJose Luis Paez NeiraNessuna valutazione finora